The Effectiveness of Nutritional Education Interventions on Dietary Intake in Young Black Males: A Near-Empty Systematic Review
Abstract
:1. Introduction
Objectives
2. Methods
2.1. Population
2.2. Intervention
2.3. Comparisons/Control
2.4. Outcomes
2.5. Study Design
2.6. Keywords/Search Terms
2.7. Search Terms
3. Results
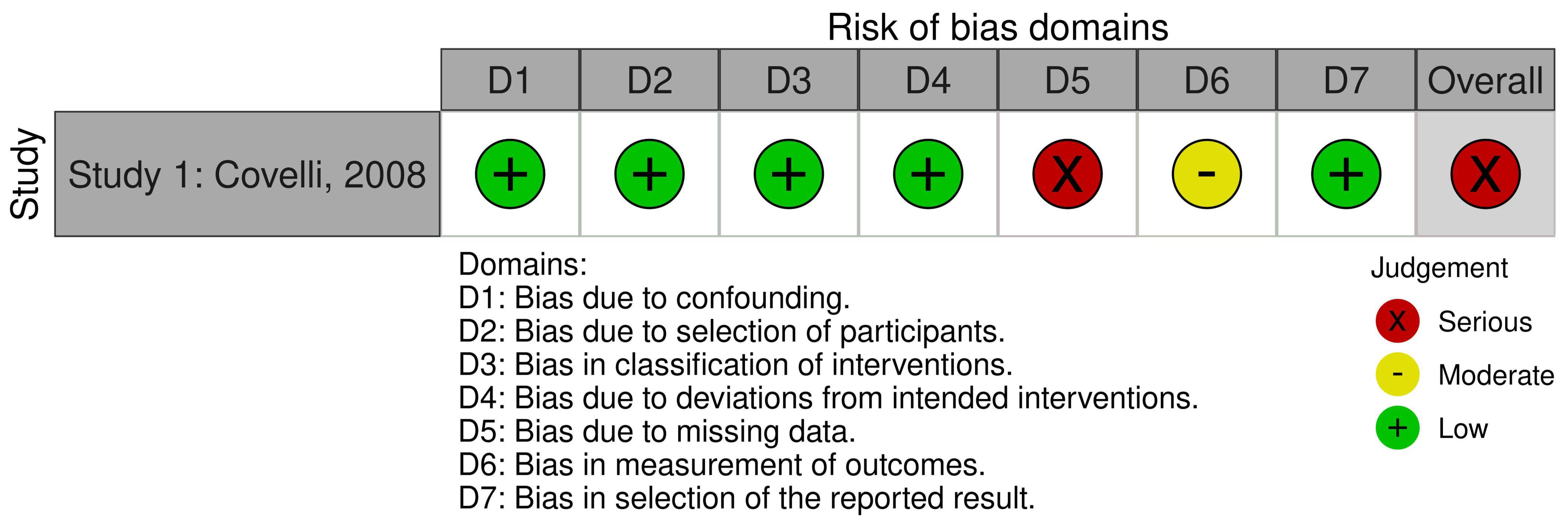
Risk of Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Fact Sheet 394: Healthy Diet; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Lascar, N.; Brown, J.; Pattison, H.; Barnett, A.H.; Bailey, C.J.; Bellary, S. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol. 2018, 6, 69–80. [Google Scholar] [CrossRef] [Green Version]
- Jackson, S.; Zhang, Z.; Wiltz, J.; Loustalot, F.; Ritchey, M.; Goodman, A.; Quanhe, Y. Hypertension Among Youths—United States, 2001–2016. MMWR Morb Mortal Wkly Rep. 2018, 67, 758–762. [Google Scholar] [CrossRef] [PubMed]
- Arispe, I.E.; Gindi, R.M.; Madans, J.H. Health, USA; CDC Centers for Disease Control and Prevention, National Center for Health Statistics: Atlanta, GA, USA, 2021. [Google Scholar] [CrossRef]
- CDC Centers for Disease Control and Prevention. CDC Vital Signs: African American Health: Creating Equal Opportunities for Health; CDC Centers for Disease Control and Prevention: Atlanta, GA, USA, 2017. [Google Scholar]
- NHS Digital. Health Survey for England 2004—Volume 1: The health of minority ethnic groups. Inf. Cent. 2006, 63–93, 205–236. [Google Scholar]
- Public Health Agency of Canada. Key Health Inequalities in Canada: A National Portrait; Public Health Agency of Canada: Nepean, ON, Canada, 2018. [Google Scholar]
- Wang, Y.; Rudd, G.A.; Wolfe, C.D. Age and ethnic disparities in incidence of stroke over time: The South London Stroke Register. Stroke 2013, 44, 3298–3304. [Google Scholar] [CrossRef] [Green Version]
- Commission on Race and Ethnic Disparities. Commission on Race and Ethnic Disparities: The Report: Health; Commission on Race and Ethnic Disparities: London, UK, 2021; Updated 28 April 2021. Available online: https://www.gov.uk/government/publications/the-report-of-the-commission-on-race-and-ethnic-disparities/health (accessed on 28 April 2022).
