Pregnant Women Living with Obesity: A Cross-Sectional Observational Study of Dietary Quality and Pregnancy Outcomes
Abstract
1. Introduction
2. Materials and Methods
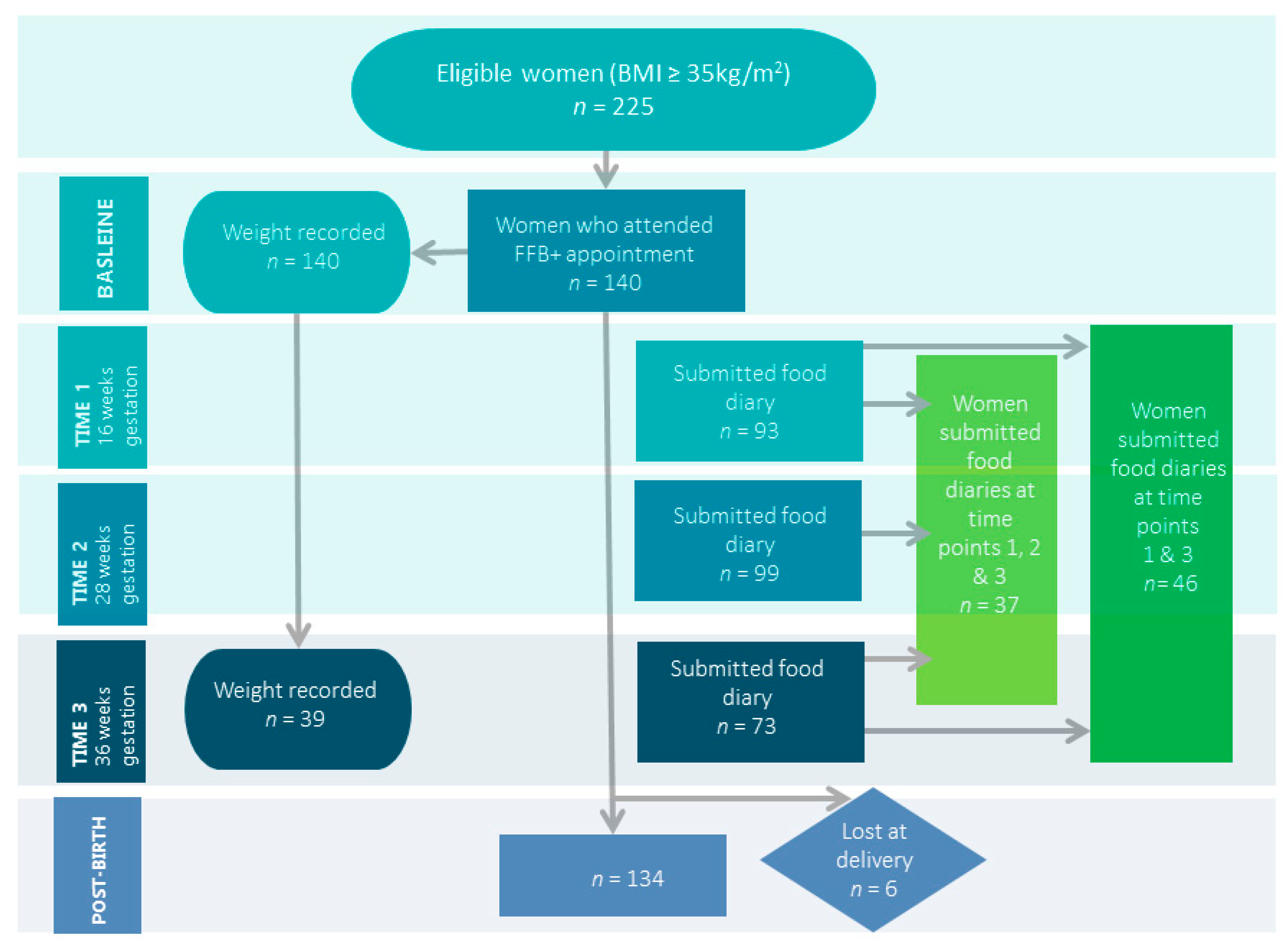
2.1. Study Design
2.2. Study Population
2.3. Dietary Measurements
2.4. Procedure
2.5. Data Analysis
3. Results
3.1. Participant Characteristics
3.2. Clinical Outcomes
3.3. Dietary Analysis
3.3.1. Macronutrients
3.3.2. Micronutrients
3.4. BMI and Dietary Composition
4. Discussion
4.1. Diet Quality
4.1.1. Macronutrients
4.1.2. Micronutrients
4.2. Clinical Outcomes
4.3. Implications for Practice
4.4. Future Research
4.5. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- NHS Digital. Statistics on Obesity, Physical Activity and Diet, England. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/england-2020 (accessed on 12 April 2021).
