Factors Associated with Dietary Change since the Outbreak of COVID-19 in Japan
Abstract
1. Introduction
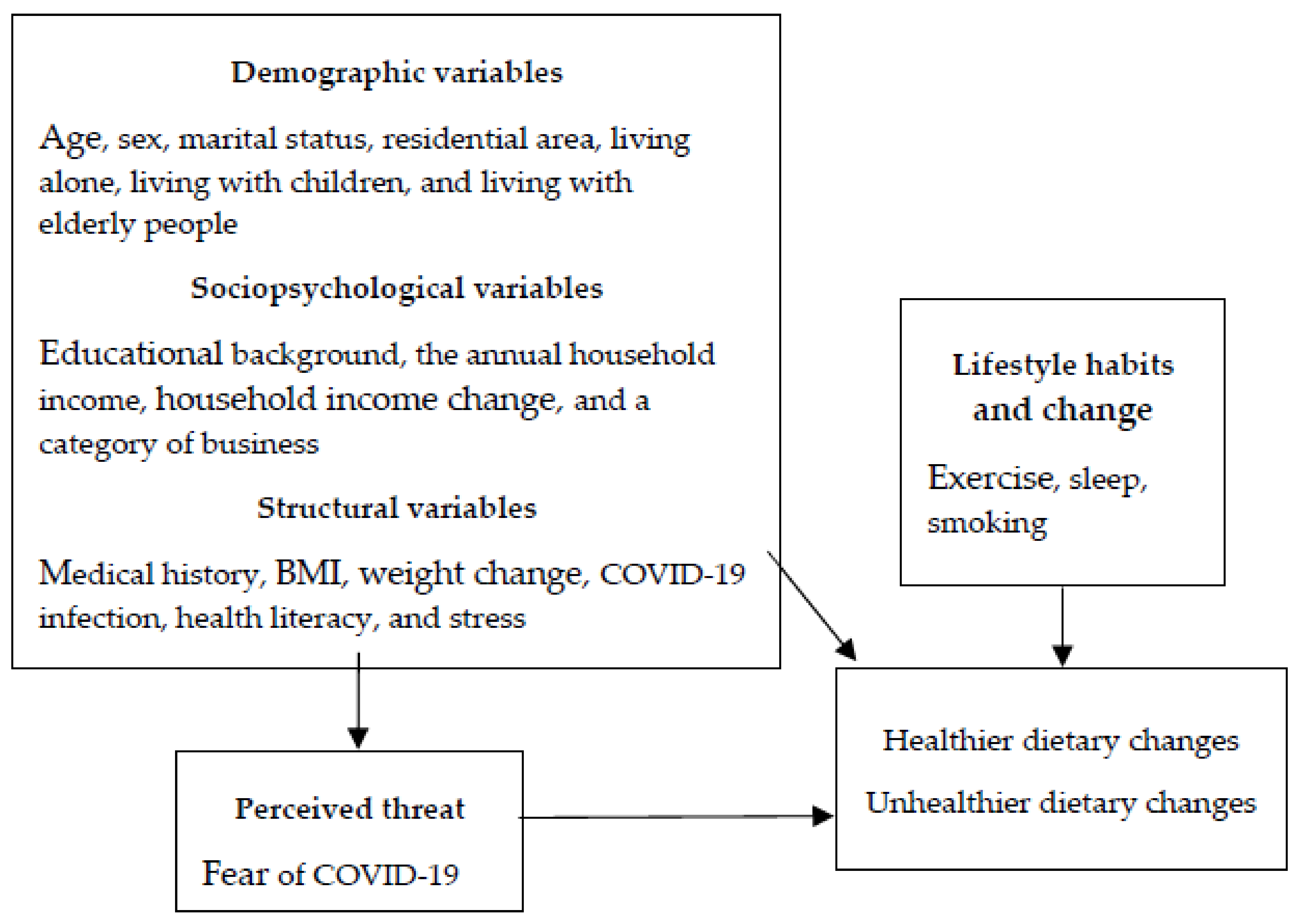
2. Materials and Methods
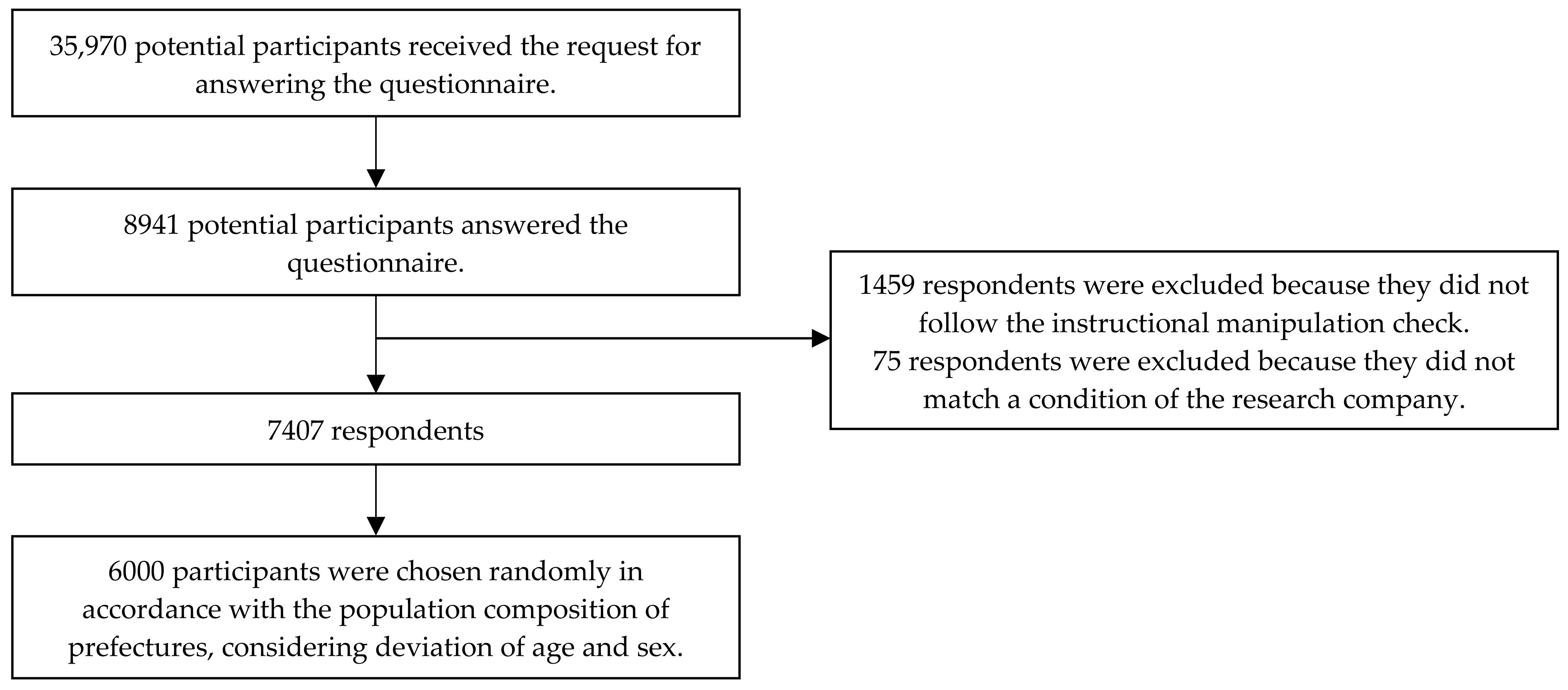
2.1. Participants and Procedures
2.2. Measurements
2.3. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Comparison of Demographic Variables among the Three Groups
3.3. Comparison of Sociopsychological Variables among the Three Groups
3.4. Comparison of Structural Variables among the Three Groups
3.5. Comparison of Lifestyle Habits and Changes among the Three Groups
3.6. Multinomial Logistic Regression Analyses of the Factors Associated with Changes in the Dietary Habits
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Karako, K.; Song, P.; Chen, Y.; Tang, W.; Kokudo, N. Overview of the characteristics of and responses to the three waves of COVID-19 in Japan during 2020–2021. Biosci. Trends 2021, 15, 1–8. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare. Example of Practicing “New Lifestyle”. Available online: https://www.mhlw.go.jp/content/en.newlifestyle.pdf (accessed on 16 February 2021).
- Cabine Secretariat. How to Prevent a Wide Spread Outbreak. Available online: https://corona.go.jp/en/prevention/ (accessed on 31 May 2021).