- Raleigh, V.; Holmes, J. The Health of People from Ethnic Minority Groups in England; The Kings Fund’s: London, UK, 2021. [Google Scholar]
- Morris, R.C.; Sebastian, A.; Forman, A.; Tanaka, M.; Schmidlin, O. Normotensive Salt Sensitivity. Hypertension 1999, 33, 18–23. [Google Scholar] [CrossRef] [Green Version]
- Svetkey, L.P.; Simons-Morton, D.; Vollmer, W.M.; Appel, L.J.; Conlin, P.R.; Ryan, D.H.; Ard, J.; Kennedy, B.M.; DASH Research Group. Effects of Dietary Patterns on Blood Pressure: Subgroup Analysis of the Dietary Approaches to Stop Hypertension (DASH) Randomized Clinical Trial. Arch. Intern. Med. 1999, 159, 285–293. [Google Scholar] [CrossRef] [Green Version]
- Viggiano, A.; Viggiano, E.; Di Costanzo, A.; Viggiano, A.; Andreozzi, E.; Romano, V.; Rianna, I.; Vicidomini, C.; Gargano, G.; Incarnato, L.; et al. Kaledo, a board game for nutrition education of children and adolescents at school: Cluster randomized controlled trial of healthy lifestyle promotion. Eur. J. Pediatrics 2015, 174, 217–228. [Google Scholar] [CrossRef]
- NICE. Behaviour Change: General Approaches; Public Health Guideline 6; NICE: London, UK, 2007; Available online: https://www.nice.org.uk/guidance/ph6 (accessed on 28 April 2022).
- McKinney, C.; Bishop, V.; Cabrera, K.; Medina, R.; Takawira, D.; Donate, N.; Rodriguez, J.L.; Guevara, B. NuFit: Nutrition and Fitness CBPR Program Evaluation community-based participatory research. J. Prev. Interv. Community 2014, 42, 112–124. [Google Scholar] [CrossRef]
- NICE. Behaviour Change: Individual Approaches; Public Health Guideline 49; NICE: London, UK, 2014; Available online: https://www.nice.org.uk/guidance/ph49 (accessed on 28 April 2022).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021); John Wiley & Sons: Hoboken, NJ, USA, 2021; Available online: www.training.cochrane.org/handbook (accessed on 28 April 2022).
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterne, J.A.C.; Higgins, J.P.T.; Elbers, R.G.; Reeves, B.C.; ROBINS-I Group. Risk Of Bias in Non-randomized Studies of Interventions (ROBINS-I): Detailed guidance. Updated 12 October 2016. Available online: http://www.riskofbias.info (accessed on 8 November 2021).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Covelli, M.M. Efficacy of a school-based cardiac health promotion intervention program for African-American adolescents. Appl. Nurs. Res. 2008, 21, 173–180. [Google Scholar] [CrossRef] [PubMed]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Michielutte, R.; Diseker, R.A. Racial differences in knowledge of cancer: A pilot study. Soc. Sci. Med. 1982, 16, 245–252. [Google Scholar] [CrossRef]
- Lefkowitz, B. Health Differentials Between White and Nonwhite Americans, Background Paper; Congress of the United States, Congressional Budget Office: Washington, DC, USA, 1977. [Google Scholar]
- Adams, J.M. Some racial differences in blood pressures and morbidity in a group of white and colored workmen. Am. J. Med. Sci. 1932, 184, 342–349. [Google Scholar] [CrossRef]
- Werch, C.E.C.; Bian, H.; Moore, M.J.; Ames, S.; DiClemente, C.C.; Weiler, R.M. Brief Multiple Behavior Interventions in a College Student Health Care Clinic. J. Adolesc. Health 2007, 41, 577–585. [Google Scholar] [CrossRef] [Green Version]
- Harmon, A.L.; Westerberg, A.L.; Bond, D.S.; Hoy, K.N.; Fries, E.A.; Danish, S.J. Cancer prevention among rural youth: Building a “Bridge“ to better health with genealogy. J. Cancer Educ. 2005, 20, 103–107. [Google Scholar] [CrossRef]
- Messiah, S.E.; D’Agostino, E.M.; Hansen, E.; Mathew, M.S.; Okeke, D.; Nardi, M.; Kardys, J.; Arheart, K.L. Longitudinal Impact of a Park-Based Afterschool Healthy Weight Program on Modifiable Cardiovascular Disease Risk Factors in Youth. J. Community Health 2018, 43, 103–116. [Google Scholar] [CrossRef]
