Probiotic and Oxytocin Combination Therapy in Patients with Autism Spectrum Disorder: A Randomized, Double-Blinded, Placebo-Controlled Pilot Trial
Abstract
1. Introduction
2. Materials and Methods
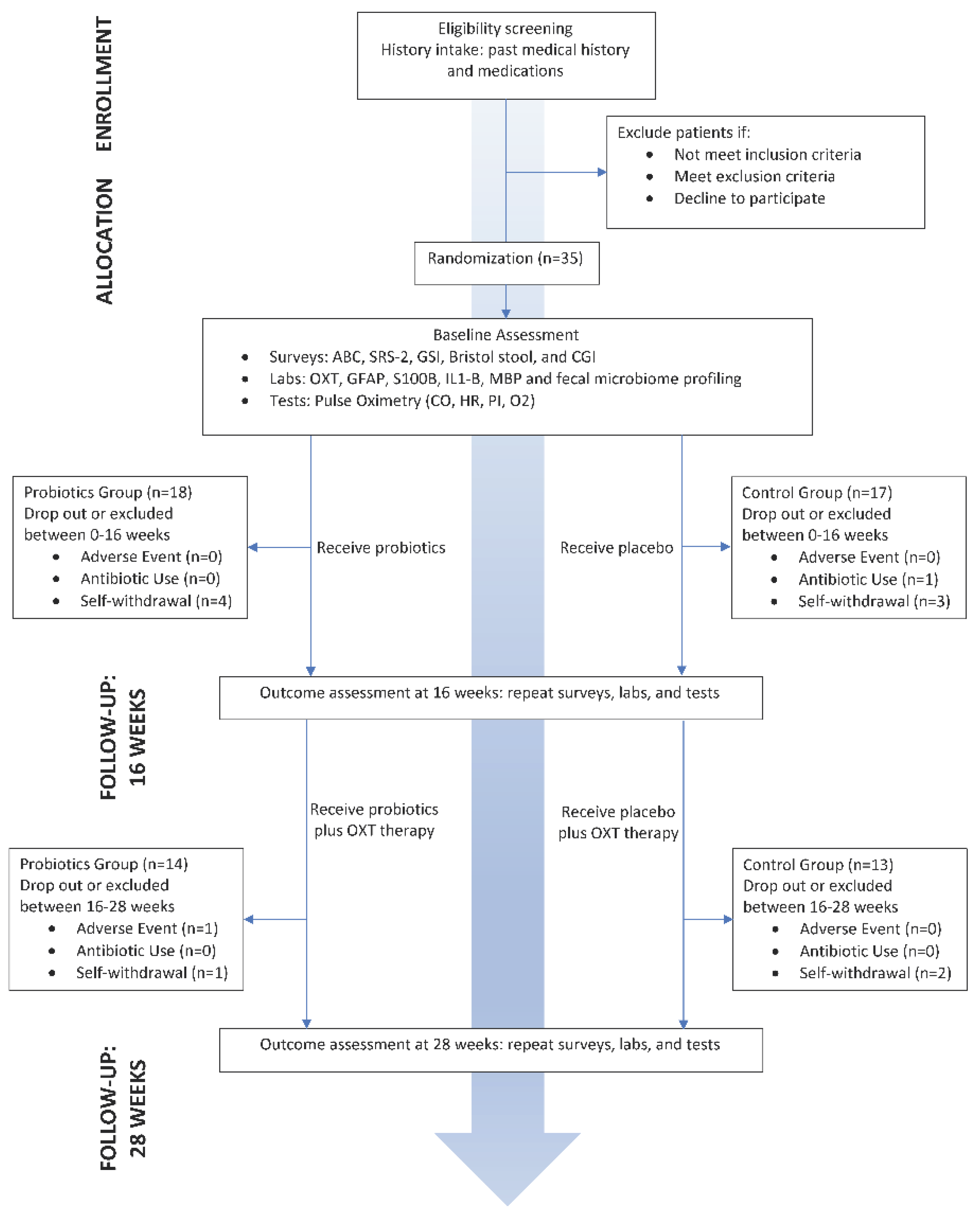
2.1. Trial Design
2.2. Participants
2.3. Randomization and Blinding
2.4. Interventions
2.5. Outcomes
2.5.1. Primary Outcome Measures
2.5.2. Secondary Outcome Measures
- Blood sample collection and circulating biomarker analysis
- GI symptom severity assessments
- Clinical Global Impression (CGI)
2.6. Stool Sample Processing
2.7. Statistical Analysis
3. Results
3.1. Demographics
3.2. Socio-Behavioral Parameters and Other Clinical Indices
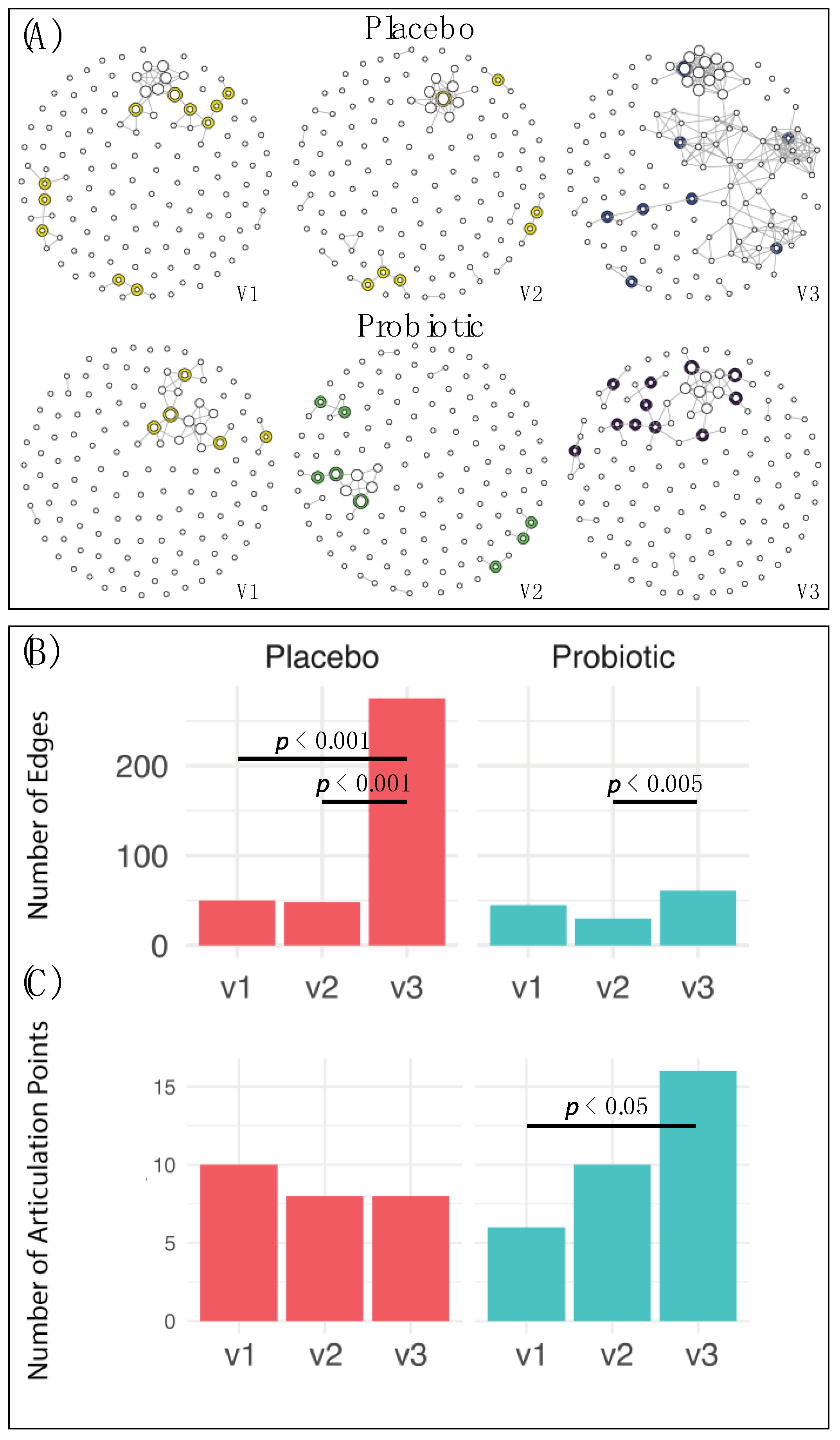
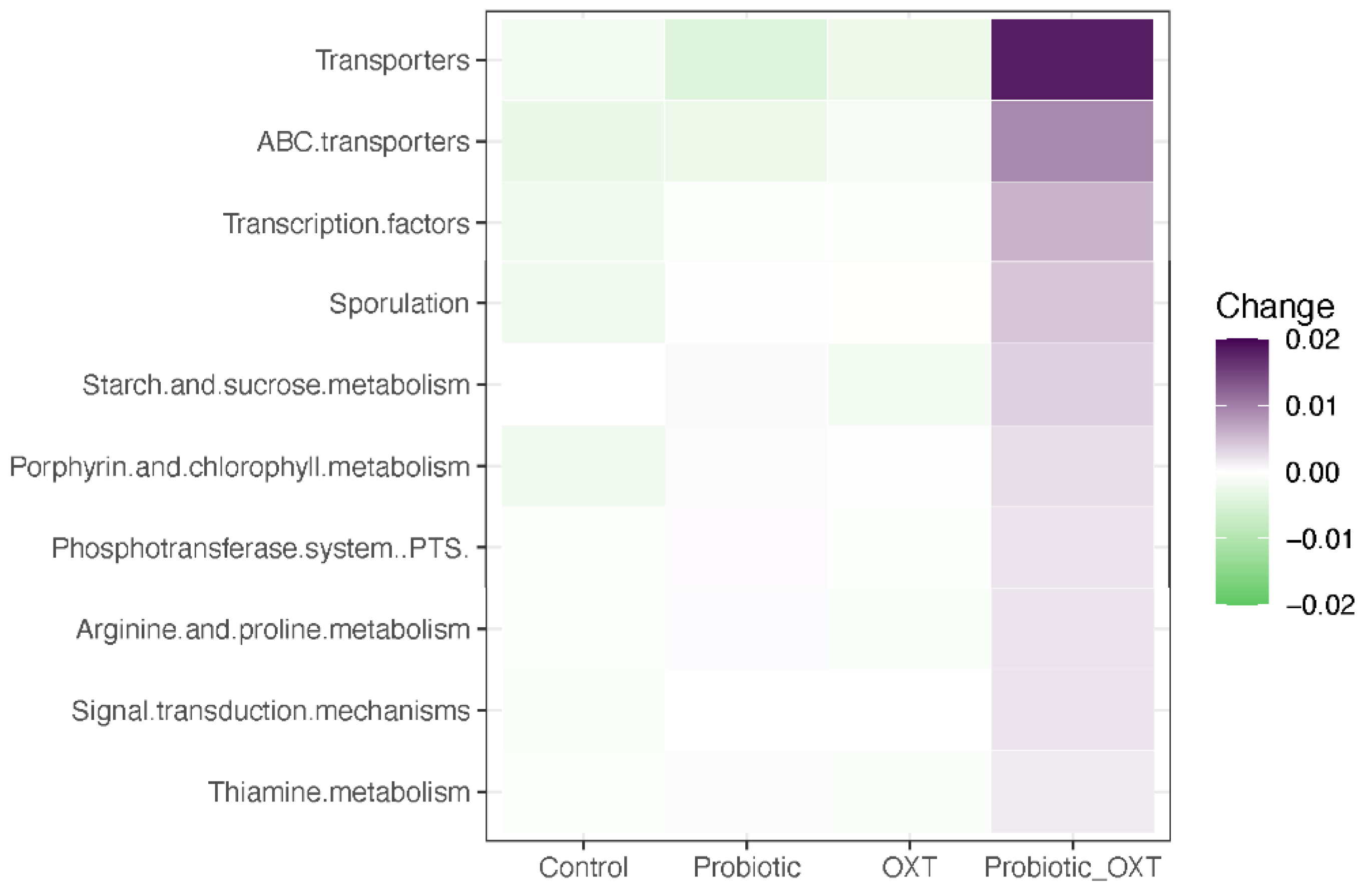
3.3. Gut Microbiome
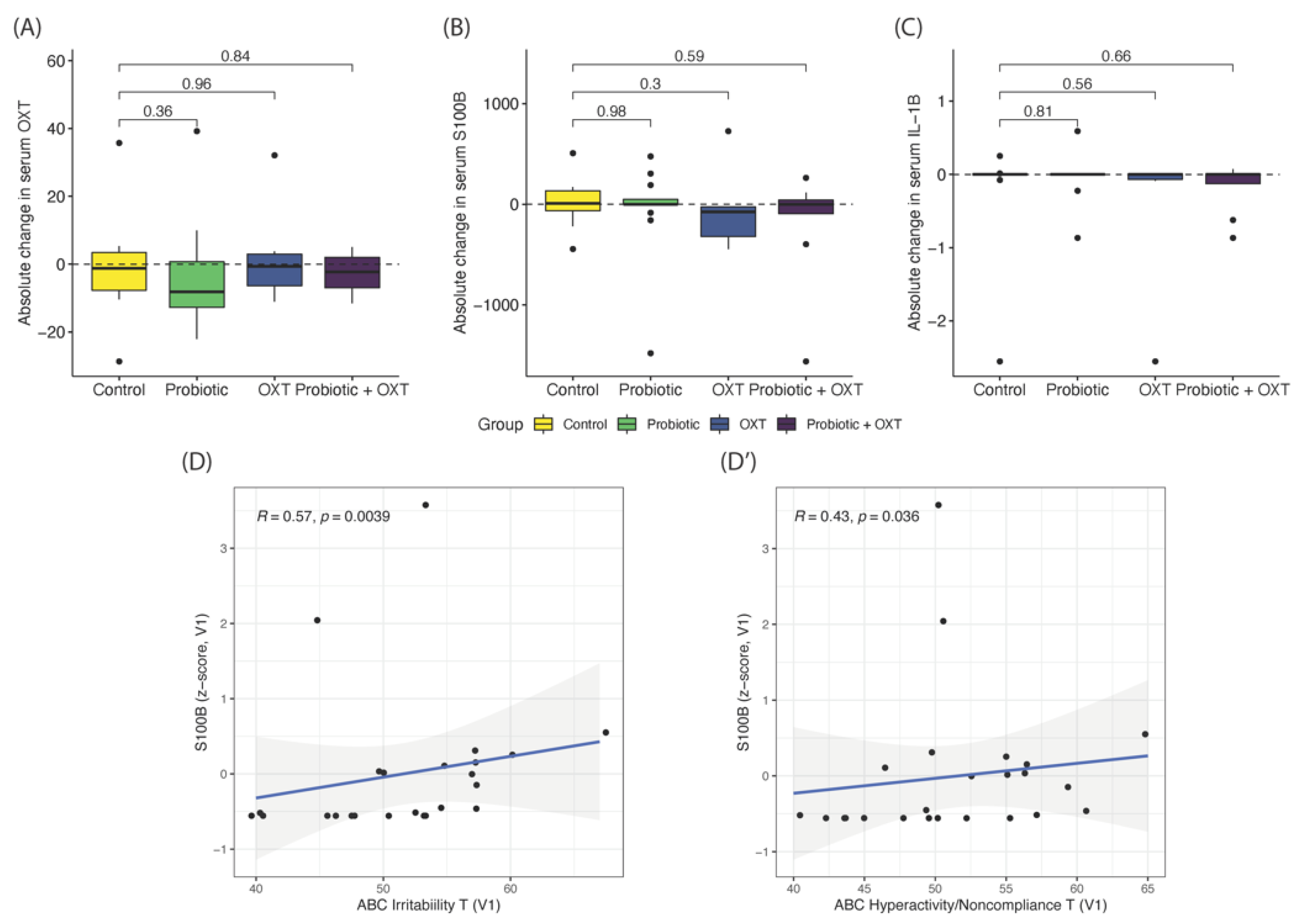
3.4. Blood Serum Markers
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maenner, M.J.; Shaw, K.A.; Baio, J.; Washington, A.; Patrick, M.; DiRienzo, M.; Christensen, D.L.; Wiggins, L.D.; Pettygrove, S.; Andrews, J.G.; et al. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2016. MMWR Surveill. Summ. 2020, 69, 1–12. [Google Scholar] [CrossRef]
- Alam, R.; Abdolmaleky, H.M.; Zhou, J.-R. Microbiome, inflammation, epigenetic alterations, and mental diseases. Am. J. Med Genet. Part B: Neuropsychiatr. Genet. 2017, 174, 651–660. [Google Scholar] [CrossRef]
- Fung, T.C.; A Olson, C.; Hsiao, T.C.F.C.A.O.E.Y. Interactions between the microbiota, immune and nervous systems in health and disease. Nat. Neurosci. 2017, 20, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.; Liu, J.; Cetinbas, M.; Sadreyev, R.; Koh, M.; Huang, H.; Adeseye, A.; He, P.; Zhu, J.; Russell, H.; et al. New and Preliminary Evidence on Altered Oral and Gut Microbiota in Individuals with Autism Spectrum Disorder (ASD): Implications for ASD Diagnosis and Subtyping Based on Microbial Biomarkers. Nutr. 2019, 11, 2128. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.-W.; Liong, M.T.; Chung, Y.-C.E.; Huang, H.-Y.; Peng, W.-S.; Cheng, Y.-F.; Lin, Y.-S.; Wu, Y.-Y.; Tsai, Y.-C. Effects of Lactobacillus plantarum PS128 on Children with Autism Spectrum Disorder in Taiwan: A Randomized, Double-Blind, Placebo-Controlled Trial. Nutr. 2019, 11, 820. [Google Scholar] [CrossRef]
- Kong, X.-J.; Liu, J.; Li, J.; Kwong, K.; Koh, M.; Sukijthamapan, P.; Guo, J.J.; Sun, Z.J.; Song, Y. Probiotics and oxytocin nasal spray as neuro-social-behavioral interventions for patients with autism spectrum disorders: A pilot randomized controlled trial protocol. Pilot Feasibility Stud. 2020, 6, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Dinan, T.G.; Stanton, C.; Cryan, J.F. Psychobiotics: A Novel Class of Psychotropic. Biol. Psychiatry 2013, 74, 720–726. [Google Scholar] [CrossRef]
- Desbonnet, L.; Garrett, L.; Clarke, G.; Bienenstock, J.; Dinan, T.G. The probiotic Bifidobacteria infantis: An assessment of potential antidepressant properties in the rat. J. Psychiatr. Res. 2008, 43, 164–174. [Google Scholar] [CrossRef]
