The Impact of a Culinary Coaching Telemedicine Program on Home Cooking and Emotional Well-Being during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
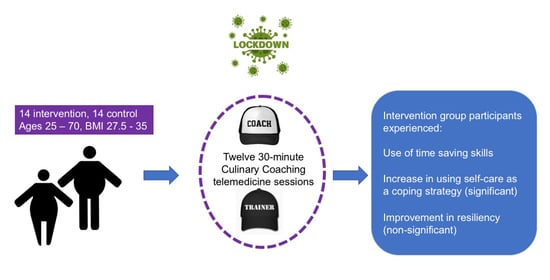
2.1. Setting and Participants
2.2. The Culinary Coaching Telemedicine Program
2.3. Pandemic Evaluation
2.4. Data Analysis
2.5. Qualitative Analysis
3. Results
3.1. Coping Strategies during the Pandemic
3.2. Pandemic-Related Changes in Home Cooking and Emotional Well-Being
3.3. CCPT-Related Changes in Home Cooking and Emotional Well-Being
3.4. Overall Change in Nutrition, Weight and Health
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Bhaskar, S.; Bradley, S.; Chattu, V.K.; Adisesh, A.; Nurtazina, A.; Kyrykbayeva, S.; Sakhamuri, S.; Moguilner, S.; Pandya, S.; Schroeder, S.; et al. Telemedicine as the New Outpatient Clinic Gone Digital: Position Paper from the Pandemic Health System Resilience PROGRAM (REPROGRAM) International Consortium (Part 2). Front. Public Health 2020, 8, 410. [Google Scholar] [CrossRef]
- Joiner, K.L.; Nam, S.; Whittemore, R. Lifestyle Interventions Based on the Diabetes Prevention Program Delivered via eHealth: A Systematic Review and Meta-analysis. Prev. Med. 2017, 100, 194–207. [Google Scholar] [CrossRef]
- Polak, R.; Pober, D.M.; Budd, M.A.; Silver, J.K.; Phillips, E.M.; Abrahamson, M.J. Improving Patients’ Home Cooking-A Case Series of Participation in a Remote Culinary Coaching Program. Appl. Physiol. Nutr. Metab. 2017, 42, 893–896. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polak, R.; Pober, D.; Finkelstein, A.; Budd, M.A.; Moore, M.; Silver, J.K.; Phillips, E.M. Innovation in Medical Education: A Culinary Coaching Tele-nutrition Training Program. Med. Educ. Online 2018, 23, 1510704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, K.E.; Alencar, M.K.; Coakley, K.E.; Swift, D.L.; Cole, N.H.; Mermier, C.M.; Kravitz, L.; Amorim, F.T.; Gibson, A.L. Telemedicine-Based Health Coaching is Effective for Inducing Weight Loss and Improving Metabolic Markers. Telemed. J. e-Health 2019, 25, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Gabriele, J.M.; Carpenter, B.D.; Tate, D.F.; Fisher, E.B. Directive and Nondirective E-coach Support for Weight Loss in Overweight Adults. Ann. Behav. Med. 2011, 41, 252–263. [Google Scholar] [CrossRef] [Green Version]
- Srivastava, P.; Verma, A.; Geronimo, C.; Button, T.M. Behavior Stages of a Physician- and Coach-Supported Cloud-Based Diabetes Prevention Program for People with Prediabetes. SAGE Open Med. 2019, 7, 2050312119841986. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bollyky, J.B.; Bravata, D.; Yang, J.; Williamson, M.; Schneider, J. Remote Lifestyle Coaching Plus a Connected Glucose Meter With Certified Diabetes Educator Support Improves Glucose and Weight Loss for People with Type 2 Diabetes. J. Diabetes Res. 2018, 2018, 3961730. [Google Scholar] [CrossRef] [PubMed]
- Tropea, P.; Schlieter, H.; Sterpi, I.; Judica, E.; Gand, K.; Caprino, M.; Gabilondo, I.; Gomez-Esteban, J.C.; Busnatu, S.; Sinescu, C.; et al. Rehabilitation, the Great Absentee of Virtual Coaching in Medical Care: Scoping Review. J. Med. Internet Res. 2019, 21, e12805. [Google Scholar] [CrossRef]
- Sell, N.M.; Silver, J.K.; Rando, S.; Draviam, A.C.; Mina, D.S.; Qadan, M. Prehabilitation Telemedicine in Neoadjuvant Surgical Oncology Patients during the Novel COVID-19 Coronavirus Pandemic. Ann. Surg. 2020, 272, e81–e83. [Google Scholar] [CrossRef]
