The Association between Nutritional Status and In-Hospital Mortality among Patients with Heart Failure—A Result of the Retrospective Nutritional Status Heart Study 2 (NSHS2)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Population
2.3. Nutritional Screening
2.4. Data Collection
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Group
3.2. Subgroup Analysis According to BMI
3.3. Subgroup Analysis According to NRS
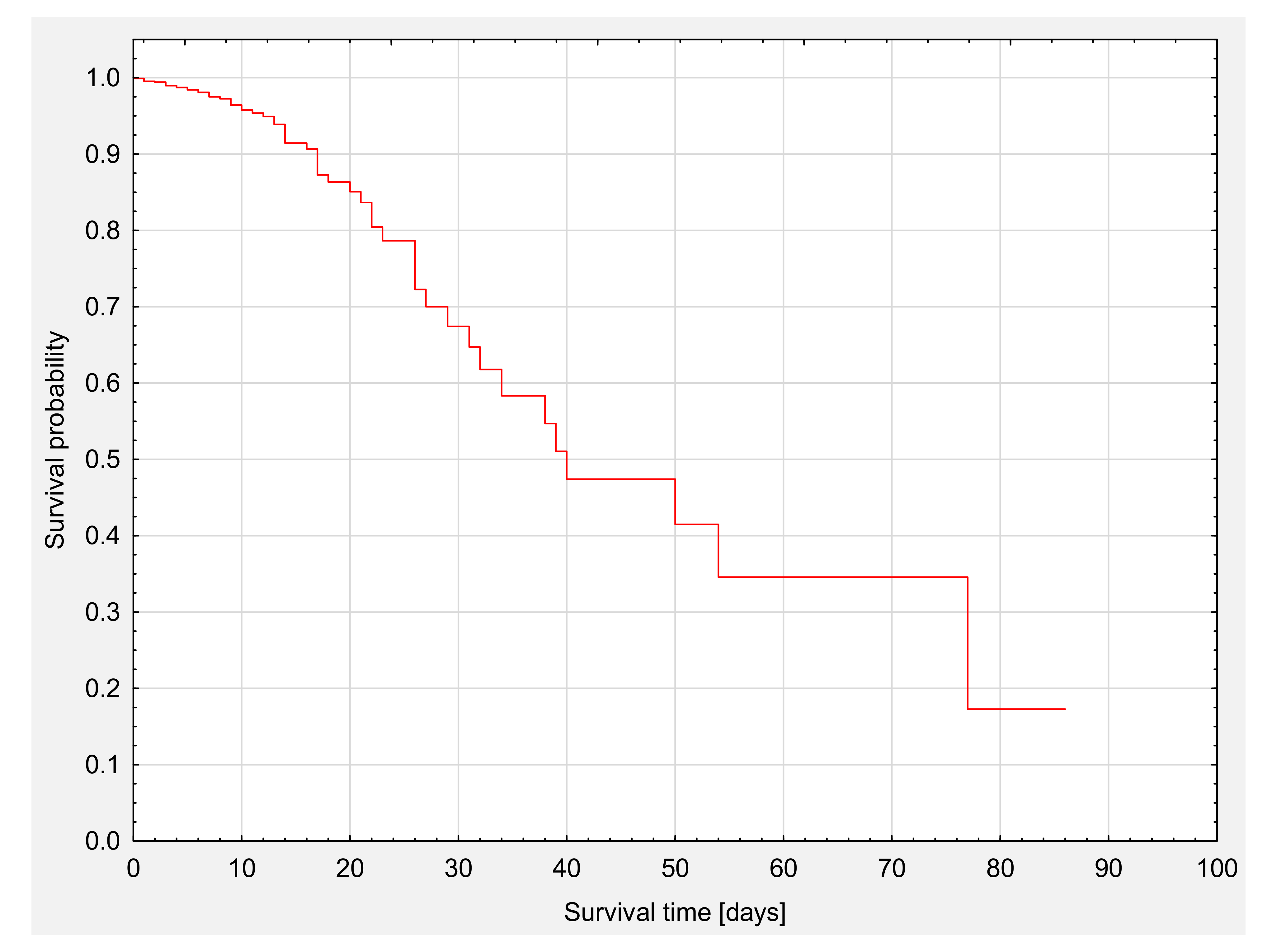
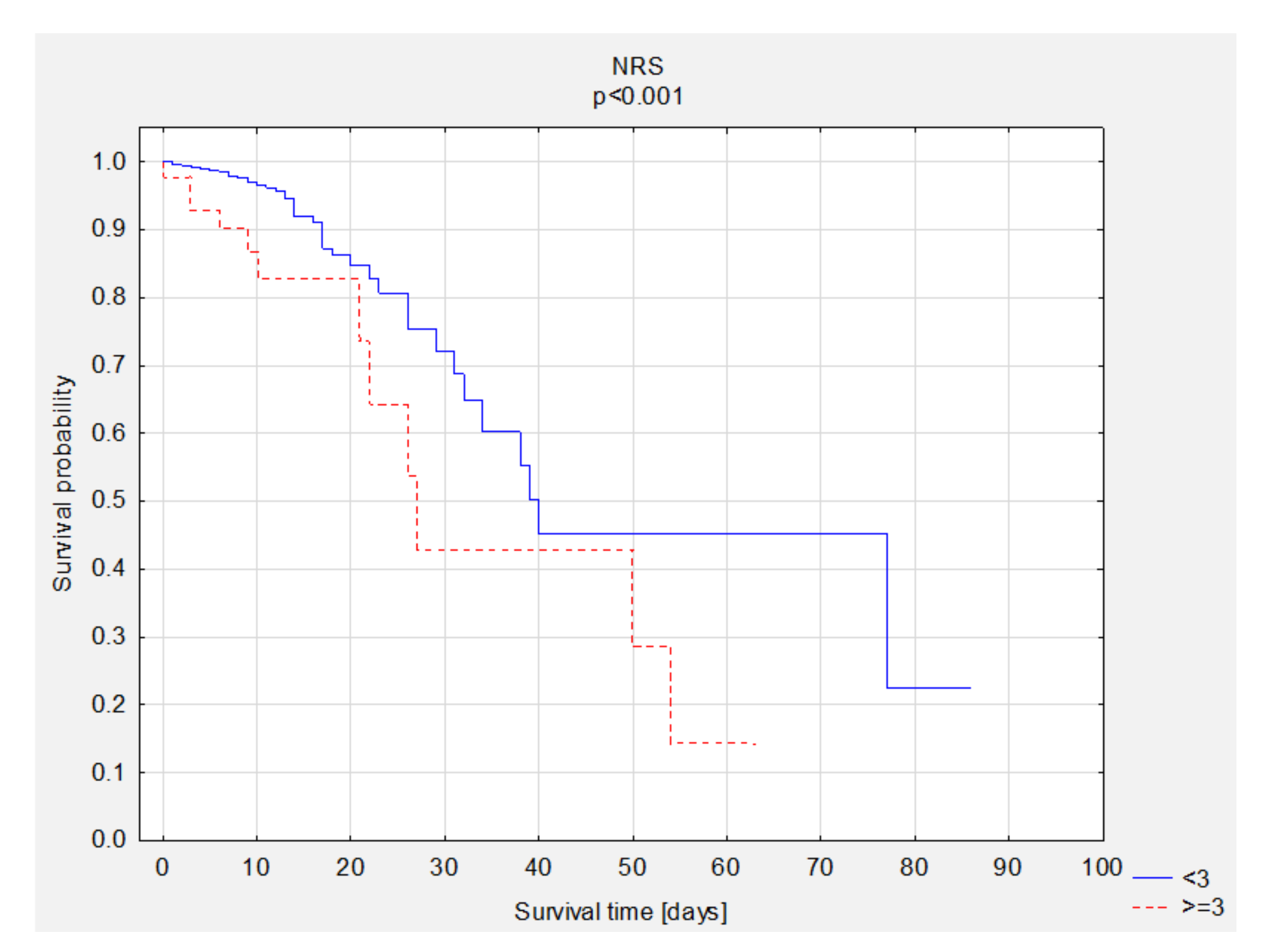
3.4. Survival Analysis
3.5. Survival Analysis—Group Comparisons
4. Discussion
Study Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K.; et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1–25. [Google Scholar] [CrossRef]
- Liu, K.; Daviglus, M.L.; Loria, C.M.; Colangelo, L.A.; Spring, B.; Moller, A.C.; Lloyd-Jones, D.M. Healthy Lifestyle Through Young Adulthood and the Presence of Low Cardiovascular Disease Risk Profile in Middle Age. Circulation 2012, 125, 996–1004. [Google Scholar] [CrossRef]
- Gerber, Y.; Weston, S.A.; Redfield, M.M.; Chamberlain, A.M.; Manemann, S.M.; Jiang, R.; Killian, J.M.; Roger, V.L. A Contemporary Appraisal of the Heart Failure Epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern. Med. 2015, 175, 996–1004. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.-P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Hear. J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef]
- Aggarwal, M.; Bozkurt, B.; Panjrath, G.; Aggarwal, B.; Ostfeld, R.J.; Barnard, N.D.; Gaggin, H.; Freeman, A.M.; Allen, K.; Madan, S.; et al. Lifestyle Modifications for Preventing and Treating Heart Failure. J. Am. Coll. Cardiol. 2018, 72, 2391–2405. [Google Scholar] [CrossRef]
- Egerstedt, A.; Berntsson, J.; Smith, M.L.; Gidlöf, O.; Nilsson, R.; Benson, M.; Wells, Q.S.; Celik, S.; Lejonberg, C.; Farrell, L.; et al. Profiling of the plasma proteome across different stages of human heart failure. Nat. Commun. 2019, 10, 5830. [Google Scholar] [CrossRef]
- Rahman, A.; Jafry, S.; Jeejeebhoy, K.; Nagpal, A.D.; Pisani, B.; Agarwala, R. Malnutrition and Cachexia in Heart Failure. J. Parenter. Enter. Nutr. 2015, 40, 475–486. [Google Scholar] [CrossRef]
- Plauth, M.; Bernal, W.; Dasarathy, S.; Merli, M.; Plank, L.D.; Schütz, T.; Bischoff, S.C. ESPEN guideline on clinical nutrition in liver disease. Clin. Nutr. 2019, 38, 485–521. [Google Scholar] [CrossRef]
- Poehlman, E.T.; Scheffers, J.; Gottlieb, S.S.; Fisher, M.L.; Vaitekevicius, P. Increased Resting Metabolic Rate in Patients with Congestive Heart Failure. Ann. Intern. Med. 1994, 121, 860–862. [Google Scholar] [CrossRef]
- Sharma, A.; Lavie, C.J.; Borer, J.S.; Vallakati, A.; Goel, S.; Lopez-Jimenez, F.; Arbab-Zadeh, A.; Mukherjee, D.; Lazar, J.M. Meta-Analysis of the Relation of Body Mass Index to All-Cause and Cardiovascular Mortality and Hospitalization in Patients with Chronic Heart Failure. Am. J. Cardiol. 2015, 115, 1428–1434. [Google Scholar] [CrossRef]
