Hyperuricemia and Its Association with Osteoporosis in a Large Asian Cohort
Abstract
1. Introduction
2. Materials and Methods
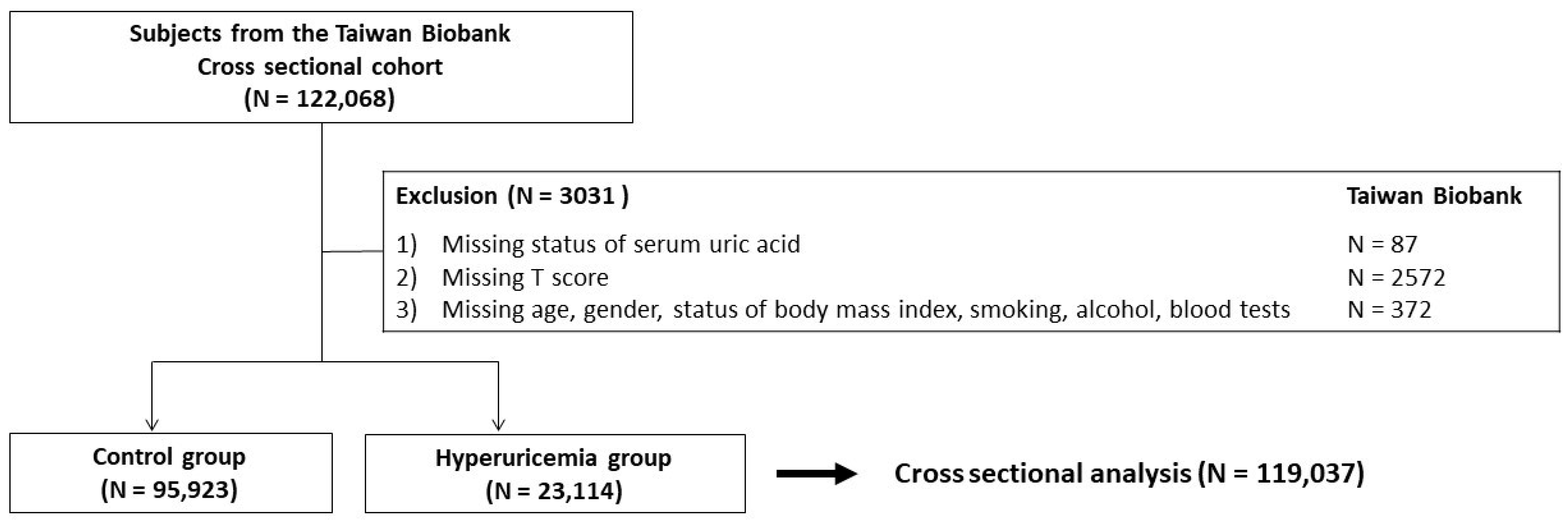
2.1. Subjects
2.2. Ethics Statement
2.3. Definition of Hyperuricemia
2.4. Definition of Osteoporosis
2.5. Covariates
2.6. Statistical Analyses
3. Results
3.1. Comparison of the Baseline Clinical Profiles among the Participants According to the Presence of Hyperuricemia
3.2. Association between the Presence of Hyperuricemia and Osteoporosis
3.3. Association between the Presence of Hyperuricemia and Osteoporosis in participants Stratified by Age and Sex
3.4. Dose–Response Effect between Serum Uric Acid and the Risk of Osteoporosis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sozen, T.; Ozisik, L.; Basaran, N.C. An overview and management of osteoporosis. Eur. J. Rheumatol. 2017, 4, 46–56. [Google Scholar] [CrossRef]
- Kanis, J.A. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: Synopsis of a WHO report. WHO Study Group. Osteoporos. Int. 1994, 4, 368–381. [Google Scholar] [CrossRef]
- Chie, W.C.; Yang, R.S.; Liu, J.P.; Tsai, K.S. High incidence rate of hip fracture in Taiwan: Estimated from a nationwide health insurance database. Osteoporos. Int. 2004, 15, 998–1002. [Google Scholar] [CrossRef]
- Wu, T.Y.; Hu, H.Y.; Lin, S.Y.; Chie, W.C.; Yang, R.S.; Liaw, C.K. Trends in hip fracture rates in Taiwan: A nationwide study from 1996 to 2010. Osteoporos. Int. 2017, 28, 653–665. [Google Scholar] [CrossRef]
- Chilibeck, P.D.; Sale, D.G.; Webber, C.E. Exercise and bone mineral density. Sports Med. 1995, 19, 103–122. [Google Scholar] [CrossRef]
- Palacios, C. The role of nutrients in bone health, from A to Z. Crit. Rev. Food Sci. Nutr. 2006, 46, 621–628. [Google Scholar] [CrossRef]
- Agidigbi, T.S.; Kim, C. Reactive Oxygen Species in Osteoclast Differentiation and Possible Pharmaceutical Targets of ROS-Mediated Osteoclast Diseases. Int. J. Mol. Sci. 2019, 20, 3576. [Google Scholar] [CrossRef]
- Domazetovic, V.; Marcucci, G.; Iantomasi, T.; Brandi, M.L.; Vincenzini, M.T. Oxidative stress in bone remodeling: Role of antioxidants. Clin. Cases Miner Bone Metab. 2017, 14, 209–216. [Google Scholar] [CrossRef]
