Time-Related Eating Patterns Are Associated with the Total Daily Intake of Calories and Macronutrients in Day and Night Shift Workers
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Ethics
2.2. Initial Assessment
2.3. Instruments
2.3.1. Anthropometric Evaluation
2.3.2. Food Intake Evaluation
2.3.3. Time-Related Eating Patterns
2.3.4. Sleep Assessment
2.3.5. Chronotype and Social Jetlag
2.4. Statistical Analysis
2.4.1. Initial Analysis
2.4.2. Comparisons of Time-Related Eating Patterns between Day and Night Workers
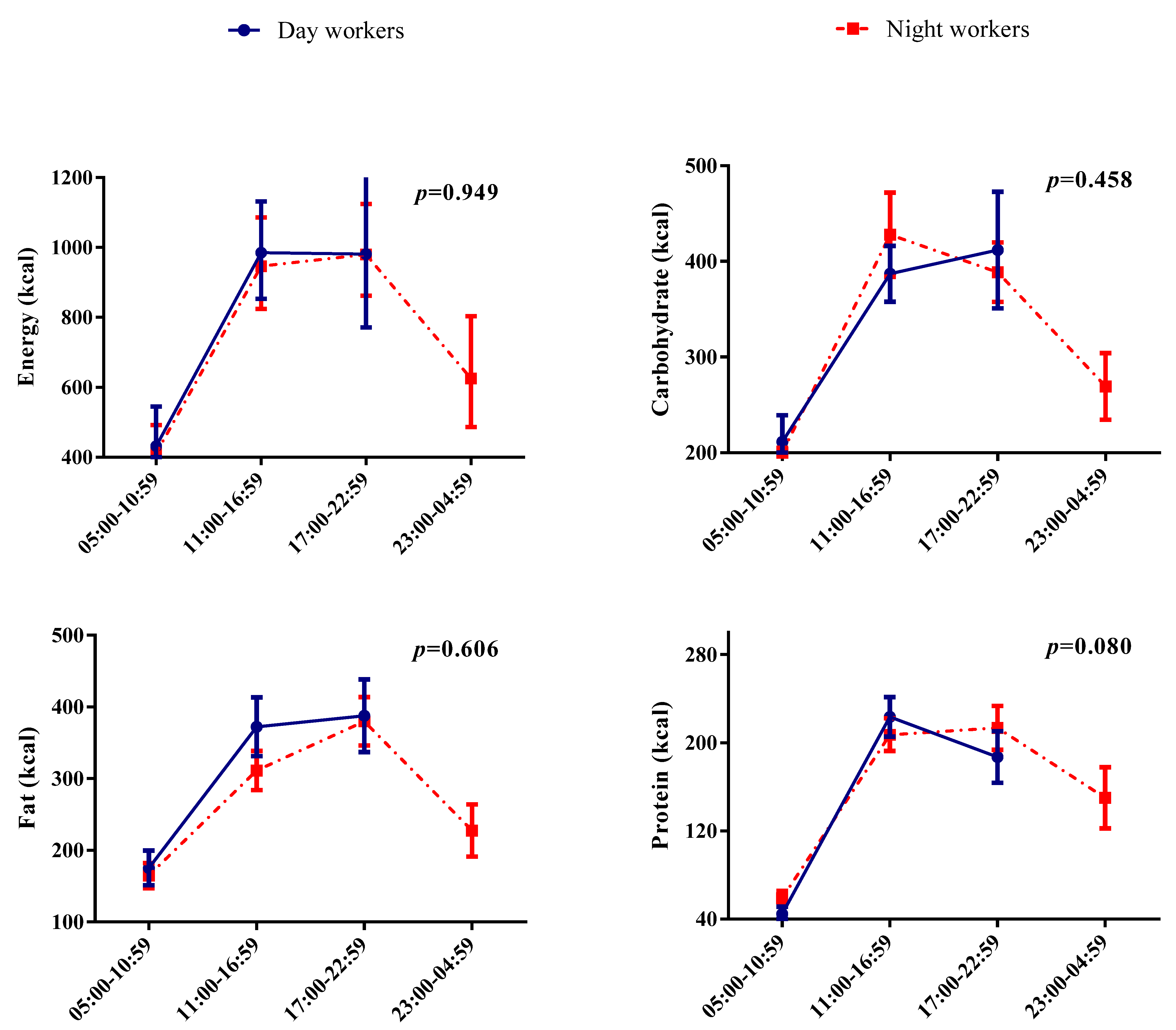
2.4.3. Analysis of the Distribution of Energy and Macronutrients throughout the Day of Day and Night Workers According to Periods
2.4.4. Association Analysis between Time-Related Eating and the Daily Intake of Calories and Macronutrients
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Esquirol, Y.; Perret, B.; Ruidavets, J.B.; Marquie, J.C.; Dienne, E.; Niezborala, M.; Ferrieres, J. Shift work and cardiovascular risk factors: New knowledge from the past decade. Arch. Cardiovasc. Dis. 2011, 104, 636–668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Costa, G. Sleep deprivation due to shift work. Handb. Clin. Neurol. 2015, 131, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Boivin, D.B.; Boudreau, P. Impacts of shift work on sleep and circadian rhythms. Pathol. Biol. 2014, 62, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Brum, M.C.B.; Filho, F.F.D.; Schnorr, C.C.; Bertoletti, O.A.; Bottega, G.B.; da Costa Rodrigues, T. Night shift work, short sleep and obesity. Diabetol. Metab. Syndr. 2020, 12, 13. [Google Scholar] [CrossRef] [Green Version]
- Kervezee, L.; Cuesta, M.; Cermakian, N.; Boivin, D.B. Simulated night shift work induces circadian misalignment of the human peripheral blood mononuclear cell transcriptome. Proc. Natl. Acad. Sci. USA 2018, 115, 5540–5545. [Google Scholar] [CrossRef] [Green Version]
- McHill, A.W.; Phillips, A.J.; Czeisler, C.A.; Keating, L.; Yee, K.; Barger, L.K.; Garaulet, M.; Scheer, F.A.; Klerman, E.B. Later circadian timing of food intake is associated with increased body fat. Am. J. Clin. Nutr. 2017, 106, 1213–1219. [Google Scholar] [CrossRef]
- Dutheil, F.; Baker, J.S.; Mermillod, M.; De Cesare, M.; Vidal, A.; Moustafa, F.; Pereira, B.; Navel, V. Shift work, and particularly permanent night shifts, promote dyslipidaemia: A systematic review and meta-analysis. Atherosclerosis 2020, 313, 156–169. [Google Scholar] [CrossRef]
- Joo, J.H.; Lee, D.W.; Choi, D.W.; Park, E.C. Association between night work and dyslipidemia in South Korean men and women: A cross-sectional study. Lipids Health Dis. 2019, 18, 75. [Google Scholar] [CrossRef] [Green Version]
- Benedito-Silva, A.A.; Evans, S.; Mendes, J.V.; Castro, J.; Gonçalves, B.S.B.; Ruiz, F.S.; Beijamini, F.; Evangelista, F.S.; Vallada, H.; Krieger, J.E.; et al. Association between light exposure and metabolic syndrome in a rural Brazilian town. PLoS ONE 2020, 15, e0238772. [Google Scholar] [CrossRef]
