Pre-Gestational Consumption of Ultra-Processed Foods and Risk of Gestational Diabetes in a Mediterranean Cohort. The SUN Project
Abstract
:1. Introduction
2. Materials and Methods
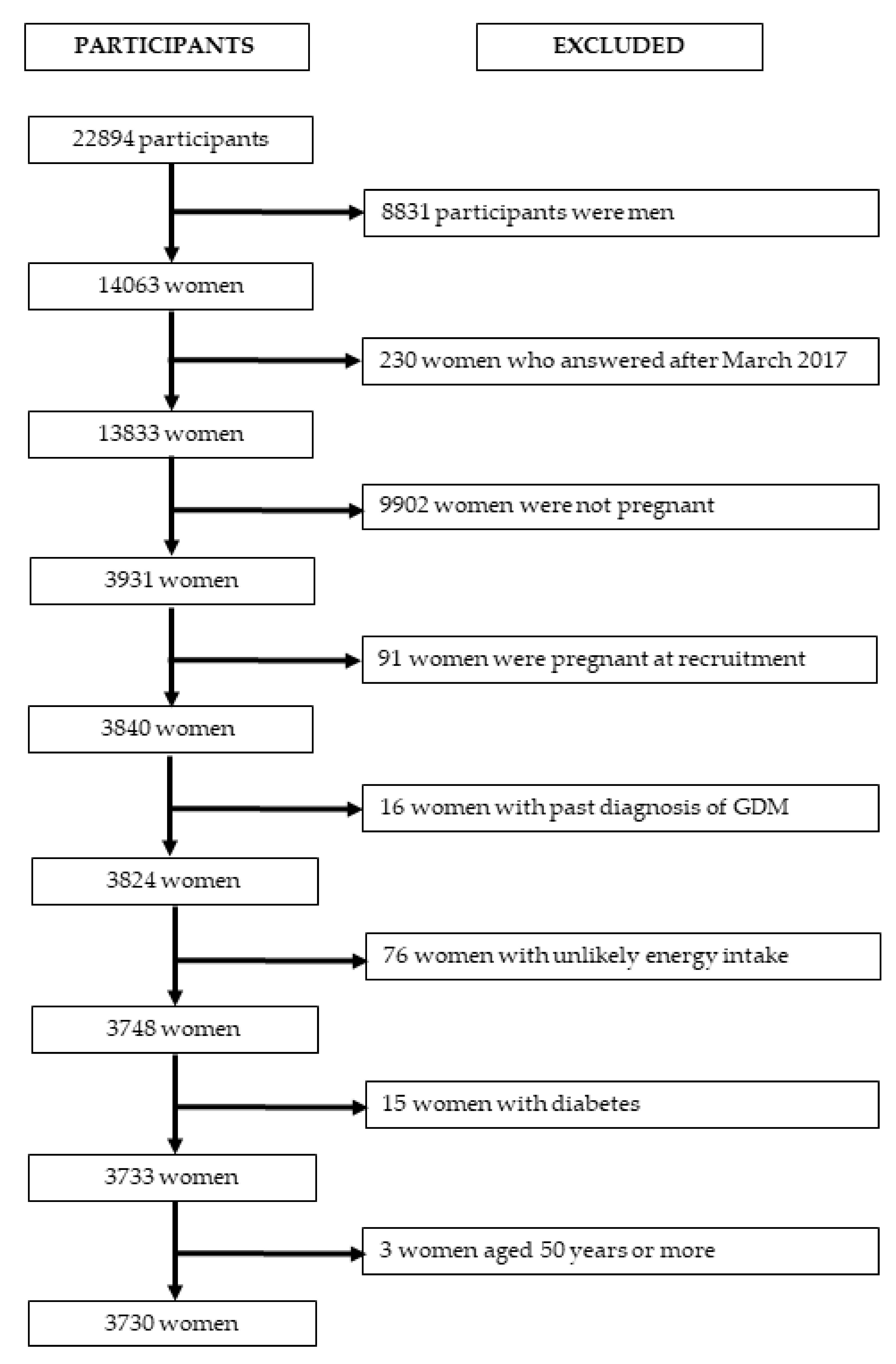
2.1. Study Design and Participants
2.2. Exposure Assessment
2.3. Outcome Assessment
2.4. Covariates Assessment
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Diabetes Association (ADA). Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2018. Diabetes Care 2018, 41, S13–S27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wendland, E.M.; Torloni, M.R.; Falavigna, M.; Trujillo, J.; Dode, M.A.; Campos, M.A.; Duncan, B.B.; Schmidt, M.I. Gestational diabetes and pregnancy outcomes--a systematic review of the World Health Organization (WHO) and the International Association of Diabetes in Pregnancy Study Groups (IADPSG) diagnostic criteria. BMC Pregnancy Childbirth 2012, 12, 23. [Google Scholar] [CrossRef] [Green Version]
- Farahvar, S.; Walfisch, A.; Sheiner, E. Gestational diabetes risk factors and long-term consequences for both mother and offspring: A literature review. Expert Rev. Endocrinol. Metab. 2019, 14, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Eades, C.E.; Cameron, D.M.; Evans, J.M.M. Prevalence of gestational diabetes mellitus in Europe: A meta-analysis. Diabetes Res. Clin. Pract. 2017, 129, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Poston, L.; Caleyachetty, R.; Cnattingius, S.; Corvalan, C.; Uauy, R.; Herring, S.; Gillman, M.W. Preconceptional and maternal obesity: Epidemiology and health consequences. Lancet Diabetes Endocrinol. 2016, 4, 1025–1036. [Google Scholar] [CrossRef]
- Durnwald, C. Gestational diabetes: Linking epidemiology, excessive gestational weight gain, adverse pregnancy outcomes, and future metabolic syndrome. Semin Perinatol 2015, 39, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Rawal, S.; Chong, Y.S. Risk factors for gestational diabetes: Is prevention possible? Diabetologia 2016, 59, 1385–1390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raghavan, R.; Dreibelbis, C.; Kingshipp, B.L.; Wong, Y.P.; Abrams, B.; Gernand, A.D.; Rasmussen, K.M.; Siega-Riz, A.M.; Stang, J.; Casavale, K.O.; et al. Dietary patterns before and during pregnancy and maternal outcomes: A systematic review. Am. J. Clin. Nutr. 2019, 109, 705s–728s. [Google Scholar] [CrossRef] [PubMed]
- Hassani Zadeh, S.; Boffetta, P.; Hosseinzadeh, M. Dietary patterns and risk of gestational diabetes mellitus: A systematic review and meta-analysis of cohort studies. Clin. Nutr. ESPEN 2020, 36, 1–9. [Google Scholar] [CrossRef]
- Rico-Campa, A.; Martinez-Gonzalez, M.A.; Alvarez-Alvarez, I.; Mendonca, R.D.; de la Fuente-Arrillaga, C.; Gomez-Donoso, C.; Bes-Rastrollo, M. Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. BMJ 2019, 365, l1949. [Google Scholar] [CrossRef] [Green Version]
- Rauber, F.; Steele, E.M.; Louzada, M.L.d.C.; Millett, C.; Monteiro, C.A.; Levy, R.B. Ultra-processed food consumption and indicators of obesity in the United Kingdom population (2008–2016). PLoS ONE 2020, 15, e0232676. [Google Scholar] [CrossRef] [PubMed]
