Development and Application of a Total Diet Quality Index for Toddlers
Abstract
1. Introduction
2. Methods
2.1. Diet Quality Index Development
2.2. Diet Quality Index Components
2.2.1. 100% Fruit Juice
2.2.2. Fats
2.2.3. Added Sugars
2.2.4. Dairy
2.2.5. Sodium
2.3. Diet Quality Index Scoring
2.4. Sampling and Data Collection
3. Results
3.1. Sample Characteristics
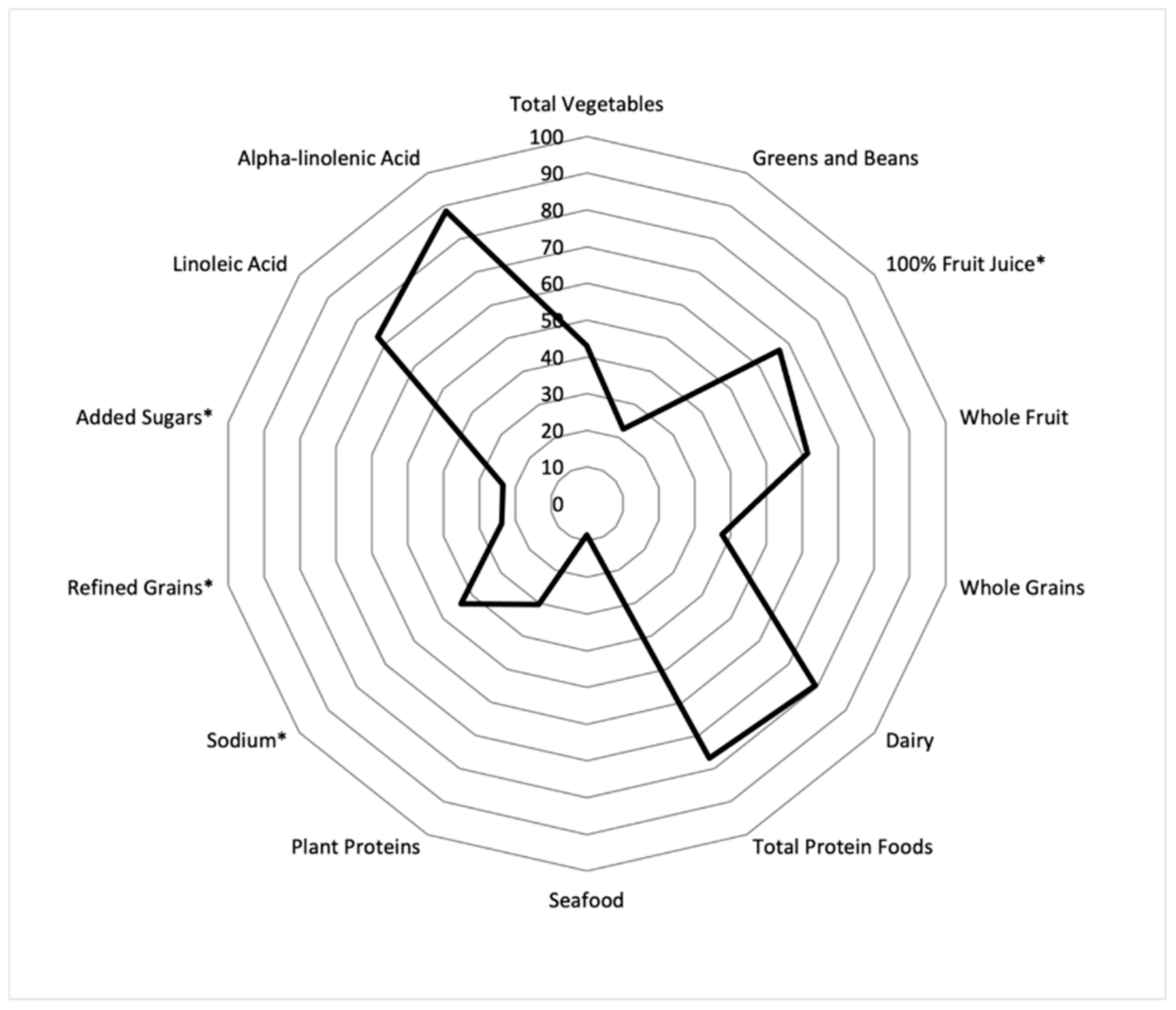
3.2. Overall Toddler DQI and Components Scores
3.3. Demographic Differences in DQI Scores
3.3.1. Breastfeeding Behavior
3.3.2. Race and Ethnicity
3.3.3. WIC Participation
3.3.4. Federal Poverty Level (FPL) Index
3.3.5. Urbanicity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Golley, R.K.; Smithers, L.G.; Mittinty, M.N.; Emmett, P.; Northstone, K.; Lynch, J.W. Diet quality of U.K. infants is associated with dietary, adiposity, cardiovascular, and cognitive outcomes measured at 7–8 years of age. J. Nutr. 2013, 143, 1611–1617. [Google Scholar] [CrossRef]
- McGuire, S. Institute of Medicine (IOM) Early Childhood Obesity Prevention Policies. Washington, DC: The National Academies Press; 2011. Adv. Nutr. 2012, 3, 56–57. [Google Scholar] [CrossRef]
- Miles, G.; Siega-Riz, A.M. Trends in Food and Beverage Consumption among Infants and Toddlers: 2005–2012. Pediatrics 2017, 139. [Google Scholar] [CrossRef] [PubMed]
- Birch, L.L.; Doub, A.E. Learning to eat: Birth to age 2 y. Am. J. Clin. Nutr. 2014, 99, 723S–728S. [Google Scholar] [CrossRef] [PubMed]
- Grimm, K.A.; Kim, S.A.; Yaroch, A.L.; Scanlon, K.S. Fruit and vegetable intake during infancy and early childhood. Pediatrics 2014, 134, S63–S69. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Pan, L.; Sherry, B.; Li, R. The association of sugar-sweetened beverage intake during infancy with sugar-sweetened beverage intake at 6 years of age. Pediatrics 2014, 134, S56–S62. [Google Scholar] [CrossRef] [PubMed]
- Rose, C.M.; Birch, L.L.; Savage, J.S. Dietary patterns in infancy are associated with child diet and weight outcomes at 6 years. Int. J. Obes. 2017, 41, 783–788. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 8th Edition. December 2015. Available online: https://health.gov/our-work/food-nutrition/previous-dietary-guidelines/2015 (accessed on 17 November 2020).