- Smiley, A.; King, D.; Bidulescu, A. The Association between Sleep Duration and Metabolic Syndrome: The NHANES 2013/2014. Nutrients 2019, 11, 2582. [Google Scholar] [CrossRef] [Green Version]
- Chellappa, S.L.; Vujovic, N.; Williams, J.S.; Scheer, F. Impact of Circadian Disruption on Cardiovascular Function and Disease. Trends Endocrinol. Metab. TEM 2019, 30, 767–779. [Google Scholar] [CrossRef] [PubMed]
- Kelly, R.M.; Finn, J.; Healy, U.; Gallen, D.; Sreenan, S.; McDermott, J.H.; Coogan, A.N. Greater social jetlag associates with higher HbA1c in adults with type 2 diabetes: A cross sectional study. Sleep Med. 2020, 66, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Rahim, A.; McIsaac, M.A.; Aronson, K.J.; Smith, P.M.; Tranmer, J.E. The Associations of Shift Work, Sleep Quality, and Incidence of Hypertension in Ontario Adults: A Population-Based Study. Can. J. Cardiol. 2021, 37, 513–518. [Google Scholar] [CrossRef] [PubMed]
- Hemiö, K.; Puttonen, S.; Viitasalo, K.; Härmä, M.; Peltonen, M.; Lindström, J. Food and nutrient intake among workers with different shift systems. Occup. Environ. Med. 2015, 72, 513–520. [Google Scholar] [CrossRef]
- Bonnell, E.K.; Huggins, C.E.; Huggins, C.T.; McCaffrey, T.A.; Palermo, C.; Bonham, M.P. Influences on Dietary Choices during Day versus Night Shift in Shift Workers: A Mixed Methods Study. Nutrients 2017, 9, 193. [Google Scholar] [CrossRef]
- Peplonska, B.; Kaluzny, P.; Trafalska, E. Rotating night shift work and nutrition of nurses and midwives. Chronobiol. Int. 2019, 36, 945–954. [Google Scholar] [CrossRef]
- Knutsson, A.; Karlsson, B.; Ornkloo, K.; Landstrom, U.; Lennernas, M.; Eriksson, K. Postprandial responses of glucose, insulin and triglycerides: Influence of the timing of meal intake during night work. Nutr. Health 2002, 16, 133–141. [Google Scholar] [CrossRef]
- Molzof, H.E.; Wirth, M.D.; Burch, J.B.; Shivappa, N.; Hebert, J.R.; Johnson, R.L.; Gamble, K.L. The impact of meal timing on cardiometabolic syndrome indicators in shift workers. Chronobiol. Int. 2017, 34, 337–348. [Google Scholar] [CrossRef] [Green Version]
- Grant, C.L.; Coates, A.M.; Dorrian, J.; Kennaway, D.J.; Wittert, G.A.; Heilbronn, L.K.; Pajcin, M.; Della Vedova, C.; Gupta, C.C.; Banks, S. Timing of food intake during simulated night shift impacts glucose metabolism: A controlled study. Chronobiol. Int. 2017, 34, 1003–1013. [Google Scholar] [CrossRef]
- Velazquez-Kronen, R.; Millen, A.E.; Ochs-Balcom, H.M.; Mnatsakanova, A.; Gu, J.K.; Andrew, M.; Violanti, J. Sleep Quality and Dietary Patterns in an Occupational Cohort of Police Officers. Behav. Sleep Med. 2021, 1–13. [Google Scholar] [CrossRef]