- Górnicka, M.; Drywień, M.E.; Zielinska, M.A.; Hamułka, J. Dietary and lifestyle changes during COVID-19 and the subsequent lockdowns among Polish adults: A cross-sectional online survey PLifeCOVID-19 study. Nutrients 2020, 12, 2324. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Pérez, C.; Molina-Montes, E.; Verardo, V.; Artach, R.; García-Villanova, B.; Guerra-Hernández, E.J.; Ruíz-López, M.R. Changes in dietary behaviours during the COVID-19 outbreak confinement in the Spanish COVIDiet study. Nutrients 2020, 12, 1730. [Google Scholar] [CrossRef] [PubMed]
- Sidor, A.; Rzymski, P. Dietary choices and habits during COVID-19 lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef]
- Papandreou, C.; Arija, V.; Aretouli, E.; Tsilidis, K.K.; Bulló, M. Comparing eating behaviours, and symptoms of depression and anxiety between Spain and Greece during the COVID-19 outbreak: Cross-sectional analysis of two different confinement strategies. Eur. Eat. Disord. Rev. 2020, 28, 836–846. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Olavarría, D.; Latorre-Román, P.A.; Guzmán-Guzmán, I.P.; Jerez-Mayorga, D.; Caamaño-Navarrete, F.; Delgado-Floody, P. Positive and negative changes in food habits, physical activity patterns, and weight status during COVID-19 confinement: Associated factors in the Chilean population. Int. J. Environ. Res. Public Health 2020, 17, 5431. [Google Scholar] [CrossRef] [PubMed]
- Poelman, M.P.; Gillebaart, M.; Schlinkert, C.; Dijkstra, S.C.; Derksen, E.; Mensink, F.; Hermans, R.C.J.; Aardening, P.; de Ridder, D.; de Vet, E. Eating behavior and food purchases during the COVID-19 lockdown: A cross-sectional study among adults in the Netherlands. Appetite 2021, 157, 105002. [Google Scholar] [CrossRef]
- Wang, X.; Lei, S.M.; Le, S.; Yang, Y.; Zhang, B.; Yao, W.; Gao, Z.; Cheng, S. Bidirectional influence of the COVID-19 pandemic lockdowns on health behaviors and quality of life among Chinese adults. Int. J. Environ. Res. Public Health 2020, 17, 5575. [Google Scholar] [CrossRef]
- Renzo, L.D.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef]
- Luo, Y.; Chen, L.; Xu, F.; Gao, X.; Han, D.; Na, L. Investigation on knowledge, attitudes, and practices about food safety and nutrition in the Chinese during the epidemic of corona virus disease 2019. Public Health Nutr. 2021, 24, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Lamarche, B.; Brassard, D.; Lapointe, A.; Laramée, C.; Kearney, M.; Côté, M.; Bélanger-Gravel, A.; Desroches, S.; Lemieux, S.; Plante, C. Changes in diet quality and food security among adults during the COVID-19–related early lockdown: Results from NutriQuébec. Am. J. Clin. Nutr. 2021, 113, 984–992. [Google Scholar] [CrossRef]
- Otaki, N.; Yano, M.; Yokoro, M.; Tanino, N.; Fukuo, K. Relationship between dietary variety and frailty in Japanese older adult women during the period of restriction on outings due to COVID-19. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020, gbaa218, published online ahead of print. [Google Scholar] [CrossRef]
- Cross, M.; Ng, S.K.; Scuffham, P. Trading health for wealth: The effect of COVID-19 response stringency. Int. J. Environ. Res. Public Health 2020, 17, 8725. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.W.S.; Lee, S.; Dong, M.C.; Taniguchi, M. What factors drive the satisfaction of citizens with governments’ responses to COVID-19? Int. J. Infect. Dis. 2021, 102, 327–331. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, M.L.; Raheem, D.; Ramos, F.; Carrascosa, C.; Saraiva, A.; Raposo, A. Highlights of current dietary guidelines in five continents. Int. J. Environ. Res. Public Health 2021, 18, 2814. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I.M. Historical origins of the health belief model. Health Educ. Monogr. 1974, 2, 328–335. [Google Scholar] [CrossRef]
