Nutraceuticals in the Prevention and Treatment of the Muscle Atrophy
Abstract
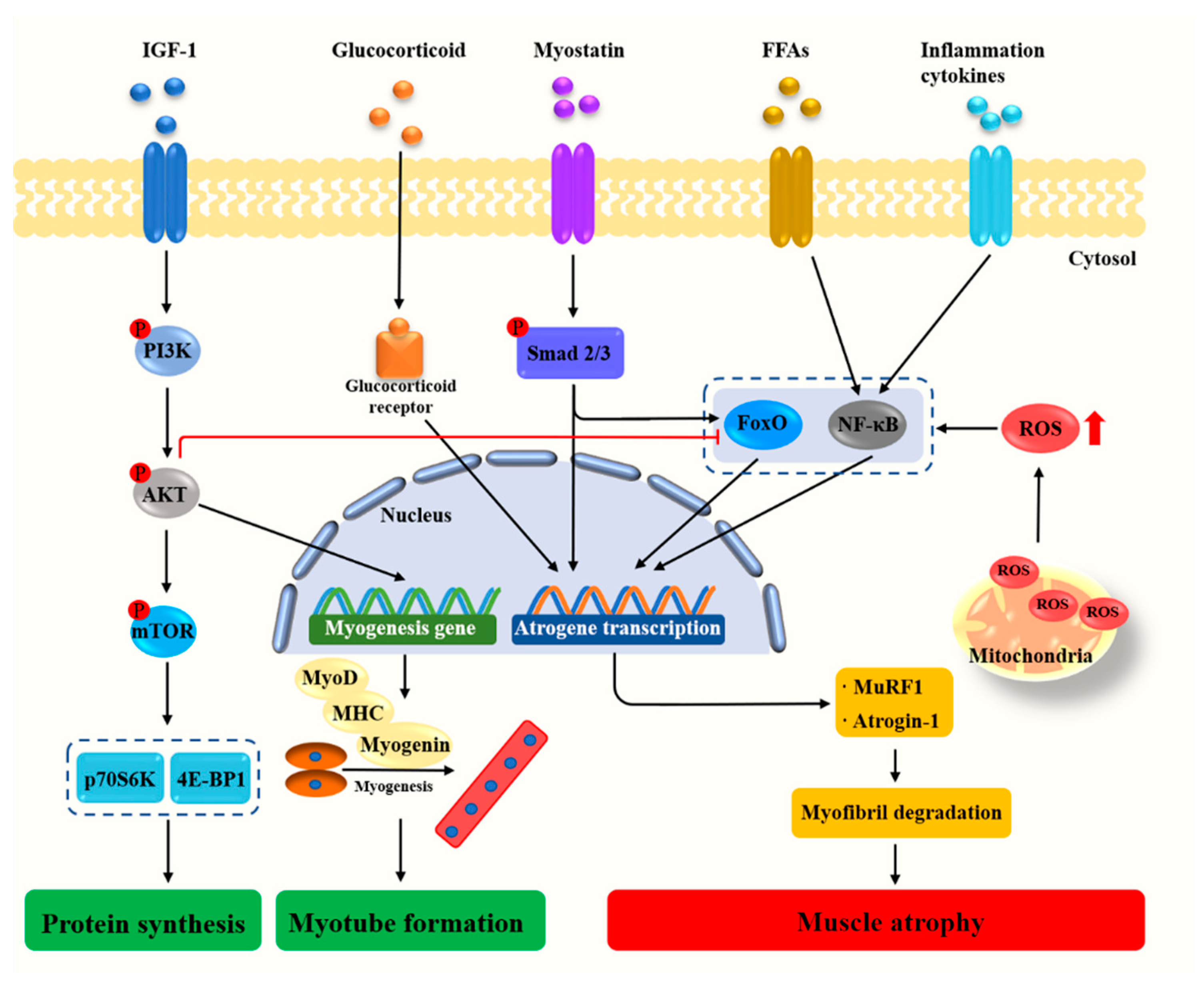
1. Introduction
2. Materials and Methods
3. Dietary Nutrients
3.1. Protein, Amino Acid, and Peptides
| Protein/Amino Acids/Peptides | Structure | Example Source | Inducer | Model | Effect | Mechanism | Ref |
|---|---|---|---|---|---|---|---|
| Whey protein | / | Egg, meat, milk | Immobilization | C57BL/6 mice | ↑ Grip strength ↑ Muscle mass ↑ Cross-sectional area of muscle fiber | ↑ mTOR signaling | [21] |
| Leucine | 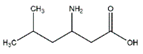 | Meat, milk | / | Human | ↑ Muscle protein | ↑ Protein synthesis ↑ mTOR signaling | [23] |
| C2C12 cells | ↑ Muscle protein | ↑ Protein synthesis ↑ mTOR signaling | [22] | ||||
| Valine |  | Meat, milk | Cachexia | NMRI mice | ↑ Muscle weight | ↑ Protein synthesis ↓ Protein degradation | [26] |
| Isoleucine |  | Meat, milk | / | SD rats | ↑ Muscle weight | ↑ Protein synthesis ↓ Protein degradation | [30] |
| Branched-chain amino acids | / | Meat, milk | Hindlimb suspension | SD rats | ↑ Muscle weight | ↑ mTOR signaling ↓ MuRF1, MAFbx | [28,30] |
| D-methionine | 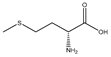 | Soybean | Cisplatin | Wistar rats | ↑ Muscle weight | ↑ MyoD ↓ MuRF1, MAFbx | [31] |
| Methionine |  | Soybean | / | Broilers | ↑ Breast muscle growth | ↑ Myf5, MEF2A | [33] |
| Glutamine | 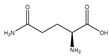 | Meat | TNF-α | C2C12 | ↑ Cell differentiation | ↓ p38 MAPK singnaling | [35] |
| Fasting | C57BL/6 mice | ↑ Muscle weight | ↑ mTOR signaling | [36] | |||
| Taurine |  | Fish, shellfish | Reduced mechanical loading | Albino mice | ↓ Muscle injury | ↓ MuRF1, caspase 3, MAFbx | [39] |
| Diquat | Piglets | ↑ Muscle protein | ↓ MuRF1, MAFbx | [40] | |||
| Cisplatin | C2C12 cells | ↑ Myotubes size | ↑ Microtubular, mitochondrial function | [38] | |||
| S-allyl cysteine | 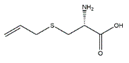 | Allium sativum | Denervation | Swiss albino mice | ↑ Muscle mass | ↓ MuRF1, MAFbx | [43] |
| H2O2 | C2C12 cells | ↑ Myotubes size | ↓ Oxidative stress, inflammation ↓ MuRF1, MAFbx | [43] | |||
| Soybean protein-derived peptides | / | Soybean | Burn injury | Wistar rats | ↑ Muscle protein | ↑ Autophagy signaling ↓ MuRF1, MAFbx | [44] |
| PYP1-5 | / | Pyropia yezoensis | Dexamethasone | C2C12 cells | ↑ Myotube size | ↓ MuRF1, MAFbx | [45] |
| N-myristoylated Cblin | / | / | Dexamethasone | C2C12 cells | ↑ Cell diameter | ↓ MuRF1, MAFbx | [46] |
| C57BL/6 mice | ↑ Muscle mass ↑ Muscle fiber cross-sectional areas | ↓ MuRF1, MAFbx |
3.2. Minerals
3.3. Vitamins
| Vitamins | Structure | Example Source | Inducer | Model | Effect | Mechanism | Ref |
|---|---|---|---|---|---|---|---|
| Vitamin C |  | Kiwi fruit, lemons | Senescence marker protein-30-konckout | Mice | ↑ Physical performance | ↓ MuRF1, MAFbx ↓ Oxidative stress | [56] |
| Vitamin D | 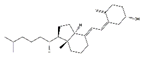 | Milk, meat | Immobilization | C57BL/6 mice | ↑ Muscle mass | ↓ Oxidative stress ↓ MuRF1, MAFbx | [60] |
| Vitamin E | 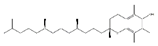 | Soybean oil | Immobilization | Wistar rats | / | ↓ Oxidative stress | [62] |
| Aging | Human | ↑ Muscle mass/strength | / | [63] | |||
| β-Carotene | 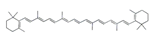 | Carrot | Denervation | ddY mice | ↑ Muscle mass | ↓ Oxidative stress ↓ MuRF1, MAFbx, USP14, USP19 | [65] |
| Coenzyme Q10 | 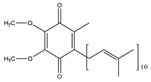 | Sardine | Disuse | SD rats | ↑ Muscle cross section | ↑ Mitochondrial biogenesis ↓ MuRF1, MAFbx, FoxO3 | [68] |
| Nicotinamide mononucleotide | 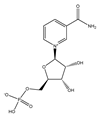 | Broccoli, avocado | Aging | C57BL/6N | ↑ Physical performance | ↑ Mtochondrial oxidative metabolism | [70] |
3.4. Fatty Acids
| Fatty Acids | Structure | Example Source | Inducer | Model | Effect | Mechanism | Ref |
|---|---|---|---|---|---|---|---|
| Docosahexaenoic acid | 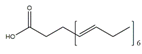 | Fish, milk | Palmitate | C2C12 cells | ↑ Cell growth | ↑ PGC-1α, Akt ↓ Endoplasmic reticulum stress | [71,72] |
| Oleic acid | 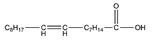 | Sesame | Palmitate | C2C12 cells | ↑ Myotube size | ↓ TNF-α, IL6 ↓ Drp1, Fis1 ↓ Myostatin, MAFbx | [74] |
| Eicosapentaenoic acid |  | Fish, nut | Arthritis | Wistar rats | ↑ Muscle mass | ↑ PCNA, MyoD, myogenin ↓ MuRF1, MAFbx | [75] |
| Arachidonic acid | 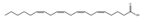 | Pine nut | / | C2C12 cells | ↑ Cell growth | ↑ Cyclooxygenase 2 | [80] |
| Azelaic acid |  | Oatmeal, barley | HFD | C57BL/6J mice | ↑ Muscle function | ↑ Mitochondrial biogenesis | [79] |
| / | C2C12 cells | / | ↑ Mitochondrial biogenesis, autophagy | [79] |
4. Phytochemicals
4.1. Polyphenols
4.2. Flavonoids
4.3. Polysaccharides
4.4. Alkaloids
4.5. Triterpenoids
| Triterpenoids | Structure | Example Source | Inducer | Model | Effect | Mechanism | Ref |
|---|---|---|---|---|---|---|---|
| Ursolic acid |  | Apples | Hind limb immobilization | SD rats | ↑ Muscle mass | ↓ MuRF1, MAFbx | [146] |
| Denervation | C57BL/6 mice | ↑ Muscle mass, muscle hypertrophy | ↑ Muscle hypertrophy ↓ MuRF1, MAFbx | [145] | |||
| / | C57BL/6N mice | ↑ Muscle weight, muscle strength, exercise capacity | ↑ IGF-1 ↓ MuRF1, MAFbx | [147] | |||
| / | C2C12 cells | ↑ Myotubes differentiation | ↑ IGF-1, Akt, mTOR, S6K1 ↓ MuRF1, MAFbx | [147] | |||
| Ginsenoside Rg1 | 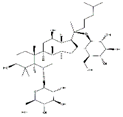 | Panax ginseng | Starvation | C2C12 cells | ↑ Myotubes differentiation | ↑ Akt/mTOR/FoxO signaling | [148] |
| Panax ginseng total protein | / | Panax ginseng | Dexamethasone | C2C12 cells | ↑ Glucose consumption | ↑ AMPK and PI3K/Akt signaling | [152] |
| Ginsenoside Rg3 | 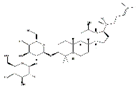 | Panax ginseng | TNF-α | C2C12 cells | ↑ Myotubes differentiation | ↑ Akt/mTOR signaling ↑ PGC1α, NRF1, Tfam | [149] |
| Ginsenoside Rb1 | 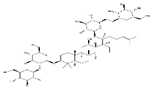 | Panax ginseng | / | C2C12 cells | ↑ Myotubes differentiation | ↑ Akt/mTOR signaling | [150] |
| Ginsenoside Rb2 | 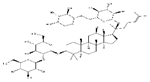 |
4.6. Others
5. Probiotics
6. Conclusions and Perspective
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cohen, S.; Nathan, J.A.; Goldberg, A.L. Muscle Wasting in Disease: Molecular Mechanisms and Promising Therapies. Nat. Rev. Drug Discov. 2015, 14, 58–74. [Google Scholar] [CrossRef]
- Mirzoev, T.M. Skeletal Muscle Recovery from Disuse Atrophy: Protein Turnover Signaling Andstrategies for Accelerating Muscle Regrowth. Int. J. Mol. Sci. 2020, 21, 7940. [Google Scholar] [CrossRef] [PubMed]
- Jackman, R.W.; Kandarian, S.C. The Molecular Basis of Skeletal Muscle Atrophy. Am. J. Physiol. Cell Physiol. 2004, 287, C834–C843. [Google Scholar] [CrossRef]
- Sartori, R.; Romanello, V.; Sandri, M. Mechanisms of Muscle Atrophy and Hypertrophy: Implications in Health and Disease. Nat. Commun. 2021, 12, 330. [Google Scholar] [CrossRef]
- Ebert, S.M.; Al-Zougbi, A.; Bodine, S.C.; Adams, C.M. Skeletal Muscle Atrophy: Discovery of Mechanisms and Potential Therapies. Physiology 2019, 34, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Clarke, B.A.; Drujan, D.; Willis, M.S.; Murphy, L.O.; Corpina, R.A.; Burova, E.; Rakhilin, S.V.; Stitt, T.N.; Patterson, C.; Latres, E.; et al. The E3 Ligase MuRF1 Degrades Myosin Heavy Chain Protein in Dexamethasone-Treated Skeletal Muscle. Cell Metab. 2007, 6, 376–385. [Google Scholar] [CrossRef]