- Martínez Steele, E.; Baraldi, L.G.; Louzada, M.L.; Moubarac, J.C.; Mozaffarian, D.; Monteiro, C.A. Ultra-processed foods and added sugars in the US diet: Evidence from a nationally representative cross-sectional study. BMJ Open 2016, 6, e009892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moubarac, J.C.; Batal, M.; Louzada, M.L.; Martinez Steele, E.; Monteiro, C.A. Consumption of ultra-processed foods predicts diet quality in Canada. Appetite 2017, 108, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Mendonca, R.D.; Pimenta, A.M.; Gea, A.; de la Fuente-Arrillaga, C.; Martinez-Gonzalez, M.A.; Lopes, A.C.; Bes-Rastrollo, M. Ultraprocessed food consumption and risk of overweight and obesity: The University of Navarra Follow-Up (SUN) cohort study. Am. J. Clin. Nutr. 2016, 104, 1433–1440. [Google Scholar] [CrossRef] [PubMed]
- Levy, R.B.; Rauber, F.; Chang, K.; Louzada, M.; Monteiro, C.A.; Millett, C.; Vamos, E.P. Ultra-processed food consumption and type 2 diabetes incidence: A prospective cohort study. Clin. Nutr. 2020. [Google Scholar] [CrossRef]
- Srour, B.; Fezeu, L.K.; Kesse-Guyot, E.; Alles, B.; Debras, C.; Druesne-Pecollo, N.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultraprocessed Food Consumption and Risk of Type 2 Diabetes Among Participants of the NutriNet-Sante Prospective Cohort. JAMA Intern. Med. 2019. [Google Scholar] [CrossRef]
- Llavero-Valero, M.; Escalada-San Martín, J.; Martínez-González, M.A.; Basterra-Gortari, F.J.; de la Fuente-Arrillaga, C.; Bes-Rastrollo, M. Ultra-processed foods and type-2 diabetes risk in the SUN project: A prospective cohort study. Clin. Nutr. 2021, 40, 2817–2824. [Google Scholar] [CrossRef]
- Hall, K.D.; Ayuketah, A.; Brychta, R.; Cai, H.; Cassimatis, T.; Chen, K.Y.; Chung, S.T.; Costa, E.; Courville, A.; Darcey, V.; et al. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab. 2019, 30, 67–77. [Google Scholar] [CrossRef] [Green Version]
- Konieczna, J.; Morey, M.; Abete, I.; Bes-Rastrollo, M.; Ruiz-Canela, M.; Vioque, J.; Gonzalez-Palacios, S.; Daimiel, L.; Salas-Salvadó, J.; Fiol, M.; et al. Contribution of ultra-processed foods in visceral fat deposition and other adiposity indicators: Prospective analysis nested in the PREDIMED-Plus trial. Clin. Nutr. 2021. [Google Scholar] [CrossRef]
- Neeland, I.J.; Ross, R.; Després, J.P.; Matsuzawa, Y.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: A position statement. Lancet Diabetes Endocrinol. 2019, 7, 715–725. [Google Scholar] [CrossRef]
- Fardet, A. Minimally processed foods are more satiating and less hyperglycemic than ultra-processed foods: A preliminary study with 98 ready-to-eat foods. Food Funct 2016, 7, 2338–2346. [Google Scholar] [CrossRef]
- Bhattacharyya, S.; I, O.S.; Katyal, S.; Unterman, T.; Tobacman, J.K. Exposure to the common food additive carrageenan leads to glucose intolerance, insulin resistance and inhibition of insulin signalling in HepG2 cells and C57BL/6J mice. Diabetologia 2012, 55, 194–203. [Google Scholar] [CrossRef]
- Buchanan, T.A.; Xiang, A.H. Gestational diabetes mellitus. J. Clin. Investig. 2005, 115, 485–491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silva, C.F.M.; Saunders, C.; Peres, W.; Folino, B.; Kamel, T.; Dos Santos, M.S.; Padilha, P. Effect of ultra-processed foods consumption on glycemic control and gestational weight gain in pregnant with pregestational diabetes mellitus using carbohydrate counting. PeerJ 2021, 9, e10514. [Google Scholar] [CrossRef]
- Martin-Moreno, J.M.; Boyle, P.; Gorgojo, L.; Maisonneuve, P.; Fernandez-Rodriguez, J.C.; Salvini, S.; Willett, W.C. Development and validation of a food frequency questionnaire in Spain. Int. J. Epidemiol. 1993, 22, 512–519. [Google Scholar] [CrossRef] [PubMed]