- Maggio, D.; Barabani, M.; Pierandrei, M.; Polidori, M.C.; Catani, M.; Mecocci, P.; Senin, U.; Pacifici, R.; Cherubini, A. Marked decrease in plasma antioxidants in aged osteoporotic women: Results of a cross-sectional study. J. Clin. Endocrinol. Metab. 2003, 88, 1523–1527. [Google Scholar] [CrossRef]
- George, C.; Minter, D.A. Hyperuricemia; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2022. [Google Scholar]
- Benn, C.L.; Dua, P.; Gurrell, R.; Loudon, P.; Pike, A.; Storer, R.I.; Vangjeli, C. Physiology of Hyperuricemia and Urate-Lowering Treatments. Front. Med. 2018, 5, 160. [Google Scholar] [CrossRef]
- Chou, C.T.; Lai, J.S. The epidemiology of hyperuricaemia and gout in Taiwan aborigines. Br. J. Rheumatol. 1998, 37, 258–262. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Si, K.; Wei, C.; Xu, L.; Zhou, Y.; Lv, W.; Dong, B.; Wang, Z.; Huang, Y.; Wang, Y.; Chen, Y. Hyperuricemia and the Risk of Heart Failure: Pathophysiology and Therapeutic Implications. Front. Endocrinol. 2021, 12, 770815. [Google Scholar] [CrossRef] [PubMed]
- Holme, I.; Aastveit, A.H.; Hammar, N.; Jungner, I.; Walldius, G. Uric acid and risk of myocardial infarction, stroke and congestive heart failure in 417,734 men and women in the Apolipoprotein MOrtality RISk study (AMORIS). J. Intern. Med. 2009, 266, 558–570. [Google Scholar] [CrossRef]
- Oda, E.; Kawai, R.; Sukumaran, V.; Watanabe, K. Uric acid is positively associated with metabolic syndrome but negatively associated with diabetes in Japanese men. Intern. Med. 2009, 48, 1785–1791. [Google Scholar] [CrossRef]
- Yao, X.; Chen, L.; Xu, H.; Zhu, Z. The Association between Serum Uric Acid and Bone Mineral Density in Older Adults. Int. J. Endocrinol. 2020, 2020, 3082318. [Google Scholar] [CrossRef] [PubMed]
- Yan, D.D.; Wang, J.; Hou, X.H.; Bao, Y.Q.; Zhang, Z.L.; Hu, C.; Jia, W.P. Association of serum uric acid levels with osteoporosis and bone turnover markers in a Chinese population. Acta Pharmacol. Sin. 2018, 39, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Carraro, S.; Bano, G.; Trevisan, C.; Solmi, M.; Luchini, C.; Manzato, E.; Caccialanza, R.; Sergi, G.; Nicetto, D.; et al. Hyperuricemia protects against low bone mineral density, osteoporosis and fractures: A systematic review and meta-analysis. Eur. J. Clin. Investig. 2016, 46, 920–930. [Google Scholar] [CrossRef]