- Savignac, H.M.; Kiely, B.; Dinan, T.G.; Cryan, J.F. Bifidobacteriaexert strain-specific effects on stress-related behavior and physiology in BALB/c mice. Neurogastroenterol. Motil. 2014, 26, 1615–1627. [Google Scholar] [CrossRef]
- Davari, S.; Talaei, S.A.; Alaei, H.; Salami, M. Probiotics treatment improves diabetes-induced impairment of synaptic activity and cognitive function: Behavioral and electrophysiological proofs for microbiome–gut-brain axis. Neuroscience 2013, 240, 287–296. [Google Scholar] [CrossRef]
- Hsiao, E.Y.; McBride, S.W.; Hsien, S.; Sharon, G.; Hyde, E.R.; McCue, T.; Codelli, J.A.; Chow, J.; Reisman, S.E.; Petrosino, J.F.; et al. Microbiota Modulate Behavioral and Physiological Abnormalities Associated with Neurodevelopmental Disorders. Cell 2013, 155, 1451–1463. [Google Scholar] [CrossRef]
- Liu, Y.-W.; Liu, W.-H.; Wu, C.-C.; Juan, Y.-C.; Wu, Y.-C.; Tsai, H.-P.; Wang, S.; Tsai, Y.-C. Psychotropic effects of Lactobacillus plantarum PS128 in early life-stressed and naïve adult mice. Brain Res. 2016, 1631, 1–12. [Google Scholar] [CrossRef]
- Liu, W.-H.; Chuang, H.-L.; Huang, Y.-T.; Wu, C.-C.; Chou, G.-T.; Wang, S.; Tsai, Y.-C. Alteration of behavior and monoamine levels attributable to Lactobacillus plantarum PS128 in germ-free mice. Behav. Brain Res. 2016, 298, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Erdman, S.; Poutahidis, T. Microbes and Oxytocin. International Review of Neurobiology 2016, 131, 91–126. [Google Scholar] [CrossRef] [PubMed]
- Pobbe, R.L.; Pearson, B.L.; Defensor, E.B.; Bolivar, V.J.; Young, W.S.; Lee, H.-J.; Blanchard, D.C.; Blanchard, R.J. Oxytocin receptor knockout mice display deficits in the expression of autism-related behaviors. Horm. Behav. 2012, 61, 436–444. [Google Scholar] [CrossRef]
- Teng, B.L.; Nikolova, V.D.; Riddick, N.V.; Agster, K.L.; Crowley, J.J.; Baker, L.K.; Koller, B.H.; Pedersen, C.A.; Jarstfer, M.B.; Moy, S.S. Reversal of social deficits by subchronic oxytocin in two autism mouse models. Neuropharmacol. 2016, 105, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Chao, S.-H.; Wu, R.-J.; Watanabe, K.; Tsai, Y.-C. Diversity of lactic acid bacteria in suan-tsai and fu-tsai, traditional fermented mustard products of Taiwan. Int. J. Food Microbiol. 2009, 135, 203–210. [Google Scholar] [CrossRef]
- Liu, W.-H.; Yang, C.-H.; Lin, C.-T.; Li, S.-W.; Cheng, W.-S.; Jiang, Y.-P.; Wu, C.-C.; Chang, C.-H.; Tsai, Y.-C. Genome architecture of Lactobacillus plantarum PS128, a probiotic strain with potential immunomodulatory activity. Gut Pathog. 2015, 7, 22. [Google Scholar] [CrossRef]
- Liao, P.-L.; Wu, C.-C.; Chen, T.-Y.; Tsai, Y.-C.; Peng, W.-S.; Yang, D.-J.; Kang, J.-J. Toxicity Studies of Lactobacillus plantarum PS128TM Isolated from Spontaneously Fermented Mustard Greens. Foods 2019, 8, 668. [Google Scholar] [CrossRef] [PubMed]
- Yatawara, C.J.; Einfeld, S.L.; Hickie, I.B.; A Davenport, T.; Guastella, A.J. The effect of oxytocin nasal spray on social interaction deficits observed in young children with autism: A randomized clinical crossover trial. Mol. Psychiatry 2016, 21, 1225–1231. [Google Scholar] [CrossRef]
