The Impact of Dietary Counselling on Achieving or Maintaining Normal Nutritional Status in Patients with Early and Locally Advanced Breast Cancer Undergoing Perioperative Chemotherapy
Abstract
:1. Introduction
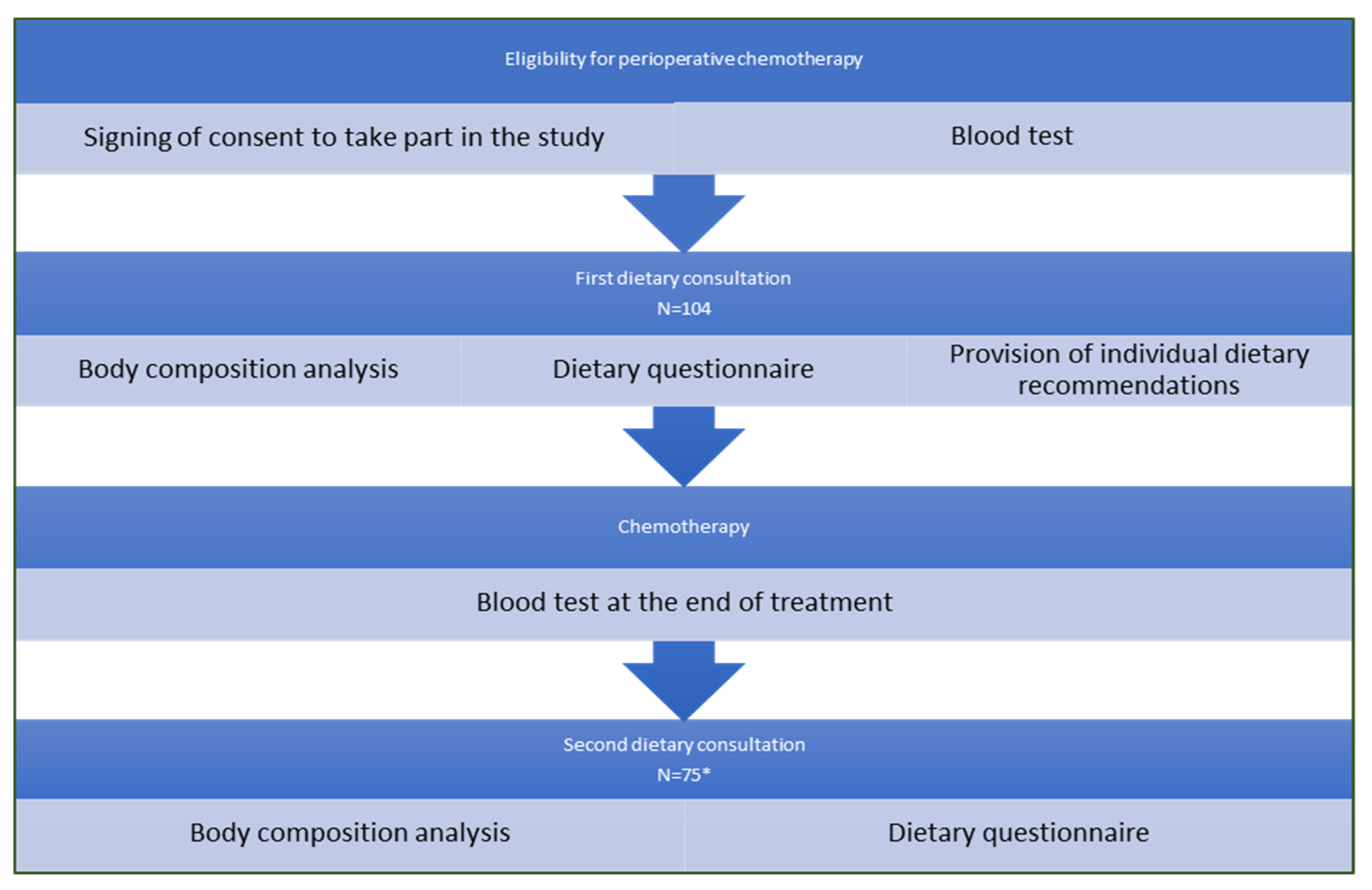
2. Purpose and Scope of Work
3. Material and Methods
3.1. Inclusion Criteria
3.2. Scope of the First Dietetic Consultation:
- Nutritional history;
- completion of the author’s questionnaire (Annex 2) on diet;
- evaluation of anthropometric parameters by means of body composition analysis with discussion of the results;
- analysis of laboratory lipid parameters;
- individual dietary advice on nutrition during chemotherapy.