- Hebden, L.; Cook, A.; van der Ploeg, H.P.; King, L.; Bauman, A.; Allman-Farinelli, M. A mobile health intervention for weight management among young adults: A pilot randomised controlled trial. J. Hum. Nutr. Diet. 2014, 27, 322–332. [Google Scholar] [CrossRef]
- Partridge, S.R.; McGeechan, K.; Bauman, A.; Phongsavan, P.; Allman-Farinelli, M. Improved eating behaviours mediate weight gain prevention of young adults: Moderation and mediation results of a randomised controlled trial of TXT2BFiT, mHealth program. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whatnall, M.C.; Patterson, A.J.; Chiu, S.; Oldmeadow, C.; Hutchesson, M.J. Feasibility and preliminary efficacy of the eating advice to students (EATS) brief web-based nutrition intervention for young adult university students: A pilot randomized controlled trial. Nutrients 2019, 11, 905. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuroko, S.; Black, K.; Chryssidis, T.; Finigan, R.; Hann, C.; Haszard, J.; Jackson, R.; Mahn, K.; Robinson, C.; Thomson, C.; et al. Create our own kai: A randomised control trial of a cooking intervention with group interview insights into adolescent cooking behaviours. Nutrients 2020, 12, 796. [Google Scholar] [CrossRef] [Green Version]
- Do, M.; Kattelmann, K.; Boeckner, L.; Greene, G.; White, A.; Hoerr, S.; Horacek, T.; Lohse, B.; Phillips, B.; Nitzke, S. Low-income young adults report increased variety in fruit and vegetable intake after a stage-tailored intervention. Nutr. Res. 2008, 28, 517–522. [Google Scholar] [CrossRef] [PubMed]
- Geria, K.; Beitz, J.M. Application of a modified diabetes prevention program with adolescents. Public Health Nurs. 2018, 35, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Whittemore, R.; Jeon, S.; Grey, M. An internet obesity prevention program for adolescents. J. Adolesc. Health 2013, 52, 439–447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nicklas, T.A.; Johnson, C.C.; Myers, L.; Farris, R.P.; Cunningham, A. Outcomes of a high school program to increase fruit and vegetable consumption: Gimme 5—A Fresh Nutrition Concept for Students. J. Sch. Health 1998, 68, 248–253. [Google Scholar] [CrossRef]
- Greene, G.W.; White, A.A.; Hoerr, S.L.; Lohse, B.; Schembre, S.M.; Riebe, D.; Patterson, J.; Kattelmann, K.K.; Shoff, S.; Horacek, T.; et al. Impact of an online healthful eating and physical activity program for college students. Am. J. Health Promot. 2012, 27, e47–e58. [Google Scholar] [CrossRef]
- Mauriello, L.M.; Ciavatta, M.M.H.; Paiva, A.L.; Sherman, K.J.; Castle, P.H.; Johnson, J.L.; Prochaska, J.M. Results of a multi-media multiple behavior obesity prevention program for adolescents. Prev. Med. 2010, 51, 451–456. [Google Scholar] [CrossRef] [Green Version]
- Werch, C.E.; Moore, M.J.; Bian, H.; Di Clemente, C.C.; Ames, S.C.; Weiler, R.M.; Thombs, D.; Pokorny, S.B.; Huang, I.-C. Efficacy of a brief image-based multiple-behavior intervention for college students. Ann. Behav. Med. 2008, 36, 149–157. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.-M.; Li, S.; Newland, A.; Leedeman, J.; Clifford, D.E.; Keeler, L.A. A peer-led non-diet behaviour change intervention: FitU. Health Educ. J. 2021, 80, 67–80. [Google Scholar] [CrossRef]
- Park, A.; Nitzke, S.; Kritsch, K.; Kattelmann, K.; White, A.; Boeckner, L.; Lohse, B.; Hoerr, S.; Greene, G.; Zhang, Z. Internet-based Interventions Have Potential to Affect Short-term Mediators and Indicators of Dietary Behavior of Young Adults. J. Nutr. Educ. Behav. 2008, 40, 288–297. [Google Scholar] [CrossRef] [PubMed]
- Richards, A.; Kattelmann, K.K.; Ren, C. Motivating 18- to 24-Year-Olds to Increase Their Fruit and Vegetable Consumption. J. Am. Diet. Assoc. 2006, 106, 1405–1411. [Google Scholar] [CrossRef]