- Denison, F.C.; Aedla, N.R.; Keag, O.; Hor, K.; Reynolds, R.M.; Milne, A.; Diamond, A. Care of Women with Obesity in Pregnancy: Green-Top Guideline. BJOG 2018, 126. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic—Report of a WHO Consultation; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- National Institute of Health and Care Excellence. Obesity: Identification, Assessment and Management—Clinical Guideline; National Institute of Health and Care Excellence: London, UK, 2014. [Google Scholar]
- Centre of Maternal and Child Enquiries. Joint Guideline Management of Women with Obesity in Pregnancy; Centre of Maternal and Child Enquiries and Royal College of Obstetricians and Gynaecologists: London, UK, 2010. [Google Scholar]
- World Health Organization. Good Maternal Nutrition: The Best Start in Life; World Health Organisation European Regional Office: Copenhagen, Denmark, 2016. [Google Scholar]
- McCann, M.T.; Newson, L.; Burden, C.; Rooney, J.S.; Charnley, M.S.; Abayomi, J.C. A qualitative study exploring midwives’ perceptions and knowledge of maternal obesity: Reflecting on their experiences of providing healthy eating and weight management advice to pregnant women. Matern. Child Nutr. 2018, 14, e12520. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Weight Gain During Pregnancy: Re-Examing the Guidelines; Institute of Medicine: Washington, WA, USA, 2009. [Google Scholar]
- American College of Obstetricians and Gynecologists. Weight gain during pregnancy: Committee opinion no. 548. Obstet. Gynecol. 2013, 121, 210–212. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. National Diet and Nutrition Survey: Results form Years 7 & 8 (Combined) of the Rolling Programme (2014/15–2015/16); Public Health England: London, UK, 2018.
- Diemert, A.; Lezius, S.; Pagenkemper, M.; Hansen, G.; Drozdowska, A.; Hecher, K.; Arck, P.; Zyriax, B.C. Maternal nutrition, inadequate gestational weight gain and birth weight: Results from a prospective birth cohort. BMC Pregnancy Childbirth 2016, 16. [Google Scholar] [CrossRef] [PubMed]
- Scientific Advisory Committee on Nutrition. Update on Folic Acid; Scientific Advisory Committee on Nutrition: London, UK, 2017.
- National Institute of Health and Care Excellence. Surveillance Report—Vitamin D: Increasing Supplement Use in At-Risk Groups (2014) NICE Guideline PH56; National Institute for Health and Care Excellence: London, UK, 2017. [Google Scholar]
- Berry, R.J.; Bailey, L.; Mulinare, J.; Bower, C.; Dary, O. Fortification of Flour with Folic Acid. Food Nutr. Bull. 2010, 31, S22–S35. [Google Scholar] [CrossRef] [PubMed]
- Scientific Advisory Committee on Nutrition. Position Statement on Iodine and Health; Public Health England: London, UK, 2014.