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025. 9th Edition. December 2020. Available online: DietaryGuidelines.gov (accessed on 29 December 2020).
- Kennedy, E.T.; Ohls, J.; Carlson, S.; Fleming, K. The Healthy Eating Index: Design and applications. J. Am. Diet. Assoc. 1995, 95, 1103–1108. [Google Scholar] [CrossRef]
- Reedy, J.; Lerman, J.L.; Krebs-Smith, S.M.; Kirkpatrick, S.I.; Pannucci, T.E.; Wilson, M.M.; Subar, A.F.; Kahle, L.L.; Tooze, J.A. Evaluation of the Healthy Eating Index-2015. J. Acad. Nutr. Diet. 2018, 118, 1622–1633. [Google Scholar] [CrossRef] [PubMed]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef] [PubMed]
- Thomson, J.L.; Tussing-Humphreys, L.M.; Goodman, M.; Landry, A.S. Diet quality in a nationally representative sample of American children by sociodemographic characteristics. Am. J. Clin. Nutr. 2019, 109, 127–138. [Google Scholar] [CrossRef]
- Dalwood, P.; Marshall, S.; Burrows, T.L.; McIntosh, A.; Collins, C.E. Diet quality indices and their associations with health-related outcomes in children and adolescents: An updated systematic review. Nutr. J. 2020, 19, 118. [Google Scholar] [CrossRef] [PubMed]
- Au, L.E.; Gurzo, K.; Paolicelli, C.; Whaley, S.E.; Weinfield, N.S.; Ritchie, L.D. Diet Quality of US Infants and Toddlers 7–24 Months Old in the WIC Infant and Toddler Feeding Practices Study-2. J. Nutr. 2018, 148, 1786–1793. [Google Scholar] [CrossRef]
- Marshall, S.; Burrows, T.; Collins, C.E. Systematic review of diet quality indices and their associations with health-related outcomes in children and adolescents. J. Hum. Nutr. Diet. 2014, 27, 577–598. [Google Scholar] [CrossRef] [PubMed]
- Kourlaba, G.; Panagiotakos, D.B. Dietary quality indices and human health: A review. Maturitas 2009, 62, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hamner, H.C.; Moore, L.V. Dietary quality among children from 6 months to 4 years, NHANES 2011-2016. Am. J. Clin. Nutr. 2020, 111, 61–69. [Google Scholar] [CrossRef]
- Dietary Guidelines Advisory Committee. Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Agriculture and the Secretary of Health and Human Services; U.S. Department of Agriculture, Agricultural Research Service: Washington, DC, USA, 2020.
