Evolution of Nutritional Status after Early Nutritional Management in COVID-19 Hospitalized Patients
Abstract
:1. Introduction
2. Materials & Methods
2.1. Study Population
2.2. Nutritional Assessment
2.3. Assessment of Severity of COVID-19
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wu, D.; Lewis, E.D.; Pae, M.; Meydani, S.N. Nutritional Modulation of Immune Function: Analysis of Evidence, Mechanisms, and Clinical Relevance. Front. Immunol. 2019, 9, 3160. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Short, K.; Kedzierska, K.; Van De Sandt, C.E. Back to the Future: Lessons Learned From the 1918 Influenza Pandemic. Front. Cell. Infect. Microbiol. 2018, 8, 343. [Google Scholar] [CrossRef] [PubMed]
- Moser, J.-A.; Galindo-Fraga, A.; Ortiz-Hernández, A.A.; Gu, W.; Hunsberger, S.; Galán-Herrera, J.; Guerrero, M.L.; Ruiz-Palacios, G.M.; Beigel, J.H. The La Red ILI 002 Study Group Underweight, overweight, and obesity as independent risk factors for hospitalization in adults and children from influenza and other respiratory viruses. Influ. Other Respir. Viruses 2019, 13, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, L.; Yan, S.; Yang, F.; Xiang, L.; Zhu, J.; Shen, B.; Gong, Z. Clinical characteristics of 25 death cases with COVID-19: A retrospective review of medical records in a single medical center, Wuhan, China. Int. J. Infect. Dis. 2020, 94, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Wei, C.; Liu, Y.; Li, Y.; Zhang, Y.; Zhong, M.; Meng, X. Evaluation of the nutritional status in patients with COVID-19. J. Clin. Biochem. Nutr. 2020, 67, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Du, X.; Liu, Y.; Chen, J.; Peng, L.; Cheng, Z.; Wang, H.H.; Luo, M.; Jin, Y.; Zhao, Y. Comparison of the Clinical Implications among Two Different Nutritional Indices in Hospitalized Patients with COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Pironi, L.; Sasdelli, A.S.; Ravaioli, F.; Baracco, B.; Battaiola, C.; Bocedi, G.; Brodosi, L.; Leoni, L.; Mari, G.A.; Musio, A. Malnutrition and nutritional therapy in patients with SARS-CoV-2 disease. Clin. Nutr. 2021, 40, 1330–1337. [Google Scholar] [CrossRef]