- Glantzounis, G.K.; Tsimoyiannis, E.C.; Kappas, A.M.; Galaris, D.A. Uric acid and oxidative stress. Curr. Pharm. Des. 2005, 11, 4145–4151. [Google Scholar] [CrossRef]
- Waring, W.S.; Webb, D.J.; Maxwell, S.R. Systemic uric acid administration increases serum antioxidant capacity in healthy volunteers. J. Cardiovasc. Pharmacol. 2001, 38, 365–371. [Google Scholar] [CrossRef]
- Lee, M.R.; Ke, H.L.; Huang, J.C.; Huang, S.P.; Geng, J.H. Obesity-related indices and its association with kidney stone disease: A cross-sectional and longitudinal cohort study. Urolithiasis 2022, 50, 55–63. [Google Scholar] [CrossRef]
- Lu, Y.H.; Geng, J.H.; Wu, D.W.; Chen, S.C.; Hung, C.H.; Kuo, C.H. Betel Nut Chewing Decreased Calcaneus Ultrasound T-Score in a Large Taiwanese Population Follow-Up Study. Nutrients 2021, 13, 3655. [Google Scholar] [CrossRef]
- Gonnelli, S.; Cepollaro, C.; Gennari, L.; Montagnani, A.; Caffarelli, C.; Merlotti, D.; Rossi, S.; Cadirni, A.; Nuti, R. Quantitative ultrasound and dual-energy X-ray absorptiometry in the prediction of fragility fracture in men. Osteoporos. Int. 2005, 16, 963–968. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, C.H. Osteoporosis screening and risk management. Clin. Interv. Aging 2007, 2, 389–394. [Google Scholar] [PubMed]
- Raja, S.; Kumar, A.; Aahooja, R.D.; Thakuria, U.; Ochani, S.; Shaukat, F. Frequency of Hyperuricemia and its Risk Factors in the Adult Population. Cureus 2019, 11, e4198. [Google Scholar] [CrossRef]
- Qiu, L.; Cheng, X.-Q.; Wu, J.; Liu, J.-t.; Xu, T.; Ding, H.-T.; Liu, Y.-H.; Ge, Z.-M.; Wang, Y.-J.; Han, H.-J.; et al. Prevalence of hyperuricemia and its related risk factors in healthy adults from Northern and Northeastern Chinese provinces. BMC Public Health 2013, 13, 664. [Google Scholar] [CrossRef] [PubMed]
- Ye, Z.; Lu, H.; Liu, P. Association between essential hypertension and bone mineral density: A systematic review and meta-analysis. Oncotarget 2017, 8, 68916–68927. [Google Scholar] [CrossRef] [PubMed]
- Kan, B.; Zhao, Q.; Wang, L.; Xue, S.; Cai, H.; Yang, S. Association between lipid biomarkers and osteoporosis: A cross-sectional study. BMC Musculoskelet. Disord. 2021, 22, 759. [Google Scholar] [CrossRef]
- DAGitty—Draw and Analyze Causal Diagrams. Available online: http://www.dagitty.net/ (accessed on 19 May 2022).
