A Cross-Sectional Pilot Study on Food Intake Patterns Identified from Very Short FFQ and Metabolic Factors Including Liver Function in Healthy Japanese Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Anthropometrics, Blood Pressure, and Biochemical Measurements
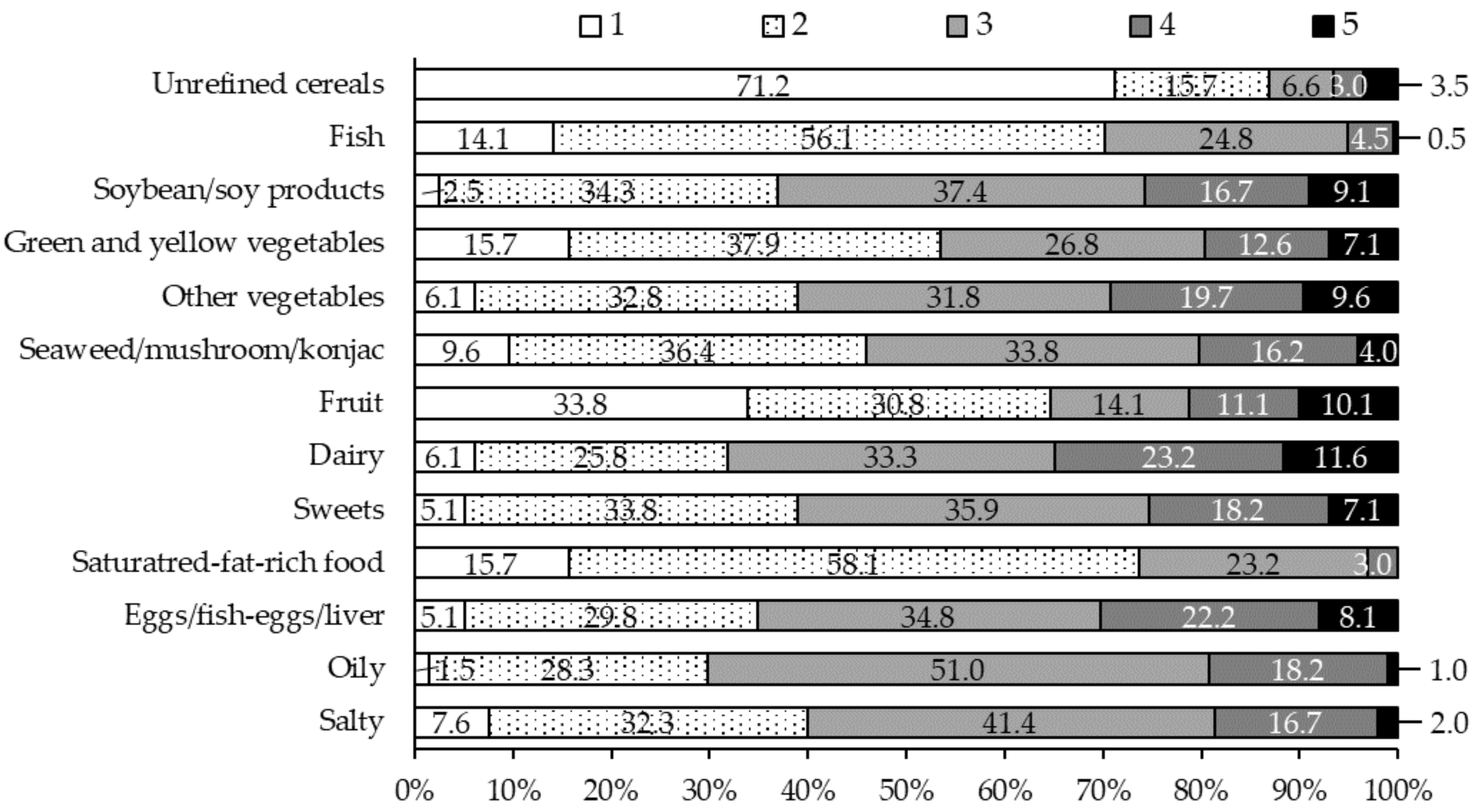
2.3. Food Frequency Questionnaire
2.4. Dietary Records and Physical Activity
2.5. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ministry of Health, Labour and Welfare. The National Health and Nutrition Survey in Japan. Trends in Prevalance of Obesity (BMI ≥ 25) and Underweight (BMI < 18.5), 1973–2019 (Subjects Aged 15 Years and Over, by Gender and Age). Available online: https://www.nibiohn.go.jp/eiken/kenkounippon21/eiyouchousa/keinen_henka_shintai.html (accessed on 11 May 2022).
