Once-Weekly Semaglutide Induces an Early Improvement in Body Composition in Patients with Type 2 Diabetes: A 26-Week Prospective Real-Life Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Institution
2.2. Ethics
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Study Protocol
Study Outcomes
2.6. Study Participants
2.7. Statistical Analysis
3. Results
3.1. Descriptive Statistics
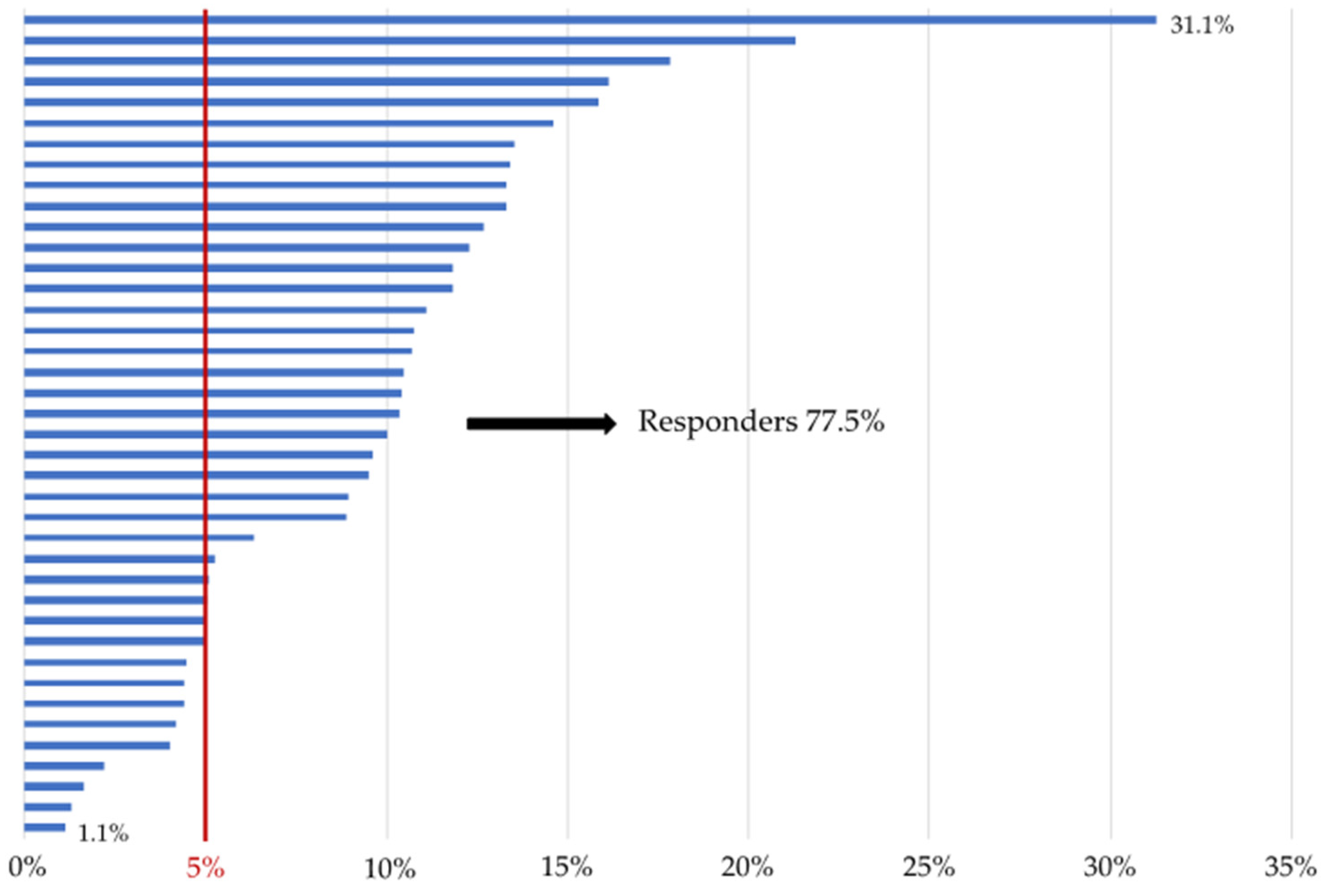
3.2. Body Weight and Composition
3.3. Glycemic Control
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Body Mass Index | BMI |
| Body Weight | BW |
| Cardiovascular | CV |
| Estimated Glomerular Filtration Rate | eGFR |
| Extracellular Water | ECW |
| Fasting Plasma Glucose | FPG |
| Fat-Free Mass | FFM |
| Fat-Free Mass Index | FFMI |
| Fat Mass Index | FMI |
| Glucagon-Like Peptide-1 Receptor Agonists | GLP-1RAs |
| Glycated Hemoglobin | HbA1c |
| Hand Grip | HG |
| Homeostasis Model Assessment for Insulin Resistance | HOMA-IR |
| Muscle Quality Index | MQI |
| Phase Angle | PhA |
| Segmental Multifrequency Bioelectrical Impedance Analysis | SMF-BIA |
| Skeletal Muscle Index | SMI |
| Skeletal Muscle Mass | SMM |
| Subcutaneous Adipose Tissue | SAT |
| Total Body Water | TBW |
| Type 2 Diabetes | T2D |
| Visceral Adipose Tissue | VAT |
| Waist Circumference | WC |
References
- Zheng, Y.; Ley, S.H.; Hu, F.B. Global Aetiology and Epidemiology of Type 2 Diabetes Mellitus and Its Complications. Nat. Rev. Endocrinol. 2018, 14, 88–98. [Google Scholar] [CrossRef] [PubMed]
- Scheen, A.J. Cardiovascular Outcome Studies in Type 2 Diabetes: Comparison between SGLT2 Inhibitors and GLP-1 Receptor Agonists. Diabetes Res. Clin. Pract. 2018, 143, 88–100. [Google Scholar] [CrossRef] [PubMed]
- Giugliano, D.; Scappaticcio, L.; Longo, M.; Caruso, P.; Maiorino, M.I.; Bellastella, G.; Ceriello, A.; Chiodini, P.; Esposito, K. GLP-1 Receptor Agonists and Cardiorenal Outcomes in Type 2 Diabetes: An Updated Meta-Analysis of Eight CVOTs. Cardiovasc. Diabetol. 2021, 20, 1–11. [Google Scholar] [CrossRef]
- Vilsbøll, T.; Christensen, M.; Junker, A.E.; Knop, F.K.; Gluud, L.L. Effects of Glucagon-like Peptide-1 Receptor Agonists on Weight Loss: Systematic Review and Meta-Analyses of Randomised Controlled Trials. BMJ 2012, 344, 7771. [Google Scholar] [CrossRef] [PubMed]