- Verduzco-Gutierrez, M.; Bean, A.C.; Tenforde, A.S.; Tapia, R.N.; Silver, J.K. How to Conduct an Outpatient Telemedicine Rehabilitation or Prehabilitation Visit. Pract. Manag. 2020, 12, 714–720. [Google Scholar] [CrossRef] [PubMed]
- Turolla, A.; Rossettini, G.; Viceconti, A.; Palese, A.; Geri, T. Musculoskeletal Physical Therapy during the COVID-19 Pandemic: Is telerehabilitation the Answer? Phys Ther. 2020, 100, 1260–1264. [Google Scholar] [CrossRef] [PubMed]
- Bhuva, S.; Lankford, C.; Patel, N.; Haddas, R. Implementation and Patient Satisfaction of Telemedicine in Spine Physical Medicine and Rehabilitation Patients during the COVID-19 Shutdown. Am. J. Phys. Med. Rehabil. 2020, 99, 1079–1085. [Google Scholar] [CrossRef]
- Wahezi, S.E.; Duarte, R.V.; Yerra, S.; Thomas, M.A.; Pujar, B.; Sehgal, N.; Argoff, C.; Manchikanti, L.; Gonzalez, D.; Jain, R.; et al. Telemedicine during COVID-19 and Beyond: A Practical Guide and Best Practices Multidisciplinary Approach for the Orthopedic and Neurologic Pain Physical Examination. Pain Physician 2020, 23, S205–S238. [Google Scholar]
- Contreras, C.M.; Metzger, G.A.; Beane, J.D.; Dedhia, P.H.; Ejaz, A.; Pawlik, T.M. Telemedicine: Patient-Provider Clinical Engagement during the COVID-19 Pandemic and Beyond. J. Gastrointest. Surg. 2020, 24, 1692–1697. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Lu, Z.A.; Que, J.Y.; Huang, X.L.; Liu, L.; Ran, M.S.; Gong, Y.M.; Yuan, K.; Yan, W.; Sun, Y.K.; et al. Prevalence of and Risk Factors Associated with Mental Health Symptoms Among the General Population in China during the Coronavirus Disease 2019 Pandemic. JAMA Netw. Open 2020, 3, e2014053. [Google Scholar] [CrossRef]
- Duncan, G.E.; Avery, A.R.; Seto, E.; Tsang, S. Perceived Change in Physical Activity Levels and Mental Health during COVID-19: Findings Among Adult Twin Pairs. PLoS ONE 2020, 15, e0237695. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating Habits and Lifestyle Changes during COVID-19 Lockdown: An Italian Survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef]
- Kolokotroni, O.; Mosquera, M.C.; Quattrocchi, A.; Heraclides, A.; Demetriou, C.; Philippou, E. Lifestyle Habits of Adults during the COVID-19 Pandemic Lockdown in Cyprus: Evidence from a Cross-Sectional Study. BMC Public Health 2021, 21, 786. [Google Scholar] [CrossRef]
- Saqib, M.A.N.; Siddiqui, S.; Qasim, M.; Jamil, M.A.; Rafique, I.; Awan, U.A.; Ahmad, H.; Afzal, M.S. Effect of COVID-19 Lockdown on Patients with Chronic Diseases. Diabetes Metab. Syndr. 2020, 14, 1621–1623. [Google Scholar] [CrossRef]
- Assaloni, R.; Pellino, V.C.; Puci, M.V.; Ferraro, O.E.; Lovecchio, N.; Girelli, A.; Vandoni, M. Coronavirus disease (Covid-19): How does the exercise practice in active people with type 1 diabetes change? A preliminary survey. Diabetes Res. Clin. Pract. 2020, 166, 108297. [Google Scholar] [CrossRef] [PubMed]
- Elran-Barak, R.; Mozeikov, M. One Month into the Reinforcement of Social Distancing due to the COVID-19 Outbreak: Subjective Health, Health Behaviors, and Loneliness among People with Chronic Medical Conditions. Int. J. Environ. Res. Public Health 2020, 17, 5403. [Google Scholar] [CrossRef]
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef]
- Belanger, M.J.; Hill, M.A.; Angelidi, A.M.; Dalamaga, M.; Sowers, J.R.; Mantzoros, C.S. Covid19 and Disparities in Nutrition and Obesity. N. Engl. J. Med. 2020, 383, e69. [Google Scholar] [CrossRef]