- de la Fuente-Arrillaga, C.; Ruiz, Z.V.; Bes-Rastrollo, M.; Sampson, L.; Martinez-Gonzalez, M.A. Reproducibility of an FFQ validated in Spain. Public Health Nutr. 2010, 13, 1364–1372. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Ballart, J.D.; Pinol, J.L.; Zazpe, I.; Corella, D.; Carrasco, P.; Toledo, E.; Perez-Bauer, M.; Martinez-Gonzalez, M.A.; Salas-Salvado, J.; Martin-Moreno, J.M. Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br. J. Nutr. 2010, 103, 1808–1816. [Google Scholar] [CrossRef] [Green Version]
- Monteiro, C.A.; Cannon, G.; Levy, R.; Moubarac, J.-C.; Jaime, P.; Martins, A.P.; Canella, D.; Louzada, M.; Parra, D. NOVA. The star shines bright. World Nutr. 2016, 7, 28–38. [Google Scholar]
- Willett, W.C.; Howe, G.R.; Kushi, L.H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 1997, 65, 1220S–1228S; discussion 1229S–1231S. [Google Scholar] [CrossRef]
- Grupo Espanol de Diabetes y Embarazo (GEDE). Guía asistencial de diabetes mellitus y embarazo (3a edicion) (Spanish Group of Diabetes and Pregnancy. Guideline for diabetes mellitus and pregnancy (3rd ed.)). Av en Diabetol. 2006, 22, 73–87. [Google Scholar]
- Metzger, B.E. Summary and Recommendations of the Third International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes 1991, 40, 197. [Google Scholar] [CrossRef] [PubMed]
- Bes-Rastrollo, M.; Pérez Valdivieso, J.R.; Sánchez-Villegas, A.; Alonso, A.; Martínez-González, M.A. Validación del peso e índice de masa corporal auto-declarados de los participantes de una cohorte de graduados universitarios. Rev. Esp. Obes. 2005, 3, 183–189. [Google Scholar]
- Martinez-Gonzalez, M.A.; Lopez-Fontana, C.; Varo, J.J.; Sanchez-Villegas, A.; Martinez, J.A. Validation of the Spanish version of the physical activity questionnaire used in the Nurses’ Health Study and the Health Professionals’ Follow-up Study. Public Health Nutr. 2005, 8, 920–927. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dominguez, L.J.; Martínez-González, M.A.; Basterra-Gortari, F.J.; Gea, A.; Barbagallo, M.; Bes-Rastrollo, M. Fast food consumption and gestational diabetes incidence in the SUN project. PLoS ONE 2014, 9, e106627. [Google Scholar] [CrossRef] [Green Version]
- Donazar-Ezcurra, M.; Lopez-Del Burgo, C.; Martinez-Gonzalez, M.A.; Dominguez, L.J.; Basterra-Gortari, F.J.; de Irala, J.; Bes-Rastrollo, M. Association of the Dietary-Based Diabetes-Risk Score (DDS) with the risk of gestational diabetes mellitus in the Seguimiento Universidad de Navarra (SUN) project. Br. J. Nutr. 2019, 122, 800–807. [Google Scholar] [CrossRef]
- Donazar-Ezcurra, M.; Lopez-Del Burgo, C.; Martinez-Gonzalez, M.A.; Basterra-Gortari, F.J.; de Irala, J.; Bes-Rastrollo, M. Soft drink consumption and gestational diabetes risk in the SUN project. Clin. Nutr. 2018, 37, 638–645. [Google Scholar] [CrossRef] [PubMed]
- Donazar-Ezcurra, M.; Lopez-Del Burgo, C.; Martinez-Gonzalez, M.A.; Basterra-Gortari, F.J.; de Irala, J.; Bes-Rastrollo, M. Pre-pregnancy adherences to empirically derived dietary patterns and gestational diabetes risk in a Mediterranean cohort: The Seguimiento Universidad de Navarra (SUN) project. Br. J. Nutr. 2017, 118, 715–721. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mari-Sanchis, A.; Diaz-Jurado, G.; Basterra-Gortari, F.J.; de la Fuente-Arrillaga, C.; Martinez-Gonzalez, M.A.; Bes-Rastrollo, M. Association between pre-pregnancy consumption of meat, iron intake, and the risk of gestational diabetes: The SUN project. Eur. J. Nutr. 2018, 57, 939–949. [Google Scholar] [CrossRef]