- National Academies of Sciences, Engineering, and Medicine. Dietary Reference Intakes for Sodium and Potassium; Stallings, V.A., Harrison, M., Oria, M., Eds.; The National Academies Press: Washington, DC, USA, 2019; pp. 230–231. [Google Scholar]
- Institute of Medicine. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements; Otten, J.J., Hellwig, J.P., Meyers, L.D., Eds.; The National Academies Press: Washington, DC, USA, 2006; pp. 536–537. [Google Scholar]
- Centers for Disease Control and Prevention. Breastfeeding Report Card United States, 2020. September 2020. Available online: https://www.cdc.gov/breastfeeding/pdf/2020-Breastfeeding-Report-Card-H.pdf (accessed on 3 December 2020).
- Ahluwalia, N.; Herrick, K.A.; Rossen, L.M.; Rhodes, D.; Kit, B.; Moshfegh, A.; Dodd, K.W. Usual nutrient intakes of US infants and toddlers generally meet or exceed Dietary Reference Intakes: Findings from NHANES 2009–2012. Am. J. Clin. Nutr. 2016, 104, 1167–1174. [Google Scholar] [CrossRef]
- Bailey, R.L.; Catellier, D.J.; Jun, S.; Dwyer, J.T.; Jacquier, E.F.; Anater, A.S.; Eldridge, A. Total Usual Nutrient Intakes of US Children (Under 48 Months): Findings from the Feeding Infants and Toddlers Study (FITS) 2016. J. Nutr. 2018, 148, 1557S–1566S. [Google Scholar] [CrossRef]
- Spahn, J.M.; Callahan, E.H.; Spill, M.K.; Wong, Y.P.; Benjamin-Neelon, S.E.; Birch, L.; Black, M.M.; Cook, J.T.; Faith, M.S.; Mennella, J.; et al. Influence of maternal diet on flavor transfer to amniotic fluid and breast milk and children’s responses: A systematic review. Am. J. Clin. Nutr. 2019, 109, 1003s–1026s. [Google Scholar] [CrossRef]
- Lott, M.; Callahan, E.; Duffy, E.W.; Story, M.; Daniels, S. Healthy Beverage Consumption in Early Childhood: Recommendations from Key National Health And Nutrition Organizations; Consensus Statement; Healthy Eating Research: Durham, NC, USA, 2019; Available online: http://healthyeatingresearch.org (accessed on 4 January 2021).