- Bonilla-Palomas, J.L.; Gámez-López, A.L.; Anguita-Sánchez, M.P.; Castillo-Domínguez, J.C.; García-Fuertes, D.; Crespín-Crespín, M.; López-Granados, A.; De Lezo, J.S. Impact of Malnutrition on Long-Term Mortality in Hospitalized Patients with Heart Failure. Rev. Española Cardiol. 2011, 64, 752–758. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.; Correia, M.; Gonzalez, M.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM criteria for the diagnosis of malnutrition–A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef]
- Kondrup, J.; Allison, S.; Elia, M.; Vellas, B.; Plauth, M. ESPEN Guidelines for Nutrition Screening 2002. Clin. Nutr. 2003, 22, 415–421. [Google Scholar] [CrossRef]
- Boban, M.; Bulj, N.; Zeljković, M.K.; Radeljić, V.; Krcmar, T.; Trbusic, M.; Delić-Brkljačić, D.; Alebic, T.; Vcev, A. Nutritional Considerations of Cardiovascular Diseases and Treatments. Nutr. Metab. Insights 2019, 12. [Google Scholar] [CrossRef]
- Correia, M.I.T.D.; Perman, M.I.; Pradelli, L.; Omaralsaleh, A.J.; Waitzberg, D.L. Economic burden of hospital malnutrition and the cost–benefit of supplemental parenteral nutrition in critically ill patients in Latin America. J. Med. Econ. 2018, 21, 1047–1056. [Google Scholar] [CrossRef] [PubMed]
- Kałużna-Oleksy, M.; Krysztofiak, H.; Migaj, J.; Wleklik, M.; Dudek, M.; Uchmanowicz, I.; Lesiak, M.; Straburzyńska-Migaj, E. Relationship between Nutritional Status and Clinical and Biochemical Parameters in Hospitalized Patients with Heart Failure with Reduced Ejection Fraction, with 1-Year Follow-Up. Nutrition 2020, 12, 2330. [Google Scholar] [CrossRef]
- Aziz, E.F.; Javed, F.; Pratap, B.; Musat, D.; Nader, A.; Pulimi, S.; Alivar, C.L.; Herzog, E.; Kukin, M.L. Malnutrition as Assessed by Nutritional Risk Index is Associated with Worse Outcome in Patients Admitted with Acute Decompensated Heart Failure: An ACAP-HF Data Analysis. Hear. Int. 2011, 6, e2. [Google Scholar] [CrossRef]
- Lu, Y.-W.; Lu, S.-F.; Chou, R.-H.; Wu, P.-S.; Ku, Y.-C.; Kuo, C.-S.; Chang, C.-C.; Tsai, Y.-L.; Wu, C.-H.; Huang, P.-H. Lipid paradox in patients with acute myocardial infarction: Potential impact of malnutrition. Clin. Nutr. 2019, 38, 2311–2318. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; A Ference, B.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur. Hear. J. 2019, 41, 111–188. [Google Scholar] [CrossRef]
- Charach, G.; George, J.; Roth, A.; Rogowski, O.; Wexler, D.; Sheps, D.; Grosskopf, I.; Weintraub, M.; Keren, G.; Rubinstein, A. Baseline Low-Density Lipoprotein Cholesterol Levels and Outcome in Patients with Heart Failure. Am. J. Cardiol. 2010, 105, 100–104. [Google Scholar] [CrossRef]
- Cho, K.H.; Jeong, M.H.; Ahn, Y.; Kim, Y.J.; Chae, S.C.; Hong, T.J.; Seong, I.W.; Chae, J.K.; Kim, C.J.; Cho, M.C.; et al. Low-Density Lipoprotein Cholesterol Level in Patients with Acute Myocardial Infarction Having Percutaneous Coronary Intervention (the Cholesterol Paradox). Am. J. Cardiol. 2010, 106, 1061–1068. [Google Scholar] [CrossRef]