- Bodine, S.C.; Latres, E.; Baumhueter, S.; Lai, V.K.; Nunez, L.; Clarke, B.A.; Poueymirou, W.T.; Panaro, F.J.; Na, E.; Dharmarajan, K.; et al. Identification of Ubiquitin Ligases Required for Skeletal Muscle Atrophy. Science 2001, 294, 1704–1708. [Google Scholar] [CrossRef]
- Okamoto, T.; Machida, S. Changes in FOXO and Proinflammatory Cytokines in the Late Stage of Immobilized Fast and Slow Muscle Atrophy. Biomed. Res. 2017, 38, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Nisr, R.B.; Shah, D.S.; Ganley, I.G.; Hundal, H.S. Proinflammatory NF-κB Signalling Promotes Mitochondrial Dysfunction in Skeletal Muscle in Response to Cellular Fuel Overloading. Cell. Mol. Life Sci. 2019, 76, 4887–4904. [Google Scholar] [CrossRef] [PubMed]
- Moylan, J.S.; Reid, M.B. Oxidative Stress, Chronic Disease, and Muscle Wasting. Muscle Nerve 2007, 35, 411–429. [Google Scholar] [CrossRef]
- Zuo, L.; Pannell, B.K. Redox Characterization of Functioning Skeletal Muscle. Front. Physiol. 2015, 6, 338. [Google Scholar] [CrossRef]
- Bindels, L.B.; Delzenne, N.M. Muscle Wasting: The Gut Microbiota as a New Therapeutic Target? Int. J. Biochem. Cell Biol. 2013, 45, 2186–2190. [Google Scholar] [CrossRef]
- Ticinesi, A.; Lauretani, F.; Milani, C.; Nouvenne, A.; Tana, C.; Del Rio, D.; Maggio, M.; Ventura, M.; Meschi, T. Aging Gut Microbiota at the Cross-Road between Nutrition, Physical Frailty, and Sarcopenia: Is There a Gut-Muscle Axis? Nutrients 2017, 9, 1303. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.N.; Huang, J.Q.; Chen, Z.Z.; Du, M.; Ren, F.Z.; Luo, J.; Fang, B. Amyotrophy Induced by a High-Fat Diet Is Closely Related to Inflammation and Protein Degradation Determined by Quantitative Phosphoproteomic Analysis in Skeletal Muscle of C57BL/6 J Mice. J. Nutr. 2020, 150, 294–302. [Google Scholar] [CrossRef]
- Muller, F.L.; Song, W.; Jang, Y.C.; Liu, Y.; Sabia, M.; Richardson, A.; Van Remmen, H. Denervation-Induced Skeletal Muscle Atrophy Is Associated with Increased Mitochondrial Ros Production. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2007, 293, R1159–R1168. [Google Scholar] [CrossRef] [PubMed]
- Schakman, O.; Kalista, S.; Barbé, C.; Loumaye, A.; Thissen, J.P. Glucocorticoid-Induced Skeletal Muscle Atrophy. Int. J. Biochem. Cell Biol. 2013, 45, 2163–2172. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Hwang, J.K. Flavonoids: Nutraceutical Potential for Counteracting Muscle Atrophy. Food Sci. Biotechnol. 2020, 29, 1619–1640. [Google Scholar] [CrossRef] [PubMed]
- Salucci, S.; Falcieri, E. Polyphenols and Their Potential Role in Preventing Skeletal Muscle Atrophy. Nutr. Res. 2020, 74, 10–22. [Google Scholar] [CrossRef] [PubMed]
- Dardevet, D.; Rémond, D.; Peyron, M.A.; Papet, I.; Savary-Auzeloux, I.; Mosoni, L. Muscle Wasting and Resistance of Muscle Anabolism: The “Anabolic Threshold Concept” for Adapted Nutritional Strategies During Sarcopenia. Sci. World J. 2012, 2012, 269531. [Google Scholar] [CrossRef]
- Miyatake, S.; Hino, K.; Natsui, Y.; Ebisu, G.; Fujita, S. Protein supplementation enhances the Protein Supplementation Enhances the Effects of Intermittent Loading on Skeletal Muscles by Activating the mTOR Signaling Pathway in a Rat Model of Disuse Atrophy. Nutrients 2020, 12, 2729. [Google Scholar] [CrossRef]
- Shin, J.E.; Park, S.J.; Ahn, S.I.; Choung, S.Y. Soluble Whey Protein Hydrolysate Ameliorates Muscle Atrophy Induced by Immobilization via Regulating the PI3K/Akt Pathway in C57BL/6 Mice. Nutrients 2020, 12, 3362. [Google Scholar] [CrossRef]
- Atherton, P.J.; Smith, K.; Etheridge, T.; Rankin, D.; Rennie, M.J. Distinct Anabolic Signalling Responses to Amino Acids in C2C12 Skeletal Muscle Cellsmuscle cells. Amino Acids 2010, 38, 1533–1539. [Google Scholar] [CrossRef] [PubMed]
- Dreyer, H.C.; Drummond, M.J.; Pennings, B.; Fujita, S.; Glynn, E.L.; Chinkes, D.L.; Dhanani, S.; Volpi, E.; Rasmussen, B.B. Leucine-Enriched Essential Amino Acid and Carbohydrate Ingestion Following Resistance Exercise Enhances mTOR Signaling and Protein Synthesis in Human Muscle. Am. J. Physiol. Endocrinol. Metab. 2008, 294, E392–E400. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, D.J.; Bukhari, S.S.I.; Phillips, B.E.; Limb, M.C.; Cegielski, J.; Brook, M.S.; Rankin, D.; Mitchell, W.K.; Kobayashi, H.; Williams, J.P.; et al. Effects of Leucine-Enriched Essential Amino Acid and Whey Protein Bolus Dosing Upon Skeletal Muscle Protein Synthesis at Rest and after Exercise in Older Women. Clin. Nutr. 2018, 37, 2011–2021. [Google Scholar] [CrossRef]
- Brooks, N.; Cloutier, G.J.; Cadena, S.M.; Layne, J.E.; Nelsen, C.A.; Freed, A.M.; Roubenoff, R.; Castaneda-Sceppa, C. Resistance Training and Timed Essential Amino Acids Protect against the Loss of Muscle Mass and Strength During 28 Days of Bed Rest and Energy Deficit. J. Appl. Physiol. 2008, 105, 241–248. [Google Scholar] [CrossRef]
- Eley, H.L.; Russell, S.T.; Tisdale, M.J. Effect of Branched-Chain Amino Acids on Muscle Atrophy in Cancer Cachexia. Biochem. J. 2007, 407, 113–120. [Google Scholar] [CrossRef]
- Appuhamy, J.A.; Knoebel, N.A.; Nayananjalie, W.A.; Escobar, J.; Hanigan, M.D. Isoleucine and Leucine Independently Regulate mTOR Signaling and Protein Synthesis in MAC-T Cells and Bovine Mammary Tissue Slices. J. Nutr. 2012, 142, 484–491. [Google Scholar] [CrossRef]
- Maki, T.; Yamamoto, D.; Nakanishi, S.; Iida, K.; Iguchi, G.; Takahashi, Y.; Kaji, H.; Chihara, K.; Okimura, Y. Branched-Chain Amino Acids Reduce Hindlimb Suspension-Induced Muscle Atrophy and Protein Levels of Atrogin-1 and MuRF1 in Rats. Nutr. Res. 2012, 32, 676–683. [Google Scholar] [CrossRef] [PubMed]
- Yamanashi, K.; Kinugawa, S.; Fukushima, A.; Kakutani, N.; Takada, S.; Obata, Y.; Nakano, I.; Yokota, T.; Kitaura, Y.; Shimomura, Y.; et al. Branched-Chain Amino Acid Supplementation Ameliorates Angiotensin II-Induced Skeletal Muscle Atrophy. Life Sci. 2020, 250, 117593. [Google Scholar] [CrossRef]
- Vieira, T.S.; Pinto, A.P.; Batitucci, G.; da Rocha, A.L.; Filho, H.T.; Gonçalves, D.A.; da Silva, A.S.R.; de Freitas, E.C. Protein Blend and Casein Supplementations before Inactive Phase Similarly Activate Mechanistic Target of Rapamycin Signaling in Rat Skeletal Muscle. Chin. J. Physiol. 2020, 63, 171–178. [Google Scholar]
- Wu, C.T.; Liao, J.M.; Ko, J.L.; Lee, Y.L.; Chang, H.Y.; Wu, C.H.; Ou, C.C. D-Methionine Ameliorates Cisplatin-Induced Muscle Atrophy via Inhibition of Muscle Degradation Pathway. Integr. Cancer Ther. 2019, 18, 1–15. [Google Scholar] [CrossRef]
- Alami-Durante, H.; Bazin, D.; Cluzeaud, M.; Fontagne-Dicharry, S.; Kaushik, S.; Geurden, I. Effect of Dietary Methionine Level on Muscle Growth Mechanisms in Juvenile Rainbow Trout (Oncorhynchus Mykiss). Aquaculture 2018, 483, 273–285. [Google Scholar] [CrossRef]
- Wen, C.; Jiang, X.; Ding, L.; Wang, T.; Zhou, Y. Effects of Dietary Methionine on Breast Muscle Growth, Myogenic Gene Expression and IGF-I Signaling in Fast- and Slow-Growing Broilers. Sci. Rep. 2017, 7, 1924. [Google Scholar] [CrossRef]
- Lambertucci, A.C.; Lambertucci, R.H.; Hirabara, S.M.; Curi, R.; Moriscot, A.S.; Alba-Loureiro, T.C.; Guimarцëes-Ferreira, L.; Levada-Pires, A.C.; Vasconcelos, D.A.; Sellitti, D.F.; et al. Glutamine Supplementation Stimulates Protein-Synthetic and Inhibits Protein-Degradative Signaling Pathways in Skeletal Muscle of Diabetic Rats. PLoS ONE 2012, 7, e50390. [Google Scholar] [CrossRef] [PubMed]
- Girven, M.; Dugdale, H.F.; Owens, D.J.; Hughes, D.C.; Stewart, C.E.; Sharples, A.P. L-Glutamine Improves Skeletal Muscle Cell Differentiation and Prevents Myotube Atrophy after Cytokine (TNF-α) Stress Via Reduced p38 MAPK Signal Transduction. J. Cell. Physiol. 2016, 231, 2720–2732. [Google Scholar] [CrossRef]