- Mousa, A.; Naqash, A.; Lim, S. Macronutrient and Micronutrient Intake during Pregnancy: An Overview of Recent Evidence. Nutrients 2019, 11, 443. [Google Scholar] [CrossRef] [PubMed]
- Blumfield, M.; Hure, A.; MacDonald-Wicks, L.; Smith, R.; Simpson, S.; Raubenheimer, D.; Collins, C. The Association between the Macronutrient Content of Maternal Diet and the Adequacy of Micronutrients during Pregnancy in the Women and Their Children’s Health (WATCH) Study. Nutrients 2012, 4, 1958–1976. [Google Scholar] [CrossRef]
- Moran, L.; Sui, Z.; Cramp, C.; Dodd, J. A decrease in diet quality occurs during pregnancy in overweight and obese women which is maintained post-partum. Int. J. Obes. 2013, 37, 704–711. [Google Scholar] [CrossRef]
- Rifas-Shiman, S.L.; Rich-Edwards, J.W.; Kleinman, K.P.; Oken, E.; Gillman, M.W. Dietary Quality during Pregnancy Varies by Maternal Characteristics in Project Viva: A US Cohort. J. Am. Diet. Assoc. 2009, 109, 1004–1011. [Google Scholar] [CrossRef]
- Bruno, R.; Petrella, E.; Bertarini, V.; Pedrielli, G.; Neri, I.; Facchinetti, F. Adherence to a lifestyle programme in overweight/obese pregnant women and effect on gestational diabetes mellitus: A randomized controlled trial. Matern. Child Nutr. 2017, 13. [Google Scholar] [CrossRef]
- Flynn, A.C.; Dalrymple, K.; Barr, S.; Poston, L.; Goff, L.M.; Rogozinska, E.; van Poppel, M.N.; Rayanagoudar, G.; Yeo, S.; Carballo, R.B.; et al. Dietary interventions in overweight and obese pregnant women: A systematic review of the content, delivery, and outcomes of randomized controlled trials. Nutr. Rev. 2016, 74, 312–328. [Google Scholar] [CrossRef] [PubMed]
- Harrison, C.L.; Lombard, C.B.; Strauss, B.J.; Teede, H.J. Optimizing healthy gestational weight gain in women at high risk of gestational diabetes: A randomized controlled trial. Obesity 2013, 21, 904–909. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, M.; Hosker, M.; Marcus, B.H.; Rosal, M.C.; Braun, B.; Stanek, E.J.; Markenson, G.; Chasan-Taber, L. A pregnancy lifestyle intervention to prevent gestational diabetes risk factors in overweight Hispanic women: A feasibility randomized controlled trial. Diabet. Med. 2015, 32, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Birdsall, K.M.; Vyas, S.; Khazaezadeh, N.; Oteng-Ntim, E. Maternal obesity: A review of interventions. Int. J. Clin. Pract. 2009, 63, 494–507. [Google Scholar] [CrossRef] [PubMed]
- Bogaerts, A.F.; Devlieger, R.; Nuyts, E.; Witters, I.; Gyselaers, W.; Van den Bergh, B.R. Effects of lifestyle intervention in obese pregnant women on gestational weight gain and mental health: A randomized controlled trial. Int. J. Obes. 2013, 37, 814–821. [Google Scholar] [CrossRef]
- Boyle, J.; Thangaratinam, S.; Goldstein, R.; Teede, H. Excess Gestational Weight Gain in Pregnancy and the Role of Lifestyle Intervention. Semin. Reprod. Med. 2016, 34, e14–e21. [Google Scholar] [CrossRef][Green Version]
- STROBE. Strobe Statement: Strengthening the Reporting of Obsevational Studies in Epidemiology. Available online: https://www.strobe-statement.org/index.php?id=available-checklists (accessed on 25 March 2021).