- Heyman, M.B.; Abrams, S.A. Fruit Juice in Infants, Children, and Adolescents: Current Recommendations. Pediatrics 2017, 139, e20170967. [Google Scholar] [CrossRef] [PubMed]
- Sonneville, K.R.; Long, M.; Rifas-Shiman, S.L.; Kleinman, K.; Gillman, M.W.; Taveras, E.M. Juice and water intake in infancy and later beverage intake and adiposity: Could juice be a gateway drink? Obesity 2015, 23, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Herrick, K.A.; Fryar, C.D.; Hamner, H.C.; Park, S.; Ogden, C.L. Added Sugars Intake among US Infants and Toddlers. J. Acad. Nutr. Diet. 2020, 120, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Anater, A.S.; Catellier, D.J.; Levine, B.A.; Krotki, K.P.; Jacquier, E.F.; Eldridge, A.; Bronstein, K.E.; Harnack, L.J.; Peasley, J.M.L.; Lutes, A.C. The Feeding Infants and Toddlers Study (FITS) 2016: Study Design and Methods. J. Nutr. 2018, 148, 1516S–1524S. [Google Scholar] [CrossRef] [PubMed]
- Suthutvoravut, U.; Abiodun, P.O.; Chomtho, S.; Chongviriyaphan, N.; Cruchet, S.; Davies, P.S.W.; Fuchs, G.J.; Gopalan, S.; van Goudoever, J.B.; Nel, E.R.; et al. Composition of Follow-Up Formula for Young Children Aged 12–36 Months: Recommendations of an International Expert Group Coordinated by the Nutrition Association of Thailand and the Early Nutrition Academy. Ann. Nutr. Metab. 2015, 67, 119–132. [Google Scholar] [CrossRef]
- Pérez-Escamilla, R.; Segura-Pérez, S.; Lott, M. Feeding Guidelines for Infants and Young Toddlers: A Responsive Parenting Approach. Nutr. Today 2017, 52, 223–231. [Google Scholar] [CrossRef]
- Tester, J.M.; Leung, C.W.; Crawford, P.B. Revised WIC Food Package and Children’s Diet Quality. Pediatrics 2016, 137, e20153557. [Google Scholar] [CrossRef] [PubMed]
- Andreyeva, T.; Luedicke, J.; Henderson, K.E.; Schwartz, M.B. The positive effects of the revised milk and cheese allowances in the special supplemental nutrition program for women, infants, and children. J. Acad. Nutr. Diet. 2014, 114, 622–630. [Google Scholar] [CrossRef] [PubMed]
- Andreyeva, T.; Luedicke, J. Federal food package revisions: Effects on purchases of whole-grain products. Am. J. Prev. Med. 2013, 45, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Andreyeva, T.; Luedicke, J.; Tripp, A.S.; Henderson, K.E. Effects of reduced juice allowances in food packages for the women, infants, and children program. Pediatrics 2013, 131, 919–927. [Google Scholar] [CrossRef]
- Weinfield, N.S.; Borger, C.; Au, L.E.; Whaley, S.E.; Berman, D.; Ritchie, L.D. Longer Participation in WIC Is Associated with Better Diet Quality in 24-Month-Old Children. J. Acad. Nutr. Diet. 2020, 120, 963–971. [Google Scholar] [CrossRef]
- Guthrie, J.F.; Catellier, D.J.; Jacquier, E.F.; Eldridge, A.L.; Johnson, W.L.; Lutes, A.C.; Anater, A.S.; Quann, E.E. WIC and non-WIC Infants and Children Differ in Usage of Some WIC-Provided Foods. J. Nutr. 2018, 148, 1547s–1556s. [Google Scholar] [CrossRef]
- United States Department of Agriculture. WIC Food Packages-Maximum Monthly Allowances. 2016. Available online: https://www.fns.usda.gov/wic/wic-food-packages-maximum-monthly-allowances (accessed on 3 January 2021).