3.3. Scope of the Second Dietetic Consultation:
- Reassessment of anthropometric parameters by means of body composition analysis with discussion of the result;
- discuss nutritional problems (nausea, vomiting, diarrhoea, food aversion) with chemotherapy with possible supplementary information on nutrition after chemotherapy;
- re-examination of laboratory lipid parameters;
- refilling in the same original questionnaire on diet.
3.4. Nutrition Education
- -
- regular consumption of 5 meals per day, including elimination of snacking between meals;
- -
- the recommended forms of heat treatment, including mainly the elimination of heat treatment with fat;
- -
- eliminating products that are sources of simple carbohydrates (sweets, confectionery, sweet dairy products, sweet drinks) and added sugar (sweetening drinks, sweetening salads, etc.)
- -
- eliminating fast food;
- -
- drink enough fluids (at least 2 litres/day);
- -
- eliminate alcohol consumption;
- -
- eating lean and unprocessed meat;
- -
- eating seafood (at least 2–3 times a week);
- -
- eating lean, natural dairy products;
- -
- eating vegetables (about 600 g) and fruit (200 g) except grapefruit and pomegranate.
3.5. Author’s Survey
3.6. Anthropometric Measurements
3.7. Laboratory Parameters Lipid Metabolism
3.8. Statistical Analysis
4. Results—Description of the Study Group
Analysis of Anthropometric and Laboratory Measurements before Treatment
5. Results—Changes after Treatment
5.1. Analysis of Parameters Related to Nutritional Status (Body Composition Analysis and Lipid Metabolism Laboratory Results) before and after Chemotherapy
5.2. Results of a Questionnaire on Diet before and after Chemotherapy
5.3. Comparison of Changes in BMI and Body Weight Values between Control and Study Groups
6. Discussion
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Didkowska, J.; Wojciechowska, U.; Czaderny, K.; Olasek, P.; Ciuba, A. Malignant Neoplasms in Poland in 2017; Centrum Onkologii-Instytut: Warsaw, Poland, 2019. [Google Scholar]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.; Atinmo, T.; Byers, T.; Chen, J.; Hirohata, T.; Jackson, A.; James, W.; Kolonel, L.; Kumanyika, S.; Leitzmann, C.; et al. Food, Nutrition, Physical Activity and the Prevention of Cancer: A Global Perspective; World Cancer Research Fund/American Institute for Cancer Research (AICR): Washington, DC, USA, 2007; p. 72. [Google Scholar]
- Cypess, A.M. Reassessing Human Adipose Tissue. N. Engl. J. Med. 2022, 386, 768–779. [Google Scholar] [CrossRef] [PubMed]
- Balkwill, F.; Mantovani, A. Inflammation and cancer: Back to Virchow? Lancet 2001, 357, 539–545. [Google Scholar] [CrossRef]