- Rauchhaus, M.; Clark, A.L.; Doehner, W.; Davos, C.; Bolger, A.; Sharma, R.; Coats, A.J.; Anker, S.D. The relationship between cholesterol and survival in patients with chronic heart failure. J. Am. Coll. Cardiol. 2003, 42, 1933–1940. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.S.; Bui, Q.T.; Jacobs, J.R.; Begelman, S.M.; Miller, D.P.; French, W.J. Relationship Between Serum Low-Density Lipoprotein Cholesterol and In-hospital Mortality Following Acute Myocardial Infarction (The Lipid Paradox). Am. J. Cardiol. 2015, 115, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Cunha, F.M.; Pereira, J.; Ribeiro, A.; Silva, S.; Araújo, J.P.; Leite-Moreira, A.; Bettencourt, P.; Lourenço, P. The cholesterol paradox may be attenuated in heart failure patients with diabetes. Minerva Med. 2020, 110, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Kwon, D.; Yi, J.-J.; Ohrr, H.; Yi, S.-W. Total cholesterol and mortality from ischemic heart disease and overall cardiovascular disease in Korean adults. Medicine 2019, 98, e17013. [Google Scholar] [CrossRef]
- Bae, J.-M.; Yang, Y.-J.; Li, Z.-M.; Ahn, Y.-O. Low Cholesterol is associated with Mortality from Cardiovascular Diseases: A Dynamic Cohort Study in Korean Adults. J. Korean Med. Sci. 2012, 27, 58–63. [Google Scholar] [CrossRef]
- Yousufuddin, M.; Takahashi, P.Y.; Major, B.; Ahmmad, E.; Al-Zubi, H.; Peters, J.; Doyle, T.; Jensen, K.; Al Ward, R.Y.; Sharma, U.; et al. Association between hyperlipidemia and mortality after incident acute myocardial infarction or acute decompensated heart failure: a propensity score matched cohort study and a meta-analysis. BMJ Open 2019, 9, e028638. [Google Scholar] [CrossRef]
- Sionis, A.; Lorite, N.M.; Bueno, H.; Payeras, A.C.; Molina, B.D.; Juanatey, J.R.G.; Urioste, L.M.R.; Gómez, J.L.Z.; Bonet, L.A.; Solé, A.A.; et al. Comments on the 2016 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Rev. Española Cardiol. 2016, 69, 1119–1125. [Google Scholar] [CrossRef]
- Donataccio, M.P.; Vanzo, A.; Bosello, O. Obesity paradox and heart failure. Eat. Weight. Disord. Stud. Anorex. Bulim. Obes. 2020, 1–11. [Google Scholar] [CrossRef]
- Hainer, V.; Aldhoon-Hainerová, I. Obesity Paradox Does Exist. Diabetes Care 2013, 36, S276–S281. [Google Scholar] [CrossRef]
- Clark, A.L.; Chyu, J.; Horwich, T.B. The Obesity Paradox in Men Versus Women with Systolic Heart Failure. Am. J. Cardiol. 2012, 110, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Kenchaiah, S.; Pocock, S.J.; Wang, D.; Finn, P.V.; Zornoff, L.A.; Skali, H.; Pfeffer, M.A.; Yusuf, S.; Swedberg, K.; Michelson, E.L.; et al. Body Mass Index and Prognosis in Patients with Chronic Heart Failure. Circulation 2007, 116, 627–636. [Google Scholar] [CrossRef]
- Hutagalung, R.; Marques, J.; Kobylka, K.; Zeidan, M.; Kabisch, B.; Brunkhorst, F.; Reinhart, K.; Sakr, Y. The obesity paradox in surgical intensive care unit patients. Intensive Care Med. 2011, 37, 1793–1799. [Google Scholar] [CrossRef]
- Niedziela, J.; Hudzik, B.; Niedziela, N.; Gąsior, M.; Gierlotka, M.; Wasilewski, J.; Myrda, K.; Lekston, A.; Poloński, L.; Rozentryt, P. The obesity paradox in acute coronary syndrome: a meta-analysis. Eur. J. Epidemiol. 2014, 29, 801–812. [Google Scholar] [CrossRef] [PubMed]
- Beckman, A.L.; Krumholz, H.A.; Krumholz, H.M. Excess weight and life expectancy after acute myocardial infarction: The obesity paradox reexamined. Am. Heart J. 2016, 172, 173–181. [Google Scholar] [CrossRef]
- Carbone, S.; Lavie, C.J.; Arena, R. Obesity and Heart Failure: Focus on the Obesity Paradox. Mayo Clin. Proc. 2017, 92, 266–279. [Google Scholar] [CrossRef]