- Allard, L.; Ouedraogo, E.; Molleville, J.; Bihan, H.; Giroux-Leprieur, B.; Sutton, A.; Baudry, C.; Josse, C.; Didier, M.; Deutsch, D.; et al. Malnutrition: Percentage and Association with Prognosis in Patients Hospitalized for Coronavirus Disease 2019. Nutrients 2020, 12, 3679. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Bedock, D.; Lassen, P.B.; Mathian, A.; Moreau, P.; Couffignal, J.; Ciangura, C.; Poitou-Bernert, C.; Jeannin, A.-C.; Mosbah, H.; Fadlallah, J.; et al. Prevalence and severity of malnutrition in hospitalized COVID-19 patients. Clin. Nutr. ESPEN 2020, 40, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, E.; Ferguson, M.; Banks, M.; Batterham, M.; Bauer, J.; Capra, S.; Isenring, E. Malnutrition and poor food intake are associated with prolonged hospital stay, frequent readmissions, and greater in-hospital mortality: Results from the Nutrition Care Day Survey 2010. Clin. Nutr. 2013, 32, 737–745. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hudson, L.; Chittams, J.; Griffith, C.; Compher, C. Malnutrition Identified by Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition Is Associated With More 30-Day Readmissions, Greater Hospital Mortality, and Longer Hospital Stays: A Retrospective Analysis of Nutrition A. J. Parenter. Enter. Nutr. 2018, 42, 892–897. [Google Scholar] [CrossRef]
- Chan, K.S.; Mourtzakis, M.; Aronson Friedman, L.; Dinglas, V.D.; Hough, C.L.; Ely, E.W.; Morris, P.E.; Hopkins, R.O.; Needham, D.M. National Institutes of Health National Heart, Lung, and Blood Institute (NHLBI) Acute Respiratory Distress Syndrome (ARDS) Network. Evaluating Muscle Mass in Survivors of Acute Respiratory Distress Syndrome: A 1-Year Multicenter Longitudinal Study. Crit. Care Med. 2018, 46, 1238–1246. [Google Scholar] [CrossRef] [PubMed]