- Keys, A.; Menotti, A.; Karvonen, M.J.; Aravanis, C.; Blackburn, H.; Buzina, R.; Djordjevic, B.S.; Dontas, A.S.; Fidanza, F.; Keys, M.H.; et al. The diet and 15-year death rate in the seven countries study. Am. J. Epidemiol. 1986, 124, 903–915. [Google Scholar] [CrossRef] [PubMed]
- Kromhout, D.; Keys, A.; Aravanis, C.; Buzina, R.; Fidanza, F.; Giampaoli, S.; Jansen, A.; Menotti, A.; Nedeljkovic, S.; Pekkarinen, M.; et al. Food consumption patterns in the 1960s in seven countries. Am. J. Clin. Nutr. 1989, 49, 889–894. [Google Scholar] [CrossRef] [PubMed]
- Kromhout, D.; Menotti, A.; Bloemberg, B.; Aravanis, C.; Blackburn, H.; Buzina, R.; Dontas, A.S.; Fidanza, F.; Giampaoli, S.; Jansen, A.; et al. Dietary saturated and trans fatty acids and cholesterol and 25-year mortality from coronary heart disease: The seven countries study. Prev. Med. 1995, 24, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Tada, N.; Maruyama, C.; Koba, S.; Tanaka, H.; Birou, S.; Teramoto, T.; Sasaki, J. Japanese dietary lifestyle and cardiovascular disease. J. Atheroscler. Thromb. 2011, 18, 723–734. [Google Scholar] [CrossRef] [Green Version]
- Otsuka, R.; Yatsuya, H.; Tamakoshi, K. Descriptive epidemiological study of food intake among Japanese adults: Analyses by age, time and birth cohort model. BMC Public Health 2014, 14, 328. [Google Scholar] [CrossRef] [Green Version]
- Saito, A.; Matsumoto, M.; Hyakutake, A.; Saito, M.; Okamoto, N.; Tsuji, M. The frequency of cooking dinner at home and its association with nutrient intake adequacy among married young-to-middle-aged Japanese women: The POTATO study. J. Nutr. Sci. 2019, 8, e14. [Google Scholar] [CrossRef] [Green Version]
- Larson-Meyer, D.E.; Newcomer, B.R.; Heilbronn, L.K.; Volaufova, J.; Smith, S.R.; Alfonso, A.J.; Lefevre, M.; Rood, J.C.; Williamson, D.A.; Ravussin, E. Effect of 6-month calorie restriction and exercise on serum and liver lipids and markers of liver function. Obesity 2008, 16, 1355–1362. [Google Scholar] [CrossRef] [Green Version]
- Riazi, K.; Raman, M.; Taylor, L.; Swain, M.G.; Shaheen, A.A. Dietary patterns and components in nonalcoholic fatty liver disease (NAFLD): What key messages can health care providers offer? Nutrients 2019, 11, 2878. [Google Scholar] [CrossRef] [Green Version]
- Castro-Barquero, S.; Ruiz-León, A.M.; Sierra-Pérez, M.; Estruch, R.; Casas, R. Dietary strategies for metabolic syndrome: A comprehensive review. Nutrients 2020, 12, 2983. [Google Scholar] [CrossRef]
- George, E.S.; Forsyth, A.; Itsiopoulos, C.; Nicoll, A.J.; Ryan, M.; Sood, S.; Roberts, S.K.; Tierney, A.C. Practical dietary recommendations for the prevention and management of nonalcoholic fatty liver disease in adults. Adv. Nutr. 2018, 9, 30–40. [Google Scholar] [CrossRef] [Green Version]
- European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 2016, 64, 1388–1402. [Google Scholar] [CrossRef]
- Anania, C.; Perla, F.M.; Olivero, F.; Pacifico, L.; Chiesa, C. Mediterranean diet and nonalcoholic fatty liver disease. World J. Gastroenterol. 2018, 24, 2083–2094. [Google Scholar] [CrossRef]
- Kamada, Y.; Takahashi, H.; Shimizu, M.; Kawaguchi, T.; Sumida, Y.; Fujii, H.; Seko, Y.; Fukunishi, S.; Tokushige, K.; Nakajima, A.; et al. Clinical practice advice on lifestyle modification in the management of nonalcoholic fatty liver disease in Japan: An expert review. J. Gastroenterol. 2021, 56, 1045–1061. [Google Scholar] [CrossRef]
- Maruyama, C.; Mae, A.; Umezawa, A.; Takahashi, T.; Umezawa, C.; Nakamura, H.; Kameyama, N. Study on validity and reproducibility of very short food frequency questionnaire (improved Plus1 Minus1) for use on nutrition education of risk factors associated with atherosclerotic diseases. J. Jpn. Soc. Metab. Clin. Nutr. 2022, 25, 187–198. (In Japanese) [Google Scholar]