- Komici, K.; Vitale, D.F.; Mancini, A.; Bencivenga, L.; Conte, M.; Provenzano, S.; Grieco, F.V.; Visaggi, L.; Ronga, I.; Cittadini, A.; et al. Impact of Malnutrition on Long-Term Mortality in Elderly Patients with Acute Myocardial Infarction. Nutrition 2019, 11, 224. [Google Scholar] [CrossRef] [PubMed]
- Cybulska, B.; Kłosiewicz-Latoszek, L. What does obesity paradox mean in coronary heart disease? Kardiol. Polska 2013, 71, 963–968. [Google Scholar] [CrossRef]
- Di Angelantonio, E.; Bhupathiraju, S.N.; Wormser, D.; Gao, P.; Kaptoge, S.; de Gonzalez, A.B.; Cairns, B.J.; Huxley, R.; Jackson, C.L.; Joshy, G.; et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 2016, 388, 776–786. [Google Scholar] [CrossRef]


| Variables | Total | Death | p-Value * | |||||
|---|---|---|---|---|---|---|---|---|
| No (998) | Yes (58) | |||||||
| n | % | n | % | n | % | |||
| Sex (n = 1056) | M | 704 | 66.7 | 671 | 67.2 | 33 | 56.9 | 0.10 |
| BMI (n = 775) | <18.5 | 12 | 1.5 | 10 | 1.4 | 2 | 5.6 | 0.039 |
| 18.5–24.9 | 203 | 26.2 | 194 | 26.3 | 9 | 25.0 | ||
| 25.0–29.9 | 264 | 34.1 | 247 | 33.4 | 17 | 47.2 | ||
| ≥30 | 296 | 38.2 | 288 | 39.0 | 8 | 22.2 | ||
| NRS (n = 1055) | <3 | 1010 | 95.7 | 964 | 96.7 | 46 | 79.3 | <0.001 |
| ≥3 | 45 | 4.3 | 33 | 3.3 | 12 | 20.7 | ||
| HF phenotype (n = 1056) | HFpEF | 304 | 28.8 | 288 | 28.9 | 15 | 25.9 | <0.001 |
| HFmrEF | 130 | 12.3 | 125 | 12.5 | 16 | 27.6 | ||
| HFrEF | 551 | 52.2 | 529 | 53.0 | 5 | 8.6 | ||
| No information | 71 | 6.7 | 56 | 5.6 | 22 | 37.9 | ||
| NYHA (n = 986) | 1 | 92 | 9.3 | 92 | 9.7 | - | - | <0.001 |
| 2 | 332 | 33.7 | 330 | 34.8 | 2 | 5.4 | ||
| 3 | 309 | 31.3 | 300 | 31.6 | 9 | 24.3 | ||
| 4 | 253 | 25.7 | 227 | 23.9 | 26 | 70.3 | ||
| CKD (n = 1056) | Yes | 395 | 37.4 | 375 | 37.6 | 20 | 34.5 | 0.64 |
| MI (n = 1056) | Yes | 326 | 30.9 | 306 | 30.7 | 20 | 34.5 | 0.54 |
| Type of MI (n = 1056) | No | 730 | 69.1 | 692 | 69.3 | 38 | 65.5 | 0.90 |
| STEMI | 90 | 8.5 | 84 | 8.4 | 6 | 10.3 | ||
| NSTEMI | 213 | 20.2 | 200 | 20.0 | 13 | 22.4 | ||
| No information | 23 | 2.2 | 22 | 2.2 | 1 | 1.7 | ||
| HT (n = 1056) | Yes | 761 | 72.1 | 722 | 72.3 | 39 | 67.2 | 0.40 |
| DM (n = 1056) | Yes | 456 | 43.2 | 428 | 42.9 | 28 | 48.3 | 0.42 |
| CS (n = 1056) | Yes | 124 | 11.7 | 113 | 11.3 | 11 | 19.0 | 0.08 |
| LDL (n = 1001) | <55 mg/dL | 150 | 15.0 | 132 | 13.9 | 18 | 36.7 | <0.001 |
| 55 to <70 mg/dL | 165 | 16.5 | 158 | 16.6 | 7 | 14.3 | ||
| 70 to <100 mg/dL | 364 | 36.4 | 346 | 36.3 | 18 | 36.7 | ||
| 100 to <116 mg/dL | 118 | 11.8 | 115 | 12.1 | 3 | 6.1 | ||
| 116 to <190 mg/dL | 192 | 19.2 | 190 | 20.0 | 2 | 4.1 | ||
| more than 190 mg/dL | 12 | 1.2 | 11 | 1.2 | 1 | 2.0 | ||
| LDL (n = 1001) | ≥70 | 686 | 68.5 | 662 | 69.5 | 24 | 49.0 | 0.003 |
| TG (n = 1009) | <135 | 701 | 69.5 | 668 | 69.7 | 33 | 66.0 | 0.34 |
| 135–200 | 207 | 20.5 | 198 | 20.6 | 9 | 18.0 | ||
| >200 | 101 | 10.0 | 93 | 9.7 | 8 | 16.0 | ||
| HDL (n = 1005) | <40 | 522 | 51.9 | 485 | 50.7 | 37 | 75.5 | 0.001 |
| >40 | 483 | 48.1 | 471 | 49.3 | 12 | 24.5 | ||
| Variables | SD | SD | SD | p-Value ** | ||||