- Caccialanza, R.; Laviano, A.; Lobascio, F.; Montagna, E.; Bruno, R.; Ludovisi, S.; Corsico, A.G.; Di Sabatino, A.; Belliato, M.; Calvi, M.; et al. Early nutritional supplementation in non-critically ill patients hospitalized for the 2019 novel coronavirus disease (COVID-19): Rationale and feasibility of a shared pragmatic protocol. Nutrition 2020, 74, 110835. [Google Scholar] [CrossRef]
- Thibault, R.; Seguin, P.; Tamion, F.; Pichard, C.; Singer, P. Nutrition of the COVID-19 patient in the intensive care unit (ICU): A practical guidance. Crit. Care 2020, 24, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Thibault, R.; Quilliot, D.; Seguin, P.; Tamion, F.; Schneider, S.; Déchelotte, P. Stratégie de prise en charge nutritionnelle à l’hôpital au cours de l’épidémie virale Covid-19: Avis d’experts de la Société Francophone de Nutrition Clinique et Métabolisme (SFNCM) [Nutritional care at hospital during the Covid-19 viral epidemic: Expert opinion from the French-speaking Society for Clinical Nutrition and Metabolism (SFNCM)]. Nutr. Clin. Métab. 2020, 34, 97–104. [Google Scholar] [CrossRef]
- Thibault, R.; Coëffier, M.; Joly, F.; Bohé, J.; Schneider, S.M.; Déchelotte, P. How the Covid-19 epidemic is challenging our practice in clinical nutrition—feedback from the field. Eur. J. Clin. Nutr. 2021, 75, 407–416. [Google Scholar] [CrossRef]
- De Lorenzo, R.; Conte, C.; Lanzani, C.; Benedetti, F.; Roveri, L.; Mazza, M.G.; Brioni, E.; Giacalone, G.; Canti, V.; Sofia, V.; et al. Residual clinical damage after COVID-19: A retrospective and prospective observational cohort study. PLoS ONE 2020, 15. [Google Scholar] [CrossRef] [PubMed]
- Barazzoni, R.; Bischoff, S.C.; Breda, J.; Wickramasinghe, K.; Krznarić, Ž.; Nitzan, D.; Pirlich, M.; Singer, P. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin. Nutr. Edinb. Scotl. 2020, 39, 1631–1638. [Google Scholar] [CrossRef]
- Ciangura, C.; Bouillot, J.-L.; Lloret-Linares, C.; Poitou, C.; Veyrie, N.; Basdevant, A.; Oppert, J.-M. Dynamics of Change in Total and Regional Body Composition after Gastric Bypass in Obese Patients. Obesity 2010, 18, 760–765. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Tao, Z.-W.; Wang, L.; Yuan, M.-L.; Liu, K.; Zhou, L.; Wei, P.-F.; Deng, Y.; Liu, J.; Liu, H.-G.; et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin. Med. J. 2020, 133, 1032–1038. [Google Scholar] [CrossRef] [PubMed]