- Polak, R.; Dill, D.; Abrahamson, M.J.; Pojednic, R.M.; Phillips, E.M. Innovation in Diabetes Care: Improving Consumption of Healthy Food through a “Chef Coaching” Program: A Case Report. Glob. Adv. Health Med. 2014, 3, 42–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carver, C.S. You Want to Measure Coping but your Protocol’s too Long: Consider the Brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef]
- Hoyt, M.A.; Marin-Chollom, A.M.; Bower, J.E.; Thomas, K.S.; Irwin, M.R.; Stanton, A.L. Approach and Avoidance Coping: Diurnal Cortisol Rhythm in Prostate Cancer Survivors. Psychoneuroendocrinology 2014, 49, 182–186. [Google Scholar] [CrossRef] [Green Version]
- Sinclair, V.G.; Wallston, K.A. The Development and Psychometric Evaluation of the Brief Resilient Coping Scale. Assessment 2004, 11, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Hanley, J.A.; McNeil, B.J. The Meaning and Use of the Area under a Receiver Operating Characteristic (ROC) Curve. Radiology 1982, 143, 29–36. [Google Scholar] [CrossRef] [Green Version]
- De Schryver, M.; De Neve, J. A Tutorial on Probabilistic Index Models. Psychol. Methods 2019, 24, 403–418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Acion, L.; Peterson, J.J.; Temple, S.; Arndt, S. Probabilistic index: An intuitive non-parametric approach to measuring the size of treatment effects. Stat. Med. 2006, 25, 591–602. [Google Scholar] [CrossRef] [PubMed]
- Dubey, S.; Biswas, P.; Ghosh, R.; Chatterjee, S.; Dubey, M.J.; Chatterjee, S.; Lahiri, D.; Lavie, C.J. Psychosocial Impact of COVID-19. Diabetes Metab. Syndr. 2020, 14, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Hill, A.J. Obesity and Eating Disorders. Obes. Rev. 2007, 8 (Suppl. 1), 151–155. [Google Scholar] [CrossRef]
- Bolton, K.W.; Praetorius, R.T.; Smith-Osborne, A. Resilience Protective Factors in an Older Adult Population: A Qualitative Interpretive Meta-Synthesis. Soc. Work. Res. 2016, 40, 171–182. [Google Scholar] [CrossRef]
- Polak, R.; Tirosh, A.; Livingston, B.; Pober, D.; Eubanks, J.E., Jr.; Silver, J.K.; Minezaki, K.; Loten, R.; Phillips, E.M. Preventing Type 2 Diabetes with Home Cooking: Current Evidence and Future Potential. Diabetes Rep. 2018, 18, 99. [Google Scholar] [CrossRef]
- Downer, S.; Berkowitz, S.A.; Harlan, T.S.; Olstad, D.L.; Mozaffarian, D. Food is Medicine: Actions to Integrate Food and Nutrition into Healthcare. BMJ 2020, 369, m2482. [Google Scholar] [CrossRef] [PubMed]
- Groesz, L.M.; McCoy, S.; Carl, J.; Saslow, L.; Stewart, J.; Adler, N.; Laraia, B.; Epel, E. What is Eating You? Stress and the Drive to Eat. Appetite 2012, 58, 717–721. [Google Scholar] [CrossRef] [Green Version]
- Khaled, K.; Tsofliou, F.; Hundley, V.; Helmreich, R.; Almilaji, O. Perceived Stress and Diet Quality in Women of Reproductive Age: A Systematic Review and Meta-Analysis. Nutr. J. 2020, 19, 92. [Google Scholar] [CrossRef]
- Ruffault, A.; Czernichow, S.; Hagger, M.S.; Ferrand, M.; Erichot, N.; Carette, C.; Boujut, E.; Flahault, C. The Effects of Mindfulness Training on Weight-Loss and Health-Related Behaviors in Adults with Overweight and Obesity: A Systematic Review and Meta-Analysis. Obes. Res. Clin. Pract. 2017, 11, 90–111. [Google Scholar] [CrossRef] [Green Version]
- Steere, H.K.; Polich, G.; Silver, J.K.; Hameed, F.; Gellhorn, A.C.; Borg-Stein, J.; Schneider, J.C. Ambulatory Rehabilitation of Patients Hospitalized with SARS CoV-2 Infections: Early Pandemic Experience in New York City and Boston. Pract. Manag. 2020, 13, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Report to Congress: E-Health and Telemedicine. Available online: https://aspe.hhs.gov/pdf-report/report-congress-e-health-and-telemedicine (accessed on 2 June 2021).