- National Academies of Sciences, Engineering and Medicine. Review of WIC Food Packages: Improving Balance and Choice: Final Report; The National Academies Press: Washington, DC, USA, 2017; pp. 443–461. [Google Scholar]
- Keim, S.A.; Branum, A.M. Dietary intake of polyunsaturated fatty acids and fish among US children 12–60 months of age. Matern. Child. Nutr. 2015, 11, 987–998. [Google Scholar] [CrossRef]
- Fiocchi, A.; Assa’ad, A.; Bahna, S. Food allergy and the introduction of solid foods to infants: A consensus document. Adverse Reactions to Foods Committee, American College of Allergy, Asthma and Immunology. Ann. Allergy Asthma Immunol. 2006, 97, 10–20. [Google Scholar] [CrossRef]
- Hamner, H.C.; Perrine, C.G.; Gupta, P.M.; Herrick, K.A.; Cogswell, M.E. Food Consumption Patterns among U.S. Children from Birth to 23 Months of Age, 2009–2014. Nutrients 2017, 9, 942. [Google Scholar] [CrossRef]
- Davis, K.E.; Li, X.; Adams-Huet, B.; Sandon, L. Infant feeding practices and dietary consumption of US infants and toddlers: National Health and Nutrition Examination Survey (NHANES) 2003–2012. Public Health Nutr. 2018, 21, 711–720. [Google Scholar] [CrossRef]
- Santiago-Torres, M.; Kratz, M.; Lampe, J.W.; Tapsoba, J.D.D.; Breymeyer, K.L.; Levy, L.; Villaseñor, A.; Wang, C.-Y.; Song, X.; Neuhouser, M.L. Metabolic responses to a traditional Mexican diet compared with a commonly consumed US diet in women of Mexican descent: A randomized crossover feeding trial. Am. J. Clin. Nutr. 2016, 103, 366–374. [Google Scholar] [CrossRef]
- Mattei, J.; Sotres-Alvarez, D.; Daviglus, M.L.; Gallo, L.C.; Gellman, M.; Hu, F.B.; Tucker, K.L.; Willett, W.C.; Siega-Riz, A.M.; van Horn, L.; et al. Diet Quality and Its Association with Cardiometabolic Risk Factors Vary by Hispanic and Latino Ethnic Background in the Hispanic Community Health Study/Study of Latinos. J. Nutr. 2016, 146, 2035–2044. [Google Scholar] [CrossRef] [PubMed]
| Toddler Diet Quality Index | Healthy Eating Index 2015 | |||||
|---|---|---|---|---|---|---|
| Component | Max Points | Standard for Max Score | Standard for Min Score | Max Points | Standard for Max Score | Standard for Min Score |
| Food and Nutrients to Increase | ||||||
| Total Fruits 1 | NA | NA | 5 | ≥0.8 c eq per 1000 kcal | No fruit | |
| Whole Fruits 2 | 10 | ≥0.48 c eq per 1000 kcal | No whole fruit | 5 | ≥0.4 c eq per 1000 kcal | No whole fruit |
| Total Vegetables | 10 | ≥0.95 c eq per 1000 kcal | No vegetables | 5 | ≥1.1 c eq per 1000 kcal | No vegetables |
| Greens and Beans | 5 | ≥0.12 c eq per 1000 kcal | No dark green vegetables or legumes | 5 | ≥0.2 c eq per 1000 kcal | No dark green vegetables or legumes |
| Whole Grains | 10 | ≥2.0 oz eq/day | No whole grains | 10 | ≥1.5 oz eq per 1000 kcal | No whole grains |
