Changes in Lifestyle and Dietary Habits during COVID-19 Lockdown in Italy: Results of an Online Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Diet
2.2. Physical Activity
2.3. Distress
2.4. Sleep Quality
2.5. Data Analysis
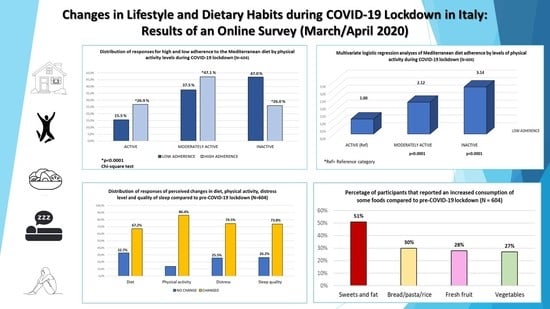
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, Y.; Shi, L.; Que, J.; Lu, Q.; Liu, L.; Lu, Z.; Xu, Y.; Liu, J.; Sun, Y.; Meng, S.; et al. The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic. Mol. Psychiatry 2021. [Google Scholar] [CrossRef]
- Clemente-Suarez, V.J.; Dalamitros, A.A.; Beltran-Velasco, A.I.; Mielgo-Ayuso, J.; Tornero-Aguilera, J.F. Social and Psychophysiological Consequences of the COVID-19 Pandemic: An Extensive Literature Review. Front. Psychol. 2020, 11, 580225. [Google Scholar] [CrossRef]
- Zhang, S.X.; Wang, Y.; Rauch, A.; Wei, F. Unprecedented disruption of lives and work: Health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020, 288, 112958. [Google Scholar] [CrossRef]
- Rodriguez-Perez, C.; Molina-Montes, E.; Verardo, V.; Artacho, R.; Garcia-Villanova, B.; Guerra-Hernandez, E.J.; Ruiz-Lopez, M.D. Changes in Dietary Behaviours during the COVID-19 Outbreak Confinement in the Spanish COVIDiet Study. Nutrients 2020, 12, 1730. [Google Scholar] [CrossRef] [PubMed]
- Lamarche, B.; Brassard, D.; Lapointe, A.; Laramee, C.; Kearney, M.; Cote, M.; Belanger-Gravel, A.; Desroches, S.; Lemieux, S.; Plante, C. Changes in diet quality and food security among adults during the COVID-19-related early lockdown: Results from NutriQuebec. Am. J. Clin. Nutr. 2021, 113, 984–992. [Google Scholar] [CrossRef] [PubMed]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attina, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef]
- Lopez-Bueno, R.; Calatayud, J.; Casana, J.; Casajus, J.A.; Smith, L.; Tully, M.A.; Andersen, L.L.; Lopez-Sanchez, G.F. COVID-19 Confinement and Health Risk Behaviors in Spain. Front. Psychol. 2020, 11, 1426. [Google Scholar] [CrossRef] [PubMed]
- Izzo, L.; Santonastaso, A.; Cotticelli, G.; Federico, A.; Pacifico, S.; Castaldo, L.; Colao, A.; Ritieni, A. An Italian Survey on Dietary Habits and Changes during the COVID-19 Lockdown. Nutrients 2021, 13, 1197. [Google Scholar] [CrossRef]
- Fuzeki, E.; Schroder, J.; Carraro, N.; Merlo, L.; Reer, R.; Groneberg, D.A.; Banzer, W. Physical Activity during the First COVID-19-Related Lockdown in Italy. Int. J. Environ. Res. Public Health 2021, 18, 2511. [Google Scholar] [CrossRef]
- Ruiz-Roso, M.B.; de Carvalho Padilha, P.; Mantilla-Escalante, D.C.; Ulloa, N.; Brun, P.; Acevedo-Correa, D.; Arantes Ferreira Peres, W.; Martorell, M.; Aires, M.T.; de Oliveira Cardoso, L.; et al. Covid-19 Confinement and Changes of Adolescent’s Dietary Trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients 2020, 12, 1807. [Google Scholar] [CrossRef]
- Pfeifer, D.; Resetar, J.; Gajdos Kljusuric, J.; Panjkota Krbavcic, I.; Vranesic Bender, D.; Rodriguez-Perez, C.; Ruiz-Lopez, M.D.; Satalic, Z. Cooking at Home and Adherence to the Mediterranean Diet During the COVID-19 Confinement: The Experience from the Croatian COVIDiet Study. Front. Nutr. 2021, 8, 617721. [Google Scholar] [CrossRef] [PubMed]
- Koball, A.M.; Meers, M.R.; Storfer-Isser, A.; Domoff, S.E.; Musher-Eizenman, D.R. Eating when bored: Revision of the emotional eating scale with a focus on boredom. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2012, 31, 521–524. [Google Scholar] [CrossRef]