- Kosmadopoulos, A.; Kervezee, L.; Boudreau, P.; Gonzales-Aste, F.; Vujovic, N.; Scheer, F.; Boivin, D.B. Effects of Shift Work on the Eating Behavior of Police Officers on Patrol. Nutrients 2020, 12, 999. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wehrens, S.M.T.; Christou, S.; Isherwood, C.; Middleton, B.; Gibbs, M.A.; Archer, S.N.; Skene, D.J.; Johnston, J.D. Meal Timing Regulates the Human Circadian System. Curr. Biol. 2017, 27, 1768–1775.e3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leung, G.K.W.; Huggins, C.E.; Bonham, M.P. Effect of meal timing on postprandial glucose response to a low glycemic index meal: A crossover trial in healthy volunteers. Clin. Nutr. 2019, 38, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Reutrakul, S.; Van Cauter, E. Interactions between sleep, circadian function, and glucose metabolism: Implications for risk and severity of diabetes. Ann. N. Y. Acad. Sci. 2014, 1311, 151–173. [Google Scholar] [CrossRef]
- Bandin, C.; Scheer, F.A.; Luque, A.J.; Avila-Gandia, V.; Zamora, S.; Madrid, J.A.; Gomez-Abellan, P.; Garaulet, M. Meal timing affects glucose tolerance, substrate oxidation and circadian-related variables: A randomized, crossover trial. Int. J. Obes. 2015, 39, 828–833. [Google Scholar] [CrossRef]
- Takahashi, M.; Ozaki, M.; Kang, M.I.; Sasaki, H.; Fukazawa, M.; Iwakami, T.; Lim, P.J.; Kim, H.K.; Aoyama, S.; Shibata, S. Effects of Meal Timing on Postprandial Glucose Metabolism and Blood Metabolites in Healthy Adults. Nutrients 2018, 10, 1763. [Google Scholar] [CrossRef] [Green Version]
- Poggiogalle, E.; Jamshed, H.; Peterson, C.M. Circadian regulation of glucose, lipid, and energy metabolism in humans. Metab. Clin. Exp. 2018, 84, 11–27. [Google Scholar] [CrossRef] [Green Version]
- Kahleova, H.; Lloren, J.I.; Mashchak, A.; Hill, M.; Fraser, G.E. Meal Frequency and Timing Are Associated with Changes in Body Mass Index in Adventist Health Study 2. J. Nutr. 2017, 147, 1722–1728. [Google Scholar] [CrossRef] [Green Version]
- Ha, K.; Song, Y. Associations of Meal Timing and Frequency with Obesity and Metabolic Syndrome among Korean Adults. Nutrients 2019, 11, 2437. [Google Scholar] [CrossRef] [Green Version]
- Zeron-Rugerio, M.F.; Hernaez, A.; Porras-Loaiza, A.P.; Cambras, T.; Izquierdo-Pulido, M. Eating Jet Lag: A Marker of the Variability in Meal Timing and Its Association with Body Mass Index. Nutrients 2019, 11, 2980. [Google Scholar] [CrossRef] [Green Version]
- Reid, K.J.; Baron, K.G.; Zee, P.C. Meal timing influences daily caloric intake in healthy adults. Nutr. Res. 2014, 34, 930–935. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- St-Onge, M.P.; Pizinger, T.; Kovtun, K.; RoyChoudhury, A. Sleep and meal timing influence food intake and its hormonal regulation in healthy adults with overweight/obesity. Eur. J. Clin. Nutr. 2019, 72, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Gontijo, C.A.; Balieiro, L.C.T.; Teixeira, G.P.; Fahmy, W.M.; Crispim, C.A.; Maia, Y.C.P. Effects of timing of food intake on eating patterns, diet quality and weight gain during pregnancy. Br. J. Nutr. 2020, 123, 922–933. [Google Scholar] [CrossRef] [PubMed]