- Vaysse, C.; Lomo, J.; Garred, O.; Fjeldheim, F.; Lofteroed, T.; Schlichting, E.; McTiernan, A.; Frydenberg, H.; Husøy, A.; Lundgren, S.; et al. Inflammation of mammary adipose tissue occurs in overweight and obese patients exhibiting early-stage breast cancer. Npj Breast Cancer 2017, 3, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iyengar, N.M.; Zhou, X.K.; Gucalp, A.; Morris, P.G.; Howe, L.R.; Giri, D.D.; Morrow, M.; Wang, H.; Pollak, M.; Jones, L.W.; et al. Systemic correlates of white adipose tissue inflammation in early-stage breast cancer. Clin. Cancer Res. 2016, 22, 2283–2289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nindrea, R.D.; Aryandono, T.; Lazuardi, L.; Dwiprahasto, I. Association of Overweight and Obesity with Breast Cancer During Premenopausal Period in Asia: A Meta-Analysis. Int. J. Prev. Med. 2019, 10, 192. [Google Scholar] [CrossRef]
- Coquet, J.B.; Caballero, V.R.; Camisasso, M.C.; González, M.F.; Niclis, C.; Román, M.D.; Muñoz, S.E.; Leone, C.M.; Procino, F.; Osella, A.R.; et al. Diet Quality, Obesity and Breast Cancer Risk: An Epidemiologic Study in Córdoba, Argentina. Nutr. Cancer 2020, 72, 1026–1035. [Google Scholar] [CrossRef]
- Nyasani, E.; Munir, I.; Perez, M.; Payne, K.; Khan, S. Linking obesity-induced leptin-signaling pathways to common endocrine-related cancers in women. Endocrine 2019, 63, 3–17. [Google Scholar] [CrossRef]
- Neuhouser, M.L.; Aragaki, A.K.; Prentice, R.L.; Manson, J.E.; Chlebowski, R.; Carty, C.L.; Ochs-Balcom, H.M.; Thomson, C.A.; Caan, B.J.; Tinker, L.F.; et al. Overweight, obesity, and postmenopausal invasive breast cancer risk: A secondary analysis of the Women’s Health Initiative randomized clinical trials. JAMA Oncol. 2015, 1, 611–621. [Google Scholar] [CrossRef]
- Gravena, A.; Lopes, T.; Demitto, M.; Borghesan, D.H.P.; Agnolo, C.M.D.; Brischiliari, S.C.R.; Carvalho, M.D.d.; Pelloso, S.M. The Obesity and the Risk of Breast Cancer among Pre and Postmenopausal Women. Asian Pac. J. Cancer Prev. 2018, 19, 2429–2436. [Google Scholar]
- Chan, D.S.; Vieira, A.R.; Aune, D.; Bandera, E.V.; Greenwood, D.C.; McTiernan, A.; Rosenblatt, D.N.; Thune, I.; Vieira, R.; Norat, T.; et al. Body mass index and survival in women with breast cancer—Systematic literature review and meta-analysis of 82 follow-up studies. Ann. Oncol. 2014, 25, 1901–1914. [Google Scholar] [CrossRef] [PubMed]
- Harborg, S.; Zachariae, R.; Olsen, J.; Johannsen, M.; Cronin-Fenton, D.; Bøggild, H.; Borgquist, S. Overweight and prognosis in triple-negative breast cancer patients: A systematic review and meta-analysis. NPJ Breast Cancer 2021, 7, 119. [Google Scholar] [CrossRef] [PubMed]
- Karatas, F.; Erdem, G.U.; Sahin, S.; Aytekin, A.; Yuce, D.; Sever, A.R.; Babacan, T.; Ates, O.; Ozisik, Y.; Altundag, K. Obesity is an independent prognostic factor of decreased pathological complete response to neoadjuvant chemotherapy in breast cancer patients. The Breast 2017, 32, 237–244. [Google Scholar] [CrossRef]