- Ranganathan, P.; Aggarwal, R.; Pramesh, C.S. Common pitfalls in statistical analysis: Odds versus risk. Perspect. Clin. Res. 2015, 6, 222–224. [Google Scholar] [CrossRef] [PubMed]
- Mechanick, J.I.; Carbone, S.; Dickerson, R.N.; Hernandez, B.J.D.; Hurt, R.T.; Irving, S.Y.; Li, D.Y.; McCarthy, M.S.; Mogensen, K.M.; Gautier, J.B.O.; et al. ASPEN COVID-19 Task Force on Nutrition Research. Clinical Nutrition Research and the COVID-19 Pandemic: A Scoping Review of the ASPEN COVID-19 Task Force on Nutrition Research. JPEN J. Parenter. Enter. Nutr. 2021, 45, 13–31. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Ruan, Q.; Yang, K.; Wang, W.; Jiang, L.; Song, J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020, 46, 846–848. [Google Scholar] [CrossRef] [Green Version]
- Zhang, P.; He, Z.; Yu, G.; Peng, D.; Feng, Y.; Ling, J.; Wang, Y.; Li, S.; Bian, Y. The modified NUTRIC score can be used for nutritional risk assessment as well as prognosis prediction in critically ill COVID-19 patients. Clin. Nutr. 2020, 40, 534–541. [Google Scholar] [CrossRef]
- Aghili, S.M.M.; Ebrahimpur, M.; Arjmand, B.; Shadman, Z.; Sani, M.P.; Qorbani, M.; Larijani, B.; Payab, M. Obesity in COVID-19 era, implications for mechanisms, comorbidities, and prognosis: A review and meta-analysis. Int. J. Obes. 2021, 45, 998–1016. [Google Scholar] [CrossRef]
- Lechien, J.R.; Chiesa-Estomba, C.M.; De Siati, D.R.; Horoi, M.; Le Bon, S.D.; Rodriguez, A.; Dequanter, D.; Blecic, S.; El Afia, F.; Distinguin, L.; et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): A multicenter European study. Eur. Arch. Otorhinolaryngol. 2020, 277, 2251–2261. [Google Scholar] [CrossRef]
- Fedele, D.; De Francesco, A.; Riso, S.; Collo, A. Obesity, malnutrition, and trace element deficiency in the coronavirus disease (COVID-19) pandemic: An overview. Nutrition 2021, 81, 111016. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [Green Version]
