Adherence to Mediterranean Diet Measured through Medi-Lite Score and Obesity: A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. The Medi-Lite Adherence Score
2.2. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
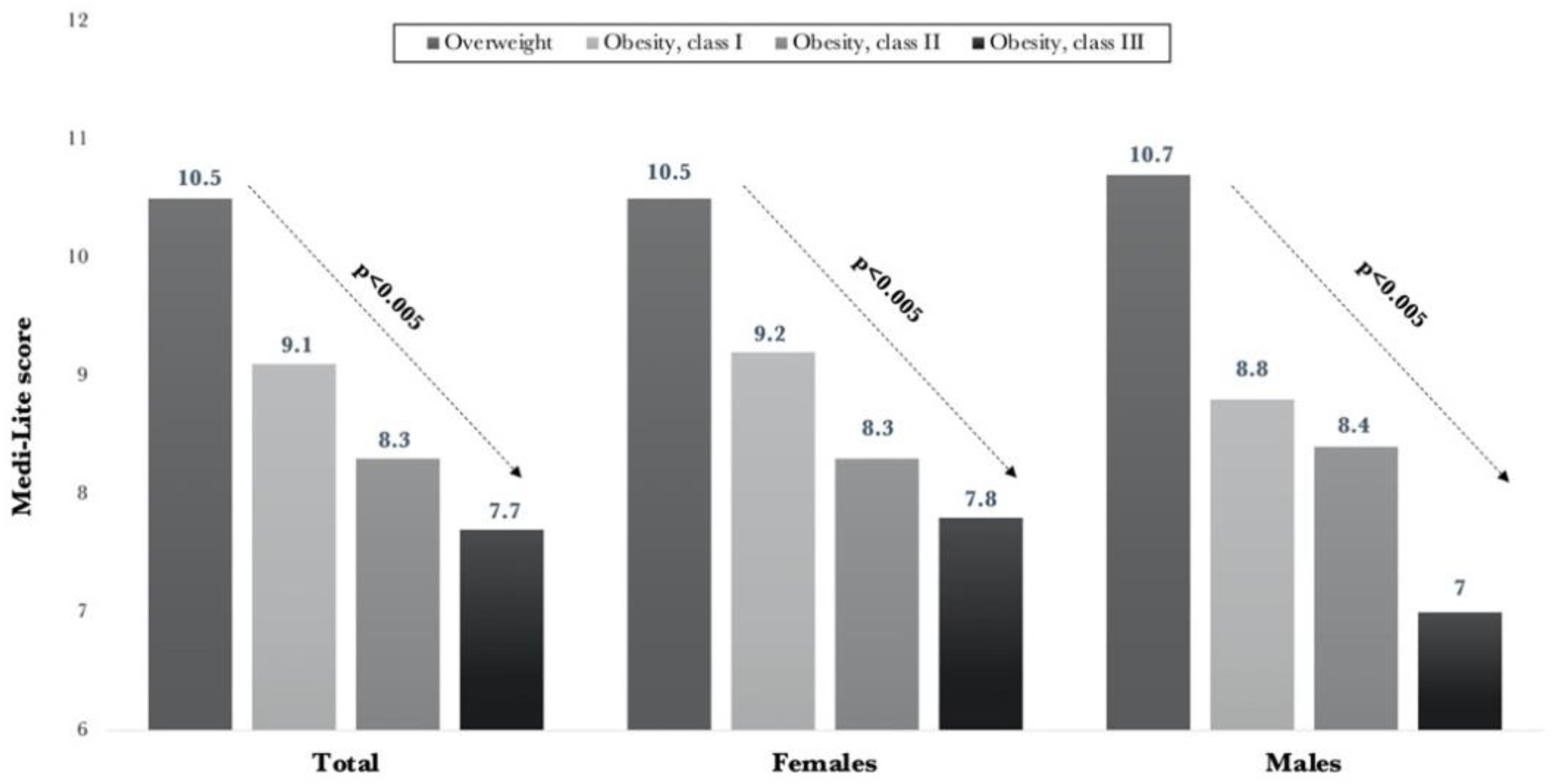
3.2. Medi-Lite Score
3.3. Medi-Lite Score and Risk of Abdominal Obesity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Martí, A.Z.; Cabañero-Martínez, M.J.; Hurtado-Sánchez, J.A.; Laguna-Pérez, A.; Ferrer-Cascales, R. Evaluation of Mediterranean diet adherence scores: A systematic review. BMJ Open 2018, 8, e019033. [Google Scholar] [CrossRef] [PubMed]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean diet and health status: An updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014, 17, 2769–2782. [Google Scholar] [CrossRef]
- Sofi, F.; Dinu, M.; Pagliai, G.; Marcucci, R.; Casini, A. Validation of a literature-based adherence score to Mediterranean diet: The MEDI-LITE score. Int. J. Food Sci. Nutr. 2017, 68, 757–762. [Google Scholar] [CrossRef]
- Lavalette, C.; Adjibade, M.; Srour, B.; Sellem, L.; Fiolet, T.; Hercberg, S.; Latino-Martel, P.; Fassier, P.; Deschasaux, M.; Kesse-Guyot, E.; et al. Cancer-Specific and General Nutritional Scores and Cancer Risk: Results from the Prospective NutriNet-Santé Cohort. Cancer Res. 2018, 78, 4427–4435. [Google Scholar] [CrossRef]
- Trebuchet, A.; Julia, C.; Fezeu, L.; Touvier, M.; Chaltiel, D.; Hercberg, S.; Galan, P.; Adjibade, M.; Kesse-Guyot, E. Prospective as-sociation between several dietary scores and risk of cardiovascular disease: Is the Mediterranean diet equally associated to CVD compared to national nutritional scores? Am. Heart J. 2019, 217, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kesse-Guyot, E.; Rebouillat, P.; Payrastre, L.; Alles, B.; Fezeu, L.K.; Druesne-Pecollo, N.; Srour, B.; Bao, W.; Touvier, M.; Galan, P.; et al. Prospective association between organic food consumption and risk of type 2 diabetes: Findings from the NutriNet-Santè cohort study. Int. J. Behav. Nutr. Phys. Activ. 2020, 17, 136. [Google Scholar] [CrossRef] [PubMed]
- Currenti, W.; Buscemi, S.; Cincione, R.I.; Cernigliaro, A.; Godos, J.; Grosso, G.; Galvano, F. Time-Restricted Feeding and Metabolic Outcomes in a Cohort of Italian Adults. Nutrition 2021, 13, 1651. [Google Scholar] [CrossRef]
- Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: Executive sum-mary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am. J. Clin. Nutr. 1998, 68, 899–917. [Google Scholar] [CrossRef]
- Lean, M.E.J.; Han, T.S.; Morrison, C.E. Waist circumference as a measure for indicating need for weight management. BMJ 1995, 311, 158–161. [Google Scholar] [CrossRef]
- World Health Organisation. Physical Status: The Use and Interpretation of Anthropometry; Technical Report Series 854; WHO: Geneva, Switzerland, 1995. [Google Scholar]
- CIHEAM/FAO. Mediterranean Food Consumption Patterns: Diet, Environment, Society, Economy and Health; (A White Paper Priority 5 of Feeding Knowledge Programme, Expo Milan); CIHEAM-IAMB: Bari, Italy; FAO: Rome, Italy, 2015. [Google Scholar]
- Dinu, M.; Pagliai, G.; Angelino, D.; Rosi, A.; Dall’Asta, M.; Bresciani, L.; Ferraris, C.; Guglielmetti, M.; Godos, J.; Del Bo’, C.; et al. Effects of Popular Diets on Anthropometric and Cardiometabolic Parameters: An Umbrella Review of Meta-Analyses of Randomized Controlled Trials. Adv. Nutr. 2020, 11, 815–833. [Google Scholar] [CrossRef]
- Vareiro, D.; Bach-Faig, A.; Quintana, B.R.; Bertomeu, I.; Buckland, G.; De Almeida, M.D.V.; Serra-Majem, L. Availability of Mediterranean and non-Mediterranean foods during the last four decades: Comparison of several geographical areas. Public Health Nutr. 2009, 12, 1667–1675. [Google Scholar] [CrossRef]
- Vilarnau, C.; Stracker, D.M.; Funtikov, A.; Da Silva, R.; Estruch, R.; Bach-Faig, A. Worldwide adherence to Mediterranean Diet between 1960 and 2011. Eur. J. Clin. Nutr. 2019, 72, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Aoun, C.; Papazian, T.; Helou, K.; El Osta, N.; Khabbaz, L.R. Comparison of five international indices of adherence to the Mediterranean diet among healthy adults: Similarities and differences. Nutr. Res. Pract. 2019, 13, 333–343. [Google Scholar] [CrossRef] [PubMed]
- Papadaki, A.; Linardakis, M. The use of composite scores to assess adherence to dietary patterns: The Mediterranean diet case. In Appetite and Nutritional Assessment, Nutrition and Diet Research Progress Series, 1st ed.; Ellsworth, S.J., Schuster, R.C., Eds.; Nova Science Publishers Inc: New York, NY, USA, 2009; pp. 285–354. [Google Scholar]