- De Vasconcelos, D.A.A.; Giesbertz, P.; de Souza, D.R.; Vitzel, K.F.; Abreu, P.; Marzuca-Nassr, G.N.; Fortes, M.A.S.; Murata, G.M.; Hirabara, S.M.; Curi, R.; et al. Oral L-Glutamine Pretreatment Attenuates Skeletal Muscle Atrophy Induced by 24-h Fasting in Mice. J. Nutr. Biochem. 2019, 70, 202–214. [Google Scholar] [CrossRef] [PubMed]
- Salehian, B.; Mahabadi, V.; Bilas, J.; Taylor, W.E.; Ma, K. The Effect of Glutamine on Prevention of Glucocorticoid-Induced Skeletal Muscle Atrophy Is Associated with Myostatin Suppression. Metabolism 2006, 55, 1239–1247. [Google Scholar] [CrossRef]
- Stacchiotti, A.; Rovetta, F.; Ferroni, M.; Corsetti, G.; Lavazza, A.; Sberveglieri, G.; Aleo, M.F. Taurine Rescues Cisplatin-Induced Muscle Atrophy in Vitro: A Morphological Study. Oxid. Med. Cell. Longev. 2014, 2014, 840951. [Google Scholar] [CrossRef] [PubMed]
- Khalil, R.M.; Abdo, W.S.; Saad, A.; Khedr, E.G. Muscle Proteolytic System Modulation through the Effect of Taurine on Mice Bearing Muscular Atrophy. Mol. Cell. Biochem. 2018, 444, 161–168. [Google Scholar] [CrossRef]
- Wen, C.; Li, F.; Guo, Q.; Zhang, L.; Duan, Y.; Wang, W.; Li, J.; He, S.; Chen, W.; Yin, Y. L-Glutamine Improves Skeletal Muscle Cell Differentiation and Prevents Myotube Atrophy after Cytokine. J. Anim. Sci. Biotechnol. 2020, 11, 56. [Google Scholar] [CrossRef]
- Cella, P.S.; Marinello, P.C.; Borges, F.H.; Ribeiro, D.F.; Chimin, P.; Testa, M.T.J.; Guirro, P.B.; Duarte, J.A.; Cecchini, R.; Guarnier, F.A.; et al. Creatine Supplementation in Walker-256 Tumor-Bearing Rats Prevents Skeletal Muscle Atrophy by Attenuating Systemic Inflammation and Protein Degradation Signaling. Eur. J. Nutr. 2020, 59, 661–669. [Google Scholar] [CrossRef] [PubMed]
- Marzuca-Nassr, G.N.; Fortes, M.A.S.; Guimarцëes-Ferreira, L.; Murata, G.M.; Vitzel, K.F.; Vasconcelos, D.A.A.; Bassit, R.A.; Curi, R. Short-Term Creatine Supplementation Changes Protein Metabolism Signaling in Hindlimb Suspension. Braz. J. Med. Biol. Res. 2019, 52, e8391. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.; Dutt, V.; Kaur, N.; Kalra, P.; Gupta, S.; Dua, A.; Dabur, R.; Saini, V.; Mittal, A. S-Allyl Cysteine: A Potential Compound against Skeletal Muscle Atrophy. Biochim. Biophys. Acta Gen. Subj. 2020, 1864, 129676. [Google Scholar] [CrossRef] [PubMed]
- Zhao, F.; Yu, Y.; Liu, W.; Zhang, J.; Liu, X.; Liu, L.; Yin, H. Small Molecular Weight Soybean Protein-Derived Peptides Nutriment Attenuates Rat Burn Injury-Induced Muscle Atrophy by Modulation of Ubiquitin-Proteasome System and Autophagy Signaling Pathway. J. Agric. Food Chem. 2018, 66, 2724–2734. [Google Scholar] [CrossRef]
- Lee, M.K.; Kim, Y.M.; Kim, I.H.; Choi, Y.H.; Nam, T.J. Pyropia Yezoensis Peptide PYP1-5 Protects against Dexamethasone-Induced Muscle Atrophy through the Downregulation of Atrogin1/MAFbx and MuRF1 in Mouse C2C12 Myotubes. Mol. Med. Rep. 2017, 15, 3507–3514. [Google Scholar] [CrossRef] [PubMed]
- Ochi, A.; Abe, T.; Nakao, R.; Yamamoto, Y.; Kitahata, K.; Takagi, M.; Hirasaka, K.; Ohno, A.; Teshima-Kondo, S.; Taesik, G.; et al. N-Myristoylated Ubiquitin Ligase Cbl-b Inhibitor Prevents on Glucocorticoid-Induced Atrophy in Mouse Skeletal Muscle. Arch. Biochem. Biophys. 2015, 570, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Eren Cimenci, C.; Uzunalli, G.; Uysal, O.; Yergoz, F.; Karaca Umay, E.; Guler, M.O.; Tekinay, A.B. Laminin Mimetic Peptide Nanofibers Regenerate Acute Muscle Defect. Acta Biomater. 2017, 60, 190–200. [Google Scholar] [CrossRef]
- Arneson-Wissink, P.C.; Hogan, K.A.; Ducharme, A.M.; Samani, A.; Jatoi, A.; Doles, J.D. The Wasting-Associated Metabolite Succinate Disrupts Myogenesis and Impairs Skeletal Muscle Regeneration. JCSM Rapid Commun. 2020, 3, 56–69. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, S.; Suematsu, C.; Kumamoto, T.; Ito, N. Calcium and Magnesium Deficiency-Induced Atrophy of Muscle and Calcium Accumulation in the Spinal Cord. Experientia 1976, 32, 915–917. [Google Scholar] [CrossRef] [PubMed]
- Seo, M.H.; Kim, M.K.; Park, S.E.; Rhee, E.J.; Park, C.Y.; Lee, W.Y.; Baek, K.H.; Song, K.H.; Kang, M.I.; Oh, K.W. The Association between Daily Calcium Intake and Sarcopenia in Older, Non-Obese Korean Adults: The Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV) 2009. Endocr. J. 2013, 60, 679–686. [Google Scholar] [CrossRef]
- Ter Borg, S.; de Groot, L.C.; Mijnarends, D.M.; de Vries, J.H.; Verlaan, S.; Meijboom, S.; Luiking, Y.C.; Schols, J.M. Differences in Nutrient Intake and Biochemical Nutrient Status between Sarcopenic and Nonsarcopenic Older Adults-Results from Maastricht Sarcopenia Study. J. Am. Med. Dir. Assoc. 2016, 17, 393–401. [Google Scholar] [CrossRef]
- Veronese, N.; Berton, L.; Carraro, S.; Bolzetta, F.; De Rui, M.; Perissinotto, E.; Toffanello, E.D.; Bano, G.; Pizzato, S.; Miotto, F.; et al. Effect of Oral Magnesium Supplementation on Physical Performance in Healthy Elderly Women Involved in a Weekly Exercise Program: A Randomized Controlled Trial. Am. J. Clin. Nutr. 2014, 100, 974–981. [Google Scholar] [CrossRef] [PubMed]
- Chariot, P.; Bignani, O. Skeletal Muscle Disorders Associated with Selenium Deficiency in Humans. Muscle Nerve 2003, 27, 662–668. [Google Scholar] [CrossRef] [PubMed]
- Fodor, J.; Al Gaadi, D.; Czirják, T.; Oláh, T.A.O.; Dienes, B.; Csernoch, L.; Szentesi, P.A.O. Improved Calcium Homeostasis and Force by Selenium Treatment and Training in Aged Mouse Skeletal Muscle. Sci. Rep. 2020, 10, 1707. [Google Scholar] [CrossRef]
- Wang, H.; Li, T.L.; Hsia, S.; Su, I.L.; Chan, Y.L.; Wu, C.J. Skeletal Muscle Atrophy Is Attenuated in Tumor-Bearing Mice under Chemotherapy by Treatment with Fish Oil and Selenium. Oncotarget 2015, 6, 7758–7773. [Google Scholar] [CrossRef]
- Takisawa, S.; Funakoshi, T.; Yatsu, T.; Nagata, K.; Aigaki, T.; Machida, S.; Ishigami, A. Vitamin C Deficiency Causes Muscle Atrophy and a Deterioration in Physical Performance. Sci. Rep. 2019, 9, 4702. [Google Scholar] [CrossRef] [PubMed]
- Makanae, Y.; Kawada, S.; Sasaki, K.; Nakazato, K.; Ishii, N. Vitamin C Administration Attenuates Overload-Induced Skeletal Muscle Hypertrophy in Rats. Acta Physiol. 2013, 208, 57–65. [Google Scholar] [CrossRef]
- Lewis, L.N.; Hayhoe, R.P.G.; Mulligan, A.A.; Luben, R.N.; Khaw, K.T.; Welch, A.A. Lower Dietary and Circulating Vitamin C in Middle- and Older-Aged Men and Women Are Associated with Lower Estimated Skeletal Muscle Mass. J. Nutr. 2020, 150, 2789–2798. [Google Scholar] [CrossRef]
- Garcia, M.; Seelaender, M.; Sotiropoulos, A.; Coletti, D.; Lancha, A.H., Jr. Vitamin D, Muscle Recovery, Sarcopenia, Cachexia, and Muscle Atrophy. Nutrition 2019, 60, 66–69. [Google Scholar] [CrossRef]
- Nakamura, S.; Sato, Y.; Kobayashi, T.; Kaneko, Y.; Ito, E.; Soma, T.; Okada, H.; Miyamoto, K.; Oya, A.; Matsumoto, M.; et al. Vitamin D Protects against Immobilization-Induced Muscle Atrophy Via Neural Crest-Derived Cells in Mice. Sci. Rep. 2020, 10, 12242. [Google Scholar] [CrossRef]
- Karnia, M.J.; Korewo, D.; Myślińska, D.; Ciepielewski, Z.M.; Puchalska, M.; Konieczna-Wolska, K.; Kowalski, K.; Kaczor, J.J. The Positive Impact of Vitamin D on Glucocorticoid-Dependent Skeletal Muscle Atrophy. Nutrients 2021, 13, 936. [Google Scholar] [CrossRef] [PubMed]
- Kondo, H.; Miura, M.; Itokawa, Y. Oxidative Stress in Skeletal Muscle Atrophied by Immobilization. Acta Physiol. Scand. 1991, 142, 527–528. [Google Scholar] [CrossRef]