- Yannakoulia, M.; Panagiotakos, D.B.; Pitsavos, C.; Tsetsekou, E.; Fappa, E.; Papageorgiou, C.; Stefanadis, C. Eating habits in relations to anxiety symptoms among apparently healthy adults. A pattern analysis from the ATTICA Study. Appetite 2008, 51, 519–525. [Google Scholar] [CrossRef]
- Moynihan, A.B.; van Tilburg, W.A.; Igou, E.R.; Wisman, A.; Donnelly, A.E.; Mulcaire, J.B. Eaten up by boredom: Consuming food to escape awareness of the bored self. Front. Psychol. 2015, 6, 369. [Google Scholar] [CrossRef]
- Montemurro, N. The emotional impact of COVID-19: From medical staff to common people. Brain Behav. Immun. 2020, 87, 23–24. [Google Scholar] [CrossRef] [PubMed]
- Lima, C.K.T.; Carvalho, P.M.M.; Lima, I.; Nunes, J.; Saraiva, J.S.; de Souza, R.I.; da Silva, C.G.L.; Neto, M.L.R. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry Res. 2020, 287, 112915. [Google Scholar] [CrossRef] [PubMed]
- Detopoulou, P.; Demopoulos, C.A.; Antonopoulou, S. Micronutrients, Phytochemicals and Mediterranean Diet: A Potential Protective Role against COVID-19 through Modulation of PAF Actions and Metabolism. Nutrients 2021, 13, 462. [Google Scholar] [CrossRef] [PubMed]
- Jayawardena, R.; Sooriyaarachchi, P.; Chourdakis, M.; Jeewandara, C.; Ranasinghe, P. Enhancing immunity in viral infections, with special emphasis on COVID-19: A review. Diabetes Metab. Syndr. 2020, 14, 367–382. [Google Scholar] [CrossRef] [PubMed]
- Gnagnarella, P.; Draga, D.; Misotti, A.M.; Sieri, S.; Spaggiari, L.; Cassano, E.; Baldini, F.; Soldati, L.; Maisonneuve, P. Validation of a short questionnaire to record adherence to the Mediterranean diet: An Italian experience. Nutr. Metab. Cardiovasc. Dis. NMCD 2018, 28, 1140–1147. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Bamia, C.; Lagiou, P.; Trichopoulos, D. Conformity to traditional Mediterranean diet and breast cancer risk in the Greek EPIC (European Prospective Investigation into Cancer and Nutrition) cohort. Am. J. Clin. Nutr. 2010, 92, 620–625. [Google Scholar] [CrossRef] [Green Version]
- Hagstromer, M.; Oja, P.; Sjostrom, M. The International Physical Activity Questionnaire (IPAQ): A study of concurrent and construct validity. Public Health Nutr. 2006, 9, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.L.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Kopp, W. How Western Diet And Lifestyle Drive The Pandemic Of Obesity And Civilization Diseases. Diabetes Metab. Syndr. Obes. Targets Ther. 2019, 12, 2221–2236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alberti-Fidanza, A.; Fidanza, F. Mediterranean Adequacy Index of Italian diets. Public Health Nutr. 2004, 7, 937–941. [Google Scholar] [CrossRef]
- Scrimshaw, N.S.; SanGiovanni, J.P. Synergism of nutrition, infection, and immunity: An overview. Am. J. Clin. Nutr. 1997, 66, 464S–477S. [Google Scholar] [CrossRef] [Green Version]
- Kontou, N.; Psaltopoulou, T.; Panagiotakos, D.; Dimopoulos, M.A.; Linos, A. The mediterranean diet in cancer prevention: A review. J. Med. Food 2011, 14, 1065–1078. [Google Scholar] [CrossRef]
- De Lorgeril, M. PREDIMED trial: Mediterranean diet may reduce the risk of type 2 diabetes. Evid. Based Med. 2011, 16, 152–153. [Google Scholar] [CrossRef]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean diet and health status: An updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014, 17, 2769–2782. [Google Scholar] [CrossRef] [Green Version]