- Martínez-González, M.A.; García-Arellano, A.; Toledo, E.; Salas-Salvadó, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schröder, H.; Arós, F.; Gómez-Gracia, E.; et al. A 14-item Medi-terranean diet assessment tool and obesity indexes among high-risk subjects: The PREDIMED trial. PLoS ONE 2012, 7, e43134. [Google Scholar] [CrossRef] [PubMed]
- Fiore, V.; Capraro, M.; Ragusa, R.; Godos, J.; Mistretta, A.; Marranzano, M. Mediterranean diet and metabolic status in post-menopausal women living in a mediterranean area. Nutr. Health Aging 2019, 5, 53–60. [Google Scholar] [CrossRef]
- Vitale, M.; Racca, E.; Izzo, A.; Giacco, A.; Parente, E.; Riccardi, G.; Giacco, R. Adherence to the traditional Mediterranean diet in a population of South of Italy: Factors involved and proposal of an educational field-based survey tool. Int. J. Food Sci. Nutr. 2018, 70, 195–201. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Sánchez-Taínta, A.; Estruch, R.; Bulló, M.; Corella, D.; Gómez-Gracia, E.; Fiol, M.; Algorta, J.; Covas, M.-I.; Lapetra, J.; Zazpe, I.; et al. Adherence to a Mediterranean-type diet and reduced prevalence of clustered cardiovascular risk factors in a cohort of 3204 high-risk patients. Eur. J. Cardiovasc. Prev. Rehab. 2008, 15, 589–593. [Google Scholar] [CrossRef]
- Bulló, M.; Garcia-Aloy, M.; Martínez-González, M.A.; Corella, D.; Fernández-Ballart, J.D.; Fiol, M.; Gómez-Gracia, E.; Estruch, R.; Ortega-Calvo, M.; Francisco, S.; et al. Association between a healthy lifestyle and general obesity and abdominal obesity in an elderly population at high cardiovascular risk. Prev. Med. 2011, 53, 155–161. [Google Scholar] [CrossRef]
- Agnoli, C.; Sieri, S.; Ricceri, F.; Giraudo, M.T.; Masala, G.; Assedi, M.; Panico, S.; Mattiello, A.; Tumino, R.; Giurdanella, M.C.; et al. Adherence to a Mediterranean diet and long-term changes in weight and waist circumference in the EPIC-Italy cohort. Nutr. Diabetes 2018, 8, 22. [Google Scholar] [CrossRef]
- Dayib, M.; Larson, J.; Slavin, J. Dietary fibers reduce obesity-related disorders: Mechanisms of action. Curr. Opin. Clin. Nutr. Metab. Care 2020, 23, 445–450. [Google Scholar] [CrossRef] [PubMed]
- Kanauchi, M.; Kanauchi, K. Development of a Mediterranean diet score adapted to Japan and its relation to obesity risk. Food Nutr. Res. 2016, 60, 32172. [Google Scholar] [CrossRef]