- Bo, Y.; Liu, C.; Ji, Z.; Yang, R.; An, Q.; Zhang, X.; You, J.; Duan, D.; Sun, Y.; Zhu, Y.; et al. A High Whey Protein, Vitamin D and E Supplement Preserves Muscle Mass, Strength, and Quality of Life in Sarcopenic Older Adults: A Double-Blind Randomized Controlled Trial. Clin. Nutr. 2019, 38, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Geng, R.; Kang, S.-G.; Huang, K.; Tong, T. Boosting the Photoaged Skin: The Potential Role of Dietary Components. Nutrients 2021, 13, 1691. [Google Scholar] [CrossRef]
- Ogawa, M.; Kariya, Y.; Kitakaze, T.; Yamaji, R.; Harada, N.; Sakamoto, T.; Hosotani, K.; Nakano, Y.; Inui, H. The Preventive Effect of β-Carotene on Denervation-Induced Soleus Muscle Atrophy in Mice. Br. J. Nutr. 2013, 109, 1349–1358. [Google Scholar] [CrossRef]
- Shen, W.; Hao, J.; Tian, C.; Ren, J.; Yang, L.; Li, X.; Luo, C.; Cotma, C.W.; Liu, J. Combination of Nutriments Improves Mitochondrial Biogenesis and Function in Skeletal Muscle of Type 2 Diabetic Goto-Kakizaki Rats. PLoS ONE 2008, 3, e2328. [Google Scholar] [CrossRef][Green Version]
- Rosa-Caldwell, M.E.; Benson, C.A.; Lee, D.E.; Brown, J.L.; Washington, T.A.; Greene, N.P.; Wiggs, M.P. Mitochondrial Function and Protein Turnover in the Diaphragm Are Altered in LLC Tumor Mmodel of Cancer Cachexia. Int. J. Mol. Sci. 2020, 21, 7841. [Google Scholar] [CrossRef]
- Liu, J.; Peng, Y.; Feng, Z.; Shi, W.; Qu, L.; Li, Y.; Liu, J.; Long, J. Reloading Functionally Ameliorates Disuse-Induced Muscle Atrophy by Reversing Mitochondrial Dysfunction, and Similar Benefits Are Gained by Administering a Combination of Mitochondrial Nutrients. Free Radic. Biol. Med. 2014, 69, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Gomes, A.P.; Price, N.L.; Ling, A.J.; Moslehi, J.J.; Montgomery, M.K.; Rajman, L.; White, J.P.; Teodoro, J.S.; Wrann, C.D.; Hubbard, B.P.; et al. Declining NAD (+) Induces a Pseudohypoxic State Disrupting Nuclear-Mitochondrial Communication During Aging. Cell 2013, 155, 1624–1638. [Google Scholar] [CrossRef]
- Mills, K.F.; Yoshida, S.; Stein, L.R.; Grozio, A.; Kubota, S.; Sasaki, Y.; Redpath, P.; Migaud, M.E.; Apte, R.S.; Uchida, K.; et al. Long-Term Administration of Nicotinamide Mononucleotide Mitigates Age-Associated Physiological Decline in Mice. Cell Metab. 2016, 24, 795–806. [Google Scholar] [CrossRef]
- Bryner, R.W.; Woodworth-Hobbs, M.E.; Williamson, D.L.; Alway, S.E. Docosahexaenoic Acid Protects Muscle Cells from Palmitate-Induced Atrophy. ISRN Obes. 2012, 2012, 647348. [Google Scholar] [CrossRef] [PubMed]
- Woodworth-Hobbs, M.E.; Perry, B.D.; Rahnert, J.A.; Hudson, M.B.; Zheng, B.; Russ Price, S. Docosahexaenoic Acid Counteracts Palmitate-Induced Endoplasmic Reticulum Stress in C2C12 Myotubes: Impact on Muscle Atrophy. Physiol. Rep. 2017, 5, e13530. [Google Scholar] [CrossRef] [PubMed]
- Woodworth-Hobbs, M.E.; Hudson, M.B.; Rahnert, J.A.; Zheng, B.; Franch, H.A.; Price, S.R. Docosahexaenoic Acid Prevents Palmitate-Induced Activation of Proteolytic Systems in C2C12 Myotubes. J. Nutr. Biochem. 2014, 25, 868–874. [Google Scholar] [CrossRef]
- Lee, H.; Lim, J.Y.; Choi, S.J. Oleate Prevents Palmitate-Induced Atrophy Via Modulation of Mitochondrial ROS Production in Skeletal Myotubes. Oxid. Med. Cell. Longev. 2017, 2017, 2739721. [Google Scholar] [CrossRef] [PubMed]
- Castillero, E.; Martín, A.I.; López-Menduiña, M.; Villanúa, M.A.; López-Calderón, A. Eicosapentaenoic Acid Attenuates Arthritis-Induced Muscle Wasting Acting on Atrogin-1 and on Myogenic Regulatory Factors. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2009, 297, R1322–R1331. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, F.; Odle, J.; Lin, X.; Zhu, H.; Shi, H.; Hou, Y.; Yin, J. Fish Oil Increases Muscle Protein Mass and Modulates Akt/FOXO, TLR4, and NOD Signaling in Weanling Piglets after Lipopolysaccharide Challenge. J. Nutr. 2013, 143, 1331–1339. [Google Scholar] [CrossRef] [PubMed]
- Komiya, Y.; Kobayashi, C.; Uchida, N.; Otsu, S.; Tanio, T.; Yokoyama, I.; Nagasao, J.; Arihara, K. Effect of Dietary Fish Oil Intake on Ubiquitin Ligase Expression During Muscle Atrophy Induced by Sciatic Nerve Denervation in Mice. Anim. Sci. J. 2019, 90, 1018–1025. [Google Scholar] [CrossRef]
- Smith, G.I.; Julliand, S.; Reeds, D.N.; Sinacore, D.R.; Klein, S.; Mittendorfer, B. Fish Oil-Derived N-3 PUFA Therapy Increases Muscle Mass and Function in Healthy Older Adults. Am. J. Clin. Nutr. 2015, 102, 115–122. [Google Scholar] [CrossRef]
- Thach, T.T.; Wu, C.; Hwang, K.Y.; Lee, S.J. Azelaic Acid Induces Mitochondrial Biogenesis in Skeletal Muscle by Activation of Olfactory Receptor 544. Front. Physiol. 2020, 11, 329. [Google Scholar] [CrossRef]
- Markworth, J.F.; Cameron-Smith, D. Arachidonic Acid Supplementation Enhances in Vitro Skeletal Muscle Cell Growth Via a COX-2-Dependent Pathway. Am. J. Physiol. Cell. Physiol. 2013, 304, C56–C67. [Google Scholar] [CrossRef]
- Shirakawa, T.; Miyawaki, A.; Matsubara, T.; Okumura, N.; Okamoto, H.; Nakai, N.; Rojasawasthien, T.; Morikawa, K.; Inoue, A.; Goto, A.; et al. Daily Oral Administration of Protease-Treated Royal Jelly Protects against Denervation-Induced Skeletal Muscle Atrophy. Nutrients 2020, 12, 3089. [Google Scholar] [CrossRef]
- Salucci, S.; Burattini, S.; Buontempo, F.; Martelli, A.M.; Falcieri, E.; Battistelli, M. Protective Effect of Different Antioxidant Agents in UVB-Irradiated Keratinocytes. Eur. J. Histochem. 2017, 61, 2784. [Google Scholar] [CrossRef]
- Salucci, S.; Burattini, S.; Giordano, F.M.; Lucarini, S.; Diamantini, G.; Falcieri, E. Further Highlighting on the Prevention of Oxidative Damage by Polyphenol-Rich Wine Extracts. J. Med. Food 2017, 20, 410–419. [Google Scholar] [CrossRef]
- Ono, T.; Takada, S.; Kinugawa, S.; Tsutsui, H. Curcumin Ameliorates Skeletal Muscle Atrophy in Type 1 Diabetic Mice by Inhibiting Protein Ubiquitination. Exp. Physiol. 2015, 100, 1052–1063. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, P.; Sharma, Y.K.; Sharma, S.; Singh, S.N.; Suryakumar, G. High Altitude Mediated Skeletal Muscle Atrophy: Protective Role of Curcumin. Biochimie 2019, 156, 138–147. [Google Scholar] [CrossRef]
- Wang, D.; Sun, H.; Song, G.; Yang, Y.; Zou, X.; Han, P.; Li, S. Resveratrol Improves Muscle Atrophy by Modulating Mitochondrial Quality Control in STZ-Induced Diabetic Mice. Mol. Nutr. Food Res. 2018, 62, e1700941. [Google Scholar] [CrossRef] [PubMed]
- Shadfar, S.; Couch, M.E.; McKinney, K.A.; Weinstein, L.J.; Yin, X.; Rodríguez, J.E.; Guttridge, D.C.; Willis, M. Resveratrol Therapy Inhibits Cancer-Induced Skeletal Muscle and Cardiac Atrophy in Vivo. Nutr. Cancer 2011, 63, 749–762. [Google Scholar] [CrossRef] [PubMed]
- Asami, Y.; Aizawa, M.; Kinoshita, M.; Ishikawa, J.; Sakuma, K. Resveratrol Attenuates Denervation-Induced Muscle Atrophy Due to the Blockade of Atrogin-1 and p62 Accumulation. Int. J. Med. Sci. 2018, 15, 628–637. [Google Scholar] [CrossRef]
- Sun, L.; Miyaji, N.; Yang, M.; Mills, E.M.; Taniyama, S.; Uchida, T.; Nikawa, T.; Li, J.; Shi, J.; Tachibana, K.; et al. Astaxanthin Prevents Atrophy in Slow Muscle Fibers by Inhibiting Mitochondrial Reactive Oxygen Species via a Mitochondria-Mediated Apoptosis Pathway. Nutrients 2021, 13, 379. [Google Scholar] [CrossRef]
- Kim, A.R.; Kim, K.M.; Byun, M.R.; Hwang, J.H.; Park, J.I.; Oh, H.T.; Kim, H.K.; Jeong, M.G.; Hwang, E.S.; Hong, J.H. Catechins Activate Muscle Stem Cells by Myf5 Induction and Stimulate Muscle Regeneration. Biochem. Biophys. Res. Commun. 2017, 489, 142–148. [Google Scholar] [CrossRef]
- Hong, K.B.; Lee, H.S.; Kim, D.H.; Moon, J.M.; Park, Y. Tannase-Converted Green Tea Extract with High (−)-Epicatechin Inhibits Skeletal Muscle Mass in Aged Mice. Evid. Based Complement. Altern. Med. 2020, 2020, 4319398. [Google Scholar] [CrossRef]