- Sanchez-Villegas, A.; Cabrera-Suarez, B.; Molero, P.; Gonzalez-Pinto, A.; Chiclana-Actis, C.; Cabrera, C.; Lahortiga-Ramos, F.; Florido-Rodriguez, M.; Vega-Perez, P.; Vega-Perez, R.; et al. Preventing the recurrence of depression with a Mediterranean diet supplemented with extra-virgin olive oil. The PREDI-DEP trial: Study protocol. BMC Psychiatry 2019, 19, 63. [Google Scholar] [CrossRef]
- Vazquez-Calvo, A.; Jimenez de Oya, N.; Martin-Acebes, M.A.; Garcia-Moruno, E.; Saiz, J.C. Antiviral Properties of the Natural Polyphenols Delphinidin and Epigallocatechin Gallate against the Flaviviruses West Nile Virus, Zika Virus, and Dengue Virus. Front. Microbiol. 2017, 8, 1314. [Google Scholar] [CrossRef]
- Villamor, E.; Fawzi, W.W. Effects of vitamin a supplementation on immune responses and correlation with clinical outcomes. Clin. Microbiol. Rev. 2005, 18, 446–464. [Google Scholar] [CrossRef] [Green Version]
- Hewison, M. An update on vitamin D and human immunity. Clin. Endocrinol. 2012, 76, 315–325. [Google Scholar] [CrossRef] [PubMed]
- Meydani, S.N.; Beharka, A.A. Recent developments in vitamin E and immune response. Nutr. Rev. 1998, 56, S49–S58. [Google Scholar] [CrossRef] [PubMed]
- Meydani, S.N.; Han, S.N.; Wu, D. Vitamin E and immune response in the aged: Molecular mechanisms and clinical implications. Immunol. Rev. 2005, 205, 269–284. [Google Scholar] [CrossRef]
- Pecora, F.; Persico, F.; Argentiero, A.; Neglia, C.; Esposito, S. The Role of Micronutrients in Support of the Immune Response against Viral Infections. Nutrients 2020, 12, 3198. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.C.; Sheen, J.M.; Hu, W.L.; Hung, Y.C. Polyphenols and Oxidative Stress in Atherosclerosis-Related Ischemic Heart Disease and Stroke. Oxidative Med. Cell. Longev. 2017, 2017, 8526438. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serino, A.; Salazar, G. Protective Role of Polyphenols against Vascular Inflammation, Aging and Cardiovascular Disease. Nutrients 2018, 11, 53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Navarro, S.L.; Li, F.; Lampe, J.W. Mechanisms of action of isothiocyanates in cancer chemoprevention: An update. Food Funct. 2011, 2, 579–587. [Google Scholar] [CrossRef]
- Talalay, P.; Fahey, J.W. Phytochemicals from cruciferous plants protect against cancer by modulating carcinogen metabolism. J. Nutr. 2001, 131, 3027S–3033S. [Google Scholar] [CrossRef]
- Jasso-Miranda, C.; Herrera-Camacho, I.; Flores-Mendoza, L.K.; Dominguez, F.; Vallejo-Ruiz, V.; Sanchez-Burgos, G.G.; Pando-Robles, V.; Santos-Lopez, G.; Reyes-Leyva, J. Antiviral and immunomodulatory effects of polyphenols on macrophages infected with dengue virus serotypes 2 and 3 enhanced or not with antibodies. Infect. Drug Resist. 2019, 12, 1833–1852. [Google Scholar] [CrossRef]
- Bowden Davies, K.A.; Sprung, V.S.; Norman, J.A.; Thompson, A.; Mitchell, K.L.; Halford, J.C.G.; Harrold, J.A.; Wilding, J.P.H.; Kemp, G.J.; Cuthbertson, D.J. Short-term decreased physical activity with increased sedentary behaviour causes metabolic derangements and altered body composition: Effects in individuals with and without a first-degree relative with type 2 diabetes. Diabetologia 2018, 61, 1282–1294. [Google Scholar] [CrossRef] [Green Version]
- De Luca, C.; Olefsky, J.M. Inflammation and insulin resistance. FEBS Lett. 2008, 582, 97–105. [Google Scholar] [CrossRef] [Green Version]