- Textor, J.; van der Zander, B.; Gilthorpe, M.S.; Liskiewicz, M.; Ellison, G.T. Robust causal inference using directed acyclic graphs: The R package ‘dagitty’. Int. J. Epidemiol. 2016, 45, 1887–1894. [Google Scholar] [CrossRef]
- Nabipour, I.; Sambrook, P.N.; Blyth, F.M.; Janu, M.R.; Waite, L.M.; Naganathan, V.; Handelsman, D.J.; Le Couteur, D.G.; Cumming, R.G.; Seibel, M.J. Serum uric acid is associated with bone health in older men: A cross-sectional population-based study. J. Bone Miner Res. 2011, 26, 955–964. [Google Scholar] [CrossRef]
- Lane, N.E.; Parimi, N.; Lui, L.Y.; Wise, B.L.; Yao, W.; Lay, Y.A.; Cawthon, P.M.; Orwoll, E.; Osteoporotic Fractures in Men Study, G. Association of serum uric acid and incident nonspine fractures in elderly men: The Osteoporotic Fractures in Men (MrOS) study. J. Bone Miner Res. 2014, 29, 1701–1707. [Google Scholar] [CrossRef]
- Bauer, D.C.; Gluer, C.C.; Cauley, J.A.; Vogt, T.M.; Ensrud, K.E.; Genant, H.K.; Black, D.M. Broadband ultrasound attenuation predicts fractures strongly and independently of densitometry in older women. A prospective study. Study of Osteoporotic Fractures Research Group. Arch. Intern. Med. 1997, 157, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Bauer, D.C.; Ewing, S.K.; Cauley, J.A.; Ensrud, K.E.; Cummings, S.R.; Orwoll, E.S.; Osteoporotic Fractures in Men Research, G. Quantitative ultrasound predicts hip and non-spine fracture in men: The MrOS study. Osteoporos. Int. 2007, 18, 771–777. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total (N = 119,037) | Control Group (N = 95,923) | Hyperuricemia Group (N = 23,114) | p-Value |
|---|---|---|---|---|
| Demographic data | ||||
| Age, years old | 50 ± 11 | 50 ± 11 | 51 ± 11 | <0.001 |
| Female, N (%) | 76,313 (64) | 65,939 (69) | 10,374 (45) | <0.001 |
| Body mass index, kg/m2 | 24.2 ± 3.8 | 23.7 ± 3.5 | 26.5 ± 3.9 | <0.001 |
| Smoked, ever, N (%) | 10,139 (9) | 23,738 (25) | 8700 (38) | <0.001 |
| Alcohol status, ever, N (%) | 715 (2) | 6922 (7) | 3217 (14) | <0.001 |
| Regular physical activity, yes, N (%) | 48,351 (41) | 38,680 (40) | 9671 (42) | <0.001 |
| Presence of menopause, yes, N (%) * | 34,985 (46) * | 28,626 (43) * | 6359 (61) * | <0.001 |
| Systolic blood pressure, mmHg | 121 ± 19 | 119 ± 18 | 127 ± 18 | <0.001 |
| Diastolic blood pressure, mmHg | 74 ± 11 | 73 ± 11 | 78 ± 11 | <0.001 |
| Comorbidities | ||||
| Hypertension, N (%) | 14,596 (12) | 9759 (10) | 4837 (21) | <0.001 |
| Diabetes mellitus, N (%) | 6128 (5) | 4664 (5) | 1464 (6) | <0.001 |
| Dyslipidemia, N (%) | 8880 (8) | 6376 (7) | 2504 (11) | <0.001 |
| Gout, N (%) | 4558 (4) | 1663 (2) | 2895 (13) | <0.001 |
| Laboratory data | ||||
| Albumin, g/dL | 4.5 ± 0.2 | 4.5 ± 0.2 | 4.6 ± 0.2 | <0.001 |
| Fasting glucose, mg/dL | 96 ± 21 | 95 ± 21 | 98 ± 19 | <0.001 |
| Total cholesterol, mg/dL | 196 ± 36 | 194 ± 35 | 202 ± 37 | <0.001 |
| Triglyceride, mg/dL | 116 ± 94 | 105 ± 81 | 158 ± 127 | <0.001 |