- Meador, B.M.; Mirza, K.A.; Tian, M.; Skelding, M.B.; Reaves, L.A.; Edens, N.K.; Tisdale, M.J.; Pereira, S.L. The Green Tea Polyphenol Epigallocatechin-3-Gallate (EGCG) Attenuates Skeletal Muscle Atrophy in a Rat Model of Sarcopenia. J. Frailty Aging 2015, 4, 209–215. [Google Scholar] [PubMed]
- Rodriguez, J.; Caille, O.; Ferreira, D.; Francaux, M. Pomegranate Extract Prevents Skeletal Muscle of Mice against Wasting Induced by Acute TNF-α Injection. Mol. Nutr. Food Res. 2017, 61, 1600169. [Google Scholar] [CrossRef] [PubMed]
- Andreux, P.A.; Blanco-Bose, W.; Ryu, D.; Burdet, F.; Ibberson, M.; Aebischer, P.; Auwerx, J.; Singh, A.; Rinsch, C. The Mitophagy Activator Urolithin a Is Safe and Induces a Molecular Signature of Improved Mitochondrial and Cellular Health in Humans. Nat. Metab. 2019, 1, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Ryu, D.A.-O.; Mouchiroud, L.; Andreux, P.A.; Katsyuba, E.; Moullan, N.; Nicolet-dit-Félix, A.A.; Williams, E.G.; Jha, P.; Lo Sasso, G.; Huzard, D.; et al. Urolithin a Induces Mitophagy and Prolongs Lifespan in C. elegans and Increases Muscle Function in Rodents. Nat. Med. 2016, 22, 879–888. [Google Scholar] [CrossRef]
- Rodriguez, J.; Pierre, N.; Naslain, D.; Bontemps, F.; Ferreira, D.; Priem, F.; Deldicque, L.; Francaux, M. Urolithin B, a Newly Identified Regulator of Skeletal Muscle Mass. J. Cachexia Sarcopenia Muscle 2017, 8, 583–597. [Google Scholar] [CrossRef] [PubMed]
- Yoshioka, Y.; Kubota, Y.; Samukawa, Y.; Yamashita, Y.; Ashida, H. Glabridin Inhibits Dexamethasone-Induced Muscle Atrophy. Arch. Biochem. Biophys. 2019, 664, 157–166. [Google Scholar] [CrossRef]
- Ito, M.; Kudo, N.; Miyake, Y.; Imai, T.; Unno, T.; Yamashita, Y.; Hirota, Y.; Ashida, H.; Osakabe, N. Flavan 3-ol Delays the Progression of Disuse Atrophy Induced by Hindlimb Suspension in Mice. Exp. Gerontol. 2017, 98, 120–123. [Google Scholar] [CrossRef]
- Liu, H.W.; Chen, Y.J.; Chang, Y.C.; Chang, S.J. Oligonol, a Low-Molecular Weight Polyphenol Derived from Lychee, Alleviates Muscle Loss in Diabetes by Suppressing Atrogin-1 and MuRF1. Nutrients 2017, 9, 1040. [Google Scholar] [CrossRef]
- Chen, M.C.; Chen, Y.L.; Lee, C.F.; Hung, C.H.; Chou, T.C. Supplementation of Magnolol Attenuates Skeletal Muscle Atrophy in Bladder Cancer-Bearing Mice Undergoing Chemotherapy Via Suppression of FoxO3 Activation and Induction of IGF-1. PLoS ONE 2015, 10, e0143594. [Google Scholar] [CrossRef]
- Han, Y.; Lee, H.; Li, H.; Ryu, J.H. Corylifol A from Psoralea corylifolia L. Enhances Myogenesis and Alleviates Muscle Atrophy. Int. J. Mol. Sci. 2020, 21, 1571. [Google Scholar] [CrossRef] [PubMed]
- Shibaguchi, T.; Yamaguchi, Y.; Miyaji, N.; Yoshihara, T.; Naito, H.; Goto, K.; Ohmori, D.; Yoshioka, T.; Sugiura, T. Astaxanthin intake attenuates muscle atrophy caused by immobilization in rats. Physiol. Rep. 2016, 4, e12885. [Google Scholar] [CrossRef]
- Khan, N.; Mukhtar, H. Tea Polyphenols in Promotion of Human Health. Nutrients 2018, 11, 39. [Google Scholar] [CrossRef]
- Yoshioka, Y.; Yamashita, Y.; Kishida, H.; Nakagawa, K.; Ashida, H. Licorice Flavonoid Oil Enhances Muscle Mass in KK-A(y) Mice. Life Sci. 2018, 205, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Frati, A.; Landi, D.; Marinelli, C.; Gianni, G.; Fontana, L.; Migliorini, M.; Pierucci, F.; Garcia-Gil, M.; Meacci, E. Nutraceutical Properties of Chestnut Flours: Beneficial Effects on Skeletal Muscle Atrophy. Food Funct. 2014, 5, 2870–2882. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Kim, M.B.; Hwang, J.K. Red Bean Extract Inhibits Immobilization-Induced Muscle Atrophy in C57BL/6N Mice. J. Med. Food 2020, 23, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Aust, O.; Stahl, W.; Sies, H.; Tronnier, H.; Heinrich, U. Supplementation with Tomato-Based Products Increases Lycopene, Phytofluene, and Phytoene Levels in Human Serum and Protects against UV-Light-Induced Erythema. Int. J. Vitam. Nutr. Res. 2005, 75, 54–60. [Google Scholar] [CrossRef]
- Kawser Hossain, M.; Abdal Dayem, A.; Han, J.; Yin, Y.; Kim, K.; Kumar Saha, S.; Yang, G.M.; Choi, H.Y.; Cho, S.G. Molecular Mechanisms of the Anti-Obesity and Anti-Diabetic Properties of Flavonoids. Int. J. Mol. Sci. 2016, 17, 569. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Chen, H.Q.; Wang, H.; Mei, W.L.; Dai, H.F. Natural Products in Agarwood and Aquilaria Plants: Chemistry, Biological Activities and Biosynthesis. Nat. Prod. Rep. 2021, 38, 528–565. [Google Scholar] [CrossRef]
- Choi, W.H.; Son, H.J.; Jang, Y.J.; Ahn, J.; Jung, C.H.; Ha, T.Y. Apigenin Ameliorates the Obesity-Induced Skeletal Muscle Atrophy by Attenuating Mitochondrial Dysfunction in the Muscle of Obese Mice. Mol. Nutr. Food Res. 2017, 61, 1700218. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, C.S.; Joe, Y.; Chung, H.T.; Ha, T.Y.; Yu, R. Quercetin Reduces Tumor Necrosis Factor Alpha-Induced Muscle Atrophy by Upregulation of Heme Oxygenase-1. J. Med. Food 2018, 21, 551–559. [Google Scholar] [CrossRef]
- Kou, X.; Li, J.; Liu, X.; Yang, X.; Fan, J.; Chen, N. Ampelopsin Attenuates the Atrophy of Skeletal Muscle from D-Gal-Induced Aging Rats through Activating AMPK/SIRT1/PGC-1α Signaling Cascade. Biomed. Pharmacother. 2017, 90, 311–320. [Google Scholar] [CrossRef]
- Kim, C.; Hwang, J.K. The 5,7-Dimethoxyflavone Suppresses Sarcopenia by Regulating Protein Turnover and Mitochondria Biogenesis-Related Pathways. Nutrients 2020, 12, 1079. [Google Scholar] [CrossRef]
- Messina, S.; Bitto, A.; Aguennouz, M.; Vita, G.L.; Polito, F.; Irrera, N.; Altavilla, D.; Marini, H.; Migliorato, A.; Squadrito, F.; et al. The Soy Isoflavone Genistein Blunts Nuclear Factor Kappa-B, MAPKs and TNF-α Activation and Ameliorates Muscle Function and Morphology in Mdx Mice. Neuromuscul. Disord. 2011, 21, 579–589. [Google Scholar] [CrossRef]
- Aoyama, S.; Jia, H.; Nakazawa, K.; Yamamura, J.; Saito, K.; Kato, H. Dietary Genistein Prevents Denervation-Induced Muscle Atrophy in Male Rodents Via Effects on Estrogen Receptor-α. J. Nutr. 2016, 146, 1147–1154. [Google Scholar] [CrossRef] [PubMed]
- Marinello, P.C.; Bernardes, S.S.; Guarnier, F.A.; Da Silva, T.N.X.; Borges, F.H.; Lopes, N.M.D.; Simão, A.N.C.; Armani, A.; Cecchini, R.; Cecchini, A.L. Isoflavin-β Modifies Muscle Oxidative Stress and Prevents a Thyrotoxicosis-Induced Loss of Muscle Mass in Rats. Muscle Nerve 2017, 56, 975–981. [Google Scholar] [CrossRef]
- Murata, M.; Kosaka, R.; Kurihara, K.; Yamashita, S.; Tachibana, H. Delphinidin Prevents Disuse Muscle Atrophy and Reduces Stress-Related Gene Expression. Biosci. Biotechnol. Biochem. 2016, 80, 1636–1640. [Google Scholar] [CrossRef]
- Murata, M.; Nonaka, H.; Komatsu, S.; Goto, M.; Morozumi, M.; Yamada, S.; Lin, I.C.; Yamashita, S.; Tachibana, H. Delphinidin Prevents Muscle Atrophy and Upregulates miR-23a Expression. J. Agric. Food Chem. 2017, 65, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Mukai, R.; Horikawa, H.; Fujikura, Y.; Kawamura, T.; Nemoto, H.; Nikawa, T.; Terao, J. Prevention of Disuse Muscle Atrophy by Dietary Ingestion of 8-Prenylnaringenin in Denervated Mice. PLoS ONE 2012, 7, e45048. [Google Scholar] [CrossRef] [PubMed]
- Shukla, S.K.; Dasgupta, A.; Mehla, K.; Gunda, V.; Vernucci, E.; Souchek, J.; Goode, G.; King, R.; Mishra, A.; Rai, I.; et al. Silibinin-Mediated Metabolic Reprogramming Attenuates Pancreatic Cancer-Induced Cachexia and Tumor Growth. Oncotarget 2015, 6, 41146–41161. [Google Scholar] [CrossRef] [PubMed]