- Iwase, T.; Nakamura, R.; Yamamoto, N.; Yoshi, A.; Itami, M.; Miyazaki, M. The effect of molecular subtype and body mass index on neo-adjuvant chemotherapy in breast cancer patients. Breast 2014, 23, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.; Coburn, S.B.; Matthews, C.E.; Falk, R.T.; LeBlanc, E.S.; Wactawski-Wende, J.; Sampson, J.; Pfeiffer, R.M.; Brinton, L.A.; Wentzensen, N.; et al. Anthropometric measures and serum estrogen metabolism in postmenopausal women: The Women’s Health Initiative Observational Study. Breast Cancer Res. 2017, 19, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iyengar, N.M.; Arthur, R.; Manson, J.E.; Chlebowski, R.T.; Kroenke, C.H.; Peterson, L.; Cheng, T.D.; Feliciano, E.C.; Lane, D.; Luo, J.; et al. Association of Body Fat and Risk of Breast Cancer in Postmenopausal Women with Normal Body Mass Index. A Secondary Analysis of a Randomized Clinical Trial and Observational Study. JAMA Oncol. 2019, 5, 155–163. [Google Scholar] [CrossRef]
- Makarem, N.; Chandran, U.; Bandera, E.V.; Parekh, N. Dietary fat in breast cancer survival. Annu. Rev. Nutr. 2013, 33, 319–348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knight, J.A.; Fan, J.; Malone, K.E.; John, E.M.; Lynch, C.F.; Langballe, R.; Bernstein, L.; Shore, R.E.; Brooks, J.D.; Reiner, A.S.; et al. Alcohol consumption and cigarette smoking in combination: A predictor of contralateral breast cancer risk in the WECARE study. Int. J. Cancer 2017, 141, 916–924. [Google Scholar] [CrossRef] [PubMed]
- Kłęk, S.; Jankowski, M.; Kruszewski, W.J.; Fijuth, J.; Kapała, A.; Kabata, P.; Wysocki, P.; Krzakowski, M.; Rutkowski, P. Clinical Nutrition in Oncology: Polish Recommendations. Oncol. Clin. Pract. 2015, 11, 172–188. [Google Scholar]
- Kapała, A. Diet in Cancer; Bouchman: Warsaw, Poland, 2016. [Google Scholar]
- D’Aiuto, M.; Chirico, A.; De Riggi, M.A.; Frasci, G.; de Laurentiis, M.; di Bonito, M.; Vici, P.; Pizzuti, L.; Sergi, D.; Maugeri-Saccà, M.; et al. Body mass index and treatment outcomes following neoadjuvant therapy in women aged 45 y or younger: Evidence from a historical cohort. Cancer Biol. Ther. 2016, 17, 470–476. [Google Scholar] [CrossRef]
- Picon-Ruiz, M.; Morata-Tarifa, C.; Valle-Goffin, J.J.; Friedman, E.R.; Slingerland, J.M. Obesity and adverse breast cancer risk and outcome: Mechanistic insights and strategies for intervention. CA Cancer J. Clin. 2017, 67, 378–397. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.H.; An, Y.; Ahn, C.; Park, B.; Lee, M.H.; Noh, D.-Y.; Park, S.K. Body mass index and risk of breast cancer molecular subtypes in Korean women: A case-control study. Breast Cancer Res. Treat. 2020, 179, 459–470. [Google Scholar] [CrossRef] [PubMed]