- Burhans, M.S.; Hagman, D.K.; Kuzma, J.N.; Schmidt, K.A.; Kratz, M. Contribution of Adipose Tissue Inflammation to the Development oftype 2 Diabetes Mellitus. Compr. Physiol. 2018, 9, 1. [Google Scholar] [CrossRef] [PubMed]
- Jorge-Galarza, E.; Medina-Urrutia, A.; Posadas-Sánchez, R.; Posadas-Romero, C.; Cardoso-Saldaña, G.; Vargas-Alarcón, G.; Caracas-Portilla, N.; González-Salazar, C.; Torres-Tamayo, M.; Juárez-Rojas, J.G. Adipose Tissue Dysfunction Increases Fatty Liver Association with Pre Diabetes and Newly Diagnosed Type 2 Diabetes Mellitus. Diabetol. Metab. Syndr. 2016, 8, 1–8. [Google Scholar] [CrossRef]
- Chait, A.; den Hartigh, L.J. Adipose Tissue Distribution, Inflammation and Its Metabolic Consequences, Including Diabetes and Cardiovascular Disease. Front. Cardiovasc. Med. 2020, 7, 22. [Google Scholar] [CrossRef]
- Kojta, I.; Chacińska, M.; Błachnio-Zabielska, A. Obesity, Bioactive Lipids, and Adipose Tissue Inflammation in Insulin Resistance. Nutrients 2020, 12, 1305. [Google Scholar] [CrossRef]
- Yang, J. Enhanced Skeletal Muscle for Effective Glucose Homeostasis. Prog. Mol. Biol. Transl. Sci. 2014, 121, 133–163. [Google Scholar] [CrossRef]
- Abdul-Ghani, M.A.; Defronzo, R.A. Pathogenesis of Insulin Resistance in Skeletal Muscle. J. Biomed. Biotechnol. 2010, 2010, 476279. [Google Scholar] [CrossRef]
- Nomura, T.; Kawae, T.; Kataoka, H.; Ikeda, Y. Assessment of Lower Extremity Muscle Mass, Muscle Strength, and Exercise Therapy in Elderly Patients with Diabetes Mellitus. Environ. Health Prev. Med. 2018, 23, 20. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Tan, Y.; Shi, Y.; Wang, X.; Liao, Z.; Wei, P. Diabetes and Sarcopenic Obesity: Pathogenesis, Diagnosis, and Treatments. Front. Endocrinol. 2020, 11, 568. [Google Scholar] [CrossRef] [PubMed]
- Rodbard, H.W.; Lingvay, I.; Reed, J.; De La Rosa, R.; Rose, L.; Sugimoto, D.; Araki, E.; Chu, P.L.; Wijayasinghe, N.; Norwood, P. Semaglutide Added to Basal Insulin in Type 2 Diabetes (SUSTAIN 5): A Randomized, Controlled Trial. J. Clin. Endocrinol. Metab. 2018, 103, 2291–2301. [Google Scholar] [CrossRef] [PubMed]
- Ahrén, B.; Atkin, S.L.; Charpentier, G.; Warren, M.L.; Wilding, J.P.H.; Birch, S.; Holst, A.G.; Leiter, L.A. Semaglutide Induces Weight Loss in Subjects with Type 2 Diabetes Regardless of Baseline BMI or Gastrointestinal Adverse Events in the SUSTAIN 1 to 5 Trials. Diabetes. Obes. Metab. 2018, 20, 2210. [Google Scholar] [CrossRef]