- Narayanan, R.P.; Weeks, A.D.; Quenby, S.; Rycroft, D.; Hart, A.; Longworth, H.; Charnley, M.; Abayomi, J.; Topping, J.; Turner, M.A.; et al. Fit for Birth—The effect of weight changes in obese pregnant women on maternal and neonatal outcomes: A pilot prospective cohort study. Clin. Obes. 2016, 6, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Dijkhuizen, M.A.; Greffeille, V.; Roos, N.; Berger, J.; Wieringa, F.T. Interventions to Improve Micronutrient Status of Women of Reproductive Age in Southeast Asia: A Narrative Review on What Works, What Might Work, and What Doesn’t Work. Matern. Child Health J. 2019, 23, 18–28. [Google Scholar] [CrossRef]
- Stephen, A.M. The Case for Diet Diaries in Longitudinal Studies. Int. J. Soc. Res. Methodol. 2007, 10, 365–377. [Google Scholar] [CrossRef]
- Nelson, M.; Atkinson, M.; Meyer, J. A Photographic Atlas of Food Portion Sizes; Food Standards Agency: London, UK, 2002.
- Food Standards Agency. Food Portion Sizes (MAFF Handbook), 3rd ed.; TSO: London, UK, 2002.
- Downlee Systems Ltd. Microdiet, Chapel le Firth; [Licenced Computer Software]; Downlee Systems Ltd.: High Peak, UK, 1 January 2005. [Google Scholar]
- McCance, R.A.; Widdowson, E.M. McCance and Widdowson’s the Composition of Foods, 6th ed.; Royal Society of Chemistry: Cambridge, UK, 2002. [Google Scholar]
- Esfahani, A.; Wong, J.M.; Mirrahimi, A.; Villa, C.R.; Kendall, C.W. The application of the glycemic index and glycemic load in weight loss: A review of the clinical evidence. IUBMB Life 2011, 63, 7–13. [Google Scholar] [CrossRef]
- Hollis, B.W.; Wagner, C.L. Nutritional vitamin D status during pregnancy: Reasons for concern. CMAJ 2006, 174, 1287–1290. [Google Scholar] [CrossRef] [PubMed]
- Jans, G.; Matthys, C.; Bogaerts, A.; Lannoo, M.; Verhaeghe, J.; Van Der Schueren, B.; Devlieger, R. Maternal Micronutrient Deficiencies and Related Adverse Neonatal Outcomes after Bariatric Surgery: A Systematic Review. Adv. Nutr. 2015, 6, 420–429. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.L.; Cederberg, H.M.S.; Wheeler, S.J.; Poston, L.; Hutchinson, C.J.; Seed, P.T.; Oliver, R.L.; Baker, P.N.; Jones, R.; Wheeler, S.; et al. Relationship between maternal growth, infant birthweight and nutrient partitioning in teenage pregnancies. BJOG Int. J. Obstet. Gynaecol. 2010, 117, 200–211. [Google Scholar] [CrossRef] [PubMed]
- Mairead, K.E.; Zhang, J.Y.; Kinsella, M.; Khasban, A.S.; Kenny, L.C. Vitamin D status is associated with uteroplacental dysfunction indicated by pre-eclampsia and small-for-gestational-age birth in a large prospective pregnancy cohort in Ireland with low vitamin D status. Am. J. Clin. Nutr. 2016, 104, 354–361. [Google Scholar]
- Williamson, C.S. Nutrition in pregnancy. Nutr. Bull. 2006, 31, 28–59. [Google Scholar] [CrossRef]
- Committee on Aspects of Medicine and Food Policy. Dietary Reference Values for Food and Nutrients for the United Kingdom No. 15; Department of Health: London, UK, 1991.
- National Institute of Health and Care Excellence. Maternal and Child Nutrition: Public Health Guidance; National Institute of Health and Care Excellence: London, UK, 2008. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 23.0; [Licenced Computer Software]; IBM Corp.: Armonk, NY, USA, 2015. [Google Scholar]
- Scientific Advisory Committee on Nutrition. Dietary Reference Values for Energy; Scientific Advisory Committee on Nutrition: London, UK, 2011.