- Brugliera, L.; Spina, A.; Castellazzi, P.; Cimino, P.; Arcuri, P.; Negro, A.; Houdayer, E.; Alemanno, F.; Giordani, A.; Mortini, P.; et al. Nutritional management of COVID-19 patients in a rehabilitation unit. Eur. J. Clin. Nutr. 2020, 74, 860–863. [Google Scholar] [CrossRef] [PubMed]

| [All] | 0 | 1 | 2 | p | |
|---|---|---|---|---|---|
| n = 91 | n = 65 | n = 20 | n = 6 | Value | |
| At admission | |||||
| Age (years) | 57.7 (15.6) | 57.5 (14.4) | 54.4 (18.3) | 70.2 (14.9) | 0.09 |
| Male, n (%) | 55 (60.4) | 40 (61.5) | 12 (60.0) | 3 (50.0) | 0.87 |
| High blood pressure, n (%) | 46 (50.5) | 5 (53.8) | 8 (40.0) | 3 (50.0) | 0.55 |
| Diabetes, n (%) | 30 (33.0) | 24 (36.9) | 6 (30.0) | 0 (0.0) | 0.22 |
| Active smoking, n (%) | 4 (4.8) | 1 (1.6) | 3 (18.8) | 0 (0.0) | 0.05 |
| Chronic obstructive pulmonary disease, n (%) | 7 (7.7) | 4 (6.2) | 1 (5.0) | 2 (33.3) | 0.08 |
| Chronic kidney disease, n (%) | 16 (17.6) | 11 (16.9) | 4 (20.0) | 1 (16.7) | 0.89 |
| Chronic heart disease, n (%) | 22 (24.2) | 13 (20.0) | 6 (30.0) | 3 (50.0) | 0.15 |
| Weight at admission (kg) | 76.3 (17.3) | 77.8 (14.5) | 75.0 (21.5) | 64.3 (25.8) | 0.18 |
| Usual weight (kg) | 80.4 (18.0) | 80.9 (15.0) | 81.3 (21.8) | 71.0 (32.4) | 0.42 |
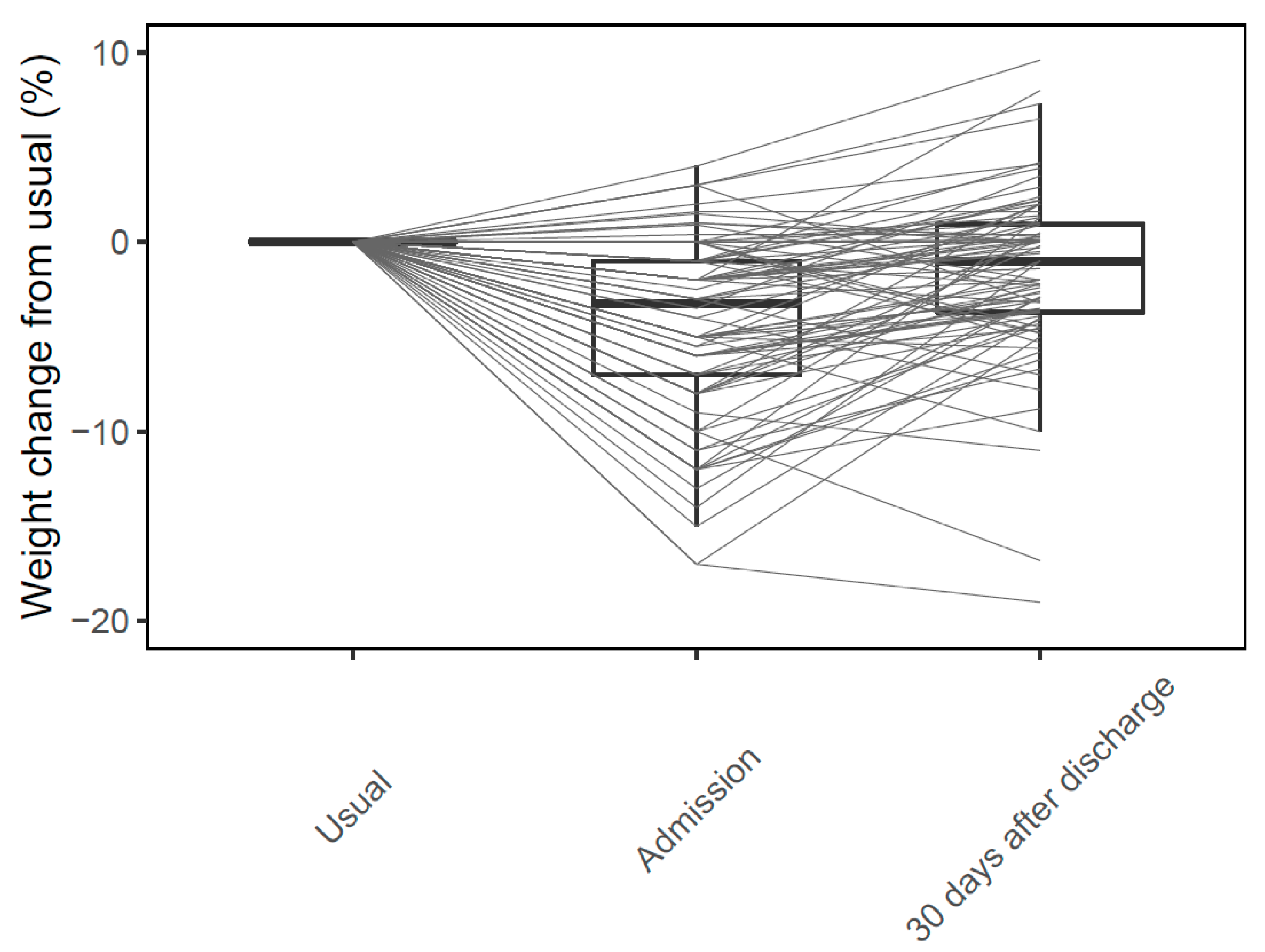
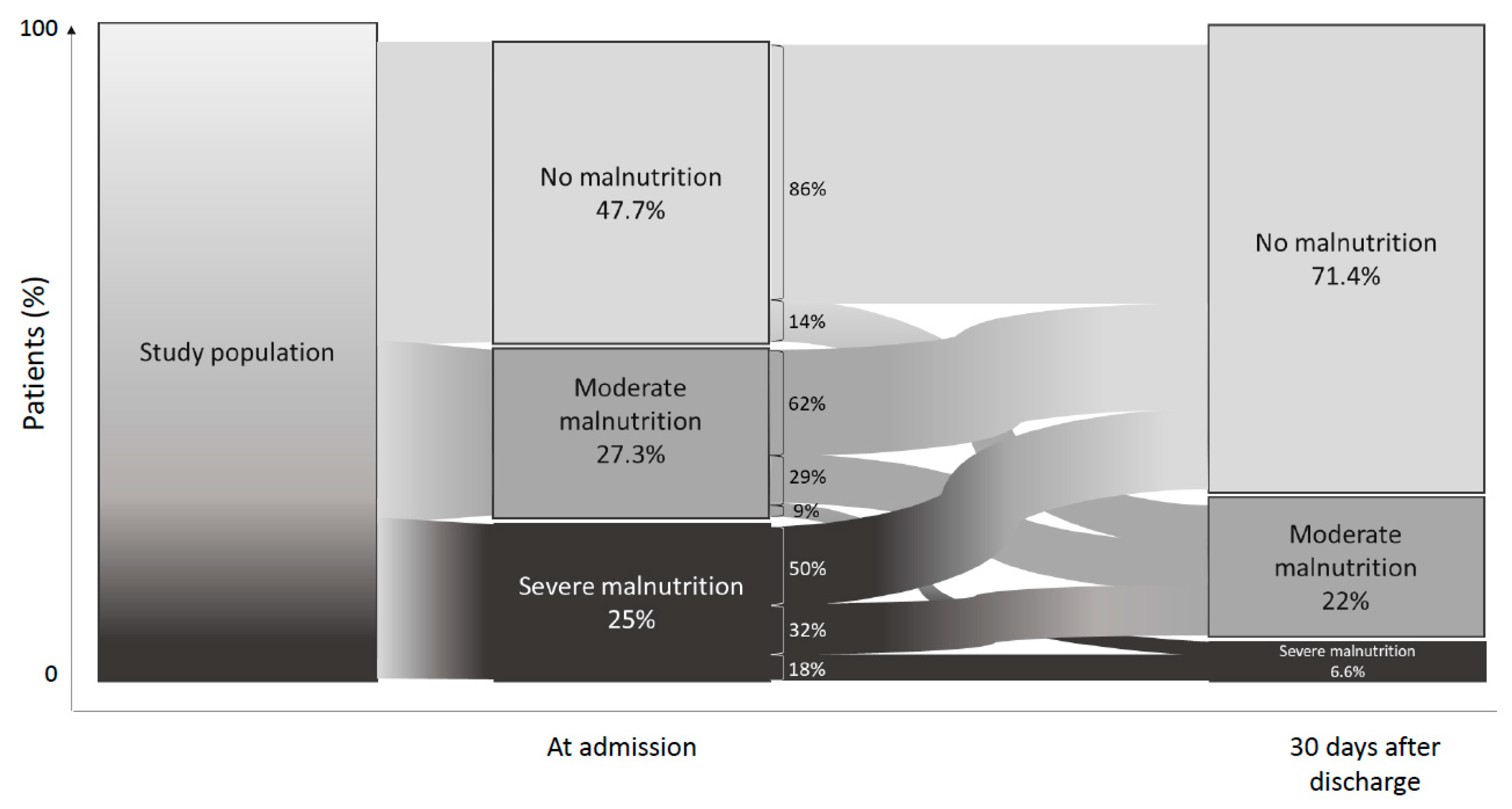
| Weight change from usual (%) | −5.4 (5.7) | −4.3 (5.3) | −8.0 (5.9) | −7.0 (7.6) | 0.03 |
| BMI (kg/m2) | 26.5 (5.1) | 26.7 (4.5) | 26.5 (6.0) | 24.1 (7.1) | 0.50 |
| Obesity, n (% BMI ≥ 30 kg/m2) | 21 (23.9) | 14 (22.6) | 6 (30.0) | 1 (16.7) | 0.83 |
| Albumin (g/L) | 30.3 (5.6) | 30.0 (5.7) | 30.8 (6.0) | 32.2 (1.7) | 0.62 |
| Transthyretin (g/L) | 0.1 (0.1) | 0.1 (0.1) | 0.2 (0.1) | 0.2 (0.1) | 0.05 |
| At 30 days after discharge | |||||
| Weight (kg) | 78.8 (17.4) | 81.1 (15.2) | 76.4 (19.5) | 62.4 (25.1) | 0.03 |
| Weight change from usual (%) | −1.8 (4.9) | 0.2 (3.7) | −5.7 (2.9) | −10.2 (6.3) | <0.01 |
| Weight change from admission (%) | 2.7 (4.3) | 3.6 (3.8) | 1.4 (5.0) | −2.0 (3.8) | <0.01 |