- Ford, M.E.; Bauza, C.E.; Findlay, V.J.; Turner, D.P.; Abraham, L.M.; Moore, L.A.; Magwood, G.; Alberg, A.J.; Gaymon, K.; Knight, K.D.; et al. BMI, physical activity, and breast cancer subtype in white, black, and Sea Island breast cancer survivors. Adv. Cancer Res. 2020, 146, 83–102. [Google Scholar] [PubMed]
- Cortesi, L.; Sebastiani, F.; Iannone, A.; Marcheselli, L.; Venturelli, M.; Piombino, C.; Toss, A.; Federico, M. Lifestyle Intervention on Body Weight and Physical Activity in Patients with Breast Cancer can reduce the Risk of Death in Obese Women: The EMILI Study. Cancers 2020, 12, 1709. [Google Scholar] [CrossRef]
- Van den Berg, M.M.G.A.; Kok, D.E.; Visser, M.; de Vries, J.H.M.; de Kruif, J.T.C.M.; de Vries, Y.; Posthuma, L.; Sommeijer, D.W.; Timmer-Bonte, A.; Los, M.; et al. Changes in body composition during and after adjuvant or neo-adjuvant chemotherapy in women with breast cancer stage I-IIIB compared with changes over a similar timeframe in women without cancer. Supportive Care Cancer 2020, 28, 1685–1693. [Google Scholar] [CrossRef] [Green Version]
- Van den Berg, M.M.G.A.; Kok, D.E.; Posthuma, L.; Kamps, L.; Kelfkens, C.S.; Buist, N.; Geenen, M.; Haringhuizen, A.; Heijns, J.B.; van Lieshout, R.H.M.A.; et al. Body composition is associated with risk of toxicity-induced modifications of treatment in women with stage I-IIIB breast cancer receiving chemotherapy. Breast Cancer Res. Treat. 2019, 173, 475–481. [Google Scholar] [CrossRef] [Green Version]
- Pedersen, B.; Groenkjaer, M.; Falkmer, U.; Delmar, C. Understanding the Essential Meaning of Measured Changes in Weight and Body Composition Among Women During and After Adjuvant Treatment for Breast Cancer: A Mixed-Methods Study. Cancer Nurs. 2017, 40, 433–444. [Google Scholar] [CrossRef]
- Tian, W.; Yao, Y.; Fan, G.; Zhou, Y.; Wu, M.; Xu, D.; Deng, Y. Changes in lipid profiles during and after (neo) adjuvant chemotherapy in women with earlystage breast cancer: A retrospective study. PLoS ONE 2019, 14, e0221866. [Google Scholar] [CrossRef]
- Yeo, W.; Mo, F.K.F.; Pang, E.; Suen, J.J.S.; Koh, J.; Loong, H.H.F.; Yip, C.C.H.; Ng, R.Y.W.; Yip, C.H.W.; Tang, N.L.S.; et al. Profiles of lipids, blood pressure and weight changes among premenopausal Chinese breast cancer patients after adjuvant chemotherapy. BMC Womens Health 2017, 17, 55. [Google Scholar] [CrossRef]
- Heideman, W.H.; Russellb, N.S.; Gundya, C.; Rookusa, M.A.; Voskuila, D.W. The frequency, magnitude and timing of post-diagnosis body weight gain in Dutch breast cancer survivors. Eur. J. Cancer 2009, 45, 119–126. [Google Scholar] [CrossRef]
- Fang, Q.; Gan, L.; Chen, Y.; Shen, K.; Wu, B. Percent Body Fat Change in Chinese Women After Adjuvant Chemotherapy for Breast Cancer Med. Sci. Monit. 2018, 24, 5988–5995. [Google Scholar] [CrossRef] [PubMed]