- Shatwan, I.M.; Alhinai, E.A.; Alawadhi, B.; Surendran, S.; Aljefree, N.M.; Almoraie, N.M. High Adherence to the Mediterranean Diet Is Associated with a Reduced Risk of Obesity among Adults in Gulf Countries. Nutrition 2021, 13, 995. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Morze, J.; Hoffmann, G. Mediterranean diet and health status: Active ingredients and pharmacological mechanisms. Br. J. Pharmacol. 2020, 177, 1241–1257. [Google Scholar] [CrossRef] [PubMed]
- Hermsdorff, H.H.M.; Zulet, M.A.; Abete, I.; Martinez, J.A. Discriminated benefits of a Mediterranean dietary pattern within a hypocaloric diet program on plasma RBP4 concentrations and other inflammatory markers in obese subjects. Endocrine 2009, 36, 445–451. [Google Scholar] [CrossRef] [PubMed]

| Males (n = 72) | Females (n = 208) | |
|---|---|---|
| Body weight | 96.1 ± 16.6 | 84.2 ± 13.8 |
| BMI, kg/m2 | 31.3 ± 4.5 | 32.2 ± 3.9 |
| Overweight, n (%) | 24 (33.3) | 94 (45.2) |
| Obesity class I, n (%) | 32 (44.4) | 78 (37.5) |
| Obesity class II, n (%) | 15 (20.8) | 28 (13.5) |
| Obesity class III, n (%) | 15 (20.8) | 28 (13.5) |
| Obesity class IV, n (%) | 1 (1.4) | 8 (3.8) |
| WC, cm | 105.7 ± 8.1 | 99.2 ± 9.1 |
| WC > 102 cm M; >88 cm F | 42 (58.3) | 192 (92.3) |
| Fat mass, kg | 32 ± 9.6 | 34.9 ± 9.6 |
| Fat mass, % | 32.8 ± 6.6 | 40.4 ± 4.9 |
| Fat mass > 25% M; >35% F | 63 (87.5) | 186 (89.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dinu, M.; Pagliai, G.; Lotti, S.; Giangrandi, I.; Colombini, B.; Sofi, F. Adherence to Mediterranean Diet Measured through Medi-Lite Score and Obesity: A Retrospective Study. Nutrients 2021, 13, 2007. https://doi.org/10.3390/nu13062007
Dinu M, Pagliai G, Lotti S, Giangrandi I, Colombini B, Sofi F. Adherence to Mediterranean Diet Measured through Medi-Lite Score and Obesity: A Retrospective Study. Nutrients. 2021; 13(6):2007. https://doi.org/10.3390/nu13062007
Chicago/Turabian StyleDinu, Monica, Giuditta Pagliai, Sofia Lotti, Ilaria Giangrandi, Barbara Colombini, and Francesco Sofi. 2021. "Adherence to Mediterranean Diet Measured through Medi-Lite Score and Obesity: A Retrospective Study" Nutrients 13, no. 6: 2007. https://doi.org/10.3390/nu13062007
APA StyleDinu, M., Pagliai, G., Lotti, S., Giangrandi, I., Colombini, B., & Sofi, F. (2021). Adherence to Mediterranean Diet Measured through Medi-Lite Score and Obesity: A Retrospective Study. Nutrients, 13(6), 2007. https://doi.org/10.3390/nu13062007