- Hernán, M.A.; Hernández-Díaz, S.; Werler, M.M.; Mitchell, A.A. Causal knowledge as a prerequisite for confounding evaluation: An application to birth defects epidemiology. Am. J. Epidemiol. 2002, 155, 176–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, C.; Schulze, M.B.; Solomon, C.G.; Hu, F.B. A prospective study of dietary patterns, meat intake and the risk of gestational diabetes mellitus. Diabetologia 2006, 49, 2604–2613. [Google Scholar] [CrossRef] [Green Version]
- Mendonca, R.D.; Lopes, A.C.; Pimenta, A.M.; Gea, A.; Martinez-Gonzalez, M.A.; Bes-Rastrollo, M. Ultra-Processed Food Consumption and the Incidence of Hypertension in a Mediterranean Cohort: The Seguimiento Universidad de Navarra Project. Am. J. Hypertens. 2017, 30, 358–366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Srour, B.; Fezeu, L.K.; Kesse-Guyot, E.; Alles, B.; Mejean, C.; Andrianasolo, R.M.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultra-processed food intake and risk of cardiovascular disease: Prospective cohort study (NutriNet-Sante). BMJ 2019, 365, l1451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fiolet, T.; Srour, B.; Sellem, L.; Kesse-Guyot, E.; Alles, B.; Mejean, C.; Deschasaux, M.; Fassier, P.; Latino-Martel, P.; Beslay, M.; et al. Consumption of ultra-processed foods and cancer risk: Results from NutriNet-Sante prospective cohort. BMJ 2018, 360, k322. [Google Scholar] [CrossRef] [Green Version]
- Sartorelli, D.S.; Crivellenti, L.C.; Zuccolotto, D.C.C.; Franco, L.J. Relationship between minimally and ultra-processed food intake during pregnancy with obesity and gestational diabetes mellitus. Cad Saude Publica 2019, 35, e00049318. [Google Scholar] [CrossRef] [PubMed]
- Challis, J.R.; Lockwood, C.J.; Myatt, L.; Norman, J.E.; Strauss, J.F.; Petraglia, F. Inflammation and Pregnancy. Reprod. Sci. 2009, 16, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Volpe, L.; Di Cianni, G.; Lencioni, C.; Cuccuru, I.; Benzi, L.; Del Prato, S. Gestational diabetes, inflammation, and late vascular disease. J. Endocrinol. Investig. 2007, 30, 873–879. [Google Scholar] [CrossRef]
- McIntyre, H.D.; Catalano, P.; Zhang, C.; Desoye, G.; Mathiesen, E.R.; Damm, P. Gestational diabetes mellitus. Nat. Rev. Dis. Primers 2019, 5, 47. [Google Scholar] [CrossRef]
- Plows, J.F.; Stanley, J.L.; Baker, P.N.; Reynolds, C.M.; Vickers, M.H. The Pathophysiology of Gestational Diabetes Mellitus. Int. J. Mol. Sci. 2018, 19, 3342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barazzoni, R.; Deutz, N.E.P.; Biolo, G.; Bischoff, S.; Boirie, Y.; Cederholm, T.; Cuerda, C.; Delzenne, N.; Leon Sanz, M.; Ljungqvist, O.; et al. Carbohydrates and insulin resistance in clinical nutrition: Recommendations from the ESPEN expert group. Clin. Nutr. 2017, 36, 355–363. [Google Scholar] [CrossRef] [Green Version]
- Macdonald, I.A. A review of recent evidence relating to sugars, insulin resistance and diabetes. Eur. J. Nutr. 2016, 55, 17–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boden, G. Effects of free fatty acids (FFA) on glucose metabolism: Significance for insulin resistance and type 2 diabetes. Exp. Clin. Endocrinol. Diabetes 2003, 111, 121–124. [Google Scholar] [CrossRef] [PubMed]
- Silva, C.A.; Santos, I.D.S.; Shivappa, N.; Hebert, J.R.; Crivellenti, L.C.; Sartorelli, D.S. The role of food processing in the inflammatory potential of diet during pregnancy. Rev. Saude Publica 2019, 53, 113. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shoelson, S.E.; Lee, J.; Goldfine, A.B. Inflammation and insulin resistance. J. Clin. Investig. 2006, 116, 1793–1801. [Google Scholar] [CrossRef]