- Weiss, P.; Murdoch, D.R. Clinical course and mortality risk of severe COVID-19. Lancet 2020, 395, 1014–1015. [Google Scholar] [CrossRef]
- Giugliano, D.; Ceriello, A.; Esposito, K. The effects of diet on inflammation: Emphasis on the metabolic syndrome. J. Am. Coll. Cardiol. 2006, 48, 677–685. [Google Scholar] [CrossRef] [Green Version]
- Tan, B.L.; Norhaizan, M.E. Effect of High-Fat Diets on Oxidative Stress, Cellular Inflammatory Response and Cognitive Function. Nutrients 2019, 11, 2579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Casas, R.; Sacanella, E.; Estruch, R. The immune protective effect of the Mediterranean diet against chronic low-grade inflammatory diseases. Endocr. Metab. Immune Disord. Drug Targets 2014, 14, 245–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Casas, R.; Estruch, R.; Sacanella, E. The Protective Effects of Extra Virgin Olive Oil on Immune-mediated Inflammatory Responses. Endocr. Metab. Immune Disord. Drug Targets 2018, 18, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R. Anti-inflammatory effects of the Mediterranean diet: The experience of the PREDIMED study. Proc. Nutr. Soc. 2010, 69, 333–340. [Google Scholar] [CrossRef] [Green Version]
- Angelidi, A.M.; Kokkinos, A.; Katechaki, E.; Ros, E.; Mantzoros, C.S. Mediterranean diet as a nutritional approach for COVID-19. Metab. Clin. Exp. 2021, 114, 154407. [Google Scholar] [CrossRef]
- Maiorino, M.I.; Bellastella, G.; Longo, M.; Caruso, P.; Esposito, K. Mediterranean Diet and COVID-19: Hypothesizing Potential Benefits in People with Diabetes. Front. Endocrinol. 2020, 11, 574315. [Google Scholar] [CrossRef]
- Sadeghi, O.; Keshteli, A.H.; Afshar, H.; Esmaillzadeh, A.; Adibi, P. Adherence to Mediterranean dietary pattern is inversely associated with depression, anxiety and psychological distress. Nutr. Neurosci. 2019, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- Gonzalez-Sanguino, C.; Ausin, B.; Castellanos, M.A.; Saiz, J.; Lopez-Gomez, A.; Ugidos, C.; Munoz, M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020, 87, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Gualano, M.R.; Lo Moro, G.; Voglino, G.; Bert, F.; Siliquini, R. Effects of Covid-19 Lockdown on Mental Health and Sleep Disturbances in Italy. Int. J. Environ. Res. Public Health 2020, 17, 4779. [Google Scholar] [CrossRef]
- Warburton, D.E.; Nicol, C.W.; Bredin, S.S. Health benefits of physical activity: The evidence. CMAJ Can. Med. Assoc. J. J. Assoc. Med Can. 2006, 174, 801–809. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef] [PubMed]
- Romero-Blanco, C.; Rodriguez-Almagro, J.; Onieva-Zafra, M.D.; Parra-Fernandez, M.L.; Prado-Laguna, M.D.C.; Hernandez-Martinez, A. Physical Activity and Sedentary Lifestyle in University Students: Changes during Confinement Due to the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6567. [Google Scholar] [CrossRef]
- Galle, F.; Sabella, E.A.; Ferracuti, S.; de Giglio, O.; Caggiano, G.; Protano, C.; Valeriani, F.; Parisi, E.A.; Valerio, G.; Liguori, G.; et al. Sedentary Behaviors and Physical Activity of Italian Undergraduate Students during Lockdown at the Time of CoViD-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6171. [Google Scholar] [CrossRef] [PubMed]
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon 2020, 6, e04315. [Google Scholar] [CrossRef]