- Parker, K.J.; Oztan, O.; Libove, R.A.; Sumiyoshi, R.D.; Jackson, L.P.; Karhson, D.S.; Summers, J.E.; Hinman, K.E.; Motonaga, K.S.; Phillips, J.M.; et al. Intranasal oxytocin treatment for social deficits and biomarkers of response in children with autism. Proc. Natl. Acad. Sci. USA 2017, 114, 8119–8124. [Google Scholar] [CrossRef] [PubMed]
- Constantino, J.; Gruber, C. Social Responsive Scale (SRS) Manual; Western Psychological Services: Los Angeles, CA, USA, 2005. [Google Scholar]
- Aman, M.G.; Singh, N.N.; Stewart, A.W.; Field, C.J. The Aberrant Behavior Checklist: A Behavior Rating Scale for the As-sessment of Treatment Effects. Am. J. Ment. Defic. 1985, 89, 485–491. [Google Scholar] [PubMed]
- Busner, J.; Targum, S.D. The Clinical Global Impressions Scale: Applying a Research Tool in Clinical Practice. Psychiatry (Edgmont) 2007, 4, 28–37. [Google Scholar]
- Bolyen, E.; Rideout, J.R.; Dillon, M.R.; Bokulich, N.A.; Abnet, C.C.; Al-Ghalith, G.A.; Alexander, H.; Alm, E.J.; Arumugam, M.; Asnicar, F.; et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat. Biotechnol. 2019, 37, 852–857. [Google Scholar] [CrossRef] [PubMed]
- Friedman, J.; Alm, E.J. Inferring Correlation Networks from Genomic Survey Data. PLoS Comput. Biol. 2012, 8, e1002687. [Google Scholar] [CrossRef] [PubMed]
- Mallick, H.; Rahnavard, A.; McIver, L.J.; Ma, S.; Zhang, Y.; Nguyen, L.H.; Tickle, T.L.; Weingart, G.; Ren, B.; Schwager, E.H.; et al. Multivariable Association Discovery in Population-Scale Meta-Omics Studies. bioRxiv 2021. [Google Scholar] [CrossRef]
- Ye, L.; Bae, M.; Cassilly, C.D.; Jabba, S.V.; Thorpe, D.W.; Martin, A.M.; Lu, H.-Y.; Wang, J.; Thompson, J.D.; Lickwar, C.R.; et al. Enteroendocrine cells sense bacterial tryptophan catabolites to activate enteric and vagal neuronal pathways. Cell Host Microbe 2021, 29, 179–196.e9. [Google Scholar] [CrossRef] [PubMed]
- Skuse, D.H.; Gallagher, L. Dopaminergic-neuropeptide interactions in the social brain. Trends Cogn. Sci. 2009, 13, 27–35. [Google Scholar] [CrossRef]
- Marotta, R.; Risoleo, M.C.; Messina, G.; Parisi, L.; Carotenuto, M.; Vetri, L.; Roccella, M. The Neurochemistry of Autism. Brain Sci. 2020, 10, 163. [Google Scholar] [CrossRef]
- Inoue, R.; Sakaue, Y.; Sawai, C.; Sawai, T.; Ozeki, M.; Romero-Pérez, G.A.; Tsukahara, T. A preliminary investigation on the relationship between gut microbiota and gene expressions in peripheral mononuclear cells of infants with autism spectrum disorders. Biosci. Biotechnol. Biochem. 2016, 80, 2450–2458. [Google Scholar] [CrossRef] [PubMed]
- Luna, R.A.; Oezguen, N.; Balderas, M.; Venkatachalam, A.; Runge, J.K.; Versalovic, J.; Veenstra-VanderWeele, J.; Anderson, G.M.; Savidge, T.; Williams, K.C. Distinct Microbiome-Neuroimmune Signatures Correlate With Functional Abdominal Pain in Children With Autism Spectrum Disorder. Cell. Mol. Gastroenterol. Hepatol. 2017, 3, 218–230. [Google Scholar] [CrossRef] [PubMed]