- Capehorn, M.S.; Catarig, A.M.; Furberg, J.K.; Janez, A.; Price, H.C.; Tadayon, S.; Vergès, B.; Marre, M. Efficacy and safety of once-weekly semaglutide 1.0mg vs once-daily liraglutide 1.2mg as add-on to 1-3 oral antidiabetic drugs in subjects with type 2 diabetes (SUSTAIN 10). Diabetes Metab. 2020, 46, 100–109. [Google Scholar] [CrossRef]
- Lingvay, I.; Hansen, T.; Macura, S.; Marre, M.; Nauck, M.A.; de la Rosa, R.; Woo, V.; Yildirim, E.; Wilding, J. Superior weight loss with once-weekly semaglutide versus other glucagon-like peptide-1 receptor agonists is independent of gastrointestinal adverse events. BMJ Open Diabetes Res Care 2020, 8, e001706. [Google Scholar] [CrossRef]
- Marso, S.P.; Bain, S.C.; Consoli, A.; Eliaschewitz, F.G.; Jódar, E.; Leiter, L.A.; Lingvay, I.; Rosenstock, J.; Seufert, J.; Warren, M.L.; et al. SUSTAIN-6 Investigators. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N. Engl. J. Med. 2016, 375, 1834–1844. [Google Scholar] [CrossRef]
- Issue Information-Declaration of Helsinki. J. Bone Miner. Res. 2022, 37, 4347. [CrossRef]
- Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes-2022. Diabetes Care 2022, 45 (Suppl. 1), S125–S143. [CrossRef]
- Bosy-Westphal, A.; Schautz, B.; Later, W.; Kehayias, J.J.; Gallagher, D.; Müller, M.J. What makes a BIA equation unique? Validity of eight-electrode multifrequency BIA to estimate body composition in a healthy adult population. Eur. J. Clin. Nutr. 2013, 67, S14–S21. [Google Scholar] [CrossRef]
- Mialich, S.M.; Faccioli Sicchieri, J.M.; Jordao, A.A. Analysis of body composition: Critical review of the use of bioelectrical impedance analysis. IJCN 2014, 2, 1–10. [Google Scholar] [CrossRef]
- Bosy-Westphal, A.; Jensen, B.; Braun, W.; Pourhassan, M.; Gallagher, D.; Müller, M.J. Quantification of whole-body and segmental skeletal muscle mass using phase-sensitive 8-electrode medical bioelectrical impedance devices. Eur. J. Clin. Nutr. 2017, 71, 1061–1067. [Google Scholar] [CrossRef] [PubMed]
- Roberts, H.C.; Denison, H.J.; Martin, H.J.; Patel, H.P.; Syddall, H.; Cooper, C.; Sayer, A.A. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardised approach. Age Ageing 2011, 40, 423–429. [Google Scholar] [CrossRef]
- Vlachos, I.S.; Hatziioannou, A.; Perelas, A.; Perrea, D.N. Sonographic assessment of regional adiposity. AJR Am. J. Roentgenol. 2007, 189, 1545–1553. [Google Scholar] [CrossRef]