- Gill, S.; Panda, S. A smartphone app reveals erratic diurnal eating patterns in humans that can be modulated for health benefits. Cell Metab. 2015, 22, 789–798. [Google Scholar] [CrossRef] [Green Version]
- Paoli, A.; Tinsley, G.; Bianco, A.; Moro, T. The Influence of Meal Frequency and Timing on Health in Humans: The Role of Fasting. Nutrients 2019, 11, 719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barrington, W.E.; Beresford, S.A.A. Eating Occasions, Obesity and Related Behaviors in Working Adults: Does it Matter When You Snack? Nutrients 2019, 11, 2320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaix, A.; Zarrinpar, A.; Miu, P.; Panda, S. Time-restricted feeding is a preventive and therapeutic intervention against diverse nutritional challenges. Cell Metab. 2014, 20, 991–1005. [Google Scholar] [CrossRef] [Green Version]
- Melkani, G.C.; Panda, S. Time-restricted feeding for prevention and treatment of cardiometabolic disorders. J. Physiol. 2017, 595, 3691–3700. [Google Scholar] [CrossRef] [Green Version]
- Lohmann, T.G.; Roche, A.F.; Martorrel, R. Anthropometrics Standardization Reference Manual; Knectis, H., Ed.; Human Knectis: Champaign, IL, USA, 1988. [Google Scholar]
- Teixeira, G.P.; Barreto, A.C.F.; Mota, M.C.; Crispim, C.A. Caloric midpoint is associated with total calorie and macronutrient intake and body mass index in undergraduate students. Chronobiol. Int. 2019, 36, 1418–1428. [Google Scholar] [CrossRef]
- Marot, L.P.; Rosa, D.E.; Lopes, T.; Moreno, C.R.C.; Crispim, C.A. Eating Duration throughout a Rotating Shift Schedule: A Case Study. J. Am. Coll. Nutr. 2021, 40, 624–631. [Google Scholar] [CrossRef]
- Gibney, M.J.; Wolever, T.M. Periodicity of eating and human health: Present perspective and future directions. Br. J. Nutr. 1997, 77 (Suppl. S1), S3–S5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marino, M.; Li, Y.; Rueschman, M.N.; Winkelman, J.W.; Ellenbogen, J.M.; Solet, J.M.; Dulin, H.; Berkman, L.F.; Buxton, O.M. Measuring sleep: Accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep 2013, 36, 1747–1755. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.L.; Hakim, A.D. Wrist actigraphy. Chest 2011, 139, 1514–1527. [Google Scholar] [CrossRef] [PubMed]
- Roenneberg, T.; Allebrandt, K.V.; Merrow, M.; Vetter, C. Social jetlag and obesity. Curr. Biol. 2012, 22, 939–943. [Google Scholar] [CrossRef] [Green Version]
- Peplonska, B.; Nowak, P.; Trafalska, E. The association between night shift work and nutrition patterns among nurses: A literature review. Med. Pr. 2019, 70, 363–376. [Google Scholar] [CrossRef]
- Tada, Y.; Kawano, Y.; Maeda, I.; Yoshizaki, T.; Sunami, A.; Yokoyama, Y.; Matsumoto, H.; Hida, A.; Komatsu, T.; Togo, F. Association of body mass index with lifestyle and rotating shift work in Japanese female nurses. Obesity 2014, 22, 2489–2493. [Google Scholar] [CrossRef]