| BMI (kg/m2) | 27.5 (4.9) | 28.0 (4.5) | 27.0 (5.4) | 23.3 (6.5) | 0.07 |
| Obesity, n (% BMI ≥ 30 kg/m2) | 64 (71.1) | 46 (71.9) | 13 (65.0) | 5 (83.3) | 0.73 |
| Weight change from usual (kg) | −1.6 (4.4) | 0.1 (3.0) | −4.9 (3.0) | −8.6 (7.7) | <0.01 |
| Muscle mass (kg) | 55.0 (12.3) | 55.9 (12.3) | 53.2 (11.1) | 49.4 (18.5) | 0.45 |
| Handgrip strength (kg) | 33.4 (19.6) | 35.2 (20.9) | 28.3 (10.1) | 28.1 (30.7) | 0.35 |
| Albumin (g/L) | 42.1 (4.7) | 42.2 (5.1) | 41.4 (3.6) | 43.0 (4.7) | 0.75 |
| Transthyretin (g/L) | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.2) | 0.3 (0.1) | 0.64 |
| COVID parameters | |||||
| Invasive ventilation, n (%) | 7 (7.9) | 2 (3.1) | 4 (21.1) | 1 (20.0) | 0.02 |
| Non-invasive ventilation, n (%) | 20 (22.2) | 11 (16.9) | 7 (36.8) | 2 (33.3) | 0.11 |
| O2 over 5 L/min during COVID, n (%) | 7 (7.7) | 1 (1.5) | 5 (25.0) | 1 (16.7) | <0.01 |
| Intensive Care Unit during COVID, n (%) | 30 (33.0) | 18 (27.7) | 10 (50.0) | 2 (33.3) | 0.16 |
| CT pulmonary infiltrate over 50%, n (%) | 9 (11.5) | 7 (12.5) | 1 (5.9) | 1 (20.0) | 0.45 |
| Leucocytes (G/L) | 6.9 (3.9) | 6.2 (2.9) | 9.3 (6.1) | 7.2 (1.8) | 0.01 |
| Lymphocytes (G/L) | 1.1 (0.5) | 1.0 (0.5) | 1.1 (0.6) | 1.4 (0.2) | 0.25 |
| Polynuclear Neutrophils (G/L) | 5.3 (3.8) | 4.6 (2.6) | 8.1 (6.7) | 5.2 (1.9) | 0.01 |
| CRP (mg/L) | 91.1 (73.3) | 100.3 (77.5) | 63.5 (50.2) | 61.2 (56.4) | 0.16 |
| D dimers (µg/L) | 1410.4 (2035.1) | 1607.2 (2291.4) | 795.0 (818.7) | 986.7 (371.0) | 0.45 |
| Baseline Predictors of Malnutrition at Day 30 | OR [CI 95%] | p Value |
|---|---|---|
| At admission | ||
| Age | 1.0 [0.9–1.0] | 0.894 |
| Male | 0.9 [0.3–2.2] | 0.735 |
| High blood pressure | 0.6 [0.2–1.6] | 0.322 |
| Diabetes | 0.5 [0.2–1.4] | 0.209 |
| Active smoking | 9.5 [1.1–197.8] | 0.058 |
| Chronic obstructive pulmonary disease | 2.0 [0.4–9.7] | 0.391 |
| Chronic kidney disease | 1.2 [0.3–3.6] | 0.794 |
| Chronic heart disease | 2.1 [0.8–5.8] | 0.146 |
| Weight at admission | 1.0 [0.9–1.0] | 0.197 |