- Lao, T.T.; Ho, L.F. Impact of iron deficiency anemia on prevalence of gestational diabetes mellitus. Diabetes Care 2004, 27, 650–656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kataria, Y.; Wu, Y.; Horskjaer, P.H.; Mandrup-Poulsen, T.; Ellervik, C. Iron Status and Gestational Diabetes-A Meta-Analysis. Nutrients 2018, 10, 621. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dietrich, S.; Jacobs, S.; Zheng, J.S.; Meidtner, K.; Schwingshackl, L.; Schulze, M.B. Gene-lifestyle interaction on risk of type 2 diabetes: A systematic review. Obes. Rev. 2019, 20, 1557–1571. [Google Scholar] [CrossRef] [PubMed]
- Bertoli, S.; Leone, A.; Battezzati, A. Human Bisphenol A Exposure and the “Diabesity Phenotype”. Dose Response 2015, 13, 1559325815599173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rolfo, A.; Nuzzo, A.M.; De Amicis, R.; Moretti, L.; Bertoli, S.; Leone, A. Fetal-Maternal Exposure to Endocrine Disruptors: Correlation with Diet Intake and Pregnancy Outcomes. Nutrients 2020, 12, 1744. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, R.M.; Ferguson, K.K.; Sheppard, L.; James-Todd, T.; Butts, S.; Chandrasekaran, S.; Swan, S.H.; Barrett, E.S.; Nguyen, R.; Bush, N.; et al. Maternal urinary phthalate metabolites in relation to gestational diabetes and glucose intolerance during pregnancy. Environ. Int. 2019, 123, 588–596. [Google Scholar] [CrossRef]
- Fisher, B.G.; Frederiksen, H.; Andersson, A.M.; Juul, A.; Thankamony, A.; Ong, K.K.; Dunger, D.B.; Hughes, I.A.; Acerini, C.L. Serum Phthalate and Triclosan Levels Have Opposing Associations With Risk Factors for Gestational Diabetes Mellitus. Front. Endocrinol. 2018, 9, 99. [Google Scholar] [CrossRef]
- Lin, C.Y.; Lin, Y.C.; Kuo, H.K.; Hwang, J.J.; Lin, J.L.; Chen, P.C.; Lin, L.Y. Association among acrylamide, blood insulin, and insulin resistance in adults. Diabetes Care 2009, 32, 2206–2211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feroe, A.G.; Attanasio, R.; Scinicariello, F. Acrolein metabolites, diabetes and insulin resistance. Environ. Res. 2016, 148, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Szoke, E.; Shrayyef, M.Z.; Messing, S.; Woerle, H.J.; van Haeften, T.W.; Meyer, C.; Mitrakou, A.; Pimenta, W.; Gerich, J.E. Effect of aging on glucose homeostasis: Accelerated deterioration of beta-cell function in individuals with impaired glucose tolerance. Diabetes Care 2008, 31, 539–543. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michaud, M.; Balardy, L.; Moulis, G.; Gaudin, C.; Peyrot, C.; Vellas, B.; Cesari, M.; Nourhashemi, F. Proinflammatory cytokines, aging, and age-related diseases. J. Am. Med. Dir. Assoc. 2013, 14, 877–882. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Gonzalez, M.A. The SUN cohort study (Seguimiento University of Navarra). Public Health Nutr. 2006, 9, 127–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rifas-Shiman, S.L.; Rich-Edwards, J.W.; Willett, W.C.; Kleinman, K.P.; Oken, E.; Gillman, M.W. Changes in dietary intake from the first to the second trimester of pregnancy. Paediatr. Perinat. Epidemiol. 2006, 20, 35–42. [Google Scholar] [CrossRef] [Green Version]
- Gabriel da Silva, L.B.; Rosado, E.L.; de Carvalho Padilha, P.; Dias, J.R.; Moreira, T.M.; de Paula, T.P.; de Barros, D.C.; Saunders, C. Food intake of women with gestational diabetes mellitus, in accordance with two methods of dietary guidance: A randomised controlled clinical trial. Br. J. Nutr. 2019, 121, 82–92. [Google Scholar] [CrossRef]