| Age (n = 1056) | 69.73 | 12.92 | 69.27 | 12.95 | 77.72 | 9.20 | <0.001 | |
| BMI [kg/m2] (n = 775) | 28.97 | 6.20 | 29.07 | 6.22 | 27.01 | 5.44 | 0.052 | |
| Height [m] (n = 763) | 169.33 | 9.13 | 169.43 | 9.11 | 167.31 | 9.44 | 0.17 | |
| Body weight [kg] (n = 761) | 82.97 | 19.50 | 83.34 | 19.62 | 75.53 | 15.40 | 0.019 | |
| NT-proBNP [pg/mL] (n = 228) | 8128.43 | 10,973.43 | 8135.63 | 11,085.30 | 7861.77 | 5944.59 | 0.95 | |
| BNP [pg/mL] (n = 775) | 1046.69 | 1445.45 | 993.85 | 1424.94 | 1865.17 | 1528.66 | <0.001 | |
| TG [mg/dL] (n = 1009) | 124.36 | 67.25 | 124.25 | 67.30 | 126.40 | 66.98 | 0.83 | |
| LDL [mg/dL] (n = 1001) | 89.38 | 36.24 | 90.32 | 36.18 | 71.16 | 32.66 | <0.001 | |
| HDL [mg/dL] (n = 1005) | 41.86 | 13.84 | 42.31 | 13.81 | 33.14 | 11.61 | <0.001 | |
| TC [mg/dL] (n = 1010) | 155.79 | 46.66 | 157.49 | 46.66 | 123.16 | 32.70 | <0.001 | |
| CRP [mg/L] (n = 1023) | 16.06 | 32.14 | 14.11 | 28.17 | 49.13 | 63.21 | <0.001 | |
| Albumin [g/dL] (n = 278) | 3.34 | 0.58 | 3.41 | 0.55 | 2.88 | 0.57 | <0.001 | |
| Transferrin [g/L] (n = 261) | 2.45 | 0.63 | 2.47 | 0.61 | 2.14 | 0.73 | 0.029 | |
| Lymphocytes [%] (n = 375) | 20.32 | 9.94 | 21.22 | 9.68 | 11.80 | 8.21 | <0.001 | |
| PCT [ng/mL] (n = 428) | 0.82 | 3.59 | 0.62 | 3.00 | 2.39 | 6.44 | 0.001 | |
| Variables | BMI | p-Value * | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| <18.5 n = 12 | 18.5–24.9 n = 203 | 25.0–29.9 n = 264 | ≥30 n = 296 | |||||||
| n | % | n | % | n | % | n | % | |||
| Sex | M | 4 | 33.3 | 130 | 64.0 | 183 | 69.3 | 205 | 69.3 | 0.041 |
| NRS | <3 | 10 | 83.3 | 189 | 93.1 | 253 | 95.8 | 290 | 98.0 | 0.009 |
| ≥3 | 2 | 16.7 | 14 | 6.9 | 11 | 4.2 | 6 | 2.0 | ||
| HF phenotype | HFpEF | 3 | 25.0 | 49 | 24.1 | 66 | 25.0 | 100 | 33.8 | 0.23 |
| HFmrEF | 2 | 16.7 | 24 | 11.8 | 37 | 14.0 | 30 | 10.1 | ||
| HFrEF | 5 | 41.7 | 113 | 55.7 | 145 | 54.9 | 149 | 50.3 | ||
| No information | 2 | 16.7 | 17 | 8.4 | 16 | 6.1 | 17 | 5.7 | ||
| NYHA | 1 | 2 | 20.0 | 25 | 13.6 | 27 | 10.8 | 20 | 7.1 | 0.26 |
| 2 | 4 | 40.0 | 62 | 33.7 | 95 | 37.8 | 100 | 35.6 | ||
| 3 | 4 | 40.0 | 47 | 25.5 | 69 | 27.5 | 88 | 31.3 | ||
| 4 | 227 | 23.9 | 50 | 27.2 | 60 | 23.9 | 73 | 26.0 | ||
| CKD | Yes | 5 | 41.7 | 72 | 35.5 | 91 | 34.5 | 129 | 43.6 | 0.11 |
| MI | Yes | 3 | 25.0 | 72 | 35.5 | 80 | 30.3 | 78 | 26.4 | 0.18 |
| Type of MI | No | 9 | 75.0 | 131 | 64.5 | 184 | 69.7 | 218 | 73.6 | 0.53 |
| STEMI | 1 | 8.3 | 16 | 7.9 | 18 | 6.8 | 23 | 7.8 | ||
| NSTEMI | 2 | 16.7 | 50 | 24.6 | 53 | 20.1 | 51 | 17.2 | ||
| No information | - | - | 6 | 3.0 | 9 | 3.4 | 4 | 1.4 | ||
| HT | Yes | 9 | 75.0 | 118 | 58.1 | 197 | 74.6 | 239 | 80.7 | <0.001 |
| DM | Yes | 1 | 8.3 | 48 | 23.6 | 123 | 46.6 | 171 | 57.8 | <0.001 |
| CS | Yes | 1 | 8.3 | 25 | 12.3 | 37 | 14.0 | 37 | 12.5 | 0.89 |
| LDL | <55 mg/dL | - | - | 17 | 8.9 | 40 | 15.6 | 48 | 17.1 | 0.09 |
| 55 to <70 mg/dL | - | - | 17 | 8.9 | 40 | 15.6 | 48 | 17.1 | ||
| 70 to <100 mg/dL | 2 | 20.0 | 27 | 14.2 | 42 | 16.3 | 50 | 17.8 | ||
| 100 to <116 mg/dL | 3 | 30.0 | 22 | 11.6 | 26 | 10.1 | 34 | 12.1 | ||
| 116 to <190 mg/dL | 1 | 10.0 | 41 | 21.6 | 56 | 21.8 | 49 | 17.4 | ||
| more than 190 mg/dL | 6 | 3.2 | 2 | 0.8 | 1 | 0.4 | ||||