- Oppenheimer, D.M.; Meyvis, T.; Davidenko, N. Instructional manipulation checks: Detecting satisficing to increase statistical power. J. Exp. Soc. Psychol. 2009, 45, 867–872. [Google Scholar] [CrossRef]
- Masuda, S.; Sakagami, T.; Morii, M. Comparison among methods for improving response quality of surveys. Jpn. J. Psychol. 2019, 90, 463–472. [Google Scholar] [CrossRef]
- Ministry of Internal Affairs and Communications. The Number of the Population Dynamic and the Household Based on the Basic Resident Registers. Available online: https://www.soumu.go.jp/main_sosiki/jichi_gyousei/daityo/jinkou_jinkoudoutai-setaisuu.html (accessed on 7 May 2021). (In Japanese)
- The Japan Institute for Labour Policy and Training, The Fourth General Survey for Households with Children, 2016. Available online: https://www.jil.go.jp/institute/research/2017/documents/175_siryo.pdf#page=206 (accessed on 16 February 2021). (In Japanese)
- Suka, M.; Odajima, T.; Kasai, M.; Igarashi, A.; Ishikawa, H.; Kusama, M.; Nakayama, T.; Sumitani, M.; Sugimori, H. The 14-item health literacy scale for Japanese adults (HLS-14). Environ. Health Prev. Med. 2013, 18, 407–415. [Google Scholar] [CrossRef]
- National Institute of Occupational Safety and Health, Japan. A Report of Survey about Items to Check Stress Symptoms. 2010. Available online: https://www.jniosh.johas.go.jp/publication/doc/houkoku/2010_04/report_stress_101129.pdf (accessed on 16 February 2021). (In Japanese)
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The fear of COVID-19 scale: Development and initial validation. Int. J. Ment. Health Addict. 2020. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare. The National Health and Nutrition Survey in Japan. 2018. Available online: https://www.mhlw.go.jp/content/000681200.pdf (accessed on 16 February 2021). (In Japanese)
- Ministry of Health, Labour and Welfare. The National Health and Nutrition Survey in Japan. 2019. Available online: https://www.mhlw.go.jp/content/000710991.pdf (accessed on 16 February 2021). (In Japanese)
- Hiep, T.N.; Binh, N.D.; Khue, M.P.; Giang, B.K.; Hoa, T.B.D.; Trung, T.N.; Thao, T.P.N.; Yen, H.N.; Kristine, S.; Andrew, P.; et al. Fear of COVID-19 scale—Associations of its scores with health literacy and health-related behaviors among medical students. Int. J. Environ. Res. Public Health 2020, 17, 4164. [Google Scholar] [CrossRef]
- Daniel, K.A.; Chung-Ying, L.; Amir, H.P. The association between health status and insomnia, mental health, and preventive behaviors: The mediating role of fear of COVID-19. Gerontol. Geriatr. Med. 2020, 6. [Google Scholar] [CrossRef]
- Papageorge, N.W.; Zahn, M.V.; Belot, M.; van den Broek-Altenburg, E.; Choi, S.; Jamison, J.C.; Tripodi, E. Socio-demographic factors associated with self-protecting behavior during the Covid-19 pandemic. J. Popul. Econ. 2021, 34, 691–738. [Google Scholar] [CrossRef]
- Zhao, A.; Li, Z.; Ke, Y.; Huo, S.; Ma, Y.; Zhang, Y.; Zhang, J.; Ren, Z. Dietary diversity among Chinese residents during the COVID-19 outbreak and its associated factors. Nutrients 2020, 12, 1699. [Google Scholar] [CrossRef]