- Van den Berg, M.M.G.A.; Winkels, R.M.; de Kruif, J.T.C.M.; van Laarhoven, H.W.M.; Visser, M.; de Vries, J.H.M.; de Vries, Y.C.; Kampman, E. Weight change during chemotherapy in breast cancer patients: A meta-analysis. BMC Cancer 2017, 17, 259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, G.H.; Kimb, J.H.; Chung, M.S. Changes in weight, body composition, and physical activity among patients with breast cancer under adjuvant chemotherapy. Eur. J. Oncol. Nurs. 2020, 44, 101680. [Google Scholar] [CrossRef] [PubMed]
- Mutschler, N.S.; Scholz, C.; Friedl, T.W.P.; Zwingers, T.; Fasching, P.A.; Beckmann, M.W.; Fehm, T.; Mohrmann, S.; Salmen, J.; Ziegler, C.; et al. Prognostic Impact of Weight Change During Adjuvant Chemotherapy in Patients with High-Risk Early Breast Cancer: Results from the ADEBAR Study. Clin. Breast Cancer 2018, 18, 175–183. [Google Scholar] [CrossRef]
- Limon-Miro, A.T.; Valencia, M.E.; Lopez-Teros, V.; Guzman-Leon, A.E.; Mendivil-Alvarado, H.; Astiazaran-Garcia, H. Bioelectric Impedance Vector Analysis (BIVA) in Breast Cancer Patients: A Tool for Research and Clinical Practice. Medicina 2019, 55, 663. [Google Scholar] [CrossRef] [Green Version]
- Freedman, R.J.; Aziz, N.; Albanes, D.; Hartman, T.; Danforth, D.; Hill, S.; Sebring, N.; Reynolds, J.C.; Yanovski, J.A. Weight and Body Composition Changes during and after Adjuvant Chemotherapy in Women with Breast Cancer. J. Clin. Endocrinol. Metab. 2004, 89, 2248–2253. [Google Scholar] [CrossRef] [Green Version]
- Li, X.; Liu, Z.L.; Wu, Y.T.; Wu, H.; Dai, W.; Arshad, B.; Xu, Z.; Li, H.; Wu, K.; Kong, L. Lipid and lipoprotein status in female breast cancer patients at initial diagnosis and during chemotherapy. Lipids Health Dis. 2018, 17, 91. [Google Scholar] [CrossRef] [Green Version]
- He, T.; Wang, C.; Tan, Q.; Wang, Z.; Li, J.; Chen, T.; Cui, K.; Wu, Y.; Sun, J.; Zheng, D.; et al. Adjuvant chemotherapy-associated lipid changes in breast cancer patients: A real-word retrospective analysis. Medicine 2020, 99, e21498. [Google Scholar] [CrossRef]
- Delgobo, M.; Agnes, J.P.; Goncalves, R.M.; dos Santos, V.W.; Parisotto, E.B.; Zamoner, A.; Zanotto-Filho, A. N-acetylcysteine and alpha-lipoic acid improve antioxidant defenses and decrease oxidative stress, inflammation and serum lipid levels in ovariectomized rats via estrogen-independent mechanisms. J. Nutr. Biochem. 2019, 67, 190–200. [Google Scholar] [CrossRef]
- Vehmanen, L.; Saarto, T.; Blomqvist, C.; Taskinen, M.R.; Elomaa, I. Tamoxifen treatment reverses the adverse effects of chemotherapy-induced ovarian failure on serum lipids. Br. J. Cancer 2004, 91, 476–481. [Google Scholar] [CrossRef]
- Ma, B.; Yeo, W.; Hui, P.; Ho, W.M.; Johnson, P.J. Acute toxicity of adjuvant doxorubicin and cyclophosphamide for early breast cancer—A retrospective review of Chinese patients and comparison with an historic Western series. Radiother. Oncol. 2002, 62, 185–189. [Google Scholar] [CrossRef]