Unprocessed or minimally processed foods
|
Processed culinary ingredients
|
Processed foods
|
Ultra-processed foods
|
| Tertiles of Energy-Adjusted Ultra-Processed Food Consumption (servings/day) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Tertile 1 | Tertile 2 | Tertile 3 | ||||||||
| <3.3 | 3.3–4.5 | >4.5 | ||||||||
| (n = 1244) | (n = 1243) | (n = 1243) | ||||||||
| P25 | P50 | P75 | P25 | P50 | P75 | P25 | P50 | P75 | p-Value | |
| Age (years) | 25 | 28 | 32 | 25 | 27 | 31 | 24 | 27 | 31 | <0.001 |
| BMI (kg/m2) | 19.5 | 20.6 | 22.3 | 19.6 | 20.8 | 22.4 | 19.9 | 21.3 | 23.1 | <0.001 |
| Physical activity (METs/day) | 4.6 | 14.7 | 29.3 | 3.4 | 13.7 | 26.7 | 3.3 | 13.3 | 26.2 | 0.005 |
| Energy (kcal/day) | 2070 | 2494 | 3019 | 1871 | 2265 | 2728 | 2012 | 2427 | 3005 | <0.001 |
| Vegetables (servings/day) | 1.8 | 2.5 | 3.5 | 1.4 | 2 | 2.9 | 1.3 | 2 | 2.9 | <0.001 |
| Fruit (servings/day) | 1.5 | 2.5 | 4 | 1.1 | 1.8 | 2.9 | 0.9 | 1.7 | 2.8 | <0.001 |
| Nuts (servings/day) | 0.5 | 0.9 | 1.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 1 | <0.001 |
| Red and processed meat (servings/day) | 1.6 | 2.3 | 3.1 | 1.7 | 2.3 | 3.1 | 1.8 | 2.4 | 3.3 | 0.005 |
| Fish (servings/week) | 3.4 | 4.9 | 7.4 | 2.9 | 4.3 | 6.3 | 2.9 | 3.9 | 6 | <0.001 |
| Cereals (servings/day) | 1.2 | 1.7 | 2.8 | 1 | 1.4 | 2.2 | 1 | 1.5 | 2.4 | <0.001 |
| Legumes (servings/week) | 1.9 | 2.5 | 3.5 | 1.5 | 2.4 | 3 | 1.4 | 2 | 3 | <0.001 |
| Milk and dairy products (servings/day) | 2.3 | 3.3 | 4.5 | 2 | 2.9 | 4.1 | 2.1 | 3.1 | 4.3 | <0.001 |
| Olive oil (g/day) | 10.7 | 25.2 | 29.5 | 8.9 | 12.1 | 25.8 | 9.5 | 13.2 | 26 | <0.001 |
| Alcohol (g/day) | 0.6 | 2.1 | 4.5 | 0.6 | 2.1 | 4.9 | 0.6 | 2.2 | 6.1 | 0.086 |
| Ultra-processed foods (servings/day) | 2.1 | 2.7 | 3 | 3.6 | 3.9 | 4.2 | 4.9 | 5.5 | 6.5 | <0.001 |
| Ultra-processed foods/energy (%) | 17.4 | 22.1 | 26.6 | 25.9 | 30.7 | 35.2 | 29.9 | 36.3 | 42.6 | <0.001 |
| N | % | N | % | N | % | |||||
| Year of entrance in the cohort | 0.032 | |||||||||
| 1999–2000 | 339 | 27.3 | 370 | 29.8 | 338 | 27.2 | ||||
| 2001–2002 | 162 | 13 | 163 | 13.1 | 181 | 14.6 | ||||
| 2003–2004 | 210 | 16.9 | 229 | 18.4 | 258 | 20.8 | ||||
| 2005–2007 | 267 | 21.5 | 268 | 21.6 | 252 | 20.3 | ||||
| 2008–2017 | 266 | 21.4 | 213 | 17.1 | 214 | 17.2 | ||||
| Education | 0.019 | |||||||||
| Diploma | 554 | 44.5 | 493 | 39.7 | 487 | 39.2 | ||||
| Bachelor | 634 | 51 | 693 | 55.8 | 711 | 57.2 | ||||
| Postgraduate | 56 | 4.5 | 57 | 4.6 | 45 | 3.6 | ||||
| Smoking status | <0.001 | |||||||||
| Never | 755 | 60.7 | 724 | 58.2 | 640 | 51.5 | ||||
| Current | 273 | 21.9 | 294 | 23.7 | 367 | 29.5 | ||||
| Former | 216 | 17.4 | 225 | 18.1 | 236 | 19 | ||||
| Hypertension | 0.194 | |||||||||
| No | 1229 | 98.8 | 1232 | 99.1 | 1222 | 98.3 | ||||
| Yes | 15 | 1.2 | 11 | 0.9 | 21 | 1.7 | ||||
| Following a nutritional therapy | <0.001 | |||||||||
| No | 1135 | 91.2 | 1162 | 93.5 | 1113 | 89.5 | ||||
| Yes | 78 | 6.3 | 58 | 4.7 | 112 | 9 | ||||
| Missing | 31 | 2.5 | 23 | 1.9 | 18 | 1.4 | ||||
| Family history of diabetes | 0.138 | |||||||||
| No | 1126 | 90.5 | 1118 | 89.9 | 1096 | 88.2 | ||||
| Yes | 118 | 9.5 | 125 | 10.1 | 147 | 11.8 | ||||
| Parity | 0.007 | |||||||||
| Nulliparous | 969 | 77.9 | 1015 | 81.7 | 1031 | 82.9 | ||||
| 1–2 pregnancies | 204 | 16.4 | 157 | 12.6 | 146 | 11.8 | ||||