| LDL | ≥70 | 8 | 80.0 | 146 | 76.8 | 175 | 68.1 | 183 | 65.1 | 0.44 |
| TG | <135 | 8 | 72.7 | 147 | 75.8 | 202 | 78.6 | 170 | 60.1 | <0.001 |
| 135–200 | 1 | 9.1 | 34 | 17.5 | 36 | 14.0 | 74 | 26.1 | ||
| >200 | 2 | 18.2 | 13 | 6.7 | 19 | 7.4 | 39 | 13.8 | ||
| HDL | <40 | 5 | 50.0 | 76 | 40.0 | 119 | 46.1 | 178 | 62.9 | <0.001 |
| >40 | 5 | 50.0 | 114 | 60.0 | 139 | 53.9 | 105 | 37.1 | ||
| Variables | BMI | p-Value ** | |||||||
|---|---|---|---|---|---|---|---|---|---|
| <18.5 n = 12 | 18.5–24.9 n = 203 | 25.0–29.9 n = 264 | ≥30 n = 296 | ||||||
| SD | SD | SD | SD | ||||||
| Age | 73.42 | 9.95 | 69.55 | 14.40 | 70.81 | 12.10 | 67.57 | 11.64 | 0.013 |
| NT-proBNP [pg/mL] | 11,620.80 | 13,684.34 | 8447.83 | 9088.24 | 8832.30 | 11,774.43 | 4830.30 | 6711.13 | 0.047 |
| BNP [pg/mL] | 1405.63 | 1398.71 | 1410.75 | 1779.29 | 1033.11 | 1461.49 | 664.78 | 830.29 | <0.001 |
| TG [mg/dL] | 110.00 | 71.80 | 113.43 | 55.74 | 117.62 | 71.61 | 137.72 | 70.51 | <0.001 |
| LDL [mg/dL] | 90.70 | 22.58 | 96.95 | 40.09 | 89.43 | 37.27 | 86.28 | 33.75 | 0.021 |
| HDL [mg/dL] | 48.90 | 17.99 | 45.39 | 14.31 | 43.11 | 13.74 | 38.60 | 10.88 | <0.001 |
| TC [mg/dL] | 154.73 | 41.11 | 164.60 | 50.59 | 155.90 | 47.33 | 152.25 | 41.52 | 0.039 |
| CRP [mg/L] | 22.86 | 45.93 | 14.65 | 28.77 | 13.88 | 29.28 | 16.86 | 31.54 | 0.54 |
| Albumin [g/dL] | 3.07 | 0.75 | 3.26 | 0.60 | 3.35 | 0.63 | 3.42 | 0.53 | 0.43 |
| Transferrin [g/L] | 2.56 | 0.42 | 2.23 | 0.58 | 2.62 | 0.64 | 2.47 | 0.68 | 0.022 |
| Lymphocytes [%] | 26.98 | 17.84 | 20.09 | 9.91 | 19.74 | 9.81 | 21.77 | 8.80 | 0.21 |
| PCT [ng/mL] | 1.42 | 3.60 | 0.91 | 3.75 | 1.25 | 5.49 | 0.38 | 1.50 | 0.38 |
| Variables | NRS | p-Value * | ||||
|---|---|---|---|---|---|---|
| <3 (n = 1010) | ≥3 (n = 45) | |||||
| n | % | n | % | |||
| Sex | M | 677 | 67.03 | 26 | 57.78 | 0.20 |
| BMI | <18.5 | 10 | 1.35 | 2 | 6.06 | 0.009 |
| 18.5–24.9 | 189 | 25.47 | 14 | 42.42 | ||
| 25.0–29.9 | 253 | 34.10 | 11 | 33.33 | ||
| ≥30 | 290 | 39.08 | 6 | 18.18 | ||
| HF phenotype | HFpEF | 290 | 28.71 | 14 | 31.11 | 0.017 |
| HFmrEF | 126 | 12.48 | 4 | 8.89 | ||
| HFrEF | 532 | 52.67 | 19 | 42.22 | ||
| No information | 62 | 6.14 | 8 | 17.78 | ||
| NYHA | 1 | 89 | 9.35 | 3 | 8.82 | 0.004 |
| 2 | 328 | 34.45 | 4 | 11.76 | ||
| 3 | 299 | 31.41 | 10 | 29.41 | ||
| 4 | 236 | 24.79 | 17 | 50.00 | ||
| CKD | Yes | 375 | 37.13 | 20 | 44.44 | 0.32 |
| MI | Yes | 309 | 30.59 | 16 | 35.56 | 0.48 |
| Type of MI | No | 701 | 69.4 | 29 | 64.4 | 0.46 |
| STEMI | 83 | 8.2 | 6 | 13.3 | ||
| NSTEMI | 203 | 20.1 | 10 | 22.2 | ||
| No information | 23 | 2.3 | 29 | 64.4 | ||
| HT | Yes | 730 | 72.28 | 30 | 66.67 | 0.41 |
| DM | Yes | 445 | 44.06 | 10 | 22.22 | 0.004 |
| CS | Yes | 118 | 11.68 | 6 | 13.33 | 0.74 |
| LDL | <55 mg/dL | 140 | 14.52 | 10 | 27.03 | 0.16 |
| 55 to <70 mg/dL | 161 | 16.70 | 4 | 10.81 | ||
| 70 to <100 mg/dL | 348 | 36.10 | 16 | 43.24 | ||
| 100 to <116 mg/dL | 114 | 11.83 | 4 | 10.81 | ||
| 116 to <190 mg/dL | 189 | 19.61 | 3 | 8.11 | ||
| more than 190 mg/dL | 12 | 1.24 | ||||
| LDL | ≥70 | 663 | 68.78 | 23 | 62.16 | 0.39 |
| TG | <135 | 672 | 69.35 | 29 | 72.50 | 0.63 |
| 135–200 | 201 | 20.74 | 6 | 15.00 | ||