- Matsuzawa, Y.; Tokunaga, K.; Kotani, K.; Keno, Y.; Kobayashi, T.; Tarui, S. Simple estimation of ideal body weight from body mass index with the lowest morbidity. Diabetes Res. Clin. Pract. 1990, 10 (Suppl. 1), S159–S164. [Google Scholar] [CrossRef]
- Tokunaga, K.; Matsuzawa, Y.; Kotani, K.; Keno, Y.; Kobatake, T.; Fujioka, S.; Tarui, S. Ideal body weight estimated from the body mass index with the lowest morbidity. Int. J. Obes. 1991, 15, 1–5. [Google Scholar]
- Bedogni, G.; Bellentani, S.; Miglioli, L.; Masutti, F.; Passalacqua, M.; Castiglione, A.; Tiribelli, C. The fatty liver index: A simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006, 6, 33. [Google Scholar] [CrossRef] [Green Version]
- Takeda-Imai, F.; Yamamoto, S.; Fujii, H.; Noda, M.; Inoue, M.; Tsugane, S. Validity and reproducibility of the self-administered shorter version of the physical activity questionnaire used in the JPHC study. Res. Exerc. Epidemiol. 2010, 12, 1–10. (In Japanese) [Google Scholar]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R., Jr.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci Sports Exerc. 2000, 32 (Suppl. 1), S498–S504. [Google Scholar] [CrossRef] [Green Version]
- Maruyama, K.; Iso, H.; Date, C.; Kikuchi, S.; Watanabe, Y.; Wada, Y.; Inaba, Y.; Tamakoshi, A.; JACC Study Group. Dietary patterns and risk of cardiovascular deaths among middle-aged Japanese: JACC study. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 519–527. [Google Scholar] [CrossRef]
- Shimazu, T.; Kuriyama, S.; Hozawa, A.; Ohmori, K.; Sato, Y.; Nakaya, N.; Nishino, Y.; Tsubono, Y.; Tsuji, I. Dietary patterns and cardiovascular disease mortality in Japan: A prospective cohort study. Int. J. Epidemiol. 2007, 36, 600–609. [Google Scholar] [CrossRef] [Green Version]
- Nanri, A.; Mizoue, T.; Shimazu, T.; Ishihara, J.; Takachi, R.; Noda, M.; Iso, H.; Sasazuki, S.; Sawada, N.; Tsugane, S.; et al. Dietary patterns and all-cause, cancer, and cardiovascular disease mortality in Japanese men and women: The Japan public health center-based prospective study. PLoS ONE 2017, 12, e0174848. [Google Scholar] [CrossRef]
- Okada, E.; Nakamura, K.; Ukawa, S.; Wakai, K.; Date, C.; Iso, H.; Tamakoshi, A. The Japanese food score and risk of all-cause, CVD and cancer mortality: The Japan collaborative cohort study. Br. J. Nutr. 2018, 120, 464–471. [Google Scholar] [CrossRef] [Green Version]
- Ma, E.; Ohira, T.; Sakai, A.; Yasumura, S.; Takahashi, A.; Kazama, J.; Shimabukuro, M.; Nakano, H.; Okazaki, K.; Maeda, M.; et al. Associations between dietary patterns and cardiometabolic risks in Japan: A cross-sectional study from the Fukushima health management survey, 2011–2015. Nutrients 2020, 12, 129. [Google Scholar] [CrossRef] [Green Version]
- Nanri, A.; Mizoue, T.; Yoshida, D.; Takahashi, R.; Takayanagi, R. Dietary patterns and A1C in Japanese men and women. Diabetes Care 2008, 31, 1568–1573. [Google Scholar] [CrossRef] [Green Version]
- Tanisawa, K.; Ito, T.; Kawakami, R.; Usui, C.; Kawamura, T.; Suzuki, K.; Sakamoto, S.; Ishii, K.; Muraoka, I.; Oka, K.; et al. Association between alcohol dietary pattern and prevalence of dyslipidaemia: WASEDA’S health study. Br. J. Nutr. 2021, 1–11. [Google Scholar] [CrossRef]
- Akter, S.; Nanri, A.; Pham, N.M.; Kurotani, K.; Mizoue, T. Dietary patterns and metabolic syndrome in a Japanese working population. Nutr. Metab. 2013, 10, 30. [Google Scholar] [CrossRef] [Green Version]
- Arisawa, K.; Uemura, H.; Yamaguchi, M.; Nakamoto, M.; Hiyoshi, M.; Sawachika, F.; Katsuura-Kamano, S. Associations of dietary patterns with metabolic syndrome and insulin resistance: A cross-sectional study in a Japanese population. J. Med. Investig. 2014, 61, 333–344. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health, Labour and Welfare. The National Health and Nutrition Survey in Japan. Trends in Mean Intakes by Food Group, 2003–2017. Available online: https://www.e-stat.go.jp/dbview?sid=0003224923&msclkid=61f9ed92d0ec11ecb1a1afcaa0102249 (accessed on 11 May 2022).