- Wing, R.R.; Lang, W.; Wadden, T.A.; Safford, M.; Knowler, W.C.; Bertoni, A.G.; Hill, J.O.; Brancati, F.L.; Peters, A.; Wagenknecht, L.; et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 2011, 34, 1481–1486. [Google Scholar] [CrossRef]
- Walowski, C.O.; Braun, W.; Maisch, M.J.; Jensen, B.; Peine, S.; Norman, K.; Müller, M.J.; Bosy-Westphal, A. Reference Values for Skeletal Muscle Mass—Current Concepts and Methodological Considerations. Nutrients 2020, 12, 755. [Google Scholar] [CrossRef]
- Heymsfield, S.B.; Wadden, T.A. Mechanisms, Pathophysiology, and Management of Obesity. N. Engl. J. Med. 2017, 376, 1492. [Google Scholar] [CrossRef] [PubMed]
- Lazzaroni, E.; Ben Nasr, M.; Loretelli, C.; Pastore, I.; Plebani, L.; Lunati, M.E.; Vallone, L.; Bolla, A.M.; Rossi, A.; Montefusco, L.; et al. Anti-diabetic drugs and weight loss in patients with type 2 diabetes. Pharmacol. Res. 2021, 171, 105782. [Google Scholar] [CrossRef] [PubMed]
- Buchwald, H.; Buchwald, J.N. Metabolic (Bariatric and Nonbariatric) Surgery for Type 2 Diabetes: A Personal Perspective Review. Diabetes Care. 2019, 42, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Moriconi, E.; Camajani, E.; Fabbri, A.; Lenzi, A.; Caprio, M. Very-Low-Calorie Ketogenic Diet as a Safe and Valuable Tool for Long-Term Glycemic Management in Patients with Obesity and Type 2 Diabetes. Nutrients 2021, 13, 758. [Google Scholar] [CrossRef] [PubMed]
- Srikanthan, P.; Horwich, T.B.; Tseng, C.H. Relation of Muscle Mass and Fat Mass to Cardiovascular Disease Mortality. Am. J. Cardiol. 2016, 117, 1355–1360. [Google Scholar] [CrossRef] [PubMed]
- McCrimmon, R.J.; Catarig, A.M.; Frias, J.P.; Lausvig, N.L.; le Roux, C.W.; Thielke, D.; Lingvay, I. Effects of once-weekly semaglutide vs once-daily canagliflozin on body composition in type 2 diabetes: A substudy of the SUSTAIN 8 randomised controlled clinical trial. Diabetologia 2020, 63, 473–485. [Google Scholar] [CrossRef] [PubMed]
- Ida, S.; Kaneko, R.; Imataka, K.; Okubo, K.; Shirakura, Y.; Azuma, K.; Fujiwara, R.; Murata, K. Effects of Antidiabetic Drugs on Muscle Mass in Type 2 Diabetes Mellitus. Curr. Diabetes Rev. 2021, 17, 293–303. [Google Scholar] [CrossRef] [PubMed]