- Jessica, M.Y.; Nicolle, M.K.; Candace, R.B.; Andrea, L.H.; Sophia, I.A.; Jonathan, F. Tobacco use changes and perceived health risks among current tobacco users during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 1795. [Google Scholar] [CrossRef]
- Nathalie, V.; Frieda, M.; Sven, V.L.; Dieter, Z.; Liesbeth, S.; Seline, V.A.; Cleo, L.C. Self-reported alcohol, tobacco, and cannabis use during COVID-19 lockdown measures: Results from a web-based survey. Eur. Addict. Res. 2020, 26, 309–315. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. People with Certain Medical Conditions. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fneed-extra-precautions%2Fgroups-at-higher-risk.html (accessed on 16 February 2021).
- Verónica, V.; Gloria, G.M.; Carina, S.G.; Sarah, M.; Manuel, J.R.; Oriol, S.; Myriam, G. Psychological health and physical activity levels during the COVID-19 pandemic: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 9419. [Google Scholar] [CrossRef]
| Demographic Variables | Total N = 6000 | Participants with Changes in Dietary Habits, n (%) | p1 | ||
|---|---|---|---|---|---|
| Healthier Group n = 1215 | Unhealthier Group n = 491 | Unchanged Group n = 4294 | |||
| Sex | |||||
| Male | 3044 (50.7) | 584 (48.1) | 242 (49.3) | 2218 (51.7) | 0.070 |
| Female | 2956 (49.3) | 631 (51.9) | 249 (50.7) | 2076 (48.3) | |
| Age, years | |||||
| 20–29 | 1099 (18.3) | 250 (20.6) | 120 (24.4) | 729 (17.0) | <0.001 |
| 30–39 | 1256 (20.9) | 246 (20.2) | 108 (22.0) | 902 (21.0) | |
| 40–49 | 1602 (26.7) | 300 (24.7) | 127 (25.9) | 1175 (27.4) | |
| 50–59 | 1405 (23.4) | 298 (24.5) | 103 (21.0) | 1004 (23.4) | |
| 60–64 | 638 (10.6) | 121 (10.0) | 33 (6.7) | 484 (11.3) | |
| Marital status | |||||
| Unmarried | 2593 (43.2) | 450 (37.0) | 265 (54.0) | 1878 (43.7) | <0.001 |
| Married | 3090 (51.5) | 708 (58.3) | 193 (39.3) | 2189 (51.0) | |
| Divorced or widowed 2 | 317 (5.3) | 57 (4.7) | 33 (6.7) | 227 (5.3) | |
| Residential area 3 | |||||
| North region | 240 (4.0) | 47 (3.9) | 15 (3.1) | 178 (4.1) | 0.075 |
| North-east region | 391 (6.5) | 86 (7.1) | 28 (5.7) | 277 (6.5) | |
| Eastern region | 2170 (36.2) | 479 (39.4) | 194 (39.5) | 1497 (34.9) | |
| Middle region | 1078 (18.0) | 214 (17.6) | 70 (14.3) | 794 (18.5) | |
| Midwest region | 971 (16.2) | 175 (14.4) | 86 (17.5) | 710 (16.5) | |
| Western region | 330 (5.5) | 55 (4.5) | 26 (5.3) | 249 (5.8) | |
| Southwest region | 167 (2.8) | 28 (2.3) | 13 (2.6) | 126 (2.9) | |
| Southern region | 653 (10.9) | 131 (10.8) | 59 (12.0) | 463 (10.8) | |
| Living alone | |||||
| Yes | 1076 (17.9) | 186 (15.3) | 139 (28.3 | 751 (17.5) | <0.001 |
| No | 4924 (82.1) | 1029 (84.7) | 352 (71.7) | 3543 (82.5) | |
| Living with children (<15 years old) | |||||
| Yes | 1173 (19.6) | 279 (23.0) | 70 (14.3) | 824 (19.2) | <0.001 |
| No | 4827(80.5) | 936 (77.0) | 421 (85.7) | 3470 (80.8) | |
| Living with elderly people (>65 years old) | |||||
| Yes | 1557 (26.0) | 296 (24.4) | 109 (22.2) | 1152 (26.8) | 0.032 |
| No | 4443 (74.1) | 919 (75.6) | 382 (77.8) | 3142 (73.2) | |
| Sociopsychological Variables | Total N = 6000 | Participants with Changes in Dietary Habits, n (%) | p1 | ||
|---|---|---|---|---|---|
| Healthier Group n = 1215 | Unhealthier Group n = 491 | Unchanged Group n = 4294 | |||
| Educational background | |||||
| Junior high school | 132 (2.2) | 16 (1.3) | 11 (2.2) | 105 (2.4) | <0.001 |