- Chichibu, H.; Yamagishi, K.; Kishida, R.; Maruyama, K.; Hayama-Terada, M.; Shimizu, Y.; Muraki, I.; Umesawa, M.; Cui, R.; Imano, H.; et al. Seaweed intake and risk of cardiovascular disease: The circulatory risk in communities study (CIRCS). J. Atheroscler. Thromb. 2021, 28, 1298–1306. [Google Scholar] [CrossRef]
- Nakashita, C.; Xi, L.; Inoue, Y.; Kabura, R.; Masuda, S.; Yamano, Y.; Katoh, T. Impact of dietary compositions and patterns on the prevalence of nonalcoholic fatty liver disease in Japanese men: A cross-sectional study. BMC Gastroenterol. 2021, 21, 342. [Google Scholar] [CrossRef]
- Ito, T.; Kawakami, R.; Tanisawa, K.; Miyawaki, R.; Ishii, K.; Torii, S.; Suzuki, K.; Sakamoto, S.; Muraoka, I.; Oka, K.; et al. Dietary patterns and abdominal obesity in middle-aged and elderly Japanese adults: Waseda alumni’s sports, exercise, daily activity, sedentariness and health study (WASEDA’S health study). Nutrition 2019, 58, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.K.; Baek, K.H.; Kang, M.I.; Park, S.E.; Rhee, E.J.; Park, C.Y.; Lee, W.Y.; Oh, K.W. Serum alkaline phosphatase, body composition, and risk of metabolic syndrome in middle-aged Korean. Endocr. J. 2013, 60, 321–328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sheng, G.; Peng, N.; Hu, C.; Zhong, L.; Zhong, M.; Zou, Y. The albumin-to-alkaline phosphatase ratio as an independent predictor of future non-alcoholic fatty liver disease in a 5-year longitudinal cohort study of a non-obese Chinese population. Lipids Health Dis. 2021, 20, 50. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.H.; Petroski, G.F.; Diaz-Arias, A.A.; Al Juboori, A.; Wheeler, A.A.; Ganga, R.R.; Pitt, J.B.; Spencer, N.M.; Hammoud, G.M.; Rector, R.S.; et al. A model incorporating serum alkaline phosphatase for prediction of liver fibrosis in adults with obesity and nonalcoholic fatty liver disease. J. Clin. Med. 2021, 10, 3311. [Google Scholar] [CrossRef]
- Tien, N.V.; Arisawa, K.; Uemura, H.; Imaeda, N.; Goto, C.; Katsuura-Kamano, S. Association between nutrient patterns and fatty liver index: Baseline survey of the Japan multi-institutional collaborative cohort study in Tokushima, Japan. J. Epidemiol. 2021. [Google Scholar] [CrossRef]
- Barchetta, I.; Cimini, F.A.; Cavallo, M.G. Vitamin D and metabolic dysfunction-associated fatty liver disease (MAFLD): An update. Nutrients 2020, 12, 3302. [Google Scholar] [CrossRef]
- Ganji, S.H.; Kashyap, M.L.; Kamanna, V.S. Niacin inhibits fat accumulation, oxidative stress, and inflammatory cytokine IL-8 in cultured hepatocytes: Impact on non-alcoholic fatty liver disease. Metabolism 2015, 64, 982–990. [Google Scholar] [CrossRef]
- Kinoshita, M.; Yokote, K.; Arai, H.; Iida, M.; Ishigaki, Y.; Ishibashi, S.; Umemoto, S.; Egusa, G.; Ohmura, H.; Okamura, T.; et al. Japan Atherosclerosis Society (JAS) guidelines for prevention of atherosclerotic cardiovascular diseases 2017. J. Atheroscler. Thromb. 2018, 25, 846–984. [Google Scholar] [CrossRef] [Green Version]
- Maruyama, C.; Nakano, R.; Shima, M.; Mae, A.; Shijo, Y.; Nakamura, E.; Okabe, Y.; Park, S.; Kameyama, N.; Hirai, S.; et al. Effects of a Japan Diet intake program on metabolic parameters in middle-aged men. J. Atheroscler. Thromb. 2017, 24, 393–401. [Google Scholar] [CrossRef] [Green Version]
- Maruyama, C.; Shijo, Y.; Kameyama, N.; Umezawa, A.; Sato, A.; Nishitani, A.; Ayaori, M.; Ikewaki, K.; Waki, M.; Teramoto, T. Effects of nutrition education program for the Japan Diet on serum LDL-cholesterol concentration in patients with dyslipidemia: A randomized controlled trial. J. Atheroscler. Thromb. 2021, 28, 1035–1051. [Google Scholar] [CrossRef]
- Chung, G.E.; Youn, J.; Kim, Y.S.; Lee, J.E.; Yang, S.Y.; Lim, J.H.; Song, J.H.; Doo, E.Y.; Kim, J.S. Dietary patterns are associated with the prevalence of nonalcoholic fatty liver disease in Korean adults. Nutrition 2019, 62, 32–38. [Google Scholar] [CrossRef]
- Howell, W.H.; McNamara, D.J.; Tosca, M.A.; Smith, B.T.; Gaines, J.A. Plasma lipid and lipoprotein responses to dietary fat and cholesterol: A meta-analysis. Am. J. Clin. Nutr. 1997, 65, 1747–1764. [Google Scholar] [CrossRef] [Green Version]
- Mozaffarian, D.; Appel, L.J.; van Horn, L. Components of a cardioprotective diet: New insights. Circulation 2011, 123, 2870–2891. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare. The National Health and Nutrition Survey in Japan. 2019. Available online: https://www.mhlw.go.jp/content/000710991.pdf (accessed on 11 May 2022).