- Cassidy, L.; Mulhern, M.; Alhomaid, R.; Livingstone, M.; Abayomi, J.; McCann, M. Maternal obesity and gestational weight gain: Associations with maternal and infant outcomes. Proc. Nutr. Soc. 2018, 77. [Google Scholar] [CrossRef]
- Velasco, I.; Bath, S.; Rayman, M.P. Iodine as Essential Nutrient during the First 1000 Days of Life. Nutrients 2018, 10, 290. [Google Scholar] [CrossRef]
- Young, M.F.; Oaks, B.; Tandon, S.; Martorell, R.; Dewey, K.; Wendt, A. Maternal Hemoglobin Concentrations Across Pregnancy and Maternal and Child Health: A Systematic Review and Meta-analysis (P11-033-19). Curr. Dev. Nutr. 2019, 3. [Google Scholar] [CrossRef]
- O’Dwyer, V.; O’Toole, F.; Darcy, S.; Farah, N.; Kennelly, M.M.; Turner, M.J. Maternal obesity and gestational weight gain. J. Obstet. Gynaecol. 2013, 33, 671–674. [Google Scholar] [CrossRef]
- Scientific Advisory Committee on Nutrition. Carbohydrates and Health Report 2015. Available online: https://www.gov.uk/government/publications/sacn-carbohydrates-and-health-report (accessed on 24 April 2021).
- Scientific Advisory Committee on Nutrition. Saturated Fates and Health Report 2019. Available online: https://www.gov.uk/government/publications/saturated-fats-and-health-sacn-report (accessed on 24 April 2021).
- National Institute of Health and Care Excellence. NICE Guideline 62—Antenatal Care for Uncomplicated Pregnancies 2008. Available online: https://www.nice.org.uk/guidance/cg62 (accessed on 24 March 2021).
- Henderson, L.; Gregory, J.; Swan, G. The National Diet and Nutrition Survey: Adults aged 19 to 64 years. Vitam Miner. Intake Urin. Anal. 2003, 3, 1–8. [Google Scholar]
- Gaillard, R. Maternal obesity during pregnancy and cardiovascular development and disease in the offspring. Eur. J. Epidemiol. 2015, 30, 1141–1152. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Bartell, T.R.; Wang, X. Preconception and Prenatal Factors and Metabolic Risk. In Handbook of Life Course Health Development; Springer: Cham, Switzerland, 2018. [Google Scholar]
- NHS Digital. Rise in Proportion of Induced Labours, New Maternity Figures Show. Available online: https://digital.nhs.uk/news-and-events/latest-news/nhs-maternity-statistics-2017-18 (accessed on 22 March 2021).
- NHS Digital. Maternity Services Monthly Statistics November 2020, Experimental Statistics. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/maternity-services-monthly-statistics/november-2020/births (accessed on 22 March 2021).
- National Institute of Health and Care Excellence. Diabetes in Pregnancy: Management from Preconception to the Postnatal Period; National Institute of Health and Care Excellence: London, UK, 2015. [Google Scholar]
- World Health Organization. Malnutrition 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 24 March 2021).