| >200 | 96 | 9.91 | 5 | 12.50 | ||
| HDL | <40 | 495 | 51.08 | 27 | 75.00 | 0.005 |
| >40 | 474 | 48.92 | 9 | 25.00 | ||
| Variables | NRS | p-Value ** | |||
|---|---|---|---|---|---|
| <3 (n = 1010) | ≥3 (n = 45) | ||||
| SD | SD | ||||
| Age | 69.36 | 12.83 | 78.02 | 12.33 | <0.001 |
| BMI [kg/m2] | 29.11 | 6.20 | 25.83 | 5.39 | 0.003 |
| Height [m] | 169.52 | 9.03 | 164.87 | 10.39 | 0.006 |
| Body weight [kg] | 83.48 | 19.45 | 70.68 | 16.65 | <0.001 |
| NT-proBNP [pg/mL] | 8012.61 | 10,979.46 | 13,293.70 | 10,443.66 | 0.29 |
| BNP [pg/mL] | 1021.53 | 1423.27 | 1612.36 | 1812.12 | 0.021 |
| TG [mg/dL] | 124.59 | 67.35 | 118.77 | 65.42 | 0.59 |
| LDL [mg/dL] | 89.86 | 36.35 | 76.95 | 31.25 | 0.033 |
| HDL [mg/dL] | 42.15 | 13.86 | 33.97 | 10.75 | <0.001 |
| TC [mg/dL] | 156.78 | 46.66 | 130.97 | 39.62 | 0.001 |
| CRP [mg/L] | 15.30 | 31.37 | 32.90 | 43.11 | <0.001 |
| Albumin [g/dL] | 3.34 | 0.58 | 3.26 | 0.55 | 0.49 |
| Transferrin [g/L] | 2.46 | 0.63 | 2.16 | 0.57 | 0.08 |
| Lymphocytes [%] | 20.74 | 9.85 | 13.61 | 9.03 | 0.001 |
| PCT [ng/mL] | 0.74 | 3.44 | 1.89 | 5.09 | 0.09 |
| Survival Time [Days] | ||
|---|---|---|
| Percentiles | 25 percentiles (lower quartile) | 26.0 |
| 50 percentiles (median) | 39.3 | |
| 75 percentiles (upper quartile) | 66.7 | |
| Descriptive Statistics | ||||||
|---|---|---|---|---|---|---|
| Me | SD | N—Death | N—Survivors | |||
| BMI | <18.5 | 12.5 | 13.8 | 10.7 | 2 | 10 |
| 18.5–24.9 | 7.0 | 8.2 | 8.7 | 9 | 194 | |
| 25.0–29.9 | 6.0 | 7.9 | 7.2 | 17 | 247 | |
| ≥30 | 6.0 | 8.7 | 9.4 | 8 | 288 | |
| NRS | <3 | 6.0 | 8.0 | 7.7 | 46 | 964 |
| ≥3 | 9.0 | 13.6 | 14.0 | 12 | 33 | |
| LDL | <55 mg/dL | 7.0 | 8.8 | 8.7 | 18 | 132 |
| 55 to <70 mg/dL | 7.0 | 7.9 | 6.5 | 7 | 158 | |
| 70 to <100 mg/dL | 6.0 | 8.6 | 9.4 | 18 | 346 | |
| 100 to <116 mg/dL | 6.0 | 7.5 | 5.8 | 3 | 115 | |
| 116 to <190 mg/dL | 6.0 | 7.6 | 7.2 | 2 | 190 | |
| more than 190 mg/dL | 4.5 | 4.8 | 2.8 | 1 | 11 | |
| p-Value | HR | 95%CI HR (Lower) | 95%CI HR (Upper) | ||
|---|---|---|---|---|---|
| Sex (n = 1056) | M | 0.283 | 0.75 | 0.45 | 1.27 |
| BMI (n = 775) | 18.5–24.9 | Ref. | |||
| <18.5 | 0.486 | 3.26 | 0.49 | 21.75 | |
| 25.0–29.9 | 0.151 | 1.60 | 0.70 | 3.66 | |
| ≥30 | 0.028 | 0.51 | 0.19 | 1.32 | |
| NRS (n = 1055) | <3 | Ref. | |||
| ≥3 | 0.014 | 2.31 | 1.19 | 4.49 | |
| HF phenotype (n = 1056) | HFpEF | Ref. | |||
| HFmrEF | 0.000 | 4.69 | 2.02 | 10.91 | |
| HFrEF | 0.376 | 0.91 | 0.33 | 2.50 | |
| No information | 0.067 | 0.84 | 0.44 | 1.61 | |
| NYHA (n = 986) | 1 | Ref. | |||
| 2 | 0.988 | 0.00 | 0.00 | ||
| 3 | 0.991 | 0.18 | 0.04 | 0.76 | |
| 4 | 0.988 | 0.37 | 0.17 | 0.82 | |
| MI (n = 1056) | Yes | 0.343 | 1.30 | 0.75 | 2.26 |
| CKD (n = 1056) | Yes | 0.321 | 0.76 | 0.44 | 1.31 |
| Type of MI (n = 1056) | No | Ref. | |||
| STEMI | 0.451 | 1.72 | 0.28 | 10.46 | |
| NSTEMI | 0.849 | 1.18 | 0.62 | 2.23 | |
| No information | 0.990 | 1.25 | 0.17 | 9.16 | |
| HT (n = 1056) | Yes | 0.506 | 0.83 | 0.48 | 1.44 |
| DM (n = 1056) | Yes | 0.714 | 1.10 | 0.65 | 1.86 |
| CS (n = 1056) | Yes | 0.249 | 1.48 | 0.76 | 2.87 |
| LDL (n = 1001) | <55 mg/dL | Ref. | |||
| 55 to <70 mg/dL | 0.826 | 0.65 | 0.11 | 3.82 | |