- Balieiro, L.C.; Rossato, L.T.; Waterhouse, J.; Paim, S.L.; Mota, M.C.; Crispim, C.A. Nutritional status and eating habits of bus drivers during the day and night. Chronobiol. Int. 2014, 31, 1123–1129. [Google Scholar] [CrossRef]
- Oussaada, S.M.; van Galen, K.A.; Cooiman, M.I.; Kleinendorst, L.; Hazebroek, E.J.; van Haelst, M.M.; Ter Horst, K.W.; Serlie, M.J. The pathogenesis of obesity. Metab. Clin. Exp. 2019, 92, 26–36. [Google Scholar] [CrossRef] [Green Version]
- Saltiel, A.R.; Olefsky, J.M. Inflammatory mechanisms linking obesity and metabolic disease. J. Clin. Investig. 2017, 127, 1–4. [Google Scholar] [CrossRef]
- Wang, J.B.; Patterson, R.E.; Ang, A.; Emond, J.A.; Shetty, N.; Arab, L. Timing of energy intake during the day is associated with the risk of obesity in adults. J. Hum. Nutr. Diet. Off. J. Br. Diet. Assoc. 2014, 27 (Suppl. S2), 255–262. [Google Scholar] [CrossRef]
- Xiao, Q.; Garaulet, M.; Scheer, F. Meal timing and obesity: Interactions with macronutrient intake and chronotype. Int. J. Obes. 2019, 43, 1701–1711. [Google Scholar] [CrossRef] [PubMed]
- de Castro, J.M. The time of day of food intake influences overall intake in humans. J. Nutr. 2004, 134, 104–111. [Google Scholar] [CrossRef] [PubMed]
- de Castro, J.M. The time of day and the proportions of macronutrients eaten are related to total daily food intake. Br. J. Nutr. 2007, 98, 1077–1083. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raynor, H.A.; Li, F.; Cardoso, C. Daily pattern of energy distribution and weight loss. Physiol. Behav. 2018, 192, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Fong, M.; Caterson, I.D.; Madigan, C.D. Are large dinners associated with excess weight, and does eating a smaller dinner achive greater weight loss? A systematic review and meta-analysis. Br. J. Nutr. 2017, 118, 616–628. [Google Scholar] [CrossRef]
- Challet, E. The circadian regulation of food intake. Nat. Rev. Endocrinol. 2019, 15, 393–405. [Google Scholar] [CrossRef]
- Crispim, C.A.; Mota, M.C. New perspectives on chrononutrition. Biol. Rhythm. Res. 2019, 50, 1–15. [Google Scholar]
- Gupta, N.J.; Kumar, V.; Panda, S. A camera-phone based study reveals erratic eating pattern and disrupted daily eating-fasting cycle among adults in India. PLoS ONE 2017, 12, e0172852. [Google Scholar] [CrossRef]
- McHill, A.W.; Melanson, E.L.; Higgins, J.; Connick, E.; Moehlman, T.M.; Stothard, E.R.; Wright, K.P., Jr. Impact of circadian misalignment on energy metabolism during simulated nightshift work. Proc. Natl. Acad. Sci. USA 2014, 111, 17302–17307. [Google Scholar] [CrossRef] [Green Version]
- Qian, J.; Morris, C.J.; Caputo, R.; Wang, W.; Garaulet, M.; Scheer, F. Sex differences in the circadian misalignment effects on energy regulation. Proc. Natl. Acad. Sci. USA 2019, 116, 23806–23812. [Google Scholar] [CrossRef]