- Narisada, A.; Shibata, E.; Hasegawa, T.; Masamura, N.; Taneda, C.; Suzuki, K. Sex differences in the association between fatty liver and type 2 diabetes incidence in non-obese Japanese: A retrospective cohort study. J. Diabetes Investig. 2021, 12, 1480–1489. [Google Scholar] [CrossRef]
| Parameters | All (n = 198) | Men (n = 96) | Women (n = 102) | p |
|---|---|---|---|---|
| Age (years) | 37 (28–44) | 34 (27–43) | 39 (30–46) | 0.006 |
| Height (cm) | 164.5 (158.5–172.0) | 172.0 (168.4–175.9) | 158.6 (155.5–163.1) | <0.001 |
| Weight (kg) | 57.5 (50.8–66.4) | 66.0 (60.6–73.0) | 51.7 (47.9–55.8) | <0.001 |
| Body mass index (kg/m2) | 21.2 (19.8–23.0) | 22.4 (20.8–24.1) | 20.6 (19.4–21.8) | <0.001 |
| Umbilical circumference (cm) | 77.1 (72.5–82.7) | 81.0 (74.9–85.0) | 75.0 (71.0–79.1) | <0.001 |
| SBP (mmHg) | 111 (103–123) | 121 (111–130) | 106 (99–112) | <0.001 |
| DBP (mmHg) | 70 (64–77) | 74 (67–84) | 67 (62–74) | <0.001 |
| Total cholesterol (mmol/L) † | 5.05 (0.83) | 5.02 (0.88) | 5.07 (0.78) | 0.690 |
| LDL-C (mmol/L) † | 2.86 (0.74) | 2.97 (0.75) | 2.77 (0.72) | 0.037 |
| HDL-C (mmol/L) | 1.68 (1.42–1.95) | 1.45 (1.27–1.68) | 1.86 (1.68–2.07) | <0.001 |
| Triglyceride (mmol/L) | 0.69 (0.51–1.05) | 0.89 (0.63–1.64) | 0.59 (0.46–0.77) | <0.001 |
| AST (U/L) | 20 (18–24) | 21 (18–26) | 19 (16–21) | <0.001 |
| ALT (U/L) | 16 (12–23) | 20 (16–28) | 14 (11–17) | <0.001 |
| ALP (U/L) | 173 (146–210) | 201 (167–234) | 156 (131–179) | <0.001 |
| γ-GT (U/L) | 19 (14–30) | 25 (18–38) | 15 (12–24) | <0.001 |
| LAP (U/L) | 49 (44–55) | 54 (49–61) | 45 (41–49) | <0.001 |
| Total bilirubin (μmol/L) | 12 (10–15) | 14 (10–15) | 11 (9–14) | 0.001 |
| Direct bilirubin (μmol/L) | 3 (3–5) | 5 (3–5) | 3 (3–3) | <0.001 |
| Indirect bilirubin (μmol/L) | 9 (7–10) | 9 (7–10) | 9 (7–10) | 0.038 |
| Fatty liver index | 6.6 (3.4–17.4) | 11.6 (6.1–31.2) | 3.9 (2.4–8.7) | <0.001 |
| Energy expenditure (kcal/day) | 2218 (1986–2598) | 2554 (2300–2973) | 1989 (1875–2183) | <0.001 |
| Food Groups | Traditional Japanese | Westernized |
|---|---|---|
| Unrefined cereals | 0.376 | −0.345 |
| Fish | 0.549 | −0.293 |
| Soybeans/soy products | 0.529 | −0.247 |
| Green and yellow vegetables | 0.787 | −0.200 |
| Other vegetables | 0.793 | −0.102 |
| Seaweed/mushrooms/konjac | 0.748 | 0.023 |
| Fruits | 0.603 | −0.067 |
| Dairy | 0.550 | 0.282 |
| Sweets | −0.024 | 0.484 |
| Saturated-fat-rich food | 0.207 | 0.774 |
| Eggs/fish-egg/liver | 0.382 | 0.440 |
| Oily | 0.094 | 0.545 |
| Salty | 0.548 | 0.293 |
| Variance explained (%) | 28.4 | 13.9 |
| Food Groups | Traditional Japanese | Westernized | ||||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | ptrend | T1 | T2 | T3 | ptrend | |
| Men/Women (n) | 41/25 | 32/34 | 23/43 | 0.007 # | 33/33 | 31/35 | 32/34 | 0.941 # |
| Cereals and potatoes | 6.60 (5.50–8.13) | 6.75 (5.50–8.25) | 6.65 (5.13–8.05) | 0.768 | 6.50 (4.83–8.05) | 6.90 (5.28–8.20) | 6.75 (5.65–8.00) | 0.412 |
| Fish | 0.10 (0.00–0.55) | 0.29 (0.00–0.76) | 0.47 (0.15–0.81) | 0.001 | 0.46 (0.00–0.74) | 0.39 (0.00–0.85) | 0.25 (0.00–0.69) | 0.233 |