| ≥3 pregnancies | 33 | 2.7 | 44 | 3.5 | 32 | 2.6 | ||||
| Missing | 38 | 3.1 | 27 | 2.2 | 34 | 2.7 | ||||
| Pregnancies during follow-up | 0.287 | |||||||||
| 1 pregnancy | 561 | 45.1 | 511 | 41.1 | 550 | 44.3 | ||||
| 2 pregnancies | 423 | 34 | 449 | 36.1 | 416 | 33.5 | ||||
| ≥3 pregnancies | 260 | 20.9 | 283 | 22.8 | 277 | 22.3 | ||||
| Gestational diabetes | 0.287 | |||||||||
| No | 1191 | 95.7 | 1172 | 94.3 | 1181 | 95 | ||||
| Yes | 53 | 4.3 | 71 | 5.7 | 62 | 5 | ||||
| Tertiles of Energy-Adjusted Ultra-Processed Food Consumption | |||||
|---|---|---|---|---|---|
| T1 | T2 | T3 | P for Trend | ||
| Pooled sample | |||||
| Ultra-processed foods | No. cases/total | 53/1244 | 71/1243 | 62/1243 | |
| Median (servings/day) | 2.7 | 3.9 | 5.5 | ||
| Model 1 OR [95% CI] | Reference | 1.36 [0.95, 1.96] | 1.18 [0.81, 1.72] | 0.474 | |
| Model 2 OR [95% CI] | Reference | 1.35 [0.94, 1.95] | 1.13 [0.77, 1.65] | 0.651 | |
| Model 3 OR [95% CI] | Reference | 1.41 [0.96, 2.06] | 1.10 [0.74, 1.64] | 0.818 | |
| Women <30 years | |||||
| Ultra-processed foods | No. cases/total | 39/846 | 49/846 | 36/846 | |
| Median (servings/day) | 2.8 | 3.9 | 5.6 | ||
| Model 1 OR [95% CI] | Reference | 1.27 [0.83, 1.96] | 0.92 [0.58, 1.46] | 0.607 | |
| Model 2 OR [95% CI] | Reference | 1.28 [0.84, 1.96] | 0.89 [0.56, 1.41] | 0.494 | |
| Model 3 OR [95% CI] | Reference | 1.25 [0.79, 1.98] | 0.89 [0.54, 1.46] | 0.524 | |
| Women ≥30 years | |||||
| Ultra-processed foods | No. cases/total | 14/398 | 20/397 | 28/397 | |
| Median (servings/day) | 2.5 | 3.8 | 5.4 | ||
| Model 1 OR [95% CI] | Reference | 1.46 [0.72, 2.92] | 2.08 [1.08, 4.02] | 0.025 | |
| Model 2 OR [95% CI] | Reference | 1.42 [0.70, 2.87] | 1.94 [0.98, 3.81] | 0.050 | |
| Model 3 OR [95% CI] | Reference | 1.56 [0.77, 3.15] | 2.05 [1.03, 4.07] | 0.041 | |
| Tertiles of Consumption | |||||
|---|---|---|---|---|---|
| No. Cases/Total | T1 | T2 | T3 | P for Trend | |
| Pooled sample | |||||
| Overall | 186/3730 | Reference | 1.41 [0.96, 2.06] | 1.10 [0.74, 1.64] | 0.818 |
| Excluding prevalent cases of CVD and cancer | 183/3671 | Reference | 1.35 [0.92, 1.98] | 1.11 [0.74, 1.65] | 0.749 |
| Changing the energy limits (≥1000 kcal and ≤3500 kcal) | 160/3338 | Reference | 1.42 [0.94, 2.14] | 1.19 [0.77, 1.84] | 0.560 |
| Excluding women following a nutritional therapy | 170/3482 | Reference | 1.30 [0.88, 1.93] | 1.10 [0.72, 1.65] | 0.796 |
| Excluding women with past pregnancies | 161/3015 | Reference | 1.47 [0.97, 2.24] | 1.16 [0.75, 1.79] | 0.670 |
| Excluding women whose first pregnancy was 10 years after recruitment | 147/3232 | Reference | 1.20 [0.78, 1.84] | 1.15 [0.76, 1.75] | 0.506 |
| Adjusting for adherence to the Mediterranean diet | 186/3730 | Reference | 1.41 [0.96, 2.08] | 1.10 [0.74, 1.65] | 0.824 |
| Adjusting for carbohydrate and saturated fat intake | 186/3730 | Reference | 1.40 [0.95, 2.06] | 1.09 [0.72, 1.64] | 0.853 |
| Using UPF baseline consumption if GDM or first pregnancy was before 10 years | 186/3730 | Reference | 1.17 [0.80, 1.72] | 1.04 [0.71, 1.53] | 0.908 |
| Using %UPF of energy intake instead of servings/day | 186/3730 | Reference | 1.09 [0.74, 1.61] | 1.09 [0.73, 1.63] | 0.682 |
| Women <30 years | |||||
| Overall | 124/2538 | Reference | 1.25 [0.79, 1.98] | 0.89 [0.54, 1.46] | 0.524 |
| Excluding prevalent cases of CVD and cancer | 122/2505 | Reference | 1.20 [0.75, 1.91] | 0.89 [0.54, 1.46] | 0.543 |
| Changing theenergy limits (≥1000 kcal and ≤3500 kcal) | 107/2264 | Reference | 1.12 [0.69, 1.84] | 0.95 [0.55, 1.63] | 0.800 |