| Dairy 3 | 10 | ≥2.1 oz eq per 1000 kcal | No dairy | 10 | ≥1.3 c eq per 1000 kcal | No dairy |
| Total Protein Foods | 5 | ≥2.0 oz eq/day | No protein foods | 5 | ≥2.5 oz eq per 1000 kcal | No protein foods |
| Seafood and Plant Proteins 4 | NA | NA | 5 | ≥0.8 c eq per 1000 kcal | No seafood or plant proteins | |
| Seafood | 2.5 | ≥0.29 c eq/day | No seafood | NA | NA | |
| Plant Proteins | 2.5 | ≥0.25 c eq per 1000 kcal | No plant proteins or legumes | NA | NA | |
| Linoleic Acid | 5 | ≥6.3% of energy | No linoleic acid | NA | NA | |
| Alpha Linolenic Acid | 5 | ≥0.63% of energy | No alpha linolenic acid | NA | NA | |
| Fatty Acids 5 | NA | NA | 10 | (PUFAs+MUFAs)/SFAs ≥2.5 | (PUFAs+MUFAs)/SFAs ≤1.2 | |
| Food and Nutrients to Limit or Decrease | ||||||
| 100% Fruit Juice | 5 | ≤4 oz/day | ≥6 oz/day | NA | NA | |
| Refined Grains | 10 | ≤0.6 oz eq per 1000 kcal | ≥2.0 oz eq per 1000 kcal | 10 | ≤1.8 oz eq per 1000 kcal | ≥4.3 oz eq per 1000 kcal |
| Sodium | 10 | ≤1.2 g/day | ≥1.5 g/day | 10 | ≤1.1 g per 1000 kcal | ≥2.0 g per 1000 kcal |
| Added Sugars | 10 | No added sugars | ≥6% of energy | 10 | ≤6.5% of energy | ≥26% of energy |
| Saturated Fats | 10 | ≤8% of energy | ≥16% of energy | |||
| Characteristic | % | SE | |
|---|---|---|---|
| Male | 50.8 | 1.7 | |
| Ever Breastfed | 77.1 | 1.4 | |
| Child First Born | 33.9 | 1.8 | |
| Child race/ethnicity | Hispanic | 15.0 | 1.2 |
| Non-Hispanic white | 65.9 | 1.6 | |
| Non-Hispanic Black | 15.1 | 1.2 | |
| Non-Hispanic Other | 4.0 | 0.7 | |
| Household income (in Dollars) | Under 10,000 | 9.2 | 1.0 |
| 10,000 to 19,999 | 8.5 | 0.9 | |
| 20,000 to 34,999 | 17.9 | 1.3 | |
| 35,000 to 49,999 | 16.9 | 1.3 | |
| 50,000 to 74,999 | 20.1 | 1.4 | |
| 75,000 to 99,999 | 12.6 | 1.1 | |
| 100,000 to 149,999 | 10.7 | 1.0 | |
| 150,000 or more | 4.2 | 0.7 | |
| Maternal education | High school or less | 22.6 | 1.4 |
| Some post-secondary | 23.5 | 1.4 | |
| College or graduate work | 53.9 | 1.7 | |
| WIC Participant | 35.1 | 1.6 | |
| Urbanicity | Urban | 80.3 | 1.3 |
| Rural | 19.7 | 1.3 | |
| Children 12–23.9 Months (n = 882) | Ever Breastfed | Race/ Ethnicity | WIC | Poverty Level | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No (n = 200) | Yes (n = 675) | Hispanic (n = 132) | Non-Hispanic White (n = 577) | Non-Hispanic Black (n = 131) | WIC (n = 306) | WIC Eligible (n = 160) | Non-WIC (n = 409) | Per 100% Increase (n = 875) | ||
| Total Toddler DQI | 48.6 (0.6) | 45.9 (1.0) | 49.5 (0.6) | 51.8 (1.1) | 47.4 (0.6) | 46.5 (1.4) | 46.6 (0.9) | 48.7 (1.1) | 51.2 (1.0) | 0.7 (0.3) |
| Foods and Nutrients to Increase | ||||||||||
| Total vegetable | 4.3 (0.1) | 4.0 (0.3) | 4.4 (0.2) | 4.5 (0.4) | 3.9 (0.2) | 5.1 (0.4) | 3.9 (0.2) | 4.6 (0.3) | 4.8 (0.3) | −0.1 (0.1) |