- Tong, T.; Kim, M.; Fau-Park, T.; Park, T. α-Ionone Attenuates High-Fat Diet-Induced Skeletal Muscle Wasting in Mice Via Activation of cAMP Signaling. Food Funct. 2019, 10, 1167–1178. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Yang, Q.; Zhang, H.; Wan, L.; Xin, B.; Cao, Y.; Zhang, J.; Guo, C. Cryptotanshinone Prevents Muscle Wasting in CT26-Induced Cancer Cachexia through Inhibiting Stat3 Signaling Pathway. J. Ethnopharmacol. 2020, 260, 113066. [Google Scholar] [CrossRef] [PubMed]
- Le, N.H.; Kim, C.S.; Park, T.; Park, J.H.; Sung, M.K.; Lee, D.G.; Hong, S.M.; Choe, S.Y.; Goto, T.; Kawada, T.; et al. Quercetin Protects against Obesity-Induced Skeletal Muscle Inflammation and Atrophy. Mediat. Inflamm. 2014, 2014, 834294. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Chen, K.; Ren, Q.; Yi, L.; Zhu, J.; Zhang, Q.; Mi, M. Dihydromyricetin Attenuates Dexamethasone-Induced Muscle Atrophy by Improving Mitochondrial Function Via the PGC-1α Pathway. Cell. Physiol. Biochem. 2018, 49, 758–779. [Google Scholar] [CrossRef]
- Lovegrove, A.; Edwards, C.H.; De Noni, I.; Patel, H.; El, S.N.; Grassby, T.; Zielke, C.; Ulmius, M.; Nilsson, L.; Butterworth, P.J.; et al. Role of Polysaccharides in Food, Digestion, and Health. Crit. Rev. Food Sci. Nutr. 2017, 57, 237–253. [Google Scholar] [CrossRef]
- Lu, L.; Wang, D.T.; Shi, Y.; Yin, Y.; Wei, L.B.; Zou, Y.C.; Huang, B.; Zhao, Y.; Wang, M.; Wan, H.; et al. Astragalus Polysaccharide Improves Muscle Atrophy from Dexamethasone- and Peroxide-Induced Injury in Vitro. Int. J. Biol. Macromol. 2013, 61, 7–16. [Google Scholar] [CrossRef]
- Lim, J.M.; Lee, Y.J.; Cho, H.R.; Park, D.C.; Jung, G.W.; Ku, S.K.; Choi, J.S. Extracellular Polysaccharides Purified from Aureobasidium Pullulans SM-2001 (Polycan) Inhibit Dexamethasone-Induced Muscle Atrophy in Mice. Int. J. Mol. Med. 2018, 41, 1245–1264. [Google Scholar] [CrossRef]
- Chen, M.C.; Hsu, W.L.; Hwang, P.A.; Chen, Y.L.; Chou, T.C. Combined Administration of Fucoidan Ameliorates Tumor and Chemotherapy-Induced Skeletal Muscle Atrophy in Bladder Cancer-Bearing Mice. Oncotarget 2016, 7, 51608–51618. [Google Scholar] [CrossRef]
- Park, K.-S.; Kim, H.J.; Hwang, J.T.; Ko, B.S. Dioscorea Nipponica Extracts Enhance Recovery from Skeletal Muscle Atrophy by Suppressing NF-κB Expression. J. Funct. Foods 2020, 73, 104109. [Google Scholar] [CrossRef]
- McBean, S.E.; Church, J.A.O.; Thompson, B.K.; Taylor, C.A.O.; Fitton, J.H.; Stringer, D.N.; Karpiniec, S.S.; Park, A.Y.; van der Poel, C.A.O. Oral Fucoidan Improves Muscle Size and Strength in Mice. Physiol. Rep. 2021, 9, e14730. [Google Scholar] [CrossRef]
- Chen, L.; Chen, L.; Wan, L.; Huo, Y.; Huang, J.; Li, J.; Lu, J.; Xin, B.; Yang, Q.; Guo, C. Matrine Improves Skeletal Muscle Atrophy by Inhibiting E3 Ubiquitin Ligases and Activating the Akt/mTOR/FoxO3α Signaling Pathway in C2C12 Myotubes and Mice. Oncol. Rep. 2019, 42, 479–494. [Google Scholar] [CrossRef]
- Lee, H.; Tuong, L.T.; Jeong, J.H.; Lee, S.J.; Bae, G.U.; Ryu, J.H. Isoquinoline Alkaloids from Coptis Japonica Stimulate the Myoblast Differentiation Via P38 MAP-Kinase and Akt Signaling Pathway. Bioorg. Med. Chem. Lett. 2017, 27, 1401–1404. [Google Scholar] [CrossRef] [PubMed]
- Yadav, A.; Singh, A.; Phogat, J.; Dahuja, A.; Dabur, R. Magnoflorine Prevent the Skeletal Muscle Atrophy Via Akt/mTOR/FoxO Signal Pathway and Increase Slow-MyHC Production in Streptozotocin-Induced Diabetic Rats. J. Ethnopharmacol. 2021, 267, 113510. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Lee, S.J.; Bae, G.U.; Baek, N.I.; Ryu, J.H. Canadine from Corydalis turtschaninovii Stimulates Myoblast Differentiation and Protects against Myotube Atrophy. Int. J. Mol. Sci. 2017, 18, 2748. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Yoo, M.; Go, G.Y.; Hwang, J.; Lee, H.G.; Kim, Y.K.; Seo, D.W.; Baek, N.I.; Ryu, J.H.; Kang, J.S.; et al. Tetrahydropalmatine Promotes Myoblast Differentiation through Activation of p38MAPK and MyoD. Biochem. Biophys. Res. Commun. 2014, 455, 147–152. [Google Scholar] [CrossRef]
- Dyle, M.C.; Ebert, S.M.; Cook, D.P.; Kunkel, S.D.; Fox, D.K.; Bongers, K.S.; Bullard, S.A.; Dierdorff, J.M.; Adams, C.M. Systems-Based Discovery of Tomatidine as a Natural Small Molecule Inhibitor of Skeletal Muscle Atrophy. J. Biol. Chem. 2014, 289, 14913–14924. [Google Scholar] [CrossRef]
- Fang, E.F.; Waltz, T.B.; Kassahun, H.; Lu, Q.; Kerr, J.S.; Morevati, M.; Fivenson, E.M.; Wollman, B.N.; Marosi, K.; Wilson, M.A.; et al. Tomatidine Enhances Lifespan and Healthspan in C. elegans through Mitophagy Induction Via the SKN-1/Nrf2 Pathway. Sci. Rep. 2017, 7, 46208. [Google Scholar] [CrossRef]
- Kim, H.; Jang, M.; Park, R.; Jo, D.; Choi, I.; Choe, J.; Oh, W.K.; Park, J. Conessine Treatment Reduces Dexamethasone-Induced Muscle Atrophy by Regulating MuRF1 and Atrogin-1 Expression. J. Microbiol. Biotechnol. 2018, 28, 520–526. [Google Scholar] [CrossRef]
- Bin, Y.; Xiao, Y.; Huang, D.; Ma, Z.; Liang, Y.; Bai, J.; Zhang, W.; Liang, Q.; Zhang, J.; Zhong, X.; et al. Theophylline Inhibits Cigarette Smoke-Induced Inflammation in Skeletal Muscle by Upregulating HDAC2 Expression and Decreasing NF-κB Activation. Am. J. Physiol. Lung Cell. Mol. Physiol. 2019, 316, L197–l205. [Google Scholar] [CrossRef]
- Abrigo, J.; Morales, M.G.; Simon, F.; Cabrera, D.; Di Capua, G.; Cabello-Verrugio, C. Apocynin Inhibits the Upregulation of TGF-β1 Expression and ROS Production Induced by TGF-β in Skeletal Muscle Cells. Phytomedicine 2015, 22, 885–893. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Tang, Z.; Wen, L.; Jiang, C.; Feng, Q. Matrine: A Review of Its Pharmacology, Pharmacokinetics, Toxicity, Clinical Application and Preparation Researches. J. Ethnopharmacol. 2021, 269, 113682. [Google Scholar] [CrossRef]
- Aydin, N.B.; Teke, T.; Toy, H.; Uzun, K. The Effect of Theophylline on the Prevention of Mechanical Ventilation-Induced Diaphragm Atrophy in Rats. Adv. Clin. Exp. Med. 2014, 23, 33–38. [Google Scholar] [CrossRef]
- Sharma, B.; Dutt, V.; Kaur, N.; Mittal, A.; Dabur, R. Tinospora Cordifolia Protects from Skeletal Muscle Atrophy by Alleviating Oxidative Stress and Inflammation Induced by Sciatic Denervation. J. Ethnopharmacol. 2020, 254, 112720. [Google Scholar] [CrossRef] [PubMed]
- Cárdenas, P.D.; Almeida, A.; Bak, S. Evolution of Structural Diversity of Triterpenoids. Front. Plant Sci. 2019, 10, 1523. [Google Scholar] [CrossRef] [PubMed]
- Kunkel, S.D.; Suneja, M.; Ebert, S.M.; Bongers, K.S.; Fox, D.K.; Malmberg, S.E.; Alipour, F.; Shields, R.K.; Adams, C.M. mRNA Expression Signatures of Human Skeletal Muscle Atrophy Identify a Natural Compound That Increases Muscle Mass. Cell Metab. 2011, 13, 627–638. [Google Scholar] [CrossRef]
- Kim, J.C.; Kang, Y.S.; Noh, E.B.; Seo, B.W.; Seo, D.Y.; Park, G.D.; Kim, S.H. Concurrent Treatment with Ursolic Acid and Low-Intensity Treadmill Exercise Improves Muscle Atrophy and Related Outcomes in Rats. Korean J. Physiol. Pharmacol. 2018, 22, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.W.; Shim, J.J.; Choi, I.D.; Kim, S.H.; Ra, J.; Ku, H.K.; Lee, D.E.; Kim, T.Y.; Jeung, W.; Lee, J.H.; et al. Apple Pomace Extract Improves Endurance in Exercise Performance by Increasing Strength and Weight of Skeletal Muscle. J. Med. Food 2015, 18, 1380–1386. [Google Scholar] [CrossRef]
- Li, F.; Li, X.; Peng, X.; Sun, L.; Jia, S.; Wang, P.; Ma, S.; Zhao, H.; Yu, Q.; Huo, H. Ginsenoside Rg1 Prevents Starvation-Induced Muscle Protein Degradation Via Regulation of AKT/mTOR/FoxO Signaling in C2C12 Myotubes. Exp. Ther. Med. 2017, 14, 1241–1247. [Google Scholar] [CrossRef]