| High-density lipoprotein cholesterol, mg/dL | 55 ± 13 | 56 ± 13 | 48 ± 12 | <0.001 |
| Low-density lipoprotein cholesterol, mg/dL | 121 ± 32 | 119 ± 31 | 128 ± 33 | <0.001 |
| Creatinine, mg/dL | 0.7 ± 0.3 | 0.7 ± 0.3 | 0.9 ± 0.4 | <0.001 |
| T score | −0.387 ± 1.627 | −0.369 ± 1.640 | −0.460 ± 1.570 | <0.001 |
| Osteoporosis, N (%) | 10,114 (9) | 8243 (9) | 1871 (8) | 0.015 |
| Parameters | Odds Ratio (95% CI) | p-Value |
|---|---|---|
| Age (per 1 year) | 1.078 (1.076 to 1.081) | <0.001 |
| Gender, female (vs. male) | 0.783 (0.751 to 0.816) | <0.001 |
| Body mass index (per 1 kg/m2) | 0.952 (0.946 to 0.957) | <0.001 |
| Smoking status, ever (vs. never) | 1.161 (1.110 to 1.214) | <0.001 |
| Alcohol status, ever (vs. never) | 1.195 (1.116 to 1.280) | <0.001 |
| Regular physical activity, yes (vs. no) | 1.298 (1.246 to 1.352) | <0.001 |
| Presence of menopause, yes (vs. no) | 0.937 (0.889 to 0.987) | 0.015 |
| Systolic blood pressure (per 1 mmHg) | 1.013 (1.012 to 1.014) | <0.001 |
| Diastolic blood pressure (per 1 mmHg) | 1.007 (1.006 to 1.009) | <0.001 |
| Hypertension, yes (vs. no) | 1.538 (1.456 to 1.625) | <0.001 |
| Diabetes mellitus, yes (vs. no) | 1.435 (1.323 to 1.556) | <0.001 |
| Dyslipidemia, yes (vs. no) | 1.439 (1.343 to 1.541) | <0.001 |
| Gout, yes (vs. no) | 1.145 (1.035 to 1.267) | 0.008 |
| Albumin (per 1 g/dL) | 0.649 (0.595 to 0.708) | <0.001 |
| Fasting glucose (per 1 g/dL) | 1.005 (1.004 to 1.006) | <0.001 |
| Total cholesterol (per 1 mg/dL) | 1.003 (1.002 to 1.003) | <0.001 |
| Triglyceride (per 1 mg/dL) | 1.000 (1.000 to 1.001) | <0.001 |
| High-density lipoprotein cholesterol (per 1 mg/dL) | 1.002 (1.001 to 1.004) | 0.006 |
| Low-density lipoprotein cholesterol (per 1 mg/dL) | 1.002 (1.001 to 1.002) | <0.001 |
| Creatinine, mg/dL | 1.236 (1.181 to 1.293) | <0.001 |
| Hyperuricemia, yes (vs. control) | 0.937 (0.889 to 0.987) | 0.015 |
| Parameters | Odds Ratio (95% CI) | p-Value |
|---|---|---|
| Age (per 1 year) | 1.067 (1.064 to 1.070) | <0.001 |
| Gender, female (vs. male) | 0.409 (0.376 to 0.444) | <0.001 |
| Body mass index (per 1 kg/m2) | 0.921 (0.915 to 0.928) | <0.001 |
| Smoking status, ever (vs. never) | 1.150 (1.085 to 1.218) | <0.001 |
| Alcohol status, ever (vs. never) | 1.029 (0.953 to 1.111) | 0.465 |
| Regular physical activity, yes (vs. no) | 0.726 (0.694 to 0.759) | <0.001 |
| Presence of menopause, yes (vs. no) | 2.375 (2.202 to 2.561) | <0.001 |
| Systolic blood pressure (per 1 mmHg) | 1.002 (1.000 to 1.004) | 0.027 |
| Diastolic blood pressure (per 1 mmHg) | 0.999 (0.996 to 1.001) | 0.330 |
| Hypertension, yes (vs. no) | 1.024 (0.962 to 1.091) | 0.453 |
| Diabetes mellitus, yes (vs. no) | 0.912 (0.828 to 1.006) | 0.065 |
| Dyslipidemia, yes (vs. no) | 0.957 (0.889 to 1.031) | 0.247 |
| Gout, yes (vs. no) | 0.950 (0.852 to 1.060) | 0.359 |
| Albumin (per 1 g/dL) | 0.850 (0.771 to 0.937) | 0.001 |
| Fasting glucose (per 1 g/dL) | 1.000 (0.999 to 1.001) | 0.481 |