- Tison, G.H.; Avram, R.; Kuhar, P.; Abreau, S.; Marcus, G.M.; Pletcher, M.J.; Olgin, J.E. Worldwide Effect of COVID-19 on Physical Activity: A Descriptive Study. Ann. Intern. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Ryu, S.; Cheong, E.; Sung, K.C. Association of Physical Activity and Inflammation with All-Cause, Cardiovascular-Related, and Cancer-Related Mortality. Mayo Clin. Proc. 2016, 91, 1706–1716. [Google Scholar] [CrossRef]
- Da Silveira, M.P.; da Silva Fagundes, K.K.; Bizuti, M.R.; Starck, E.; Rossi, R.C.; de Resende, E.S.D.T. Physical exercise as a tool to help the immune system against COVID-19: An integrative review of the current literature. Clin. Exp. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, B.K.; Hoffman-Goetz, L. Exercise and the immune system: Regulation, integration, and adaptation. Physiol. Rev. 2000, 80, 1055–1081. [Google Scholar] [CrossRef] [Green Version]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. Jama 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Perales, F.; Pozo-Cruz, J.D.; Pozo-Cruz, B.D. Impact of physical activity on psychological distress: A prospective analysis of an Australian national sample. Am. J. Public Health 2014, 104, e91–e97. [Google Scholar] [CrossRef]
- Kredlow, M.A.; Capozzoli, M.C.; Hearon, B.A.; Calkins, A.W.; Otto, M.W. The effects of physical activity on sleep: A meta-analytic review. J. Behav. Med. 2015, 38, 427–449. [Google Scholar] [CrossRef]
- Matta, J.; Hoertel, N.; Kesse-Guyot, E.; Plesz, M.; Wiernik, E.; Carette, C.; Czernichow, S.; Limosin, F.; Goldberg, M.; Zins, M.; et al. Diet and physical activity in the association between depression and metabolic syndrome: Constances study. J. Affect. Disord. 2019, 244, 25–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibson-Smith, D.; Bot, M.; Brouwer, I.A.; Visser, M.; Giltay, E.J.; Penninx, B. Association of food groups with depression and anxiety disorders. Eur. J. Nutr. 2020, 59, 767–778. [Google Scholar] [CrossRef] [Green Version]
- Hamer, M.; Kivimaki, M.; Gale, C.R.; Batty, G.D. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK. Brain Behav. Immun. 2020, 87, 184–187. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity 2020. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Wang, Y.; Xue, J.; Zhao, N.; Zhu, T. The Impact of COVID-19 Epidemic Declaration on Psychological Consequences: A Study on Active Weibo Users. Int. J. Environ. Res. Public Health 2020, 17, 2032. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moser, J.S.; Galindo-Fraga, A.; Ortiz-Hernandez, A.A.; Gu, W.; Hunsberger, S.; Galan-Herrera, J.F.; Guerrero, M.L.; Ruiz-Palacios, G.M.; Beigel, J.H.; La Red, I.L.I.S.G. Underweight, overweight, and obesity as independent risk factors for hospitalization in adults and children from influenza and other respiratory viruses. Influenza Other Respir. Viruses 2019, 13, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Taeymans, J.; Luijckx, E.; Rogan, S.; Haas, K.; Baur, H. Physical Activity, Nutritional Habits, and Sleeping Behavior in Students and Employees of a Swiss University During the COVID-19 Lockdown Period: Questionnaire Survey Study. JMIR Public Health Surveill. 2021, 7, e26330. [Google Scholar] [CrossRef] [PubMed]
- Barkley, J.E.; Lepp, A.; Glickman, E.; Farnell, G.; Beiting, J.; Wiet, R.; Dowdell, B. The Acute Effects of the COVID-19 Pandemic on Physical Activity and Sedentary Behavior in University Students and Employees. Int. J. Exerc. Sci. 2020, 13, 1326–1339. [Google Scholar]