- Lee, S.J.; Bae, J.H.; Lee, H.; Lee, H.; Park, J.; Kang, J.S.; Bae, G.U. Ginsenoside Rg3 Upregulates Myotube Formation and Mitochondrial Function, Thereby Protecting Myotube Atrophy Induced by Tumor Necrosis Factor-Alpha. J. Ethnopharmacol. 2019, 242, 112054. [Google Scholar] [CrossRef] [PubMed]
- Go, G.Y.; Jo, A.; Seo, D.W.; Kim, W.Y.; Kim, Y.K.; So, E.Y.; Chen, Q.; Kang, J.S.; Bae, G.U.; Lee, S.J. Ginsenoside Rb1 and Rb2 Upregulate Akt/mTOR Signaling-Mediated Muscular Hypertrophy and Myoblast Differentiation. J. Ginseng Res. 2020, 44, 435–441. [Google Scholar] [CrossRef]
- Seok, Y.M.; Yoo, J.M.; Nam, Y.; Kim, J.; Kim, J.S.; Son, J.H.; Kim, H.J. Mountain Ginseng Inhibits Skeletal Muscle Atrophy by Decreasing Muscle Ring finger Protein-1 and Atrogin1 through Forkhead Box O3 in L6 Myotubes. J. Ethnopharmacol. 2021, 270, 113557. [Google Scholar] [CrossRef]
- Jiang, R.; Wang, M.; Shi, L.; Zhou, J.; Ma, R.; Feng, K.; Chen, X.; Xu, X.; Li, X.; Li, T.; et al. Panax Ginseng Total Protein Facilitates Recovery from Dexamethasone-Induced Muscle Atrophy through the Activation of Glucose Consumption in C2C12 Myotubes. BioMed Res. Int. 2019, 2019, 3719643. [Google Scholar] [CrossRef] [PubMed]
- Baek, S.; Kim, J.; Moon, B.S.; Park, S.M.; Jung, D.E.; Kang, S.Y.; Lee, S.J.; Oh, S.J.; Kwon, S.H.; Nam, M.H.; et al. Camphene Attenuates Skeletal Muscle Atrophy by Regulating Oxidative Stress and Lipid Metabolism in Rats. Nutrients 2020, 12, 3731. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; Yuan, Y.; Liao, Z.; Xing, K.; Zhu, C.; Xu, Y.; Yu, L.; Wang, L.; Wang, S.; Zhu, X.; et al. α-Ketoglutarate Prevents Skeletal Muscle Protein Degradation and Muscle Atrophy through PHD3/ADRB2 Pathway. FASEB J. 2018, 32, 488–499. [Google Scholar] [CrossRef]
- Kaur, N.; Gupta, P.; Saini, V.; Sherawat, S.; Gupta, S.; Dua, A.; Kumar, V.; Injeti, E.; Mittal, A. Cinnamaldehyde Regulates H2O2-Induced Skeletal Muscle Atrophy by Ameliorating the Proteolytic and Antioxidant Defense Systems. J. Cell. Physiol. 2019, 234, 6194–6208. [Google Scholar] [CrossRef]
- Yoshikawa, M.; Hosokawa, M.; Miyashita, K.; Nishino, H.; Hashimoto, T. Effects of Fucoxanthin on the Inhibition of Dexamethasone-Induced Skeletal Muscle Loss in Mice. Nutrients 2021, 13, 1079. [Google Scholar] [CrossRef]
- Han, Y.H.; Mun, J.G.; Jeon, H.D.; Yoon, D.H.; Choi, B.M.; Kee, J.Y.; Hong, S.H. The Extract of Arctium lappa L. Fruit (Arctii Fructus) Improves Cancer-Induced Cachexia by Inhibiting Weight Loss of Skeletal Muscle and Adipose Tissue. Nutrients 2020, 12, 3195. [Google Scholar] [CrossRef]
- Bindels, L.B.; Beck, R.; Schakman, O.; Martin, J.C.; De Backer, F.; Sohet, F.M.; Dewulf, E.M.; Pachikian, B.D.; Neyrinck, A.M.; Thissen, J.P.; et al. Restoring Specific Lactobacilli Levels Decreases Inflammation and Muscle Atrophy Markers in an Acute Leukemia Mouse Model. PLoS ONE 2012, 7, e37971. [Google Scholar] [CrossRef]
- Chen, Y.M.; Wei, L.; Chiu, Y.S.; Hsu, Y.J.; Tsai, T.Y.; Wang, M.F.; Huang, C.C. Lactobacillus plantarum TWK10 Supplementation Improves Exercise Performance and Increases Muscle Mass in Mice. Nutrients 2016, 8, 205. [Google Scholar] [CrossRef]
- Schieber, A.M.; Lee, Y.M.; Chang, M.W.; Leblanc, M.; Collins, B.; Downes, M.; Evans, R.M.; Ayres, J.S. Disease Tolerance Mediated by Microbiome E. coli Involves Inflammasome and IGF-1 Signaling. Science 2015, 350, 558–563. [Google Scholar] [CrossRef] [PubMed]
- Ni, Y.; Yang, X.; Zheng, L.; Wang, Z.; Wu, L.; Jiang, J.; Yang, T.; Ma, L.; Fu, Z. Lactobacillus and Bifidobacterium Improves Physiological Function and Cognitive Ability in Aged Mice by the Regulation of Gut Microbiota. Mol. Nutr. Food Res. 2019, 63, e1900603. [Google Scholar] [CrossRef]
- Kok, C.R.; Hutkins, R. Yogurt and other fermented foods as sources of health-promoting bacteria. Nutr. Rev. 2018, 76, 4–15. [Google Scholar] [CrossRef]
- Iwasa, M.; Aoi, W.; Mune, K.; Yamauchi, H.; Furuta, K.; Sasaki, S.; Takeda, K.; Harada, K.; Wada, S.; Nakamura, Y.; et al. Fermented Milk Improves Glucose Metabolism in Exercise-Induced Muscle Damage in Young Healthy Men. Nutr. J. 2013, 12, 83. [Google Scholar] [CrossRef] [PubMed]
- An, J.M.; Kang, E.A.; Han, Y.M.; Oh, J.Y.; Lee, D.Y.; Choi, S.H.; Kim, D.H.; Hahm, K.B. Dietary Intake of Probiotic Kimchi Ameliorated Il-6-Driven Cancer Cachexia. J. Clin. Biochem. Nutr. 2019, 65, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Buigues, C.; Fernández-Garrido, J.; Pruimboom, L.; Hoogland, A.J.; Navarro-Martínez, R.; Martínez-Martínez, M.; Verdejo, Y.; Mascarós, M.C.; Peris, C.; Cauli, O. Effect of a Prebiotic Formulation on Frailty Syndrome: A Randomized, Double-Blind Clinical Trial. Int. J. Mol. Sci. 2016, 17, 932. [Google Scholar] [CrossRef]
- Lahiri, S.; Kim, H.; Garcia-Perez, I.; Reza, M.M.; Martin, K.A.; Kundu, P.; Cox, L.M.; Selkrig, J.; Posma, J.M.; Zhang, H.; et al. The Gut Microbiota Influences Skeletal Muscle Mass and Function in Mice. Sci. Transl. Med. 2019, 11, eaan5662. [Google Scholar] [CrossRef]
- Wang, L.L.; Guo, H.H.; Huang, S.; Feng, C.L.; Han, Y.X.; Jiang, J.D. Comprehensive Evaluation of SCFA Production in the Intestinal Bacteria Regulated by Berberine Using Gas-Chromatography Combined with Polymerase Chain Reaction. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2017, 1057, 70–80. [Google Scholar] [CrossRef]
- Kawabata, K.; Yoshioka, Y.; Terao, J. Role of Intestinal Microbiota in the Bioavailability and Physiological Functions of Dietary Polyphenols. Molecules 2019, 24, 370. [Google Scholar] [CrossRef] [PubMed]
| Minerals | Structure | Example Source | Inducer | Model | Effect | Mechanism | Ref |
|---|---|---|---|---|---|---|---|
| Magnesium | / | Egg, meat | Aging | Human | ↑ Muscle strength | / | [52] |
| Calcium | / | Egg, meat | Calcium/magnesium deficiency | Human | ↑ Muscle mass, strength, and physical performance | / | [50] |
| Selenium | / | Egg, meat | Selenium deficiency | Human | / | / | [53] |
| Aging | C57BL/6 mice | ↑ Muscle performance | ↑ Ca2+ flux, oxidative stress tolerance | [54] | |||
| Tumor | C57BL/6 mice | ↓ Inflammation, muscle atrophy | ↓ IL-6, TNF-α, myostatin | [55] |
| Polyphenols | Structure | Example Source | Inducer | Model | Effect | Mechanism | Ref |
|---|---|---|---|---|---|---|---|
| Curcumin |  | Turmeric | Streptozotocin | C57BL/6J mice | ↑ Muscle weight | ↓ NF-κB, TNF-α, IL-1β ↓ MuRF1, MAFbx | [84] |
| Chronic hypobaric hypoxia | SD rats | ↑ Muscle mass and improved physical performance | ↓ Muscle proteolysis | [85] | |||
| Resveratrol |  | Red wine | Streptozotocin | C57BL/6J mice | ↑ Muscle weight, fiber size | ↑ Mitochondrial biogenesis ↓ MuRF-1, cleaved caspase-3, mitophagy | [86] |
| C26 adenocarcinoma | CD2F1 mice | ↑ Muscle mass | ↓ NF-κB, MuRF1 | [87] | |||
| Denervation | ICR mice | ↑ Muscle weight | ↓ MAFbx | [88] | |||
| Astaxanthin |  | Shrimp, crab | Immobilization | Wistar rats | ↑ Muscle mass | ↓ Oxidative stress, proteolysis, apoptosis, ROS | [89] |
| Epicatechin gallate |  | Green tea | Cardiotoxin | C57BL/6 mice | ↑ Muscle fiber size | ↑ Myf5, MyoD | [90] |
| Epicatechin |  | Cocoa, green tea | Aging | ICR mice | ↑ Bone mass | ↑ MyoD, SOD ↓ MuRF1 | [91] |
| Epigallocatechin-3-gallate |  | Green tea | Aging | SD rats | ↑ Muscle mass, muscle fiber cross-sectional areas | ↑ IGF-1, IL-15 ↓ MuRF1, MAFbx | [92] |
| Pomegranate extract | / | Pomegranate | TNF-α | C57BL/6 mice | ↑ Muscle mass | ↓ Oxidative stress, NF-κB activation, Akt/mTOR signaling | [93] |
| Urolithin A |  | Pomegranate | Aging/ | Human | ↑ Muscle founction | ↑ Mitochondrial founction | [94] |