- McHill, A.W.; Wright, K.P., Jr. Role of sleep and circadian disruption on energy expenditure and in metabolic predisposition to human obesity and metabolic disease. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2017, 18 (Suppl. S1), 15–24. [Google Scholar] [CrossRef] [PubMed]
- Stenvers, D.J.; Scheer, F.; Schrauwen, P.; la Fleur, S.E.; Kalsbeek, A. Circadian clocks and insulin resistance. Nat. Rev. Endocrinol. 2019, 15, 75–89. [Google Scholar] [CrossRef] [PubMed]
- Morris, C.J.; Purvis, T.E.; Hu, K.; Scheer, F.A. Circadian misalignment increases cardiovascular disease risk factors in humans. Proc. Natl. Acad. Sci. USA 2016, 113, E1402–E1411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silva, C.M.; Mota, M.C.; Miranda, M.T.; Paim, S.L.; Waterhouse, J.; Crispim, C.A. Chronotype, social jetlag and sleep debt are associated with dietary intake among Brazilian undergraduate students. Chronobiol. Int. 2016, 33, 740–748. [Google Scholar] [CrossRef]
- Mota, M.C.; Silva, C.M.; Balieiro, L.C.T.; Goncalves, B.F.; Fahmy, W.M.; Crispim, C.A. Association between social jetlag food consumption and meal times in patients with obesity-related chronic diseases. PLoS ONE 2019, 14, e0212126. [Google Scholar] [CrossRef] [Green Version]
- Carvalho, A.C.; Mota, M.C.; Marot, L.P.; Mattar, L.A.; de Sousa, J.A.G.; Araujo, A.C.T.; da Costa Assis, C.T.; Crispim, C.A. Circadian Misalignment Is Negatively Associated with the Anthropometric, Metabolic and Food Intake Outcomes of Bariatric Patients 6 Months After Surgery. Obes. Surg. 2021, 31, 159–169. [Google Scholar] [CrossRef] [PubMed]
- McMahon, D.M.; Burch, J.B.; Youngstedt, S.D.; Wirth, M.D.; Hardin, J.W.; Hurley, T.G.; Blair, S.N.; Hand, G.A.; Shook, R.P.; Drenowatz, C.; et al. Relationships between chronotype, social jetlag, sleep, obesity and blood pressure in healthy young adults. Chronobiol. Int. 2019, 36, 493–509. [Google Scholar] [CrossRef]
- Mota, M.C.; Silva, C.M.; Balieiro, L.C.T.; Fahmy, W.M.; Crispim, C.A. Social jetlag and metabolic control in non-communicable chronic diseases: A study addressing different obesity statuses. Sci. Rep. 2017, 7, 6358. [Google Scholar] [CrossRef] [Green Version]
- Parsons, M.J.; Moffitt, T.E.; Gregory, A.M.; Goldman-Mellor, S.; Nolan, P.M.; Poulton, R.; Caspi, A. Social jetlag, obesity and metabolic disorder: Investigation in a cohort study. Int. J. Obes. 2015, 39, 842–848. [Google Scholar] [CrossRef] [Green Version]
| Day Shift Workers (n = 29) | Night Shift Workers (n = 52) | p | |
|---|---|---|---|
| Age (years) | 36.4 ± 0.9 | 38.5 ± 0.7 | 0.081 |
| Marital status | |||
| Single (%) | 20.7 (6) | 25.0 (13) | 0.661 |
| Married (%) | 79.3 (23) | 75.0 (39) | |
| Schooling | |||
| High-school (%) | 24.1 (7) | 28.8 (15) | 0.650 |
| Graduate (%) | 62.1 (18) | 63.5 (33) | |
| Postgraduate (%) | 13.8 (4) | 7.7 (4) | |
| Smoking | |||
| Yes (%) | 3.4 (1) | 15.4 (8) | 0.101 |
| No (%) | 96.6 (28) | 84.6 (44) | |
| Alcoholic beverages | |||
| Yes (%) | 62.1 (18) | 75.0 (39) | 0.222 |