- Averina, O.V.; Kovtun, A.S.; Polyakova, S.I.; Savilova, A.M.; Rebrikov, D.V.; Danilenko, V.N. The bacterial neurometabolic signature of the gut microbiota of young children with autism spectrum disorders. J. Med Microbiol. 2020, 69, 558–571. [Google Scholar] [CrossRef]
- Lustgarten, M.S. The Role of the Gut Microbiome on Skeletal Muscle Mass and Physical Function: 2019 Update. Front. Physiol. 2019, 10, 1435. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Mantrana, I.; Selma-Royo, M.; Alcantara, C.; Collado, M.C. Shifts on Gut Microbiota Associated to Mediterranean Diet Adherence and Specific Dietary Intakes on General Adult Population. Front. Microbiol. 2018, 9, 890. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, H.; Zhu, L.; Xu, Y.; Liu, N.; Sun, X.; Hu, L.; Huang, H.; Wei, K.; Zhu, R. Dynamic Distribution of Gut Microbiota in Goats at Different Ages and Health States. Front. Microbiol. 2018, 9, 2509. [Google Scholar] [CrossRef]
- Guo, M.; Li, Z. Polysaccharides isolated fromNostoc communeVaucher inhibit colitis-associated colon tumorigenesis in mice and modulate gut microbiota. Food Funct. 2019, 10, 6873–6881. [Google Scholar] [CrossRef]
- Gao, B.; Zhong, M.; Shen, Q.; Wu, Y.; Cao, M.; Ju, S.; Chen, L. Gut microbiota in early pregnancy among women with Hyperglycaemia vs. Normal blood glucose. BMC Pregnancy Childbirth 2020, 20, 1–11. [Google Scholar] [CrossRef]
- Ma, S.; You, Y.; Huang, L.; Long, S.; Zhang, J.; Guo, C.; Zhang, N.; Wu, X.; Xiao, Y.; Tan, H. Alterations in Gut Microbiota of Gestational Diabetes Patients During the First Trimester of Pregnancy. Front. Cell. Infect. Microbiol. 2020, 10, 58. [Google Scholar] [CrossRef] [PubMed]
- Strati, F.; Cavalieri, D.; Albanese, D.; De Felice, C.; Donati, C.; Hayek, J.; Jousson, O.; Leoncini, S.; Renzi, D.; Calabrò, A.; et al. New evidences on the altered gut microbiota in autism spectrum disorders. Microbiome 2017, 5, 1–11. [Google Scholar] [CrossRef]
- Tomova, A.; Soltys, K.; Kemenyova, P.; Karhanek, M.; Babinska, K. The Influence of Food Intake Specificity in Children with Autism on Gut Microbiota. Int. J. Mol. Sci. 2020, 21, 2797. [Google Scholar] [CrossRef]
- Berding, K.; Donovan, S.M. Diet Can Impact Microbiota Composition in Children with Autism Spectrum Disorder. Front. Neurosci. 2018, 12, 515. [Google Scholar] [CrossRef]
- El Hage, R.; Hernandez-Sanabria, E.; Arroyo, M.C.; Props, R.; Van De Wiele, T. Propionate-Producing Consortium Restores Antibiotic-Induced Dysbiosis in a Dynamic in vitro Model of the Human Intestinal Microbial Ecosystem. Front. Microbiol. 2019, 10, 1206. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.-W.; Park, J.G.; Ilhan, Z.E.; Wallstrom, G.; LaBaer, J.; Adams, J.B.; Krajmalnik-Brown, R. Reduced Incidence of Prevotella and Other Fermenters in Intestinal Microflora of Autistic Children. PLOS ONE 2013, 8, e68322. [Google Scholar] [CrossRef] [PubMed]
- Jarett, J.K.; Carlson, A.; Serao, M.R.; Strickland, J.; Serfilippi, L.; Ganz, H.H. Diets with and without edible cricket support a similar level of diversity in the gut microbiome of dogs. PeerJ 2019, 7, e7661. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Ma, W.; Zhang, J.; He, Y.; Wang, J. Analysis of gut microbiota profiles and microbe-disease associations in children with autism spectrum disorders in China. Sci. Rep. 2018, 8, 1–9. [Google Scholar] [CrossRef]