| Greens and beans | 1.1 (0.1) | 0.8 (0.2) | 1.3 (0.1) | 1.4 (0.2) | 0.9 (0.1) | 1.4 (0.2) | 0.9 (0.1) | 1.3 (0.2) | 1.4 (0.2) | 0.0 (0.1) |
| Whole fruit | 6.2 (0.2) | 5.5 (0.4) | 6.4 (0.2) | 6.1 (0.4) | 6.4 (0.2) | 5.8 (0.5) | 5.6 (0.3) | 6.8 (0.4) | 6.7 (0.3) | 0.2 (0.1) |
| Whole grains | 3.8 (0.2) | 2.9 (0.3) | 4.0 (0.2) | 3.7 (0.3) | 3.8 (0.2) | 3.6 (0.4) | 3.7 (0.3) | 3.6 (0.3) | 3.9 (0.3) | 0.1 (0.1) |
| Dairy | 7.9 (0.1) | 8.0 (0.2) | 7.9 (0.1) | 8.0 (0.3) | 8.1 (0.1) | 7.1 (0.3) | 7.9 (0.2) | 7.7 (0.3) | 8.2 (0.2) | 0.1 (0.1) |
| Total proteins | 3.8 (0.1) | 3.8 (0.1) | 3.9 (0.1) | 3.8 (0.2) | 3.9 (0.1) | 4.1 (0.2) | 3.9 (0.1) | 4.0 (0.2) | 3.7 (0.1) | 0.0 (0.1) |
| Seafood | 0.2 (0.0) | 0.1 (0.1) | 0.2 (0.0) | 0.1 (0.1) | 0.2 (0.0) | 0.3 (0.1) | 0.2 (0.1) | 0.2 (0.1) | 0.2 (0.1) | 0.0 (0.0) |
| Plant proteins | 0.8 (0.1) | 0.7 (0.1) | 0.8 (0.1) | 0.8 (0.1) | 0.8 (0.1) | 0.9 (0.1) | 0.8 (0.1) | 0.7 (0.1) | 0.8 (0.1) | 0.1 (0.0) |
| Linoleic acid | 3.6 (0.1) | 3.8 (0.1) | 3.6 (0.1) | 3.6 (0.1) | 3.7 (0.1) | 3.7 (0.1) | 3.6 (0.1) | 3.8 (0.1) | 3.6 (0.1) | −0.1 (0.0) |
| Alpha-linolenic acid | 4.4 (0.0) | 4.5 (0.1) | 4.4 (0.1) | 4.5 (0.1) | 4.4 (0.1) | 4.4 (0.1) | 4.4 (0.1) | 4.4 (0.1) | 4.4 (0.1) | 0.0 (0.0) |
| Foods and Nutrients to Limit or Decrease | ||||||||||
| 100% fruit juice | 3.4 (0.1) | 3.1 (0.2) | 3.4 (0.1) | 3.2 (0.2) | 3.5 (0.1) | 3.3 (0.3) | 3.0 (0.2) | 3.4 (0.2) | 3.8 (0.2) | 0.1 (0.1) |
| Sodium | 4.4 (0.2) | 4.7 (0.4) | 4.3 (0.2) | 5.5 (0.5) | 3.8 (0.2) | 3.5 (0.5) | 4.2 (0.3) | 3.7 (0.4) | 5.0 (0.4) | 0.2 (0.1) |
| Refined grains | 2.4 (0.2) | 1.9 (0.3) | 2.5 (0.2) | 3.2 (0.4) | 2.1 (0.2) | 2.1 (0.4) | 2.2 (0.3) | 2.5 (0.3) | 2.6 (0.3) | 0.1 (0.1) |
| Added sugars | 2.3 (0.1) | 2.2 (0.3) | 2.4 (0.1) | 3.4 (0.4) | 2.0 (0.1) | 1.4 (0.3) | 2.4 (0.2) | 2.2 (0.3) | 2.3 (0.2) | 0.1 (0.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kay, M.C.; Duffy, E.W.; Harnack, L.J.; Anater, A.S.; Hampton, J.C.; Eldridge, A.L.; Story, M. Development and Application of a Total Diet Quality Index for Toddlers. Nutrients 2021, 13, 1943. https://doi.org/10.3390/nu13061943
Kay MC, Duffy EW, Harnack LJ, Anater AS, Hampton JC, Eldridge AL, Story M. Development and Application of a Total Diet Quality Index for Toddlers. Nutrients. 2021; 13(6):1943. https://doi.org/10.3390/nu13061943
Chicago/Turabian StyleKay, Melissa C., Emily W. Duffy, Lisa J. Harnack, Andrea S. Anater, Joel C. Hampton, Alison L. Eldridge, and Mary Story. 2021. "Development and Application of a Total Diet Quality Index for Toddlers" Nutrients 13, no. 6: 1943. https://doi.org/10.3390/nu13061943
APA StyleKay, M. C., Duffy, E. W., Harnack, L. J., Anater, A. S., Hampton, J. C., Eldridge, A. L., & Story, M. (2021). Development and Application of a Total Diet Quality Index for Toddlers. Nutrients, 13(6), 1943. https://doi.org/10.3390/nu13061943