| No (%) | 37.9 (11) | 25.0 (13) | |
| Regular physical exercise | |||
| Yes (%) | 51.7 (15) | 90.4 (47) | <0.001 |
| No (%) | 48.3 (14) | 9.6 (5) | |
| Time of shift work (years) | 3.4 ± 0.5 | 7.1 ± 0.8 | <0.001 |
| Weight (kg) | 91.6 ± 2.1 | 87.7 ± 1.5 | 0.131 |
| Height (m) | 1.78 ± 0.01 | 1.76 ± 0.00 | 0.086 |
| WC (cm) | 98.5 ± 1.6 | 95.9 ± 1.2 | 0.201 |
| BMI (kg/m²) | 28.7 ± 0.6 | 28.2 ± 0.4 | 0.519 |
| Sleep duration (hours) | 5.9 ± 0.2 | 4.8 ± 0.1 | 0.002 |
| MSF | 3:20 ± 0:20 | 3:40 ± 0:15 | 0.443 |
| Social jetlag (hours) | 1.2 ± 0.1 | 6.1 ± 0.4 | <0.001 |
| Day Shift Workers (n = 29) | Night Shift Workers (n = 52) | p | |
|---|---|---|---|
| Number of meals | 3.9 ± 0.1 | 4.1 ± 0.1 | 0.185 |
| Time of the first meal (h) | 8.4 ± 0.3 | 8.8 ± 0.2 | 0.288 |
| Time of the last meal (h) | 20.5 ± 0.2 | 23.1 ± 0.2 | <0.001 |
| Eating duration (hours) | 12.1 ± 0.4 | 14.4 ± 0.3 | <0.001 |
| Night fasting (hours) | 10.0 ± 0.4 | 7.3 ± 0.2 | <0.001 |
| Caloric midpoint (h) | 14.8 ± 0.4 | 15.9 ± 0.3 | 0.037 |
| Energy (kcal) | 2329.2 ± 198.3 | 2774.9 ± 170.4 | 0.095 |
| Energy (kcal/kg) | 24.8 ± 2.0 | 27.9 ± 1.5 | 0.184 |
| Carbohydrate (kcal) | 980.7 ± 89.6 | 1193.7 ± 91.1 | 0.099 |
| Carbohydrate (kcal/kg) | 31.1 ± 3.3 | 36.0 ± 2.5 | 0.175 |
| Fat (kcal) | 903.6 ± 88.1 | 1005.5 ± 71.1 | 0.375 |
| Fat (kcal/kg) | 9.6 ± 0.8 | 10.0 ± 0.6 | 0.691 |
| Protein (kcal) | 444.9 ± 39.7 | 575.6 ± 37.8 | 0.020 |
| Protein (kcal/kg) | 4.7 ± 0.3 | 5.8 ± 0.3 | 0.038 |
| Energy and Macronutrients | Day Workers (n = 29) | Night Workers (n = 52) | Shift | Caloric Midpoint | Shift and Caloric Midpoint Interaction | ||
|---|---|---|---|---|---|---|---|
| Early Eaters (n = 19) | Late Eaters (n = 10) | Early Eaters (n = 18) | Late Eaters (n = 25) | p | p | p | |
| Energy (kcal) | 2024.7 ± 135.0 | 2907.9 ± 462.5 | 2611.3 ± 242.3 | 2894.9 ± 233.5 | 0.238 | 0.028 | 0.222 |
| Energy (kcal/kg) | 22.1 ± 1.6 | 30.0 ± 3.3 | 26.7 ± 2.5 | 28.8 ± 2.1 | 0.405 | 0.035 | 0.204 |
| Energy (%) | 35.4 ± 1.0 | 35.7 ± 1.2 | 31.4 ± 0.9 | 32.1 ± 0.7 | <0.001 | 0.597 | 0.816 |
| Carbohydrate (kcal) | 307.5 ± 23.2 | 405.8 ± 70.8 | 324.7 ± 30.7 | 340.5 ± 34.2 | 0.606 | 0.167 | 0.328 |
| Carbohydrate (kcal/kg) | 29.1 ± 2.5 | 35.0 ± 4.5 | 36.6 ± 3.8 | 35.6 ± 4.0 | 0.268 | 0.470 | 0.338 |
| Carbohydrate (%) | 44.2 ± 1.7 | 39.7 ± 2.5 | 46.8 ± 1.9 | 40.1 ± 2.1 | 0.525 | 0.010 | 0.629 |
| Fat (kcal) | 264.0 ± 21.8 | 418.7 ± 65.9 | 258.5 ± 30.5 | 302.4 ± 23.0 | 0.126 | 0.006 | 0.180 |
| Fat (kcal/kg) | 8.2 ± 0.7 | 12.3 ± 1.4 | 9.5 ± 1.17 | 10.4 ± 0.7 | 0.938 | 0.019 | 0.143 |
| Fat (%) | 36.5 ± 1.5 | 40.3 ± 2.0 | 34.0 ± 1.7 | 36.4 ± 1.4 | 0.062 | 0.071 | 0.758 |
| Protein (kcal) | 131.4 ± 8.4 | 204.1 ± 29.3 | 133.3 ± 10.4 | 187.3 ± 16.5 | 0.715 | <0.001 | 0.613 |
| Protein (kcal/kg) | 4.1 ± 0.2 | 6.0 ± 0.8 | 4.9 ± 0.4 | 6.5 ± 0.5 | 0.181 | 0.001 | 0.560 |
| Protein (%) | 19.1 ± 0.7 | 19.8 ± 1.5 | 19.1 ± 1.0 | 23.5 ± 1.4 | 0.165 | 0.042 | 0.151 |