- De Angelis, M.; Francavilla, R.; Piccolo, M.; De Giacomo, A.; Gobbetti, M. Autism spectrum disorders and intestinal microbiota. Gut Microbes 2015, 6, 207–213. [Google Scholar] [CrossRef]
- Layeghifard, M.; Hwang, D.M.; Guttman, D.S. Disentangling Interactions in the Microbiome: A Network Perspective. Trends Microbiol. 2017, 25, 217–228. [Google Scholar] [CrossRef]
- Liu, F.; Horton-Sparks, K.; Hull, V.; Li, R.W.; Martínez-Cerdeño, V. The valproic acid rat model of autism presents with gut bacterial dysbiosis similar to that in human autism. Mol. Autism 2018, 9, 1–13. [Google Scholar] [CrossRef]
- Iritani, S.; Torii, Y.; Habuchi, C.; Sekiguchi, H.; Fujishiro, H.; Yoshida, M.; Go, Y.; Iriki, A.; Isoda, M.; Ozaki, N. The neuropathological investigation of the brain in a monkey model of autism spectrum disorder with ABCA13 deletion. Int. J. Dev. Neurosci. 2018, 71, 130–139. [Google Scholar] [CrossRef]
- Rose, D.R.; Yang, H.; Serena, G.; Sturgeon, C.; Ma, B.; Careaga, M.; Hughes, H.K.; Angkustsiri, K.; Rose, M.; Hertz-Picciotto, I. Differential Immune Responses and Microbiota Profiles in Children with Autism Spectrum Disorders and Co-Morbid Gas-trointestinal Symptoms. Brain Behav. Immun. 2018, 70, 354–368. [Google Scholar] [CrossRef]
- Oliphant, K.; Allen-Vercoe, E. Macronutrient metabolism by the human gut microbiome: Major fermentation by-products and their impact on host health. Microbiome 2019, 7, 1–15. [Google Scholar] [CrossRef]
- Fritz, J.H. Arginine Cools the Inflamed Gut. Infect. Immun. 2013, 81, 3500–3502. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, M.K.; Kartawy, M.; Amal, H. The role of nitric oxide in brain disorders: Autism spectrum disorder and other psychiatric, neurological, and neurodegenerative disorders. Redox Biol. 2020, 34, 101567. [Google Scholar] [CrossRef] [PubMed]
- Dhir, S.; Tarasenko, M.; Napoli, E.; Giulivi, C. Neurological, Psychiatric, and Biochemical Aspects of Thiamine Deficiency in Children and Adults. Front. Psychiatry 2019, 10, 207. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.; Liu, K.; Liu, J.; Liu, Y.-W.; Xu, L.; Wang, H.; Zhu, Y.; Wang, P.; Li, Z.; Wen, J.; et al. Dysbiotic Gut Microbiota and Dysregulation of Cytokine Profile in Children and Teens With Autism Spectrum Disorder. Front. Neurosci. 2021, 15, 635925. [Google Scholar] [CrossRef]
- Udayappan, S.; Manneras-Holm, L.; Chaplin-Scott, A.; Belzer, C.; Herrema, H.; Dallinga-Thie, G.M.; Duncan, S.H.; Stroes, E.S.G.; Groen, A.K.; Flint, H.J.; et al. Oral treatment with Eubacterium hallii improves insulin sensitivity in db/db mice. npj Biofilms Microbiomes 2016, 2, 16009. [Google Scholar] [CrossRef]