- Sommer, A.C.; Blumenthal, E.Z. Telemedicine in Ophthalmology in View of the Emerging COVID-19 Outbreak. Graefes Arch. Clin. Exp. Ophthalmol. 2020, 258, 2341–2352. [Google Scholar] [CrossRef] [PubMed]
- Abbasi-Feinberg, F. Telemedicine Coding and Reimbursement-Current and Future Trends. Sleep Med. Clin. 2020, 15, 417–429. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.K. The Growth of Telehealth: 20 Things to Know. Becker’s Hospital Review. Available online: https://www.beckershospitalreview.com/healthcare-information-technology/the-growth-of-telehealth-20-things-to-know.html (accessed on 2 January 2021).
- Tenforde, A.S.; Borgstrom, H.; Polich, G.; Steere, H.; Davis, I.S.; Cotton, K.; O’Donnell, M.; Silver, J.K. Outpatient Physical, Occupational, and Speech Therapy Synchronous Telemedicine: A Survey Study of Patient Satisfaction with Virtual Visits during the COVID-19 Pandemic. Am. J. Phys. Med. Rehabil. 2020, 99, 977–981. [Google Scholar] [CrossRef] [PubMed]
| Control (n = 14) | Intervention (n = 14) | Total (n = 28) | p-Value | |
|---|---|---|---|---|
| Mean age, years (median, interquartile range) | 51.6 (54.5, 14) | 45(47, 23) | 48.3 (51.5, 22.5) | 0.26 |
| Age ≥ 65, n | 1 (7%) | 0 | 1 (4%) | 0.31 |
| Female | 10 (71%) | 9 (64%) | 19 (68%) | 0.69 |
| Marital Status | 0.86 | |||
| Married | 7 (50%) | 6 (43%) | 13 (46%) | |
| Living together | 2 (14%) | 3 (21%) | 5 (18%) | |
| Never married | 3 (21%) | 4 (29%) | 7 (25%) | |
| Divorced | 2 (14%) | 1 (7%) | 3 (11%) | |
| Employment Status | 0.59 | |||
| Employed | 13 (93%) | 12 (86%) | 25 (89%) | |
| Student | 0 (0%) | 1 (7%) | 1 (4%) | |
| Other | 1 (7%) | 1 (7%) | 2 (7%) | |
| Yearly Household Income | 0.73 | |||
| Below the average | 4 (29%) | 4 (29%) | 8 (29%) | |
| Around the average | 3 (21%) | 1 (7%) | 4 (14%) | |
| Above the average | 6 (43%) | 8 (57%) | 14 (50%) | |
| Unknown | 1 (7%) | 1 (7%) | 2 (7%) | |
| Health Status | ||||
| Hypertension | 2 (14%) | 1 (7%) | 3 (11%) | 0.54 |
| Hyperlipidemia | 2 (14%) | 3 (21%) | 5 (18%) | 0.62 |
| Type 2 diabetes | 0 (0%) | 1 (7%) | 1 (4%) | 0.31 |
| Control | Intervention | p-Value | M_W Score | |
|---|---|---|---|---|
| n = 14, Mean (SD) | n = 14, Mean (SD) | |||
| Approach strategies | ||||
| Positive reframing | 5.71 (1.44) | 5.43 (1.60) | 0.71 | 0.46 |
| Active coping | 5.79 (1.12) | 5.93 (1.54) | 0.63 | 0.55 |
| Planning | 5.36 (1.55) | 5.71 (1.14) | 0.55 | 0.57 |
| Emotional support | 4.71 (1.73) | 5.14 (1.75) | 0.55 | 0.57 |