- Pierce, B.; Bowden, B.; McCullagh, M.; Diehl, A.; Chissell, Z.; Rodriguez, R.; Berman, B.M.; D’Adamo, C.R.; D Adamo, C.R. A Summer Health Program for African-American High School Students in Baltimore, Maryland: Community Partnership for Integrative Health. Explor. J. Sci. Health 2017, 13, 186–197. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.K.; Bernhardt, J.M.; Waldmiller, M.; Jackson, B.; Potenziani, D.; Weathers, B.; Demissie, S. Varying the message source in computer-tailored nutrition education. Patient Educ. Couns. 1999, 36, 157–169. [Google Scholar] [CrossRef]
- Heo, M.; Jimenez, C.C.; Lim, J.; Isasi, C.R.; Blank, A.E.; Lounsbury, D.W.; Fredericks, L.; Bouchard, M.; Faith, M.S.; Wylie, J. Effective nationwide school-based participatory extramural program on adolescent body mass index, health knowledge and behaviors. BMC Pediatr. 2018, 18, 7. [Google Scholar] [CrossRef] [Green Version]
- Krebs, P.; Prochaska, J.O.; Rossi, J.S. A meta-analysis of computer-tailored interventions for health behavior change. Prev. Med. 2010, 51, 214–221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Resnicow, K.; Jackson, A.; Blissett, D.; Wang, T.; McCarty, F.; Rahotep, S.; Periasamy, S. Results of the healthy body healthy spirit trial. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2005, 24, 339–348. [Google Scholar] [CrossRef]
- Kerr, D.A.; Harray, A.J.; Pollard, C.M.; Dhaliwal, S.S.; Delp, E.J.; Howat, P.A.; Pickering, M.R.; Ahmad, Z.; Meng, X.; Pratt, I.S.; et al. The connecting health and technology study: A 6-month randomized controlled trial to improve nutrition behaviours using a mobile food record and text messaging support in young adults. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 52. [Google Scholar] [CrossRef] [Green Version]
- De Bourdeaudhuij, I.; Brug, J. Tailoring dietary feedback to reduce fat intake: An intervention at the family level. Health Educ. Res. 2000, 15, 449–462. [Google Scholar] [CrossRef] [Green Version]
- De Bourdeaudhuij, I.; Brug, J.; Vandelanotte, C.; Van Oost, P. Differences in impact between a family- versus an individual-based tailored intervention to reduce fat intake. Health Educ. Res. 2002, 17, 435–449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Candari, C.J.; Cylus, J.; Nolte, E. Assessing the Economic Costs of Unhealthy Diets and Low Physical Activity: An Evidence Review and Proposed Framework; WWHO Regional Office for Europe: Copenhagen, Denmark, 2017. [Google Scholar]

| Population | Interventions | NOT |
|---|---|---|
| Young people Young persons Adolescent * Teenage * Youth * Juvenile * Black * African American * Afr *-Caribbean * BAME Male Men Boy * | Nutrition * Diet Food * Intervention * Education * Medical Nutrition * Therap * | Supplement * Infusion * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jones, H.E.; Haskell-Ramsay, C.F.; Briggs, M.A.; Young, J. The Effectiveness of Nutritional Education Interventions on Dietary Intake in Young Black Males: A Near-Empty Systematic Review. Nutrients 2022, 14, 2264. https://doi.org/10.3390/nu14112264
Jones HE, Haskell-Ramsay CF, Briggs MA, Young J. The Effectiveness of Nutritional Education Interventions on Dietary Intake in Young Black Males: A Near-Empty Systematic Review. Nutrients. 2022; 14(11):2264. https://doi.org/10.3390/nu14112264
Chicago/Turabian StyleJones, Hannah E., Crystal F. Haskell-Ramsay, Marc A. Briggs, and Julie Young. 2022. "The Effectiveness of Nutritional Education Interventions on Dietary Intake in Young Black Males: A Near-Empty Systematic Review" Nutrients 14, no. 11: 2264. https://doi.org/10.3390/nu14112264
APA StyleJones, H. E., Haskell-Ramsay, C. F., Briggs, M. A., & Young, J. (2022). The Effectiveness of Nutritional Education Interventions on Dietary Intake in Young Black Males: A Near-Empty Systematic Review. Nutrients, 14(11), 2264. https://doi.org/10.3390/nu14112264