| Total cholesterol (per 1 mg/dL) | 0.998 (0.996 to 1.000) | 0.091 |
| Triglyceride (per 1 mg/dL) | 1.001 (1.000 to 1.001) | <0.001 |
| High-density lipoprotein cholesterol (per 1 mg/dL) | 1.003 (1.000 to 1.006) | 0.072 |
| Low-density lipoprotein cholesterol (per 1 mg/dL) | 1.002 (0.999 to 1.004) | 0.194 |
| Creatinine, mg/dL | 1.061 (0.999 to 1.127) | 0.054 |
| Hyperuricemia, yes (vs. control) | 0.916 (0.864 to 0.970) | 0.003 |
| Characteristics | Crude Odds Ratio (95% CI) | p-Value | Adjusted Odds Ratio (95% CI) | p-Value |
|---|---|---|---|---|
| Gender, female, >65 years old (N = 4757) | ||||
| Hyperuricemia (+) | 0.641 (0.536 to 0.767) | <0.001 | 0.806 (0.662 to 0.981) | 0.032 |
| Hyperuricemia (−) | 1.00 | 1.00 | ||
| Gender, female, ≤65 years old (N = 71,556) | ||||
| Hyperuricemia (+) | 0.988 (0.906 to 1.077) | 0.779 | 0.863 (0.785 to 0.950) | 0.003 |
| Hyperuricemia (−) | 1.00 | 1.00 | ||
| Gender, male, >65 years old (N = 3763) | ||||
| Hyperuricemia (+) | 0.863 (0.701 to 1.062) | 0.164 | 0.966 (0.772 to 1.208) | 0.762 |
| Hyperuricemia (−) | 1.00 | 1.00 | ||
| Gender, male, ≤65 years old (N = 38,961) | ||||
| Hyperuricemia (+) | 0.797 (0.737 to 0.862) | <0.001 | 0.932 (0.856 to 1.015) | 0.106 |
| Hyperuricemia (−) | 1.00 | 1.00 | ||
| Characteristics | Number of Cases (%) | Number at Risk | Adjusted Odds Ratio (95% CI) | p-Value |
|---|---|---|---|---|
| Serum uric acid ≤ 4.0 mg/dL | 1387 (7.8) | 17,819 | 1.00 (reference) | |
| 4.0 mg/dL < serum uric acid ≤ 5.0 mg/dL | 2168 (7.6) | 28,516 | 0.859 (0.797 to 0.926) | <0.001 |
| 5.0 mg/dL < serum uric acid ≤ 6.0 mg/dL | 1467 (8.0) | 18,263 | 0.824 (0.757 to 0.896) | <0.001 |
| 6.0 mg/dL < serum uric acid ≤ 7.0 mg/dL | 713 (8.1) | 8789 | 0.794 (0.714 to 0.883) | <0.001 |
| 7.0 mg/dL < serum uric acid ≤ 8.0 mg/dL | 152 (7.0) | 2166 | 0.641 (0.532 to 0.773) | <0.001 |
| Serum uric acid > 8.0 mg/dL | 63 (8.3) | 760 | 0.777 (0.585 to 1.031) | 0.081 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, J.-Y.; Lee, J.-I.; Lu, C.-C.; Su, Y.-D.; Chiu, C.-T.; Chen, S.-C.; Geng, J.-H.; Chen, C.-H. Hyperuricemia and Its Association with Osteoporosis in a Large Asian Cohort. Nutrients 2022, 14, 2206. https://doi.org/10.3390/nu14112206
Li J-Y, Lee J-I, Lu C-C, Su Y-D, Chiu C-T, Chen S-C, Geng J-H, Chen C-H. Hyperuricemia and Its Association with Osteoporosis in a Large Asian Cohort. Nutrients. 2022; 14(11):2206. https://doi.org/10.3390/nu14112206
Chicago/Turabian StyleLi, Jhong-You, Jia-In Lee, Cheng-Chang Lu, Yu-De Su, Chao-Tse Chiu, Szu-Chia Chen, Jiun-Hung Geng, and Chung-Hwan Chen. 2022. "Hyperuricemia and Its Association with Osteoporosis in a Large Asian Cohort" Nutrients 14, no. 11: 2206. https://doi.org/10.3390/nu14112206
APA StyleLi, J.-Y., Lee, J.-I., Lu, C.-C., Su, Y.-D., Chiu, C.-T., Chen, S.-C., Geng, J.-H., & Chen, C.-H. (2022). Hyperuricemia and Its Association with Osteoporosis in a Large Asian Cohort. Nutrients, 14(11), 2206. https://doi.org/10.3390/nu14112206