- Husarova, V.M.; Lakatosova, S.; Pivovarciova, A.; Babinska, K.; Bakos, J.; Durdiakova, J.; Kubranska, A.; Ondrejka, I.; Ostatnikova, D. Plasma Oxytocin in Children with Autism and Its Correlations with Behavioral Parameters in Children and Parents. Psychiatry Investig. 2016, 13, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.-F.; Dai, Y.-C.; Wu, J.; Jia, M.-X.; Zhang, J.-S.; Shou, X.-J.; Han, S.-P.; Zhang, R.; Han, J.-S. Plasma Oxytocin and Arginine-Vasopressin Levels in Children with Autism Spectrum Disorder in China: Associations with Symptoms. Neurosci. Bull. 2016, 32, 423–432. [Google Scholar] [CrossRef]
- Miller, M.; Bales, K.L.; Taylor, S.L.; Yoon, J.; Hostetler, C.M.; Carter, C.S.; Solomon, M. Oxytocin and Vasopressin in Children and Adolescents With Autism Spectrum Disorders: Sex Differences and Associations With Symptoms. Autism Res. 2013, 6, 91–102. [Google Scholar] [CrossRef] [PubMed]
- Parker, K.J.; Garner, J.P.; Libove, R.A.; Hyde, S.A.; Hornbeak, K.B.; Carson, D.S.; Liao, C.-P.; Phillips, J.M.; Hallmayer, J.F.; Hardan, A.Y. Plasma oxytocin concentrations and OXTR polymorphisms predict social impairments in children with and without autism spectrum disorder. Proc. Natl. Acad. Sci. USA 2014, 111, 12258–12263. [Google Scholar] [CrossRef]
- Jansen, L.M.C.; Wied, C.C.G.-D.; Wiegant, V.M.; Westenberg, H.G.M.; Lahuis, B.E.; Van Engeland, H. Autonomic and Neuroendocrine Responses to a Psychosocial Stressor in Adults with Autistic Spectrum Disorder. J. Autism Dev. Disord. 2006, 36, 891–899. [Google Scholar] [CrossRef]
- Dadds, M.R.; Moul, C.; Cauchi, A.; Dobson-Stone, C.; Hawes, D.J.; Brennan, J.; Ebstein, R.E. Methylation of the oxytocin receptor gene and oxytocin blood levels in the development of psychopathy. Dev. Psychopathol. 2013, 26, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Jin, D.; Liu, H.-X.; Hirai, H.; Torashima, T.; Nagai, T.; Lopatina, O.; Shnayder, N.A.; Yamada, K.; Noda, M.; Seike, T.; et al. CD38 is critical for social behaviour by regulating oxytocin secretion. Nat. Cell Biol. 2007, 446, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, T.; Otowa, T.; Abe, O.; Kuwabara, H.; Aoki, Y.; Natsubori, T.; Takao, H.; Kakiuchi, C.; Kondo, K.; Ikeda, M.; et al. Oxytocin receptor gene variations predict neural and behavioral response to oxytocin in autism. Soc. Cogn. Affect. Neurosci. 2016, 12, 496–506. [Google Scholar] [CrossRef]
- Masi, A.; Quintana, D.S.; Glozier, N.; Lloyd, A.R.; Hickie, I.B.; Guastella, A.J. Cytokine aberrations in autism spectrum disorder: A systematic review and meta-analysis. Mol. Psychiatry 2014, 20, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Guloksuz, S.A.; Abali, O.; Cetin, E.A.; Gazioglu, S.B.; Deniz, G.; Yildirim, A.; Kawikova, I.; Guloksuz, S.; Leckman, J.F. Elevated plasma concentrations of S100 calcium-binding protein B and tumor necrosis factor alpha in children with autism spectrum disorders. Rev. Bras. Psiquiatr. 2017, 39, 195–200. [Google Scholar] [CrossRef]
- Abou-Donia, M.B.; Suliman, H.B.; Siniscalco, D.; Antonucci, N.; Elkafrawy, P. De novo Blood Biomarkers in Autism: Autoantibodies against Neuronal and Glial Proteins. Behav. Sci. 2019, 9, 47. [Google Scholar] [CrossRef] [PubMed]