- Elia, M. The Cost of Malnutrition in England and Potential Cost Savings from Nutritional Interventions (Short Version); Malnutrition Action Group of BAPEN and the National Institute for Health Research Southampton Biomedical Research Centre: Southampton, UK, 2015. [Google Scholar]
- Abayomi, J.C.; Charnley, M.S.; Cassidy, L.; McCann, M.T.; Jones, J.; Wright, M.; Newson, L.M. A patient and public involvement investigation into healthy eating and weight management advice during pregnancy. Int. J. Qual. Health Care 2020, 32, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Hrolfsdottir, L.; Schalkwijk, C.G.; Birgisdottir, B.E.; Gunnarsdottir, I.; Maslova, E.; Granstrom, C.; Strom, M.; Olsen, S.F.; Halldorsson, T.I. Maternal diet, gestational weight gain, and inflammatory markers during pregnancy. Obesity 2016, 24, 2133–2139. [Google Scholar] [CrossRef] [PubMed]
- Anant, S.; Summerfield, M.; Zhou, Y.; Zhou, T.; Wu, C.; Alpini, G.; Zhang, K.K.; Xie, L. A long-term maternal diet transition from high-fat diet to normal fat diet during pre-pregnancy avoids adipose tissue inflammation in next generation. PLoS ONE 2018, 13. [Google Scholar] [CrossRef]
- Charnley, M.; Abayomi, J. Micronutrients and the use of vitamin and mineral supplements during pregnancy and lactation. Br. J. Midwifery 2016, 24, 405–414. [Google Scholar] [CrossRef]
- Poli, V.F.S.; Sanches, R.B.; Moraes, A.D.S.; Fidalgo, J.P.N.; Nascimento, M.A.; Bresciani, P.; Andrade-Silva, S.G.; Cipullo, M.A.T.; Clemente, J.C.; Caranti, D.A. The excessive caloric intake and micronutrient deficiencies related to obesity after a long-term interdisciplinary therapy. Nutrition 2017, 38, 113–119. [Google Scholar] [CrossRef]
- Hazart, J.; Le Guennec, D.; Accoceberry, M.; Lemery, D.; Mulliez, A.; Farigon, N.; Lahaye, C.; Miolanne-Debouit, M.; Boirie, Y. Maternal Nutritional Deficiencies and Small-for-Gestational-Age Neonates at Birth of Women Who Have Undergone Bariatric Surgery. J. Pregnancy 2017. [Google Scholar] [CrossRef]
- Williamson, C.; Wyness, L. Nutritional requirements in pregnancy and use of dietary supplements. Community Pract. 2013, 86, 44. [Google Scholar]
- National Institute of Health and Care Excellence. NICE Guideline 27—Weight Management Before, During and After Pregnancy; National Institute of Health and Care Excellence: London, UK, 2010. [Google Scholar]
| Body Mass Index * n = 140 | |||||
|---|---|---|---|---|---|
| 35–39.9 n = 80 (57%) | 40–44.9 n = 37 (26%) | 45–49.9 n = 15 (11%) | 50+ n = 8 (6%) | All BMI (100%) | |
| Age (n = 140) | |||||
| 18–24 25–29 30–39 40+ | 15 (11) 32 (23) 27 (19) 6 (4) | 4 (3) 13 (9) 16 (11) 4 (3) | 4 (3) 6 (4) 4 (3) 1 (1) | 1 (1) 4 (3) 3 (2) 0 | 24 (17) 55 (39) 50 (36) 11 (8) |
| Parity (n = 140) | |||||