- Bosy-Westphal, A.; Braun, W.; Schautz, B.; Müller, M.J. Issues in characterizing resting energy expenditure in obesity and after weight loss. Front. Physiol. 2013, 4, 47. [Google Scholar] [CrossRef] [PubMed]


| Baseline Characteristics | Mean (s.d.) | Median (min; max) |
|---|---|---|
| Body mass index (kg/m2) | 38.8 (7.7) | 36.9 (28.1; 60.7) |
| Waist circumference (cm) | 123.4 (14.4) | 120 (101; 161) |
| Fasting glycemia (mg/dL) | 129.9 (36.6) | 121.5 (87; 221) |
| Glycated hemoglobin (mmol/mol) | 52.9 (21.6) | 44.5 (33; 128) |
| Serum creatinine (mg/dL) | 0.9 (0.2) | 0.85 (0.40; 1.65) |
| Glomerular filtration rate (mL/min/1.73 m2) | 87.8 (22.9) | 88 (41; 153) |
| Fasting serum insulin (mUI/L) | 22.6 (15.2) | 20.1 (3.8; 75) |
| Fasting serum C-peptide (ng/mL) | 3.7 (1.5) | 3.4 (1.3; 8.1) |
| HOMA-IR index | 6.9 (4.7) | 5.3 (1.6; 21.8) |
| Visceral adipose tissue (L) | 5.7 (2.9) | 5.1 (2.3; 14.9) |
| Fat mass index (kg/m2) | 17.1 (6.3) | 15.7 (6; 36.6) |
| Fat-free mass index (kg/m2) | 21.4 (3.1) | 21.7 (15.7; 29.8) |
| Skeletal muscle mass (kg) Skeletal muscle index (kg/m2) Hand grip (kg) MQI (kg/kg) | 28.2 (6.2) 10.4 (1.8) 32.5 (9.8) 1.1 (0.6) | 28.3 (15.9; 42.1) 10.7 (6.8; 15.10) 32 (15; 60) 1.1 (0.5; 3.15) |
| Total body water (L) | 42.9 (9.1) | 42.7 (24; 62.6) |
| Extracellular body water (L) | 19.4 (3.7) | 18.6 (12.7; 28) |
| Extracellular body water to total body water ratio | 45.6 (2.6) | 44.8 (40.9; 53) |
| Phase angle (°) | 5.8 (0.8) | 5.7 (3.9; 7.5) |
| US-VAT (cm) | 6.9 (2.4) | 6.5 (3; 13) |
| Parameters | Time | ||
|---|---|---|---|
| T0 | Variation at T3 | Variation at T6 | |
| Body weight (kg) | 103.96 ± 3.03 | −7.83 ± 0.72 ** | −9.89 ± 0.99 ** # |
| Body mass index (kg/m2) | 38.81 ± 1.18 | −3.05 ± 0.30 ** | −3.36 ± 0.42 ** |
| Waist circumference (cm) | 123.53 ± 2.24 | −6.32 ± 1.12 ** | −7.31 ± 1.15 ** |
| Fasting glycemia (mg/dL) | 129.95 ± 5.71 | −15.57 ± 4.41 ** | −23.56 ± 4.45 ** ## |
| HbA1c (mmol/mol) | 52.86 ± 3.36 | −10.72 ± 2.80 ** | −11.16 ± 2.99 ** |
| Serum creatinine (mg/dL) | 0.88 ± 0.04 | 0.03 ± 0.03 | 0.01 ± 0.03 |
| eGFR (mL/min/1.73 m2) | 87.85 ± 3.57 | 0.85 ± 2.55 | −2.02 ± 2.52 |
| Fasting serum insulin (mUI/L) | 22.59 ± 2.46 | −0.76 ± 3.17 | −5.22 ± 2.16 * |
| Fasting serum C-peptide (ng/mL) | 3.72 ± 0.24 | 0.08 ± 0.29 | −0.13 ± 0.27 |
| HOMA-IR index | 6.88 ± 0.77 | −1.22 ± 1.06 | −2.62 ± 0.79 ** |
| Visceral adipose tissue (L) | 5.74 ± 0.45 | −0.55 ± 0.27 * | −0.95 ± 0.24 * # |