- Pelucchi, C.; Galeone, C.; Negri, E.; La Vecchia, C. Trends in adherence to the Mediterranean diet in an Italian population between 1991 and 2006. Eur. J. Clin. Nutr. 2010, 64, 1052–1056. [Google Scholar] [CrossRef] [Green Version]
| Women n = 433 | Men n = 171 | Total n = 604 | p * | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Age | 29.7 | ±10.2 | 30.1 | ±11.0 | 29.8 | ±10.4 | 0.65 † |
| n | (%) | n | (%) | N | (%) | ||
| Age group | |||||||
| <26 | 200 | 46.2 | 73 | 42.7 | 273 | 45.2 | 0.51 |
| 26–35 | 147 | 33.9 | 57 | 33.3 | 204 | 33.8 | |
| >35 | 86 | 19.9 | 41 | 23.9 | 127 | 21.0 | |
| Total | 433 | 100 | 171 | 100 | 604 | 100 | |
| Marital Status | |||||||
| Unmarried | 341 | 78.8 | 134 | 78.4 | 475 | 78.6 | 0.96 |
| Married | 18 | 4.2 | 8 | 4.7 | 26 | 4.3 | |
| Divorced/Widow | 74 | 17.1 | 29 | 16.9 | 103 | 17.1 | |
| Total | 433 | 100 | 171 | 100 | 604 | 100 | |
| Occupation | |||||||
| Students | 192 | 44.3 | 68 | 39.8 | 260 | 43.1 | 0.53 |
| Workers | 141 | 32.6 | 63 | 36.8 | 204 | 33.8 | |
| Other | 100 | 23.1 | 40 | 23.4 | 140 | 23.2 | |
| Total | 433 | 100 | 171 | 100 | 604 | 100 | |
| Area of residence | |||||||
| South | 364 | 84.0 | 131 | 76.6 | 495 | 81.5 | 0.09 |
| Center/North | 69 | 15.9 | 40 | 23.4 | 109 | 18.1 | |
| Total | 433 | 100 | 171 | 100 | 604 | 100 | |
| Women n = 433 | Men n = 171 | Total n = 604 | ||||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |
| Diet adherence a | ||||||
| Low | 264 | 61.0 | 117 | 68.4 | 381 | 63.1 |
| High | 169 | 39.0 | 54 | 31.6 | 223 | 36.9 |
| Total | 433 | 100.0 | 171 | 100.0 | 604 | 100.0 |
| Self-reported dietary changes | ||||||
| No | 134 | 31.0 | 63 | 36.8 | 197 | 32.7 |
| Yes | 298 | 69.0 | 108 | 63.2 | 406 | 67.3 |
| Dietary changes | ||||||
| Reduced | 174 | 40.2 | 70 | 40.9 | 244 | 40.4 |
| No change | 118 | 27.3 | 41 | 24.0 | 159 | 26.3 |
| Increased | 141 | 32.6 | 60 | 35.1 | 201 | 33.3 |
| Physical activity b | ||||||
| Active | 81 | 18.7 | 38 | 22.2 | 119 | 19.7 |
| Moderately active | 178 | 41.1 | 70 | 40.9 | 248 | 41.1 |
| Inactive | 174 | 40.2 | 63 | 36.8 | 237 | 39.2 |
| Total | 433 | 100.0 | 171 | 100.0 | 604 | 100.0 |
| Physical activity changes | ||||||
| No change | 65 | 15.0 | 17 | 9.9 | 82 | 13.6 |
| Less sedentary | 70 | 16.2 | 16 | 9.4 | 86 | 14.2 |
| More sedentary | 298 | 68.8 | 138 | 80.7 | 436 | 72.2 |
| Distress c | ||||||
| Low | 124 | 28.6 | 92 | 53.8 | 216 | 35.8 |
| Medium | 183 | 42.3 | 43 | 25.1 | 226 | 37.4 |
| High | 126 | 29.1 | 36 | 21.1 | 162 | 26.8 |
| Total | 433 | 100.0 | 171 | 100.0 | 604 | 100.0 |
| Distress changes | ||||||
| As usual | 94 | 21.7 | 60 | 35.1 | 154 | 25.5 |
| Much less than usual | 31 | 7.2 | 24 | 14.0 | 55 | 9.1 |
| Much more than usual | 88 | 20.3 | 24 | 14.0 | 112 | 18.5 |
| A little less than usual | 15 | 3.5 | 3 | 1.8 | 18 | 3.0 |
| A little more than usual | 205 | 47.3 | 60 | 35.1 | 265 | 43.9 |
| Sleep quality d | ||||||
| Low | 278 | 64.2 | 92 | 53.8 | 370 | 61.3 |
| High | 155 | 35.8 | 79 | 46.2 | 234 | 38.7 |
| Total | 433 | 100.0 | 171 | 100.0 | 604 | 100.0 |
| Sleep quality changes | ||||||
| No changes | 103 | 23.8 | 55 | 32.2 | 158 | 26.2 |
| Sleep more | 87 | 20.1 | 34 | 19.9 | 121 | 20.0 |
| Sleep better | 14 | 3.2 | 12 | 7.0 | 26 | 4.3 |
| Sleep less | 56 | 12.9 | 18 | 10.5 | 74 | 12.3 |
| Sleep worse | 174 | 40.0 | 52 | 30.4 | 225 | 37.3 |
| Mediterranean Diet Adherence a | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women n = 433 | Men n = 171 | Total n = 604 | |||||||||||||