| Primip (1st pregnancy) Multip (2nd + pregnancy) § Missing | 32 (23) 47 (34) 1 (1) | 10 (7) 27 (19) 0 | 6 (4) 8 (6) 1 (1) | 5 (4) 3 (2) 0 | 53 (38) 85 (61) 2 (2) |
| Smoking status (n = 140) | |||||
| Given up Non-smoker Smoker Missing | 9 (7) 62 (44) 8 (6) 1 (1) | 7 (5) 24 (17) 6 (4) 0 | 0 10 (7) 4 (3) 1 (1) | 1 (1) 7 (5) 0 0 | 17 (12) 103 (74) 18 (13) 2 (1) |
| Body Mass Index | |||||
|---|---|---|---|---|---|
| 35–39.9 | 40–44.9 | 45–49.9 | 50+ | All BMI | |
| n = 80 (57%) | n = 37 (26%) | n = 15 (11%) | n = 8 (6%) | −100% | |
| Weight gain at 36 weeks (n = 39) | |||||
| Less than 0 | 2 (5) | 4 (10) | 1 (3) | 0 | 7 (18) |
| 0–4.9 kg | 9 (23) | 4 (10) | 1 (3) | 0 | 14 (36) |
| 5–9 kg | 7 (18) | 2 (5) | 0 | 0 | 9 (23) |
| 9 kg+ | 7 (18) | 1 (3) | 1 (3) | 0 | 9 (23) |
| Birth weight kg (n = 134) | |||||
| 0.1–2.49 | 6 (3) | 1 (1) | 1 (1) | 1 (1) | 9 (7) |
| 2.5–4.49 | 67 (50) | 33 (25) | 12 (9) | 6 (4) | 118 (88) |
| 4.5–6.00 | 3 (2) | 2 (2) | 1 (1) | 1 (1) | 7 (5) |
| Hypertension (n = 134) | |||||
| Yes | 7 (5) | 1 (1) | 2 (2) | 2 (2) | 12 (9) |
| No | 69 (52) | 35 (26) | 12 (9) | 6 (5) | 122 (91) |
| Pre-eclampsia (n = 134) | |||||
| Yes | 10 (8) | 3 (2) | 3 (2) | 0 | 16 (12) |
| No | 66 (49) | 33 (25) | 11 (8) | 8 (6) | 118 (88) |
| Gestational Diabetes 28 weeks (n = 134) | |||||
| Yes | 6 (5) | 4 (3) | 1 (1) | 0 | 11 (8) |
| No | 70 (52) | 32 (24) | 13 (10) | 8 (6) | 123 (92) |
| Birth outcome (n = 134) | |||||
| Live birth | 75 (56) | 36 (27) | 14 (11) | 8 (6) | 133 (99) |
| Stillborn | 1 (0.8) | 0 | 0 | 0 | 1 (1) |
| Induction of labour (n = 134) | |||||
| No | 52 (39) | 24 (18) | 8 (6) | 5 (4) | 89 (66) |
| Yes | 24 (18) | 12 (9) | 6 (5) | 3 (2) | 45 (34) |
| Mode of delivery (n = 134) | |||||
| Spontaneous | 39 (30) | 16 (12) | 7 (5) | 3 (2) | 65 (48) |
| Instrumental | 6 (5) | 2 (2) | 2 (2) | 0 | 10 (7) |
| Elective caesarean | 13 (10) | 8 (6) | 2 (2) | 2 (2) | 25 (19) |
| Emergency caesarean (EmC) | 14 (11) | 8 (6) | 3 (2) | 2 (2) | 27 (20) |
| EmC with failure to progress | 4 (3) | 2 (2) | 0 | 2 (2) | 8 (6) |
| Admitted to Special Care Baby Unit (n = 133) | |||||
| No | 67 (50) | 34 (26) | 13 (10) | 7 (5) | 121 (91) |
| Yes | 8 (6) | 2 (2) | 1 (1) | 1 (1) | 12 (9) |
| APGAR score 1 min (n = 133) | |||||
| Critically low 0–3 | 3 (2) | 3 (2) | 1 (1) | 0 | 7 (5) |
| Low 4–6 | 11 (8) | 4 (3) | 4 (3) | 3 (2) | 22 (17) |
| Normal 7–10 | 61 (46) | 29 (22) | 9 (7) | 5 (4) | 104 (78) |
| APGAR score 5 min (n = 133) | |||||
| Low 4–6 | 2 (2) | 3 (2) | 0 | 0 | 5 (4) |
| Normal 7–10 | 73 (55) | 33 (25) | 14 (10) | 8 (6) | 128 (96) |
| Dietary Reference Values (DRV) | Time 1 (16–20 Weeks) (n = 93) | Time 2 (28 Weeks) (n = 99) | Time 3 (36 Weeks) (n = 73) | Changed over Time (n = 37) | |
|---|---|---|---|---|---|
| Macronutrient | EAR for energy | Mean ± SD % (EI) | Mean ± SD % (EI) | Mean ± SD % (EI) | |