| Excluding women following a nutritional therapy | 113/2383 | Reference | 1.16 [0.73, 1.86] | 0.84 [0.50, 1.42] | 0.451 |
| Excluding women with past pregnancies | 120/2341 | Reference | 1.26 [0.79, 2.02] | 0.92 [0.55, 1.55] | 0.647 |
| Excluding women whose first pregnancy was 10 years after recruitment | 90/2098 | Reference | 1.06 [0.63, 1.79] | 0.83 [0.47, 1.47] | 0.499 |
| Adjusting for adherence to the Mediterranean diet | 124/2538 | Reference | 1.24 [0.78, 1.98] | 0.89 [0.53, 1.47] | 0.522 |
| Adjusting for carbohydrate and saturated fat intake | 124/2538 | Reference | 1.24 [0.78, 1.97] | 0.87 [0.52, 1.45] | 0.480 |
| Using UPF baseline consumption if GDM or first pregnancy was before 10 years | 124/2538 | Reference | 1.14 [0.72, 1.80] | 0.88 [0.54, 1.43] | 0.545 |
| Using %UPF of energy intake instead of servings/day | 124/2538 | Reference | 0.95 [0.60, 1.49] | 0.83 [0.51, 1.35] | 0.439 |
| Women ≥30 years | |||||
| Overall | 62/1192 | Reference | 1.56 [0.77, 3.15] | 2.05 [1.03, 4.07] | 0.041 |
| Excluding prevalent cases of CVD and cancer | 61/1166 | Reference | 1.50 [0.73, 3.06] | 2.05 [1.02, 4.10] | 0.042 |
| Changing the energy limits (≥1000 kcal and ≤3500 kcal) | 53/1074 | Reference | 2.04 [0.91, 4.60] | 2.36 [1.04, 5.36] | 0.045 |
| Excluding women following a nutritional therapy | 57/1099 | Reference | 1.49 [0.71, 3.13] | 2.21 [1.08, 4.55] | 0.028 |
| Excluding women with past pregnancies | 41/674 | Reference | 1.85 [0.71, 4.83] | 3.23 [1.27, 8.22] | 0.011 |
| Excluding women whose first pregnancy was 10 years after recruitment | 53/1134 | Reference | 1.48 [0.69, 3.21] | 2.50 [1.20, 5.22] | 0.011 |
| Adjusting for adherence to the Mediterranean diet | 62/1192 | Reference | 1.57 [0.78, 3.14] | 2.06 [1.05, 4.06] | 0.039 |
| Adjusting for carbohydrate and saturated fat intake | 62/1192 | Reference | 1.61 [0.78, 3.30] | 2.16 [1.06, 4.42] | 0.034 |
| Using UPF baseline consumption if GDM or first pregnancy was before 10 years | 62/1192 | Reference | 1.26 [0.62, 2.59] | 1.55 [0.81, 2.97] | 0.180 |
| Using %UPF of energy intake instead of servings/day | 62/1192 | Reference | 0.92 [0.44, 1.91] | 1.52 [0.77, 3.01] | 0.208 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leone, A.; Martínez-González, M.Á.; Craig, W.; Fresán, U.; Gómez-Donoso, C.; Bes-Rastrollo, M. Pre-Gestational Consumption of Ultra-Processed Foods and Risk of Gestational Diabetes in a Mediterranean Cohort. The SUN Project. Nutrients 2021, 13, 2202. https://doi.org/10.3390/nu13072202
Leone A, Martínez-González MÁ, Craig W, Fresán U, Gómez-Donoso C, Bes-Rastrollo M. Pre-Gestational Consumption of Ultra-Processed Foods and Risk of Gestational Diabetes in a Mediterranean Cohort. The SUN Project. Nutrients. 2021; 13(7):2202. https://doi.org/10.3390/nu13072202
Chicago/Turabian StyleLeone, Alessandro, Miguel Ángel Martínez-González, Winston Craig, Ujué Fresán, Clara Gómez-Donoso, and Maira Bes-Rastrollo. 2021. "Pre-Gestational Consumption of Ultra-Processed Foods and Risk of Gestational Diabetes in a Mediterranean Cohort. The SUN Project" Nutrients 13, no. 7: 2202. https://doi.org/10.3390/nu13072202
APA StyleLeone, A., Martínez-González, M. Á., Craig, W., Fresán, U., Gómez-Donoso, C., & Bes-Rastrollo, M. (2021). Pre-Gestational Consumption of Ultra-Processed Foods and Risk of Gestational Diabetes in a Mediterranean Cohort. The SUN Project. Nutrients, 13(7), 2202. https://doi.org/10.3390/nu13072202