| Low | High | p * | Low | High | p * | Low | High | p * | |||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | ||||
| Self-reported dietary changes | |||||||||||||||
| No | 83 | 31.6 | 51 | 30.2 | 0.84 | 39 | 33.3 | 24 | 44.4 | 0.22 | 122 | 32.1 | 75 | 33.6 | 0.77 |
| Yes | 180 | 68.4 | 118 | 69.8 | 78 | 66.7 | 30 | 55.6 | 258 | 67.9 | 148 | 66.4 | |||
| Total | 263 | 100.0 | 169 | 100.0 | 117 | 100.0 | 54 | 100.0 | 380 | 100.0 | 223 | 100.0 | |||
| Dietary changes | |||||||||||||||
| Reduced | 105 | 39.8 | 69 | 40.8 | 0.25 | 52 | 44.4 | 18 | 33.3 | <0.01 | 157 | 41.2 | 87 | 39.0 | 0.015 |
| No change | 66 | 25.0 | 52 | 30.8 | 20 | 17.1 | 21 | 38.9 | 86 | 22.6 | 73 | 32.7 | |||
| Increased | 93 | 35.2 | 48 | 28.4 | 45 | 38.5 | 15 | 27.8 | 138 | 36.2 | 63 | 28.3 | |||
| Total | 264 | 100.0 | 169 | 100.0 | 117 | 100.0 | 54 | 100.0 | 381 | 100.0 | 223 | 100.0 | |||
| Physical activity b | |||||||||||||||
| Active | 41 | 15.5 | 40 | 23.7 | <0.0001 | 18 | 15.4 | 20 | 37.0 | <0.01 | 59 | 15.5 | 60 | 26.9 | <0.0001 |
| Moderately active | 94 | 35.6 | 84 | 49.7 | 49 | 41.9 | 21 | 38.9 | 143 | 37.5 | 105 | 47.1 | |||
| Inactive | 129 | 48.9 | 45 | 26.6 | 50 | 42.7 | 13 | 24.1 | 179 | 47.0 | 58 | 26.0 | |||
| Total | 264 | 100.0 | 169 | 100.0 | 117 | 100.0 | 54 | 100.0 | 381 | 100.0 | 223 | 100.0 | |||
| Distress c | |||||||||||||||
| Low | 78 | 29.5 | 46 | 27.2 | 0.84 | 59 | 50.4 | 33 | 61.1 | 0.32 | 137 | 36.0 | 79 | 35.4 | 0.79 |
| Medium | 109 | 41.3 | 74 | 43.8 | 30 | 25.6 | 13 | 24.1 | 139 | 36.5 | 87 | 39.0 | |||
| High | 77 | 29.2 | 49 | 29.0 | 28 | 23.9 | 8 | 14.8 | 105 | 27.6 | 57 | 25.6 | |||
| Total | 264 | 100.0 | 169 | 100.0 | 117 | 100.0 | 54 | 100.0 | 381 | 100.0 | 223 | 100.0 | |||
| Sleep quality d | |||||||||||||||
| Low | 168 | 63.6 | 110 | 65.1 | 0.84 | 70 | 59.8 | 22 | 40.7 | <0.05 | 238 | 62.5 | 132 | 59.2 | 0.28 |
| High | 96 | 36.4 | 59 | 34.9 | 47 | 40.2 | 32 | 59.3 | 143 | 37.5 | 91 | 40.8 | |||
| Total | 264 | 100.0 | 169 | 100.0 | 117 | 100.0 | 54 | 100.0 | 381 | 100.0 | 223 | 100.0 | |||
| Self-Reported Dietary Changes | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women n = 433 | Men n = 171 | Total n = 604 | |||||||||||||
| No | Yes | p * | No | Yes | p * | No | Yes | p * | |||||||
| n | (%) | n | (%) | n | (%) | N | (%) | n | (%) | n | (%) | ||||
| Physical activity a | |||||||||||||||
| Active | 28 | 20.9 | 53 | 17.8 | 0.69 | 11 | 17.5 | 27 | 25.0 | 0.22 | 39 | 19.8 | 80 | 19.7 | 0.92 |
| Moderately active | 52 | 38.8 | 126 | 42.3 | 31 | 49.2 | 39 | 36.1 | 83 | 42.1 | 165 | 40.6 | |||
| Inactive | 54 | 40.3 | 119 | 39.9 | 21 | 33.3 | 42 | 38.9 | 75 | 38.1 | 161 | 39.7 | |||
| Total | 134 | 100.0 | 298 | 100.0 | 63 | 100.0 | 108 | 100.0 | 197 | 100.0 | 406 | 100.0 | |||
| Distress b | |||||||||||||||
| Low | 49 | 36.6 | 75 | 25.2 | <0.05 | 38 | 60.3 | 54 | 50.0 | 0.23 | 87 | 44.2 | 129 | 31.8 | <0.01 |
| Medium | 54 | 40.3 | 128 | 43.0 | 16 | 25.4 | 27 | 25.0 | 70 | 35.5 | 155 | 38.2 | |||
| High | 31 | 23.1 | 95 | 31.9 | 9 | 14.3 | 27 | 25.0 | 40 | 20.3 | 122 | 30.0 | |||
| Total | 134 | 100.0 | 298 | 100.0 | 63 | 100.0 | 108 | 100.0 | 197 | 100.0 | 406 | 100.0 | |||
| Sleep quality c | |||||||||||||||
| Low | 80 | 59.7 | 198 | 66.4 | 0.21 | 32 | 50.8 | 60 | 55.6 | 0.65 | 112 | 56.9 | 258 | 63.5 | 0.13 |
| High | 54 | 40.3 | 100 | 33.6 | 31 | 49.2 | 48 | 44.4 | 85 | 43.1 | 148 | 36.5 | |||