- Anderson, C.; Harriigan, M.; George, S.M.; Ferrucci, L.M.; Sanft, T.; Irwin, M.L.; Cartmel, B. Changes in diet quality in a randomized weight loss trial in breast cancer survivors: The lifestyle, exercise, and nutrition (LEAN) study. EG Breast Cancer 2016, 2, 16026. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variable | Parameter | Dietary Consultation Group | Control Group | ||
|---|---|---|---|---|---|
| N = 104 | % | N = 40 | % | ||
| cT | 0 | 1 | 1 | 0 | 0 |
| 1 | 8 | 7.7 | 4 | 10 | |
| 2 | 58 | 55.7 | 23 | 57.5 | |
| 3 | 34 | 32.7 | 12 | 30 | |
| 4d | 3 | 2.9 | 1 | 2.5 | |
| cN | 0 | 49 | 47.2 | 10 | 25 |
| 1 | 46 | 44.2 | 25 | 62.5 | |
| 2 | 5 | 4.8 | 4 | 10 | |
| 3 | 4 | 3.8 | 1 | 2.5 | |
| G | 1 | 11 | 10.5 | 3 | 7.5 |
| 2 | 65 | 62.5 | 29 | 72.5 | |
| 3 | 28 | 27 | 8 | 20 | |
| ER | positive | 40 | 38.5 | 12 | 30 |
| negative | 64 | 61.5 | 28 | 70 | |
| PR | positive | 32 | 30.8 | 11 | 27.5 |
| negative | 72 | 69.2 | 29 | 72.5 | |
| HER2 | positive | 15 | 14,4 | 4 | 10 |
| negative | 89 | 85.6 | 36 | 90 | |
| Type of neoadjuvant treatment | TCarbH | 15 | 14.4 | 4 | 10 |
| ACdd/ PCL weekly | 45 | 43.3 | 19 | 47.5 | |
| AC/PCL weekly | 44 | 42.3 | 17 | 42.5 | |
| Characteristics of achieved responses to treatment | pCR | 64 | 61.5 | 22 | 55 |
| Non-pCR | 40 | 38.5 | 18 | 45 | |
| All N = 104 | Before Menopause N = 72 | After the Menopause N = 32 | |
|---|---|---|---|
| BMI: <18.49 | 3 (2.9%) | 3 (4.2%) | 0 (0%) |
| BMI: 18.5–24.99 | 43 (41.4%) | 36 (50%) | 7 (21.9%) |
| BMI: 25.0–29.99 | 33 (31.7%) | 17 (23.6) | 16 (50%) |
| BMI: ≥30 | 25 (24%) | 16 (22.2%) | 9 (28.1%) |
| %Fat—normal | 54 (51.9%) | 41 (57%) | 13 (40.6%) |
| %Fat above normal | 43 (41.4%) | 25 (34.7%) | 18 (56.3%) |
| % Fat below normal | 7 (6.7%) | 6 (8.3%) | 1 (3.1%) |
| All N = 104 | Before Menopause N = 72 | After the Menopause N = 32 | p Value | ||||
|---|---|---|---|---|---|---|---|
| Average | SD | Average | SD | Average | SD | ||
| Fat (%) | 31.6 | 7.4 | 29.8 | 7.1 | 35.2 | 7.0 | 0.0054 * |
| Fat mass (kg) | 22.2 | 8.3 | 20.6 | 7.9 | 25.3 | 8.3 | 0.0279 * |
| FFM—Fat-free Mass (kg) | 45.4 | 5.9 | 45.6 | 6.4 | 45.0 | 5.0 | 0.540 |
| TBW—Total body water (%) | 33.5 | 3.6 | 33.8 | 3.6 | 32.9 | 3.7 | 0.458 |
| All N = 104 | Before Menopause N = 72 | After the Menopause N = 32 | p Value | ||||
|---|---|---|---|---|---|---|---|
| Average | SD | Average | SD | Average | SD | ||
| Total cholesterol mg/gL | 188.2+ | 46.5 | 178.5 | 45.9 | 207.7 | 41.9 | 0.0219 * |
| HDL (mg/dL) | 53.9 | 14.4 | 52.3 | 15.8 | 57.0 | 10.9 | 0.05 |
| LDL (mg/dL) | 113.1 | 33.7 | 110.2 | 31.0 | 119.5 | 39.2 | 0.54 |
| TG (mg/dL) | 107.7 | 60.8 | 99.7 | 52.9 | 124.1 | 72.9 | 0.138 |
| N = 75 | Before | After | Change | p Value | |||
|---|---|---|---|---|---|---|---|
| Average | SD | Average | SD | Average | SD | ||