| Seafoods | 0.13 (0.00–0.26) | 0.08 (0.00–0.27) | 0.16 (0.03–0.43) | 0.070 | 0.21 (0.01–0.45) | 0.09 (0.00–0.31) | 0.11 (0.00–0.24) | 0.075 |
| Soybean/soy products | 0.40 (0.18–1.13) | 0.50 (0.18–0.93) | 0.80 (0.30–1.40) | 0.006 | 0.55 (0.28–1.63) | 0.60 (0.28–1.13) | 0.40 (0.10–0.90) | 0.043 |
| Green and yellow vegetables | 0.70 (0.70–1.13) | 1.10 (0.70–1.63) | 1.50 (0.95–2.63) | <0.001 | 1.20 (0.60–2.23) | 1.20 (0.80–2.20) | 0.80 (0.40–1.40) | 0.001 |
| Other vegetables | 1.65 (1.30-2.43) | 1.90 (1.30–2.70) | 2.75 (2.10–3.50) | <0.001 | 2.30 (1.38–3.20) | 2.10 (1.45–2.90) | 2.00 (1.30–2.80) | 0.228 |
| Seaweed/mushroom/konjac | 0.20 (0.18–0.4) | 0.25 (0.18–0.50) | 0.40 (0.20–0.80) | 0.001 | 0.30 (0.10–0.70) | 0.30 (0.10–0.50) | 0.30 (0.10–0.40) | 0.392 |
| Fruit | 0.05 (0.00–0.4) | 0.40 (0.00–1.80) | 0.95 (0.30–1.83) | <0.001 | 0.60 (0.00–1.83) | 0.30 (0.00–1.10) | 0.30 (0.00–1.33) | 0.265 |
| Milk and dairy products | 0.40 (0.30–1.53) | 1.20 (0.30–2.95) | 1.75 (1.08–2.63) | <0.001 | 0.95 (0.10–2.33) | 1.25 (0.18–2.43) | 1.30 (0.40–2.50) | 0.127 |
| Sweets | 0.80 (0.28–1.43) | 0.70 (0.28–1.23) | 0.80 (0.30–1.23) | 0.907 | 0.75 (0.20–1.33) | 0.60 (0.10–1.03) | 0.90 (0.50–1.60) | 0.034 |
| Sugar and jam | 0.10 (0.10–0.20) | 0.10 (0.10–0.10) | 0.10 (0.10–0.20) | 0.129 | 0.10 (0.10–0.20) | 0.10 (0.00–0.10) | 0.10 (0.10–0.20) | 0.794 |
| Sweetened beverages | 0.95 (0.00–3.00) | 0.25 (0.00–2.15) | 0.00 (0.00–1.13) | 0.032 | 0.00 (0.00–1.90) | 0.00 (0.00–1.60) | 1.00 (0.00–2.98) | 0.063 |
| Meat/poultry | 1.41 (0.91–2.35) | 1.58 (0.91–2.22) | 1.41 (0.93–1.86) | 0.306 | 1.43 (0.82–1.93) | 1.59 (1.02–2.40) | 1.43 (0.97–2.05) | 0.350 |
| Meat products | 0.13 (0.00–0.35) | 0.06 (0.00–0.26) | 0.09 (0.00–0.33) | 0.398 | 0.03 (0.00–0.24) | 0.01 (0.03–0.22) | 0.22 (0.06–0.42) | <0.001 |
| Butter and margarine | 0.03 (0.00–0.08) | 0.03 (0.00–0.08) | 0.03 (0.00–0.06) | 0.329 | 0.02 (0.00–0.07) | 0.02 (0.00–0.07) | 0.04 (0.02–0.09) | 0.004 |
| Eggs/fish-egg/liver | 0.54 (0.30–0.78) | 0.56 (0.30–0.83) | 0.63 (0.42–1.02) | 0.011 | 0.49 (0.16–0.80) | 0.58 (0.26–0.75) | 0.68 (0.39–1.06) | 0.002 |
| Oily seasonings | 0.34 (0.19–0.43) | 0.37 (0.19–0.52) | 0.28 (0.16–0.46) | 0.583 | 0.28 (0.14–0.43) | 0.41 (0.22–0.52) | 0.34 (0.22–0.45) | 0.305 |
| Salty products | 0.08 (0.00–0.26) | 0.10 (0.00–0.31) | 0.19 (0.03–0.53) | 0.073 | 0.08 (0.00–0.39) | 0.12 (0.05–0.45) | 0.10 (0.01–0.32) | 0.841 |
| Non-oil seasonings | 0.57 (0.39–0.70) | 0.63 (0.39–0.86) | 0.65 (0.53–0.92) | 0.002 | 0.60 (0.41–0.85) | 0.64 (0.46–0.87) | 0.63 (0.47–0.74) | 0.963 |
| Nutrients | Traditional Japanese | Westernized | ||||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | ptrend | T1 | T2 | T3 | ptrend | |
| Men/Women (n) | 41/25 | 32/34 | 23/43 | 0.007 # | 33/33 | 31/35 | 32/34 | 0.941 # |
| Energy (kcal/IBW) | 30.2 (26.2–34.4) | 32.2 (27.2–36.5) | 32.8 (27.2–36.8) | 0.053 | 30.1 (26.5–33.6) | 31.6 (25.8–35.9) | 33.3 (28.8–37.9) | 0.008 |
| Carbohydrate (%energy) | 48.3 (44.6–53.0) | 48.8 (45.2–53.4) | 49.6 (45.2–53.2) | 0.374 | 49.4 (45.1–55.2) | 49.0 (45.3–53.0) | 48.4 (44.8–52.1) | 0.314 |