| Fat mass index (kg/m2) | 17.10 ± 0.99 | −2.19 ± 0.46 ** | −3.04 ± 0.43 ** # |
| Fat-free mass index (kg/m2) | 21.45 ± 0.47 | −0.61 ± 0.24 * | −0.74 ± 0.17 ** |
| Skeletal muscle mass (kg) | 28.16 ± 0.98 | −1.31 ± 0.37 ** | −1.53 ± 0.36 ** |
| Skeletal muscle index (kg/m2) | 10.36 ± 0.27 | −0.52 ± 0.14 ** | −0.51 ± 0.14 ** |
| HG (kg) | 32.49 ± 1.64 | 0.49 ± 1.75 | 0.76 ± 1.26 |
| MQI (kg/kg) | 1.06 ± 0.09 | 0.16 ± 0.09 | 0.17 ± 0.08 |
| Total body water (L) | 42.95 ± 1.39 | −0.20 ± 0.79 | −0.87 ± 1.13 |
| Extracellular body water (L) | 19.45 ± 0.56 | −0.10 ± 0.32 | −0.41 ± 0.48 |
| ECW to TBW ratio | 45.6 ± 0.41 | −0.24 ± 0.36 | 0.00 ± 0.35 |
| Phase angle (°) | 5.76 ± 0.12 | −0.15 ± 0.10 | −0.21 ± 0.10 |
| US-VAT (cm) | 6.93 ± 0.39 | −1.45 ± 0.23 ** | −1.49 ± 0.33 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Volpe, S.; Lisco, G.; Racaniello, D.; Fanelli, M.; Colaianni, V.; Vozza, A.; Triggiani, V.; Sabbà, C.; Tortorella, C.; De Pergola, G.; et al. Once-Weekly Semaglutide Induces an Early Improvement in Body Composition in Patients with Type 2 Diabetes: A 26-Week Prospective Real-Life Study. Nutrients 2022, 14, 2414. https://doi.org/10.3390/nu14122414
Volpe S, Lisco G, Racaniello D, Fanelli M, Colaianni V, Vozza A, Triggiani V, Sabbà C, Tortorella C, De Pergola G, et al. Once-Weekly Semaglutide Induces an Early Improvement in Body Composition in Patients with Type 2 Diabetes: A 26-Week Prospective Real-Life Study. Nutrients. 2022; 14(12):2414. https://doi.org/10.3390/nu14122414
Chicago/Turabian StyleVolpe, Sara, Giuseppe Lisco, Davide Racaniello, Margherita Fanelli, Valentina Colaianni, Alfredo Vozza, Vincenzo Triggiani, Carlo Sabbà, Cosimo Tortorella, Giovanni De Pergola, and et al. 2022. "Once-Weekly Semaglutide Induces an Early Improvement in Body Composition in Patients with Type 2 Diabetes: A 26-Week Prospective Real-Life Study" Nutrients 14, no. 12: 2414. https://doi.org/10.3390/nu14122414
APA StyleVolpe, S., Lisco, G., Racaniello, D., Fanelli, M., Colaianni, V., Vozza, A., Triggiani, V., Sabbà, C., Tortorella, C., De Pergola, G., & Piazzolla, G. (2022). Once-Weekly Semaglutide Induces an Early Improvement in Body Composition in Patients with Type 2 Diabetes: A 26-Week Prospective Real-Life Study. Nutrients, 14(12), 2414. https://doi.org/10.3390/nu14122414