- Esnafoglu, E.; Ayyıldız, S.N.; Cırrık, S.; Erturk, E.Y.; Erdil, A.; Daglı, A.; Noyan, T. Evaluation of serum Neuron-specific enolase, S100B, myelin basic protein and glial fibrilliary acidic protein as brain specific proteins in children with autism spectrum disorder. Int. J. Dev. Neurosci. 2017, 61, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Mostafa, G.A.; Al-Ayadhi, L.Y. A lack of association between hyperserotonemia and the increased frequency of serum anti-myelin basic protein auto-antibodies in autistic children. J. Neuroinflamm. 2011, 8, 71. [Google Scholar] [CrossRef]
- Gonzalez-Gronow, M.; Cuchacovich, M.; Francos, R.; Cuchacovich, S.; Blanco, A.; Sandoval, R.; Gomez, C.F.; Valenzuela, J.A.; Ray, R.; Pizzo, S.V. Catalytic autoantibodies against myelin basic protein (MBP) isolated from serum of autistic children impair in vitro models of synaptic plasticity in rat hippocampus. J. Neuroimmunol. 2015, 287, 1–8. [Google Scholar] [CrossRef]
- Kern, J.K.; Geier, D.A.; Sykes, L.K.; Geier, M.R. Relevance of Neuroinflammation and Encephalitis in Autism. Front. Cell. Neurosci. 2016, 9, 519. [Google Scholar] [CrossRef] [PubMed]

| Placebo (n = 17) | Probiotic (n = 18) | p-Value * | |
|---|---|---|---|
| Demographic | |||
| Age (Mean ± SD) | 10.7 ± 4.76 | 9.85 ± 4.91 | 0.66 |
| Sex (N, %) | |||
| Male | 11 (64.7%) | 15 (83.3%) | 0.38 |
| Female | 6 (35.3%) | 3 (16.7%) | |
| Ethnicity (N, %) | |||
| Asian | 14 (82.4%) | 14 (77.8%) | 0.62 |
| Hispanic | 0 | 1 (5.5%) | |
| White | 3 (17.6%) | 3 (16.7%) | |
| Clinical Indices | |||
| GI Severity Index (Mean ± SD) | 3.33 ± 1.37 | 2.54 ± 2.03 | 0.18 |
| Stool Type (Bristol stool chart; N, %) | |||
| Type 1&2 (Constipated) | 1 (5.9%) | 1 (5.6%) | 1.00 |
| Type 3&4 (Normal) | 12 (70.6%) | 13 (72.2%) | |
| Type 5, 6, 7 (Loose Stool) | 3 (17.6%) | 3 (16.7%) | |
| ABC Standardized Score (T-score, Mean ± SD) | 278 ± 34.8 | 272 ± 30.2 | 0.38 |
| SRS Standardized Score (T-score, Mean ± SD) | 83.0 ± 12.1 | 82.3 ± 11.5 | 0.96 |
| CGI-S (Mean ± SD) | 5.12 ± 1.17 | 5.11 ± 0.90 | 0.97 |
| Improvement in Score (Mean Change ± SD) | p-Value * | ||||||
|---|---|---|---|---|---|---|---|
| Control | Probiotic | OXT | Probiotic + OXT | Probiotic | OXT | Probiotic + OXT | |
| ABC | |||||||
| Total Score | 15.00 ± 26.75 | 6.67 ± 26.00 | 12.33 ± 23.16 | −10.43 ± 31.91 | 0.48 | 0.84 | 0.077 |
| Irritability (S1) | 3.45 ± 6.67 | −0.92 ± 6.20 | 2.17 ± 3.97 | −2.43 ± 9.86 | 0.19 | 0.84 | 0.20 |
| Social Withdrawal (S2) | 1.82 ± 8.30 | 3.50 ± 6.36 | 1.67 ± 7.92 | −4.00 ± 10.26 | 0.46 | 1 | 0.28 |
| Stereotypic Behavior (S3) | 3.18 ± 4.38 | 1.17 ± 6.64 | 1.83 ± 5.78 | −1.29 ± 4.27 | 0.67 | 0.45 | 0.069 |
| Hyperactivity/Noncompliance (S4) | 5.64 ± 8.31 | 2.33 ± 8.91 | 5.50 ± 7.45 | −1.57 ± 10.50 | 0.34 | 0.84 | 0.16 |
| Inappropriate Speech (S5) | 0.91 ± 2.12 | 0.58 ± 1.78 | 1.67 ± 3.31 | −1.14 ± 3.02 | 0.66 | 0.80 | 0.20 |
| SRS | |||||||
| Total Score | 22.09 ± 23.71 | 12.31 ± 22.21 | 10.00 ± 24.71 | 4.88 ± 22.95 | 0.45 | 0.23 | 0.26 |
| Awareness | 1.18 ± 2.36 | 1.15 ± 2.58 | 1.33 ± 2.58 | 0.13 ± 3.04 | 0.86 | 0.96 | 0.28 |