| Use of informational support | 3.86 (1.99) | 4.50 (2.14) | 0.31 | 0.61 |
| Acceptance | 6.43 (1.16) | 6.57 (1.55) | 0.67 | 0.55 |
| Self-care | 4.64 (1.69) | 6.14 (1.66) | 0.03 | 0.74 |
| Overall approach strategies | 36.5 (6.28) | 39.43 (7.17) | 0.26 | |
| Avoidance strategies | ||||
| Self-distraction | 5.64 (1.45) | 5.57 (1.65) | 0.83 | 0.53 |
| Denial | 2.64 (0.84) | 2.42 (0.85) | 0.26 | 0.39 |
| Substance use | 2.29 (0.83) | 2.43 (1.16) | 0.87 | 0.51 |
| Behavioral disengagement | 2.14 (0.36) | 2.21 (0.43) | >0.90 | 0.54 |
| Venting | 4.29 (1.68) | 4.07 (1.59) | 0.79 | 0.47 |
| Self-blame | 2.79 (0.70) | 3.14 (1.41) | 0.77 | 0.52 |
| Overall avoidance strategies | 19.79 (3.68) | 19.86 (4.28) | 0.96 | |
| Neither approach nor avoidance | ||||
| Humor | 4.14 (1.88) | 4.29 (1.90) | 0.91 | 0.51 |
| Religion | 3.93 (1.81) | 3.64 (2.34) | 0.39 | 0.41 |
| Resiliency Level | Control, n (%) | Intervention, n (%) | Total, n (%) |
|---|---|---|---|
| Low | 4 (28.6%) | 1(7.1%) | 5 (17.8%) |
| Medium | 6 (42.8%) | 8 (57.1%) | 14 (50%) |
| High | 4 (28.6%) | 5 (35.8%) | 9 (32.2%) |
| Total | 14 (100%) | 14 (100%) | 28 (100%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silver, J.K.; Finkelstein, A.; Minezaki, K.; Parks, K.; Budd, M.A.; Tello, M.; Paganoni, S.; Tirosh, A.; Polak, R. The Impact of a Culinary Coaching Telemedicine Program on Home Cooking and Emotional Well-Being during the COVID-19 Pandemic. Nutrients 2021, 13, 2311. https://doi.org/10.3390/nu13072311
Silver JK, Finkelstein A, Minezaki K, Parks K, Budd MA, Tello M, Paganoni S, Tirosh A, Polak R. The Impact of a Culinary Coaching Telemedicine Program on Home Cooking and Emotional Well-Being during the COVID-19 Pandemic. Nutrients. 2021; 13(7):2311. https://doi.org/10.3390/nu13072311
Chicago/Turabian StyleSilver, Julie K., Adi Finkelstein, Kaya Minezaki, Kimberly Parks, Maggi A. Budd, Monique Tello, Sabrina Paganoni, Amir Tirosh, and Rani Polak. 2021. "The Impact of a Culinary Coaching Telemedicine Program on Home Cooking and Emotional Well-Being during the COVID-19 Pandemic" Nutrients 13, no. 7: 2311. https://doi.org/10.3390/nu13072311
APA StyleSilver, J. K., Finkelstein, A., Minezaki, K., Parks, K., Budd, M. A., Tello, M., Paganoni, S., Tirosh, A., & Polak, R. (2021). The Impact of a Culinary Coaching Telemedicine Program on Home Cooking and Emotional Well-Being during the COVID-19 Pandemic. Nutrients, 13(7), 2311. https://doi.org/10.3390/nu13072311