| Dietary fiber (g/1000 kcal) | 5.9 (4.7–6.5) | 6.6 (5.3–7.9) | 7.8 (5.3–9.6) | <0.001 | 7.5 (5.9–9.4) | 6.9 (5.7–8.5) | 6.0 (4.8–7.3) | <0.001 |
| Protein (%energy) | 14.1 (12.6–15.4) | 14.0 (12.5–15.5) | 15.5 (12.5–16.7) | <0.001 | 14.3 (13.2–16.1) | 15.2 (13.3–16.5) | 14.2 (12.6–15.4) | 0.154 |
| Fat (%energy) | 33.3 (29.2–36.7) | 32.9 (29.1–36.3) | 32.2 (29.1–34.6) | 0.243 | 31.4 (27.2–35.3) | 32.7 (29.1–35.9) | 33.7 (30.1–36.7) | 0.018 |
| Cholesterol (mg/IBW) | 4.9 (3.3–6.4) | 4.9 (3.6–6.6) | 5.7 (3.6–7.4) | 0.519 | 4.6 (3.6–5.9) | 5.0 (4.2–6.7) | 5.7 (4.3–7.2) | 0.002 |
| SFA (%energy) | 10.2 (8.5–11.3) | 9.8 (8.1–11.6) | 9.7 (8.1–10.8) | 0.075 | 9.4 (7.9–11.0) | 9.4 (8.0–11.0) | 10.2 (9.4–11.9) | 0.001 |
| MUFA (%energy) | 12.8 (11.2–14.1) | 12.5 (10.7–14.1) | 11.6 (10.7–13.4) | 0.445 | 11.4 (9.8–13.6) | 12.4 (10.9–13.9) | 13.0 (11.6–14.2) | 0.522 |
| PUFA (%energy) | 6.4 (5.6–7.5) | 6.5 (5.6–7.7) | 6.3 (5.6–6.9) | 0.004 | 6.2 (5.1–7.5) | 6.8 (5.9–8.0) | 6.1 (5.4–6.9) | 0.005 |
| n-6 PUFA (mg/IBW) | 185 (145–219) | 193 (152–231) | 184 (152–221) | 0.783 | 173 (128–221) | 195 (160–232) | 186 (154–222) | 0.157 |
| n-3 PUFA (mg/IBW) | 33 (22–46) | 33 (24–50) | 37 (24–52) | 0.036 | 35 (26–48) | 37 (24–52) | 33 (25–44) | 0.632 |
| EPA + DHA (mg/IBW) | 3 (1–9) | 5 (2–16) | 10 (2–17) | 0.001 | 7 (2–16) | 7 (2–16) | 4 (2–13) | 0.415 |
| β-carotene (μg/IBW) | 30 (19–53) | 46 (27–68) | 60 (27–87) | <0.001 | 57 (29–87) | 51 (28–73) | 40 (24–56) | 0.007 |
| α-tocopherol (mg/IBW) | 0.11 (0.09–0.12) | 0.12 (0.10–0.15) | 0.13 (0.10–0.16) | <0.001 | 0.11 (0.09–0.15) | 0.13 (0.10–0.15) | 0.11 (0.10–0.15) | 0.432 |
| Vitamin C (μg/IBW) | 1.07 (0.76–1.61) | 1.44 (0.96–2.01) | 1.62 (0.96–2.10) | <0.001 | 1.53 (0.99–2.04) | 1.34 (0.91–2.00) | 1.25 (0.85–1.82) | 0.172 |
| Vitamin D(mg/IBW) | 0.05 (0.03–0.09) | 0.08 (0.04–0.12) | 0.11 (0.04–0.17) | <0.001 | 0.08 (0.03–0.16) | 0.08 (0.03–0.13) | 0.07 (0.04–0.12) | 0.588 |
| Sodium (mg/IBW) | 54.7 (47.4–63.2) | 57.4 (46.9–68.9) | 57.6 (50.0–65.0) | 0.201 | 54.2 (43.7–63.1) | 55.9 (48.6–68.1) | 58.4 (52.4–66.5) | 0.043 |
| Potassium (mg/IBW) | 34.6 (28.5–46.3) | 40.7 (34.3–46.2) | 43.3 (36.5–50.1) | <0.001 | 39.1 (34.9–49.8) | 41.0 (33.4–49.0) | 38.1 (30.5–46.1) | 0.095 |
| Traditional Japanese | Westernized | |||||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | ptrend | T1 | T2 | T3 | ptrend | |
| Men/Women (n) | 41/25 | 32/34 | 23/43 | 0.007 # | 33/33 | 31/35 | 32/34 | 0.941 # |
| Height (cm) | 167 (153–182) | 166 (148–182) | 163 (152–179) | 0.013 | 165 (154–180) | 165 (148–181) | 166 (150–182) | 0.684 |
| Weight (kg) | 62.3 (45.2–87.0) | 60.3 (46.2–83.1) | 56.9 (45.3–78.3) | 0.002 | 59.4 (46.1–84) | 59.9 (44.8–84.4) | 60.2 (46.2–83.5) | 0.639 |
| Body mass index (kg/m2) | 21.8 (20.3–23.6) | 21.2 (19.7–23.7) | 20.6 (19.5–22.4) | 0.014 | 20.9 (19.8–22.4) | 21.5 (19.7–23.3) | 21.3 (20.3–23.6) | 0.466 |
| Umbilical circumference (cm) | 78.6 (74.0–85.7) | 78.4 (72.4–82.2) | 75.2 (71.9–82.1) | 0.053 | 76.4 (72.9–83) | 76.3 (71.0–82.6) | 78.2 (73.5–83.0) | 0.599 |
| SBP (mmHg) | 112 (105–123) | 112 (103–126) | 108 (102–121) | 0.100 | 109 (104–122) | 112 (102–125) | 112 (104–122) | 0.470 |