| Total Energy (kcals) | 1945 kcal T1 and T2 2145 kcals T3 | 1849 ± 591 95% | 1984 ± 526 102% | 2066 ± 587 93% | p > 0.05 |
| Protein %E | 15% of EI | 15.8 ± 3.0 106% | 16.2 ± 4.4 108% 1 | 14.8 ± 4.4 98.4% | p = 0.031 |
| Total Fat %E | 35% of EI | 33.4 ± 6.8 95% 2 | 34.8 ± 6.2 99% | 35.7 ± 6.2 102% | p > 0.05 |
| SFA %E | 11% of EI | 12.0 ± 3.3 109% | 12.9 ± 3.2 117% 1 | 13.3 ± 3.2 121% 1 | p = 0.0015 |
| MUFA %E | 13% of EI | 10.7 ± 3.1 82% 2 | 11.3 ± 2.9 87% 2 | 11.5 ± 2.6 88% 2 | p > 0.05 |
| PUFA %E | 6.5% of EI | 5.6 ± 2.4 86% 2 | 5.65 ± 2.1 87% 2 | 5.8 ± 2.1 89% 2 | p > 0.05 |
| P:S Ratio | 0.8:1 | 0.51 ± 0.26 64% 2 | 0.47 ± 0.23 59% EAR 2 | 0.46 ± 0.21 58% 2 | p > 0.05 |
| CHO %E | 50% of EI | 50.7 ± 7.5 101% | 48.9 ± 6.6 98% EAR | 47.3 ± 6.8 95% 2 | p > 0.05 |
| NSP * g/day | 18g/day | 12.8 ± 5.2 71% 2 | 12.8 ± 4.1 71% EAR 2 | 12.8 ± 4.1 71% 2 | p > 0.05 |
| Sugars %E | 5% of EAR | 23.5 214% 1 | 24.9 226% EAR1 | 22.5 205% 1 | p > 0.05 |
| Starch %E | 39% of EAR | 26 67% 2 | 27 69% 2 | 28 72% 2 | p > 0.05 |
| Micronutrient and (UK Recommended Intake) | DRV | Ranges | Time 1 % Achieved | Time 2 % Achieved | Time 3 % Achieved |
|---|---|---|---|---|---|
| Iron (14.8 mg) | <LRNI LRNI ≥ RNI | <7.99 8.0–14.7 ≥14.8 | 31.2 54.8 2 14.0 | 23.2 66.7 2 10.1 | 17.8 63.0 2 19.2 |
| Calcium (700 mg) | <LRNI LRNI RNI | <399.9 400–699.9 ≥700 | 5.4 28.0 1 66.7 | 2.0 23.2 1 74.7 | 5.5 15.1 1 79.5 |
| Iodine (140 μg) | <LRNI LRNI RNI | <69.9 70–139.9 ≥140 | 18.3 50.5 2 31.2 | 13.1 51.5 1 35.4 | 8.2 35.6 56.2 |
| Vitamin D (10 μg) * | <RNI RNI | <9.99 ≥10 | 96.8 2 3.2 | 98.0 2 2.0 | 98.6 2 1.4 |
| Folate (300 μg) | <LRNI LRNI RNI | <99.9 100–299.9 ≥300 | 1.1 66.7 2 32.3 | 0 73.7 2 26.3 | 0 65.8 34.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Charnley, M.; Newson, L.; Weeks, A.; Abayomi, J. Pregnant Women Living with Obesity: A Cross-Sectional Observational Study of Dietary Quality and Pregnancy Outcomes. Nutrients 2021, 13, 1652. https://doi.org/10.3390/nu13051652
Charnley M, Newson L, Weeks A, Abayomi J. Pregnant Women Living with Obesity: A Cross-Sectional Observational Study of Dietary Quality and Pregnancy Outcomes. Nutrients. 2021; 13(5):1652. https://doi.org/10.3390/nu13051652
Chicago/Turabian StyleCharnley, Margaret, Lisa Newson, Andrew Weeks, and Julie Abayomi. 2021. "Pregnant Women Living with Obesity: A Cross-Sectional Observational Study of Dietary Quality and Pregnancy Outcomes" Nutrients 13, no. 5: 1652. https://doi.org/10.3390/nu13051652
APA StyleCharnley, M., Newson, L., Weeks, A., & Abayomi, J. (2021). Pregnant Women Living with Obesity: A Cross-Sectional Observational Study of Dietary Quality and Pregnancy Outcomes. Nutrients, 13(5), 1652. https://doi.org/10.3390/nu13051652