| Usual weight | 1.0 [0.9–1.0] | 0.634 |
| Weight change from usual | 1.1 [1.0–1.2] | 0.013 |
| BMI | 1.0 [0.9–1.1] | 0.524 |
| Obesity (BMI ≥ 30 kg/m2) | 1.3 [0.4–3.6] | 0.663 |
| Albumin | 1.0 [1.0–1.1] | 0.408 |
| Transthyretin | 1.1 [1.0–1.2] | 0.061 |
| COVID parameters | ||
| Invasive ventilation | 8.3 [1.6–61.2] | 0.016 |
| Non-invasive ventilation | 2.8 [1.0–7.9] | 0.056 |
| O2 over 5 L/min during COVID | 3.2 [1.2–8.9] | 0.021 |
| Intensive Care Unit during COVID | 2.2 [0.9–5.8] | 0.094 |
| CT pulmonary infiltrate over 50% | 0.7 [1.0–3.2] | 0.673 |
| Leucocytes | 1.2 [1.0–1.4] | 0.017 |
| Lymphocytes | 1.9 [0.7–5.3] | 0.190 |
| Polynuclear Neutrophils | 1.2 [1.0–1.4] | 0.024 |
| CRP | 1.0 [0.9–1.0] | 0.060 |
| D dimers | 1.0 [0.9–1.0] | 0.181 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bedock, D.; Couffignal, J.; Bel Lassen, P.; Soares, L.; Mathian, A.; Fadlallah, J.P.; Amoura, Z.; Oppert, J.-M.; Faucher, P. Evolution of Nutritional Status after Early Nutritional Management in COVID-19 Hospitalized Patients. Nutrients 2021, 13, 2276. https://doi.org/10.3390/nu13072276
Bedock D, Couffignal J, Bel Lassen P, Soares L, Mathian A, Fadlallah JP, Amoura Z, Oppert J-M, Faucher P. Evolution of Nutritional Status after Early Nutritional Management in COVID-19 Hospitalized Patients. Nutrients. 2021; 13(7):2276. https://doi.org/10.3390/nu13072276
Chicago/Turabian StyleBedock, Dorothée, Julie Couffignal, Pierre Bel Lassen, Leila Soares, Alexis Mathian, Jehane P. Fadlallah, Zahir Amoura, Jean-Michel Oppert, and Pauline Faucher. 2021. "Evolution of Nutritional Status after Early Nutritional Management in COVID-19 Hospitalized Patients" Nutrients 13, no. 7: 2276. https://doi.org/10.3390/nu13072276
APA StyleBedock, D., Couffignal, J., Bel Lassen, P., Soares, L., Mathian, A., Fadlallah, J. P., Amoura, Z., Oppert, J.-M., & Faucher, P. (2021). Evolution of Nutritional Status after Early Nutritional Management in COVID-19 Hospitalized Patients. Nutrients, 13(7), 2276. https://doi.org/10.3390/nu13072276