| High school | 1518 (25.3) | 253 (20.8) | 123 (25.1) | 1142 (26.6) | |
| Professional school | 682 (11.4) | 116 (9.5) | 59 (12.0) | 507 (11.8) | |
| Junior college 2 | 616 (10.3) | 136 (11.2) | 44 (9.0) | 436 (10.2) | |
| College 3 | 2702 (45.0) | 606 (49.9) | 230 (46.8) | 1866 (43.5) | |
| Graduate school | 350 (5.8) | 88 (7.2) | 24 (4.9) | 238 (5.5) | |
| Industrial classification | |||||
| Fishery, agriculture | 44 (0.7) | 9 (0.7) | 4 (0.8) | 31 (0.7) | 0.184 |
| Construction | 204 (3.4) | 38 (3.1) | 22 (4.5) | 144 (3.4) | |
| Manufacture | 743 (12.4) | 154 (12.7) | 71 (14.5) | 518 (12.1) | |
| Electricity, gas | 53 (0.9) | 12 (1.0) | 5 (1.0) | 36 (0.8) | |
| Information | 274 (4.6) | 66 (5.4) | 25 (5.1) | 183 (4.3) | |
| Transportation | 207 (3.5) | 28 (2.3)- | 24 (4.9) | 155 (3.6) | |
| Wholesale | 475 (7.9) | 96 (7.9) | 32 (6.5) | 347 (8.1) | |
| Finance | 237 (4.0) | 52 (4.3) | 16 (3.3) | 169 (3.9) | |
| Accommodations | 130 (2.2) | 20 (1.6) | 10 (2.0) | 100 (2.3) | |
| Medical services | 397 (6.6) | 73 (6.0) | 33 (6.7) | 291 (6.8) | |
| School education | 265 (4.4) | 76 (6.3) | 22 (4.5) | 167 (3.9)- | |
| Compound services | 36 (0.6) | 9 (0.7) | 3 (0.6) | 24 (0.6) | |
| Other services | 564 (9.4) | 106 (8.7) | 47 (9.6) | 411 (9.6) | |
| Public services | 256 (4.3) | 55 (4.5) | 17 (3.5) | 184 (4.3) | |
| Other | 530 (8.8) | 110 (9.1) | 41 (8.4) | 379 (8.8) | |
| Not working | 1585 (26.4) | 311 (25.6) | 119 (24.2) | 1155 (26.9) | |
| Annual household income (million JPY) 4 | |||||
| Less than one | 309 (6.0) | 48 (4.4) | 38 (8.8) | 223 (6.1) | <0.001 |
| One to two | 353 (6.8) | 45 (4.2) | 39 (9.0) | 269 (7.4) | |
| Two to three | 540 (10.5) | 93 (8.6) | 65 (15.1) | 382 (10.5) | |
| Three to four | 663 (12.9) | 136 (12.5) | 71 (16.5) | 456 (12.5) | |
| Four to five | 655 (12.7) | 116 (10.7) | 45 (10.4) | 494 (13.6) | |
| Five to six | 565 (11.0) | 112 (10.3) | 40 (9.3) | 413 (11.3) | |
| Six to seven | 489 (9.5) | 113 (10.4) | 41 (9.5) | 335 (9.2) | |
| Seven to eight | 431 (8.4) | 87 (8.0) | 27 (6.3) | 317 (8.7) | |
| Eight to nine | 277 (5.4) | 76 (7.0) | 15 (3.5) | 186 (5.1) | |
| Nine to ten | 261 (5.1) | 75 (6.9) | 11 (2.6) | 175 (4.8) | |
| More than ten | 615 (11.9) | 183 (16.9) | 39 (9.0) | 393 (10.8) | |
| Household-income change | |||||
| Decrease | 1317 (22.0) | 343 (28.2) | 175 (35.6) | 799 (18.6) | <0.001 |
| Increase | 362 (6.0) | 104 (8.6) | 32 (6.5) | 226 (5.3) | |
| No change | 4321 (72.0) | 768 (63.2) | 284 (57.8) | 3269 (76.1) | |
| Structural Variables | Total N = 6000 | Participants with Changes in Dietary Habits, n (%) | p1 | ||
|---|---|---|---|---|---|
| Healthier Group n = 1215 | Unhealthier Group n = 491 | Unchanged Group n = 4294 | |||
| Medical history | |||||
| Diabetes | |||||
| No | 5789 (96.5) | 1172 (96.5) | 465 (94.7) | 4152 (96.7) | 0.077 |
| Yes | 211 (3.5) | 43 (3.5) | 26 (5.3) | 142 (3.3) | |
| High blood pressure | |||||
| No | 5408 (90.1) | 1077 (88.6) | 434 (88.4) | 3897(90.8) | 0.037 |
| Yes | 592 (9.9) | 138 (11.4) | 57 (11.6) | 397 (9.2) | |
| Dyslipidemia | |||||
| No | 5524 (92.1) | 1099 (90.5) | 432 (88.0) | 3993 (93.0) | <0.001 |
| Yes | 476 (7.9) | 116 (9.5) | 59 (12.0) | 301 (7.0) | |
| Heart disease | |||||
| No | 5899 (98.3) | 1190 (97.9) | 480 (97.8) | 4229 (98.5) | 0.260 |
| Yes | 101 (1.7) | 25 (2.1) | 11 (2.2) | 65 (1.5) | |
| Stroke | |||||
| No | 5943 (99.1) | 1195 (98.4) | 483 (98.4) | 4265 (99.3) | 0.002 |