| Independent Variables | Dependent Variables | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day Shift Workers (n = 29) | Night Shift Workers (n = 52) | |||||||||||||||
| Time-Related Eating Patterns | Energy (kcal) | Carbohydrate (kcal) | Fat (kcal) | Protein (kcal) | Energy (kcal) | Carbohydrate (kcal) | Fat (kcal) | Protein (kcal) | ||||||||
| β | p | β | p | β | p | β | p | β | p | β | p | β | p | β | p | |
| Number of meals | 0.406 | 0.022 | 0.470 | 0.005 | 0.250 | 0.189 | 0.409 | 0.031 | 0.363 | 0.011 | 0.414 | 0.004 | 0.227 | 0.113 | 0.213 | 0.144 |
| Time of the first meal | −0.401 | 0.024 | −0.374 | 0.031 | −0.365 | 0.051 | −0.351 | 0.068 | 0.080 | 0.572 | −0.055 | 0.705 | 0.127 | 0.364 | 0.255 | 0.068 |
| Time of the last meal | 0.352 | 0.044 | 0.299 | 0.082 | 0.284 | 0.124 | 0.451 | 0.013 | 0.424 | 0.002 | 0.346 | 0.016 | 0.286 | 0.042 | 0.536 | <0.001 |
| Eating duration | 0.473 | 0.004 | 0.418 | 0.011 | 0.412 | 0.020 | 0.505 | 0.004 | 0.320 | 0.023 | 0.364 | 0.010 | 0.158 | 0.266 | 0.267 | 0.060 |
| Night fasting | −0.396 | 0.019 | −0.356 | 0.032 | −0.284 | 0.119 | −0.546 | 0.002 | −0.446 | 0.001 | −0.408 | 0.004 | −0.270 | 0.052 | −0.520 | <0.001 |
| Caloric midpoint | 0.421 | 0.014 | 0.243 | 0.162 | 0.475 | 0.007 | 0.501 | 0.005 | 0.102 | 0.482 | 0.027 | 0.854 | 0.068 | 0.633 | 0.265 | 0.063 |
| Social jetlag | −0.040 | 0.827 | −0.101 | 0.576 | −0.016 | 0.932 | 0.314 | 0.756 | 0.209 | 0.151 | 0.166 | 0.265 | 0.282 | 0.047 | 0.011 | 0.942 |
| Sleep duration | −0.266 | 0.144 | −0.171 | 0.340 | −0.332 | 0.077 | −0.204 | 0.298 | 0.074 | 0.652 | 0.155 | 0.347 | −0.010 | 0.951 | −0.031 | 0.850 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, C.M.; Teixeira, B.S.; Wright, K.P., Jr.; Maia, Y.C.d.P.; Crispim, C.A. Time-Related Eating Patterns Are Associated with the Total Daily Intake of Calories and Macronutrients in Day and Night Shift Workers. Nutrients 2022, 14, 2202. https://doi.org/10.3390/nu14112202
Silva CM, Teixeira BS, Wright KP Jr., Maia YCdP, Crispim CA. Time-Related Eating Patterns Are Associated with the Total Daily Intake of Calories and Macronutrients in Day and Night Shift Workers. Nutrients. 2022; 14(11):2202. https://doi.org/10.3390/nu14112202
Chicago/Turabian StyleSilva, Catarina Mendes, Bruno Simão Teixeira, Kenneth P. Wright, Jr., Yara Cristina de Paiva Maia, and Cibele Aparecida Crispim. 2022. "Time-Related Eating Patterns Are Associated with the Total Daily Intake of Calories and Macronutrients in Day and Night Shift Workers" Nutrients 14, no. 11: 2202. https://doi.org/10.3390/nu14112202
APA StyleSilva, C. M., Teixeira, B. S., Wright, K. P., Jr., Maia, Y. C. d. P., & Crispim, C. A. (2022). Time-Related Eating Patterns Are Associated with the Total Daily Intake of Calories and Macronutrients in Day and Night Shift Workers. Nutrients, 14(11), 2202. https://doi.org/10.3390/nu14112202