| Body weight (kg) | 68.2 | 12.0 | 68.4 | 11.5 | 0.1 | 4.4 | 0.671 |
| BMI (kg/m2) | 25.3 | 4.4 | 25.5 | 4.3 | 0.1 | 1.4 | 0.274 |
| Fat (%) | 31.6 | 7.4 | 30.2 | 6.8 | −1.8 | 3.9 | <0.001 * |
| Fat mass (kg) | 22.2 | 8.3 | 21.4 | 7.8 | −1.2 | 3.5 | 0.018 * |
| FFM—fat-free mass (kg) | 45.4 | 5.9 | 47.1 | 5.9 | 1.5 | 5.4 | <0.001 * |
| TBW—total body water (%) | 33.5 | 3.6 | 34.8 | 3.5 | 1.2 | 1.4 | <0.001 * |
| N = 75 | Before | After | Change | p Value | |||
|---|---|---|---|---|---|---|---|
| Average | SD | Average | SD | Average | SD | ||
| Total cholesterol (mg/dL) | 188.2 | 46.4 | 196.6 | 44.4 | 8.9 | 48.4 | 0.019 * |
| HDL (mg/dL) | 53.9 | 14.4 | 50.7 | 11.0 | −3.3 | 10.4 | 0.027 * |
| LDL (mg/dL) | 113.1 | 33.7 | 124.4 | 54.3 | 12.6 | 52.5 | 0.019 * |
| TG (mg/dL) | 107.7 | 60.8 | 146.8 | 84.9 | 42.1 | 74.6 | <0.001 * |
| N = 75 | Before | After | Change | p Value | |||
|---|---|---|---|---|---|---|---|
| Average | SD | Average | SD | Average | SD | ||
| Survey points | 7.4 | 3.5 | 12.2 | 3.3 | 4.8 | 4.4 | <0.001 * |
| Control Group N = 40 | Study Group N = 75 | p Value | |||
|---|---|---|---|---|---|
| Average | SD | Average | SD | ||
| Body weight delta (kg) | 1.8 | 3.8 | 0.1 | 4.4 | p= 0.023 * |
| Delta BMI (kg/m2) | 0.7 | 1.4 | 0.1 | 1.4 | 0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jodkiewicz, M.; Jagiełło-Gruszfeld, A.; Surwiłło-Snarska, A.; Kotowicz, B.; Fuksiewicz, M.; Kowalska, M.M. The Impact of Dietary Counselling on Achieving or Maintaining Normal Nutritional Status in Patients with Early and Locally Advanced Breast Cancer Undergoing Perioperative Chemotherapy. Nutrients 2022, 14, 2541. https://doi.org/10.3390/nu14122541
Jodkiewicz M, Jagiełło-Gruszfeld A, Surwiłło-Snarska A, Kotowicz B, Fuksiewicz M, Kowalska MM. The Impact of Dietary Counselling on Achieving or Maintaining Normal Nutritional Status in Patients with Early and Locally Advanced Breast Cancer Undergoing Perioperative Chemotherapy. Nutrients. 2022; 14(12):2541. https://doi.org/10.3390/nu14122541
Chicago/Turabian StyleJodkiewicz, Magdalena, Agnieszka Jagiełło-Gruszfeld, Agnieszka Surwiłło-Snarska, Beata Kotowicz, Małgorzata Fuksiewicz, and Maria Małgorzata Kowalska. 2022. "The Impact of Dietary Counselling on Achieving or Maintaining Normal Nutritional Status in Patients with Early and Locally Advanced Breast Cancer Undergoing Perioperative Chemotherapy" Nutrients 14, no. 12: 2541. https://doi.org/10.3390/nu14122541
APA StyleJodkiewicz, M., Jagiełło-Gruszfeld, A., Surwiłło-Snarska, A., Kotowicz, B., Fuksiewicz, M., & Kowalska, M. M. (2022). The Impact of Dietary Counselling on Achieving or Maintaining Normal Nutritional Status in Patients with Early and Locally Advanced Breast Cancer Undergoing Perioperative Chemotherapy. Nutrients, 14(12), 2541. https://doi.org/10.3390/nu14122541