| Yes | 57 (1.0) | 20 (1.6) | 8 (1.6) | 29 (0.7) | |
| Chronic renal failure | |||||
| No | 5962 (99.4) | 1205 (99.2) | 481 (98.0) | 4276 (99.6) | <0.001 |
| Yes | 38 (0.6) | 10 (0.8) | 10 (2.0) | 18 (0.4) | |
| COPD 1 | |||||
| No | 5974 (99.6) | 1201 (98.8) | 488 (99.4) | 4285 (99.8) | <0.001 |
| Yes | 26 (0.4) | 14 (1.2) | 3 (0.6) | 9 (0.2) | |
| Malignant neoplasms | |||||
| No | 5842 (97.4) | 1172 (96.5) | 476 (96.9) | 4194 (97.7) | 0.056 |
| Yes | 158 (2.6) | 43 (3.5) | 15 (3.1) | 100 (2.3) | |
| BMI (kg/m2) | |||||
| <18.5 | 841 (14.1) | 149 (12.3) | 78 (15.9) | 614 (14.4) | 0.001 |
| 18.5–25.0 | 3986 (66.6) | 849 (70.0) | 292 (59.5) | 2845 (66.5) | |
| >25.0 | 1154 (19.3) | 215 (17.7) | 121 (24.6) | 818 (19.1) | |
| Weight change 2 | |||||
| Decrease | 308 (5.1) | 118 (9.7) | 44 (9.0) | 146 (3.4) | <0.001 |
| Increase | 321 (5.4) | 79 (6.5) | 77 (15.7) | 165 (3.9) | |
| No change | 5352 (89.5) | 1016 (83.8) | 370 (75.4) | 3966 (92.7) | |
| Median value (25, 75 percentile) | p3 | ||||
| Health literacy | 50 (43, 56) | 52 (45, 58) a | 49 (43, 55) b | 50 (42, 56) b | <0.001 |
| Stress | 16 (11, 21) | 16 (11, 21) a | 20 (16, 26) b | 15 (10, 20) c | <0.001 |
| COVID-19 infection | |||||
| Oneself | n (%) | p1 | |||
| Not infected | 5958 (99.3) | 1189 (97.9) | 484 (98.6) | 4285 (99.8) | <0.001 |
| Infected | 42 (0.7) | 26 (2.1) | 7 (1.4) | 9 (0.2) | |
| Family living together | |||||
| Not infected | 5968 (99.5) | 1197 (98.5) | 487 (99.2) | 4284 (99.8) | <0.001 |
| Infected | 32 (0.5) | 18 (1.5) | 4 (0.8) | 10 (0.2) | |
| Other family and relatives | |||||
| Not infected | 5957 (99.3) | 1193 (98.2) | 485 (98.8) | 4279 (99.7) | <0.001 |
| Infected | 43 (0.7) | 22 (1.8) | 6 (1.2) | 15 (0.3) | |
| Colleagues | |||||
| Not infected | 5822 (97.0) | 1159 (95.4) | 462 (94.1) | 4201 (97.8) | <0.001 |
| Infected | 178 (3.0) | 56 (4.6) | 29 (5.9) | 93 (2.2) | |
| Friends | |||||
| Not infected | 5863 (97.7) | 1152 (94.8) | 475 (96.7) | 4236 (98.6) | <0.001 |
| Infected | 137 (2.3) | 63 (5.2) | 16 (3.3) | 58 (1.4) | |
| Median value (25, 75 percentile) | p3 | ||||
| Fear of COVID-19 | 18 (14, 21) | 19 (15, 22) a | 19 (15, 23) a | 18 (14, 21) b | <0.001 |
| Lifestyle Habits | Total N = 6000 | Participants with Changes in Dietary Habits, n (%) | p1 | ||
|---|---|---|---|---|---|
| Healthier Group n = 1215 | Unhealthier Group n = 491 | Unchanged Group n = 4294 | |||
| Exercise frequency | |||||
| Almost none | 3386 (56.4) | 436 (35.9) | 305 (62.1) | 2645 (61.6) | <0.001 |
| 1–3 times a month | 437 (7.3) | 95 (7.8) | 46 (9.4) | 296 (6.9) | |
| 1–2 times a week | 937 (15.6) | 270 (22.2) | 64 (13.0) | 603 (14.0) | |
| 3–4 times a week | 545 (9.1) | 177 (14.6) | 39 (7.9) | 329 (7.7) | |
| 5–6 times a week | 353 (5.9) | 112 (9.2) | 18 (3.7) | 223 (5.2) | |
| Every day | 342 (5.7) | 125 (10.3) | 19 (3.9) | 198 (4.6) | |
| Sleep time, hours | |||||
| <5 | 580 (9.7) | 88 (7.2) | 83 (16.9) | 409 (9.5) | <0.001 |
| 5–6 | 1789 (29.8) | 349 (28.7) | 149 (30.3) | 1291 (30.1) | |
| 6–7 | 2056 (34.3) | 449 (37.0) | 127 (25.9) | 1480 (34.5) | |
| 7–8 | 1174 (19.6) | 261 (21.5) | 90 (18.3) | 823 (19.2) | |
| 8–9 | 282 (4.7) | 52 (4.3) | 23 (4.7) | 207 (4.8) | |
| >9 | 119 (2.0) | 16 (1.3) | 19 (3.9) | 84 (2.0) | |
| Smoking | |||||
| No | 4903 (81.7) | 956 (78.7) | 392 (79.8) | 3555 (82.8) | 0.003 |
| Yes | 1097 (18.3) | 259 (21.3) | 99 (20.2) | 739 (17.2) | |
| Lifestyle changes | |||||
| Exercise times per week | |||||