| Aging/HFD | C57BL/6J mice | ↑ Muscle founction | ↑ Mitochondrial founction | [95] | |||
| / | C2C12 cells | / | ↑ Mitochondrial founction | [95] | |||
| / | C. elegans | ↑ Lifespan, muscle heath | ↑ Mitochondrial founction | [95] | |||
| Urolithin B |  | Pomegranate | Denervation | Mice | ↑ Muscle weight | ↓ FoxO1, FoxO3, MAFbx MuRF1 | [96] |
| / | C2C12 cells | ↑ Protein synthesis | ↑ mTORC1 signaling | [96] | |||
| Glabridin | 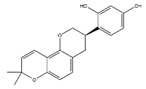 | Licorice | Dexamethasone | C2C12 cells | ↑ Muscle protein | ↓ MuRF1 | [97] |
| Flavan 3-ol |  | Cocoa | Hindlimb suspension | C57BL/6J mice | ↑ Muscle mass | ↓ MuRF1 | [98] |
| Oligonol | / | Lychee | / | db/db mice | ↑ Muscle fiber size | ↑ Sirtuin 1 ↓ MuRF1, MAFbx, FoxO3a | [99] |
| Palmitate | C2C12 cells | ↑ Myotube differentiation | ↓ MuRF1, MAFbx | [99] | |||
| Magnolol | 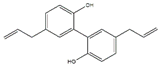 | Magnolia officinalis | Bladder cancer | BALB/c mice | ↑ Muscle protein ↓ inflammation | ↑ IGF-1 ↓ MuRF1, MAFbx, FoxO3a | [100] |
| Corylifol A |  | Psoralea corylifolia L. | Dexamethasone | C2C12 cells | ↑ Mononuclear myotubes | ↑ p38 MAPK ↓ MuRF1, MAFbx | [101] |
| Flavonoids | Structure | Example Source | Inducer | Model | Effect | Mechanism | Ref |
|---|---|---|---|---|---|---|---|
| Apigenin | 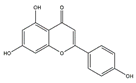 | Parsley, celery, and grapefrui | HFD | C57BL/6 mice | ↑ Exercise capacity | ↓ MuRF1, MAFbx | [110] |
| Palmitic acid | C2C12 cells | / | ↑ Mitochondrial content | [110] | |||
| Quercetin | 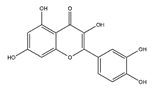 | Onions | HFD | C57BL/6J mice | ↑ Muscle mass, muscle fiber size | ↓ Nrf2, NF-κB, TNF-α ↓ MuRF1, MAFbx | [111] |
| Ampelopsin (dihydromyricetin) |  | Rattan tea (Ampelopsis grossedentata) | D-galactose /Dexamethasone | SD rats | ↑ Muscle strength, fiber cross-sectional area | ↑ Myotube diameter, mitochondrial content, Tfam, PGC-1α | [112] |
| 5,7-Dimethoxyflavone |  | Black ginger (Kaempferia parviflora) | Aging | C57BL/6 mice | ↑ Muscle mass, strength | ↑ Muscle mass, mitochondrial content, Tfam, PGC-1α ↓ MuRF1, MAFbx | [113] |
| Genistein |  | Soybean | / | mdx mice | ↑ Muscle function and morphology | ↑ Muscle function, morphology ↓ NF-κB, TNF-α | [114] |
| Denervation | C57BL6/J mice | ↑ Muscle strength | ↓ MuRF1, MAFbx | [115] | |||
| Isoflavin-β | / | Soybean | Thyrotoxicosis | Wistar rats | ↑ Muscle mass | ↑ Mitochondrial cytochrome oxidase activity | [116] |
| Delphinidin | 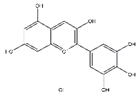 | Blueberry | Disuse | C57BL/6J mice | ↑ Muscle weight | ↑ NFATc3, miR-23a ↓ MuRF1 | [117,118] |
| 8-Prenylnaringenin | 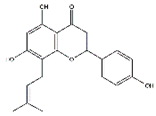 | Hop (Humulus lupulus) | Denervation | C57BL/6 mice | ↑ Muscle weight | ↑ Akt, IGF-1 | [119] |
| Silibinin | 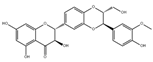 | Milk thistle (Silybum marianum) | Pancreatic cancer | NCr-nu/nu mice | ↑ Muscle strength | ↓ MuRF1, MAFbx | [120] |
| α-Ionone | 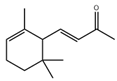 | Violets, blackberries, plums | HFD | C57BL/6N | ↑ Muscle weight/strength | ↑ cAMP ↓ MuRF1, MAFbx | [121] |
| Palmitic acid | C2C12 cells | ↑ Myotube size | ↑ cAMP, MyoD, Myogenin ↓ MuRF1, MAFbx | [121] | |||
| Cryptotanshinone |  | Danshen | CT26 colon carcinoma | BALB/c mice | ↑ Muscle mass | ↓ MuRF1, MAFbx ↓ STAT3 signaling | [122] |
| C2C12 cells | / | ↓ MuRF1, MAFbx | [122] |
| Polysaccharides | Structure | Example Source | Inducer | Model | Effect | Mechanism | Ref |
|---|---|---|---|---|---|---|---|
| Astragalus polysaccharide | / | Astragalus membranaceus Bunge | Dexamethasone | C2C12 cells | ↑ Myotube diameter | ↑ Akt, mTOR, p70S6K, rpS6 | [126] |
| Extracellular polysaccharides | / | Aureobasidium pullulans | Dexamethasone | ICR mice | ↑ Calf thickness, calf muscle strength, gastrocnemius muscle thickness and weight | ↑ AkT, PI3K ↓ MAFbx, MuRF1, myostatin, sirtuin 1 | [127] |
| Fucoidan | 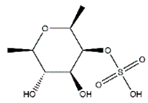 | Brown algae | Cancer cachexia, chemotherapy | BALB/c mice | ↑ Body weight, muscle weight | ↓ Inflammation ↓ FoxO3, MuRF1, MAFbx ↑ IGF-1 signaling | [128] |
| Alkaloids | Structure | Example Source | Inducer | Model | Effect | Mechanism | Ref |
|---|---|---|---|---|---|---|---|
| Matrine |  | Sophora flavescens | Cachexia | Mice | ↑ Muscle fiber size, muscle mass | ↓ MuRF1, MAFbx | [131] |
| Dexamethasone | C2C12 cells | ↓ Apoptosis | ↑ Akt/mTOR/p-FoxO3a ↓ MuRF1, MAFbx | [131] | |||
| Isoquinoline alkaloids | / | Coptis japonica | / | C2C12 cells | ↑ Myoblast differentiation | ↑ p38/MAPK, Akt | [132] |
| Magnoflorine | 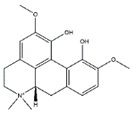 | Coptis japonica | CT26 colon carcinoma | C2C12 cells | ↑ Myoblast differentiation | ↑ p38/MAPK, Akt ↓ MuRF1, MAFbx | [132,133] |
| Streptozotocin | Wistar rats | ↑ Muscle mass | ↓ MAFbx, MuRF-1 | [133] | |||
| Canadine | 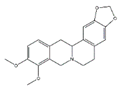 | Corydalis turtschaninovii | CT26 colon carcinoma | C2C12 cells | ↑ Myoblast Differentiation | ↑ p38/MAPK, Akt signaling ↓ MAFbx, MuRF1 | [134] |
| Tetrahydropalmatine |  | Corydalis turtschaninovii | / | C2C12 cells | ↑ Myoblast Differentiation | ↑ p38/MAPK, Akt signaling | [135] |
| Tomatidine |  | Tomatoes | Aging | C57BL/6 mice | ↑ Muscle mass | ↑ mTOR signaling | [136] |
| / | Human skeletal myotubes, C2C12 cells | ↑ Myotube size | ↑ mTOR signaling | [136] | |||
| Aging | C. elegans | ↑ Muscle function | ↑ Nrf2 signaling, mitophagy antioxidant | [137] | |||
| Conessine | 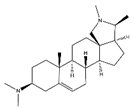 | / | H2O2 | C2C12 cells | ↑ Myoblast Differentiation | ↓ MuRF1, MAFbx | [138] |
| Theophylline | 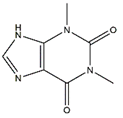 | Green tea | Cigarette smoke | Kunming mice | ↓ Inflammation | ↑ Histone deacetylase 2 ↓ IL-8, TNF-α, NF-κB | [139] |
| Cigarette smoke extract | C2C12 cells | ↓ Inflammation | ↑ Histone deacetylase 2 ↓ IL-8, TNF-α, NF-κB | [139] | |||
| Apocynin | 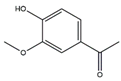 | Picrorhiza kurroa Royle ex Benth (Scrophulariaceae) | TGF-β1 | C2C12 cells | ↑ Myotubes differentiation | ↓ TGF-β1, ROS | [140] |
| Others | Structure | Example Source | Inducer | Model | Effect | Mechanism | Ref |
|---|---|---|---|---|---|---|---|
| α-Ketoglutarate | 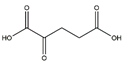 | / | Corticosterone | C57BL/6J mice | ↑ Muscle mass | ↓ MuRF1, MAFbx | [154] |
| C2C12 cells | ↑ Myotube size | ↓ MuRF1, MAFbx | [154] | ||||
| Cinnamaldehyde |  | Cinnamon | H2O2 | C2C12 cells | ↑ Myotube diameter | ↓ MuRF1, MAFbx ↓ Oxidative stress | [155] |
| Fucoxanthin | 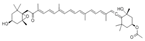 | Undaria pinnatifida | Dexamethasone | ICR mice | ↑ Muscle mass | ↓ Oxidative stress | [156] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Liu, Q.; Quan, H.; Kang, S.-G.; Huang, K.; Tong, T. Nutraceuticals in the Prevention and Treatment of the Muscle Atrophy. Nutrients 2021, 13, 1914. https://doi.org/10.3390/nu13061914
Wang Y, Liu Q, Quan H, Kang S-G, Huang K, Tong T. Nutraceuticals in the Prevention and Treatment of the Muscle Atrophy. Nutrients. 2021; 13(6):1914. https://doi.org/10.3390/nu13061914
Chicago/Turabian StyleWang, Yanan, Qing Liu, Helong Quan, Seong-Gook Kang, Kunlun Huang, and Tao Tong. 2021. "Nutraceuticals in the Prevention and Treatment of the Muscle Atrophy" Nutrients 13, no. 6: 1914. https://doi.org/10.3390/nu13061914
APA StyleWang, Y., Liu, Q., Quan, H., Kang, S.-G., Huang, K., & Tong, T. (2021). Nutraceuticals in the Prevention and Treatment of the Muscle Atrophy. Nutrients, 13(6), 1914. https://doi.org/10.3390/nu13061914