| DBP (mmHg) | 73 (64–77) | 70 (64–79) | 70 (63–76) | 0.224 | 69 (63–77) | 70 (64–77) | 72 (64–77) | 0.218 |
| Total cholesterol (mmol/L) † | 5.17 (0.77) | 4.94 (0.92) | 5.04 (0.79) | 0.249 | 5.01 (0.90) | 5.09 (0.90) | 5.05 (0.69) | 0.489 |
| LDL-C (mmol/L) † | 2.97 (0.71) | 2.80 (0.84) | 2.82 (0.67) | 0.225 | 2.86 (0.78) | 2.83 (0.82) | 2.89 (0.62) | 0.840 |
| HDL-C (mmol/L) | 1.62 (1.34–1.99) | 1.64 (1.29–1.93) | 1.72 (1.57–1.95) | 0.023 | 1.62 (1.29–1.93) | 1.72 (1.42–2.02) | 1.68 (1.47–1.89) | 0.314 |
| Triglyceride (mmol/L) | 0.78 (0.55–1.31) | 0.67 (0.52–1.00) | 0.67 (0.46–0.93) | 0.018 | 0.76 (0.53–1.03) | 0.68 (0.50–1.05) | 0.67 (0.50–1.06) | 0.518 |
| AST (U/L) | 19(17–25) | 20 (18–24) | 20 (18–23) | 0.817 | 19 (18–24) | 20 (18–23) | 19 (18–25) | 0.833 |
| ALT (U/L) | 16 (12–25) | 18 (14–24) | 15 (12–20) | 0.205 | 16 (12–23) | 16 (13–25) | 16 (12–22) | 0.661 |
| ALP (U/L) | 188 (156–224) | 175 (146–228) | 163 (140–200) | 0.031 | 172 (153–211) | 189 (135–225) | 168 (145–203) | 0.659 |
| γ-GT (U/L) | 23 (14–34) | 20 (15–33) | 18 (14–26) | 0.100 | 19 (14–31) | 22 (15–35) | 19 (14–30) | 0.958 |
| LAP (U/L) | 51 (45–58) | 49 (45–55) | 47 (42–54) | 0.019 | 48 (42–54) | 49 (45–56) | 50 (44–57) | 0.190 |
| Total bilirubin (μmol/L) | 14 (10–15) | 12 (9–15) | 12 (10–14) | 0.690 | 14 (10–15) | 10 (9–15) | 12 (10–14) | 0.470 |
| Direct bilirubin (μmol/L) | 3 (3–5) | 3 (3–5) | 3 (3–5) | 0.343 | 3 (3–5) | 3 (3–5) | 3 (3–5) | 0.232 |
| Indirect bilirubin (μmol/L) | 9 (7–10) | 8 (7–10) | 9 (7–10) | 0.922 | 9 (7–10) | 8 (7–10) | 9 (7–10) | 0.619 |
| Fatty liver index | 9.4 (4.6–23.4) | 6.8 (3.6–14.8) | 5.7 (2.9–11.4) | 0.003 | 6.6 (3.2–17.1) | 6.6 (3.4–18.8) | 6.7 (3.7–11.9) | 0.937 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uchiyama, M.; Maruyama, C.; Umezawa, A.; Kameyama, N.; Sato, A.; Kamoshita, K.; Komine, S.; Hasegawa, S. A Cross-Sectional Pilot Study on Food Intake Patterns Identified from Very Short FFQ and Metabolic Factors Including Liver Function in Healthy Japanese Adults. Nutrients 2022, 14, 2442. https://doi.org/10.3390/nu14122442
Uchiyama M, Maruyama C, Umezawa A, Kameyama N, Sato A, Kamoshita K, Komine S, Hasegawa S. A Cross-Sectional Pilot Study on Food Intake Patterns Identified from Very Short FFQ and Metabolic Factors Including Liver Function in Healthy Japanese Adults. Nutrients. 2022; 14(12):2442. https://doi.org/10.3390/nu14122442
Chicago/Turabian StyleUchiyama, Miya, Chizuko Maruyama, Ariko Umezawa, Noriko Kameyama, Aisa Sato, Kanako Kamoshita, Seina Komine, and Sayaka Hasegawa. 2022. "A Cross-Sectional Pilot Study on Food Intake Patterns Identified from Very Short FFQ and Metabolic Factors Including Liver Function in Healthy Japanese Adults" Nutrients 14, no. 12: 2442. https://doi.org/10.3390/nu14122442
APA StyleUchiyama, M., Maruyama, C., Umezawa, A., Kameyama, N., Sato, A., Kamoshita, K., Komine, S., & Hasegawa, S. (2022). A Cross-Sectional Pilot Study on Food Intake Patterns Identified from Very Short FFQ and Metabolic Factors Including Liver Function in Healthy Japanese Adults. Nutrients, 14(12), 2442. https://doi.org/10.3390/nu14122442