| 70 to <100 mg/dL | 0.413 | 0.34 | 0.06 | 2.13 | |
| 100 to <116 mg/dL | 0.386 | 0.06 | 0.01 | 0.48 | |
| 116 to <190 mg/dL | 0.009 | 0.10 | 0.02 | 0.45 | |
| more than 190 mg/dL | 0.038 | 3.20 | 0.41 | 25.22 | |
| LDL (n = 1001) | ≥70 | 0.003 | 0.42 | 0.24 | 0.75 |
| TG (n = 1009) | <135 | Ref. | |||
| 135–200 | 0.656 | 1.90 | 0.89 | 4.05 | |
| >200 | 0.130 | 2.53 | 1.16 | 5.52 | |
| HDL (n = 1005) | <40 | Ref. | |||
| >40 | 0.110 | 0.58 | 0.30 | 1.13 | |
| Variables | |||||
| Age (n = 1056) | 0.000 | 1.05 | 1.02 | 1.07 | |
| BMI [kg/m2] (n = 775) | 0.048 | 0.94 | 0.89 | 1.00 | |
| Height [m] (n = 763) | 0.435 | 0.99 | 0.95 | 1.02 | |
| Body weight [kg] (n = 761) | 0.019 | 0.98 | 0.96 | 1.00 | |
| NT-proBNP [pg/mL] (n = 228) | 0.779 | 1.00 | 1.00 | 1.00 | |
| BNP [pg/mL] (n = 775) | 0.006 | 1.00 | 1.00 | 1.00 | |
| TG [mg/dL] (n = 1009) | 0.050 | 1.00 | 1.00 | 1.01 | |
| LDL [mg/dL] (n = 1001) | 0.002 | 0.98 | 0.97 | 0.99 | |
| HDL [mg/dL] (n = 1005) | 0.001 | 0.95 | 0.93 | 0.98 | |
| TC [mg/dL] (n = 1010) | 0.000 | 0.98 | 0.98 | 0.99 | |
| CRP [mg/L] (n = 1023) | 0.000 | 1.01 | 1.01 | 1.01 | |
| Albumin [g/dL] (n = 278) | 0.000 | 0.34 | 0.19 | 0.62 | |
| Transferrin [g/L] (n = 261) | 0.126 | 0.56 | 0.27 | 1.18 | |
| Lymphocytes [%] (n = 375) | 0.000 | 0.92 | 0.88 | 0.96 | |
| PCT [ng/mL] (n = 428) | 0.003 | 1.07 | 1.02 | 1.12 | |
| Beta | Standard Error | Chi-Square | p-Value | HR | 95% CI HR (Lower) | 95%CI HR (Upper) | ||
|---|---|---|---|---|---|---|---|---|
| TC | −0.02 | 0.01 | 7.79 | 0.005 | 0.98 | 0.97 | 0.99 | |
| BMI | Underweight | 1.24 | 0.80 | 2.369 | 0.12 | 12.30 | 0.80 | 189.92 |
| Overweight | 0.04 | 0.39 | 0.009 | 0.93 | 0.87 | 0.29 | 2.65 | |
| Obesity | −1.45 | 0.50 | 8.447 | 0.004 | 0.20 | 0.05 | 0.79 | |
| TG | 135–200 | 0.65 | 0.46 | 2.007 | 0.16 | 6.15 | 1.69 | 22.40 |
| >200 | 0.52 | 0.55 | 0.899 | 0.34 | 5.42 | 1.03 | 28.36 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Czapla, M.; Juárez-Vela, R.; Łokieć, K.; Karniej, P. The Association between Nutritional Status and In-Hospital Mortality among Patients with Heart Failure—A Result of the Retrospective Nutritional Status Heart Study 2 (NSHS2). Nutrients 2021, 13, 1669. https://doi.org/10.3390/nu13051669
Czapla M, Juárez-Vela R, Łokieć K, Karniej P. The Association between Nutritional Status and In-Hospital Mortality among Patients with Heart Failure—A Result of the Retrospective Nutritional Status Heart Study 2 (NSHS2). Nutrients. 2021; 13(5):1669. https://doi.org/10.3390/nu13051669
Chicago/Turabian StyleCzapla, Michał, Raúl Juárez-Vela, Katarzyna Łokieć, and Piotr Karniej. 2021. "The Association between Nutritional Status and In-Hospital Mortality among Patients with Heart Failure—A Result of the Retrospective Nutritional Status Heart Study 2 (NSHS2)" Nutrients 13, no. 5: 1669. https://doi.org/10.3390/nu13051669
APA StyleCzapla, M., Juárez-Vela, R., Łokieć, K., & Karniej, P. (2021). The Association between Nutritional Status and In-Hospital Mortality among Patients with Heart Failure—A Result of the Retrospective Nutritional Status Heart Study 2 (NSHS2). Nutrients, 13(5), 1669. https://doi.org/10.3390/nu13051669