| Cognition | 4.73 ± 4.54 | 0.92 ± 4.31 | 2.00 ± 5.18 | 0.38 ± 5.53 | 0.15 | 0.15 | 0.059 |
| Communication | 7.09 ± 9.45 | 4.46 ± 7.13 | 0.50 ± 9.09 | 2.00 ± 8.11 | 0.68 | 0.11 | 0.36 |
| Motivation | 3.27 ± 3.58 | 2.54 ± 4.96 | 2.83 ± 5.67 | 0.88 ± 6.15 | 0.77 | 0.61 | 0.16 |
| Mannerisms | 5.82 ± 6.82 | 3.23 ± 6.61 | 3.33 ± 6.09 | 1.50 ± 5.50 | 0.58 | 0.39 | 0.20 |
| Clinical Feature | Microbiome Taxa | R | FDR * |
|---|---|---|---|
| ABC Inappropriate Speech (T) | Lachnospiraceae (uncultured) | −0.68 | 0.04247 |
| SRS Communication (T) | Eubacterium hallii Group | −0.55 | 0.04282 |
| SRS Mannerisms (T) | Eubacterium hallii Group | −0.60 | 0.01753 |
| SRS Motivation (T) | Rikenellaceae | −0.58 | 0.0645 |
| Alistipes | −0.58 | 0.0645 | |
| Eubacterium hallii Group | −0.56 | 0.0645 | |
| SRS Total Score (T) | Eubacterium hallii Group | −0.59 | 0.00767 |
| Clinical Feature | Microbiome Taxa | Probiotic Group (n = 18) | Placebo Group (n = 17) | ||
|---|---|---|---|---|---|
| R | p-Value | R | p-Value | ||
| SRS Cognition T (V1) | Eubacterium hallii Group (V3-V1) | 0.71 | 0.050 | 0.01 | 0.790 |
| SRS Cognition T (V3-V1) | Eubacterium hallii Group (V1) | −0.97 | 0.005 * | 0.17 | 0.750 |
| ABC Stereotypic Behavior T (V1) | Rikenellaceae (V3-V1) | 0.94 | 0.017 | 0.20 | 0.590 |
| Alistipes (V3-V1) | 0.94 | 0.017 | −0.02 | 0.960 | |
| Christensenellaceae R-7 Group (V3-V1) | 0.82 | 0.046 | −0.09 | 0.810 | |
| Ruminococcaceae UCG-002 (V3-V1) | 0.83 | 0.058 | −0.37 | 0.290 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kong, X.-J.; Liu, J.; Liu, K.; Koh, M.; Sherman, H.; Liu, S.; Tian, R.; Sukijthamapan, P.; Wang, J.; Fong, M.; et al. Probiotic and Oxytocin Combination Therapy in Patients with Autism Spectrum Disorder: A Randomized, Double-Blinded, Placebo-Controlled Pilot Trial. Nutrients 2021, 13, 1552. https://doi.org/10.3390/nu13051552
Kong X-J, Liu J, Liu K, Koh M, Sherman H, Liu S, Tian R, Sukijthamapan P, Wang J, Fong M, et al. Probiotic and Oxytocin Combination Therapy in Patients with Autism Spectrum Disorder: A Randomized, Double-Blinded, Placebo-Controlled Pilot Trial. Nutrients. 2021; 13(5):1552. https://doi.org/10.3390/nu13051552
Chicago/Turabian StyleKong, Xue-Jun, Jun Liu, Kevin Liu, Madelyn Koh, Hannah Sherman, Siyu Liu, Ruiyi Tian, Piyawat Sukijthamapan, Jiuju Wang, Michelle Fong, and et al. 2021. "Probiotic and Oxytocin Combination Therapy in Patients with Autism Spectrum Disorder: A Randomized, Double-Blinded, Placebo-Controlled Pilot Trial" Nutrients 13, no. 5: 1552. https://doi.org/10.3390/nu13051552
APA StyleKong, X.-J., Liu, J., Liu, K., Koh, M., Sherman, H., Liu, S., Tian, R., Sukijthamapan, P., Wang, J., Fong, M., Xu, L., Clairmont, C., Jeong, M.-S., Li, A., Lopes, M., Hagan, V., Dutton, T., Chan, S.-T., Lee, H., ... Song, Y. (2021). Probiotic and Oxytocin Combination Therapy in Patients with Autism Spectrum Disorder: A Randomized, Double-Blinded, Placebo-Controlled Pilot Trial. Nutrients, 13(5), 1552. https://doi.org/10.3390/nu13051552