| Decreased | 1094 (18.2) | 320 (26.3) | 223 (45.4) | 551 (12.8) | <0.001 |
| Increased | 642 (10.7) | 310 (25.5) | 50 (10.2) | 282 (6.6) | |
| No change | 4264 (71.1) | 585 (48.1) | 218 (44.4) | 3461 (80.6) | |
| Sleep time per day | |||||
| Decreased | 588 (9.8) | 146 (12.0) | 144 (29.3) | 298 (6.9) | <0.001 |
| Increased | 717 (12.0) | 341 (28.1) | 105 (21.4) | 271 (6.3) | |
| No change | 4695 (78.3) | 728 (59.9) | 242 (49.3) | 3725 (86.7) | |
| Smoking | |||||
| Quit smoking | 70 (1.2) | 24 (2.0) | 10 (2.0) | 36 (0.8) | <0.001 |
| Started smoking | 25 (0.4) | 16 (1.3) | 3 (0.6) | 6 (0.1) | |
| No change 2 | 5905 (98.4) | 1175 (96.7) | 478 (97.4) | 4252 (99.0) | |
| Factors | Reference | Participants with Changes in Dietary Habits Odds Ratio (95% CI) Based on Unchanged Group | |
|---|---|---|---|
| Healthier Group | Unhealthier Group | ||
| Demographic variables | |||
| Living alone | Not living alone | 0.93 (0.76–1.15) | 1.62 (1.25–2.10) *** |
| Sociopsychological variables | |||
| Annual household income | 1.08 (1.05–1.10) *** | 0.97 (0.93–1.01) | |
| Household-income change | |||
| Decrease | No change | 1.42 (1.18–1.70) *** | 1.53 (1.20–1.95) ** |
| Increase | No change | 1.58 (1.18–2.10) ** | 1.09 (0.70–1.69) |
| Structural variables | |||
| Colleague | Uninfected | 1.39 (0.92–2.10) | 1.88 (1.13–3.14) * |
| Friends | Uninfected | 2.05 (1.32–3.18) ** | 1.54 (0.81–2.91) |
| Health literacy | 1.02 (1.01–1.03) *** | 1.00 (0.98–1.01) | |
| Stress | 0.99 (0.98–1.00) | 1.05 (1.04–1.07) *** | |
| Weight change | |||
| Decrease | No change | 2.32 (1.72–3.13) *** | 2.21 (1.47–3.32) *** |
| Increase | No change | 1.28 (0.92–1.78) | 3.11 (2.21–4.37) *** |
| Perceived threat | |||
| Fear of COVID-19 | 1.06 (1.04–1.07) *** | 1.02 (1.00–1.04) * | |
| Lifestyle habits | |||
| Exercise | 1.22 (1.16–1.28) *** | 0.96 (0.88–1.04) | |
| Smoking | Not smoking | 1.43 (1.18–1.73) *** | 1.37 (1.04–1.80) * |
| Lifestyle change | |||
| Exercise frequency per week | |||
| Decrease | No change | 2.22 (1.81–2.72) *** | 2.88 (2.19–3.78) *** |
| Increase | No change | 3.10 (2.45–3.92) *** | 1.94 (1.29–2.92) ** |
| Sleep duration per day | |||
| Decrease | No change | 1.44 (1.11–1.87) ** | 3.10 (2.29–4.20) *** |
| Increase | No change | 3.07 (2.46–3.83) *** | 2.69 (1.95–3.71) *** |
| Smoking | |||
| Quit smoking | No change | 1.67 (0.88–3.17) | 1.90 (0.84–4.29) |
| Started smoking | No change | 4.25 (1.23–14.7) * | 1.65 (0.31–8.77) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shimpo, M.; Akamatsu, R.; Kojima, Y.; Yokoyama, T.; Okuhara, T.; Chiba, T. Factors Associated with Dietary Change since the Outbreak of COVID-19 in Japan. Nutrients 2021, 13, 2039. https://doi.org/10.3390/nu13062039
Shimpo M, Akamatsu R, Kojima Y, Yokoyama T, Okuhara T, Chiba T. Factors Associated with Dietary Change since the Outbreak of COVID-19 in Japan. Nutrients. 2021; 13(6):2039. https://doi.org/10.3390/nu13062039
Chicago/Turabian StyleShimpo, Misa, Rie Akamatsu, Yui Kojima, Tetsuji Yokoyama, Tsuyoshi Okuhara, and Tsuyoshi Chiba. 2021. "Factors Associated with Dietary Change since the Outbreak of COVID-19 in Japan" Nutrients 13, no. 6: 2039. https://doi.org/10.3390/nu13062039
APA StyleShimpo, M., Akamatsu, R., Kojima, Y., Yokoyama, T., Okuhara, T., & Chiba, T. (2021). Factors Associated with Dietary Change since the Outbreak of COVID-19 in Japan. Nutrients, 13(6), 2039. https://doi.org/10.3390/nu13062039