| Total | 134 | 100.0 | 298 | 100.0 | 63 | 100.0 | 108 | 100.0 | 197 | 100.0 | 406 | 100.0 | |||
| Physical Activity Level a | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women n = 433 | Men n = 171 | Total n = 604 | |||||||||||||||||||
| Inactive | Moderately Active | Active | p * | Inactive | Moderately Active | Active | p * | Inactive | Moderately Active | Active | p * | ||||||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | ||||
| Distress b | |||||||||||||||||||||
| Low | 72 | 14.4 | 62 | 35.2 | 39 | 46.9 | 0.46 | 29 | 46.0 | 45 | 64.3 | 33 | 86.8 | <0.001 | 101 | 42.6 | 107 | 43.5 | 72 | 59.5 | <0.008 |
| Medium | 77 | 14.3 | 88 | 50 | 34 | 40.9 | 16 | 25.4 | 18 | 25.7 | 5 | 13.2 | 93 | 39.2 | 106 | 43.1 | 39 | 32.2 | |||
| High | 25 | 14.4 | 26 | 14.8 | 10 | 12.1 | 18 | 28.6 | 7 | 10 | 0 | 0 | 43 | 18.1 | 33 | 13.4 | 10 | 8.3 | |||
| Total | 174 | 100 | 176 | 100 | 83 | 100 | 63 | 100 | 70 | 100 | 38 | 100 | 237 | 100 | 246 | 100 | 121 | 100 | |||
| Sleep Quality c | |||||||||||||||||||||
| Low | 148 | 85.1 | 156 | 88.6 | 68 | 81.9 | 0.32 | 55 | 87.3 | 67 | 95.7 | 36 | 94.7 | 0.16 | 203 | 85.7 | 223 | 90.7 | 104 | 14.1 | 0.27 |
| High | 26 | 14.9 | 20 | 11.4 | 15 | 18.1 | 8 | 12.7 | 3 | 4.3 | 2 | 5.3 | 34 | 14.3 | 23 | 9.3 | 17 | 85.9 | |||
| Total | 174 | 100 | 176 | 100 | 83 | 100 | 63 | 100 | 70 | 100 | 38 | 100 | 237 | 100 | 246 | 100 | 121 | 100 | |||
| Low Mediterranean Diet Adherence a | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women n = 433 | Men n = 171 | Total n = 604 | ||||||||||
| OR b | 95% CI | p c | OR b | 95% CI | p c | OR b | 95% CI | p c | ||||
| Lower Limit | Upper Limit | Lower Limit | Upper Limit | Lower Limit | Upper Limit | |||||||
| Physical activity d | ||||||||||||
| Active | 1(Ref e) | 1(Ref) | 1(Ref) | |||||||||
| Moderately active | 2.50 | 1.59 | 3.92 | <0.0001 | 1.75 | 0.75 | 4.13 | 0.195 | 2.12 | 1.422 | 3.16 | <0.0001 |
| Inactive | 2.93 | 1.69 | 5.11 | <0.0001 | 4.96 | 1.94 | 12.7 | 0.001 | 3.14 | 1.953 | 5.03 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prete, M.; Luzzetti, A.; Augustin, L.S.A.; Porciello, G.; Montagnese, C.; Calabrese, I.; Ballarin, G.; Coluccia, S.; Patel, L.; Vitale, S.; et al. Changes in Lifestyle and Dietary Habits during COVID-19 Lockdown in Italy: Results of an Online Survey. Nutrients 2021, 13, 1923. https://doi.org/10.3390/nu13061923
Prete M, Luzzetti A, Augustin LSA, Porciello G, Montagnese C, Calabrese I, Ballarin G, Coluccia S, Patel L, Vitale S, et al. Changes in Lifestyle and Dietary Habits during COVID-19 Lockdown in Italy: Results of an Online Survey. Nutrients. 2021; 13(6):1923. https://doi.org/10.3390/nu13061923
Chicago/Turabian StylePrete, Melania, Anna Luzzetti, Livia S. A. Augustin, Giuseppe Porciello, Concetta Montagnese, Ilaria Calabrese, Giada Ballarin, Sergio Coluccia, Linia Patel, Sara Vitale, and et al. 2021. "Changes in Lifestyle and Dietary Habits during COVID-19 Lockdown in Italy: Results of an Online Survey" Nutrients 13, no. 6: 1923. https://doi.org/10.3390/nu13061923
APA StylePrete, M., Luzzetti, A., Augustin, L. S. A., Porciello, G., Montagnese, C., Calabrese, I., Ballarin, G., Coluccia, S., Patel, L., Vitale, S., Palumbo, E., Celentano, E., La Vecchia, C., & Crispo, A. (2021). Changes in Lifestyle and Dietary Habits during COVID-19 Lockdown in Italy: Results of an Online Survey. Nutrients, 13(6), 1923. https://doi.org/10.3390/nu13061923