Efficacy of Low-Carbohydrate Ketogenic Diet as an Adjuvant Cancer Therapy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analysis
3. Results
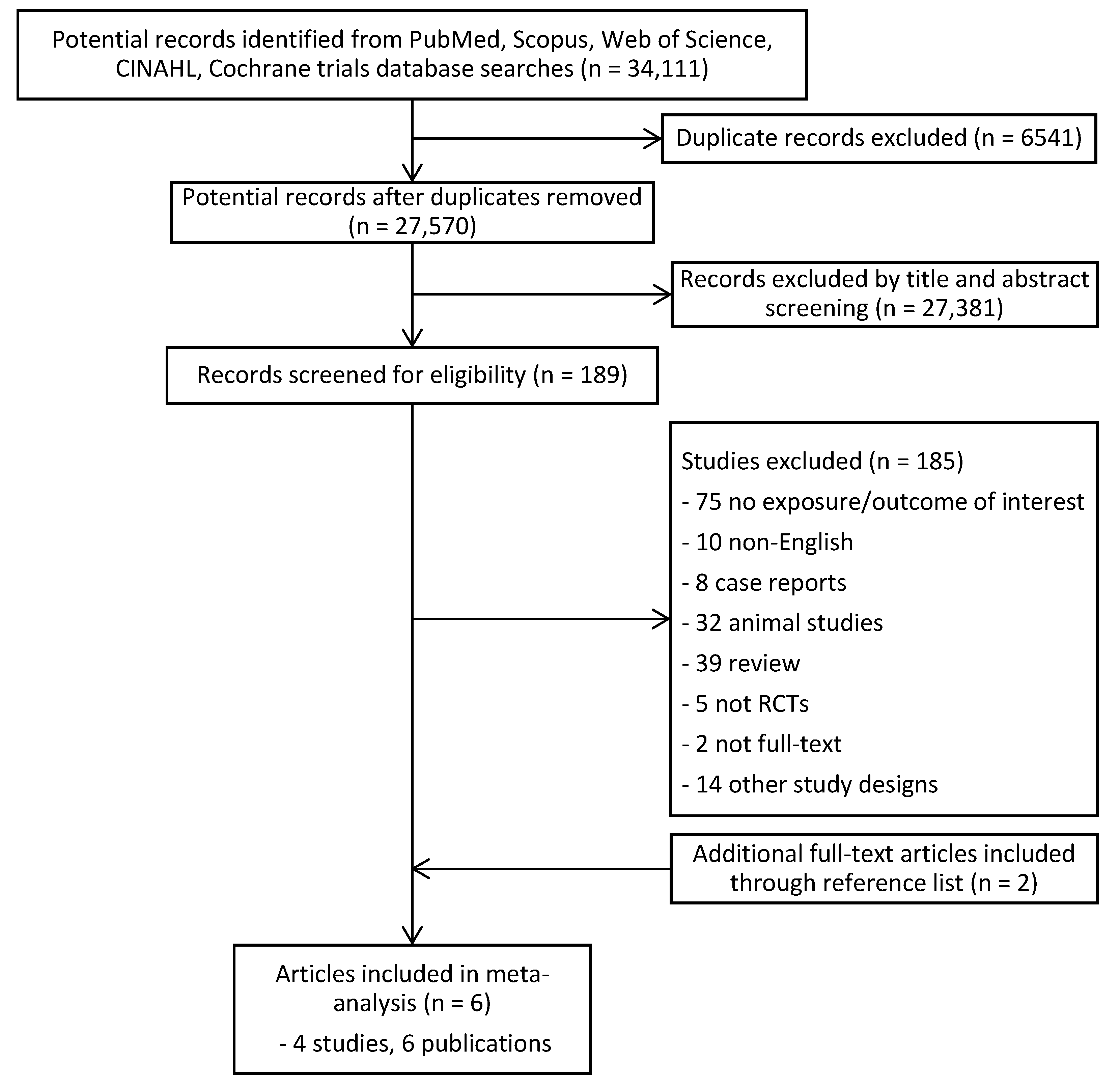
3.1. Study Selection
3.2. Study Characteristics
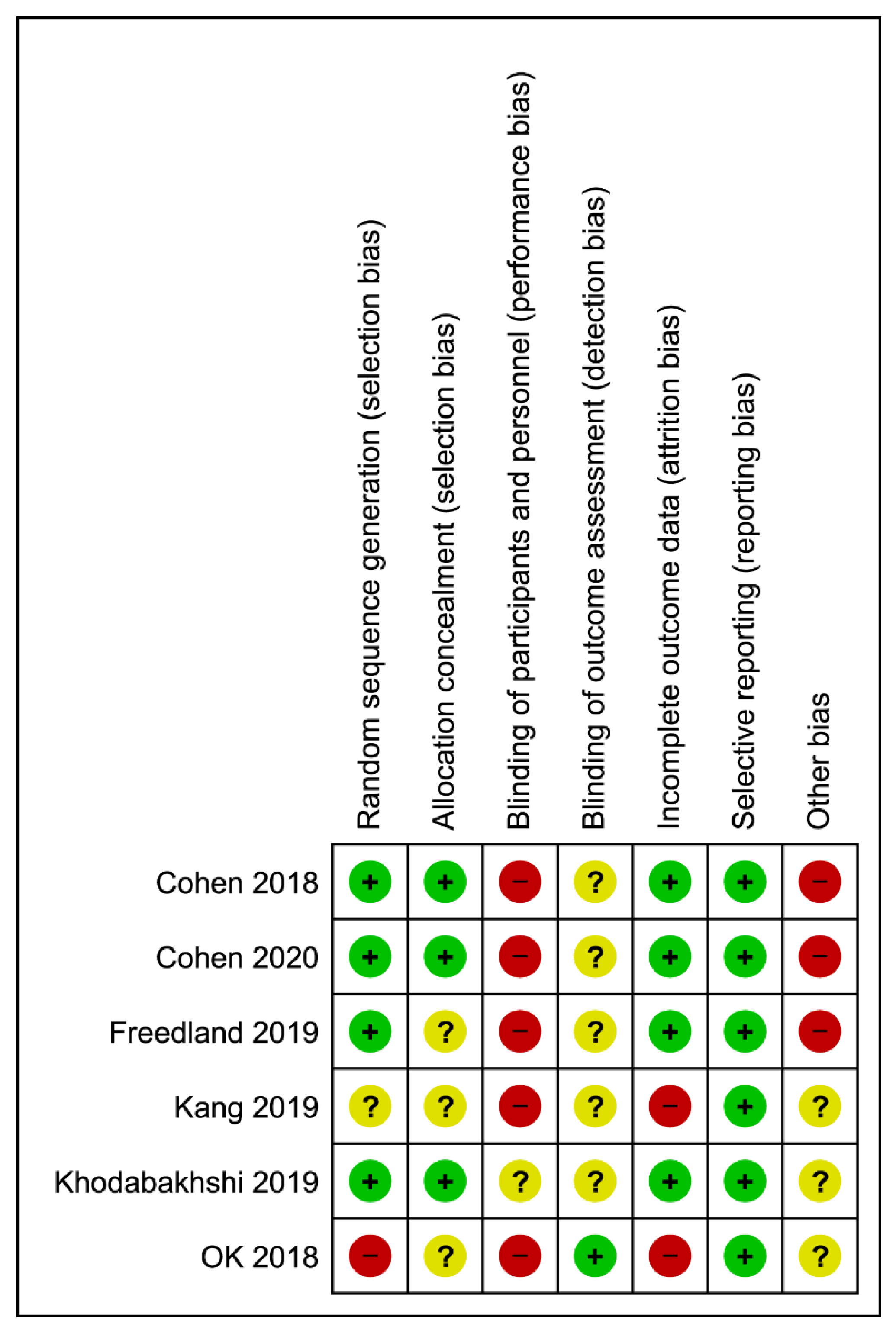
3.3. Study Quality of Trials
3.4. Findings
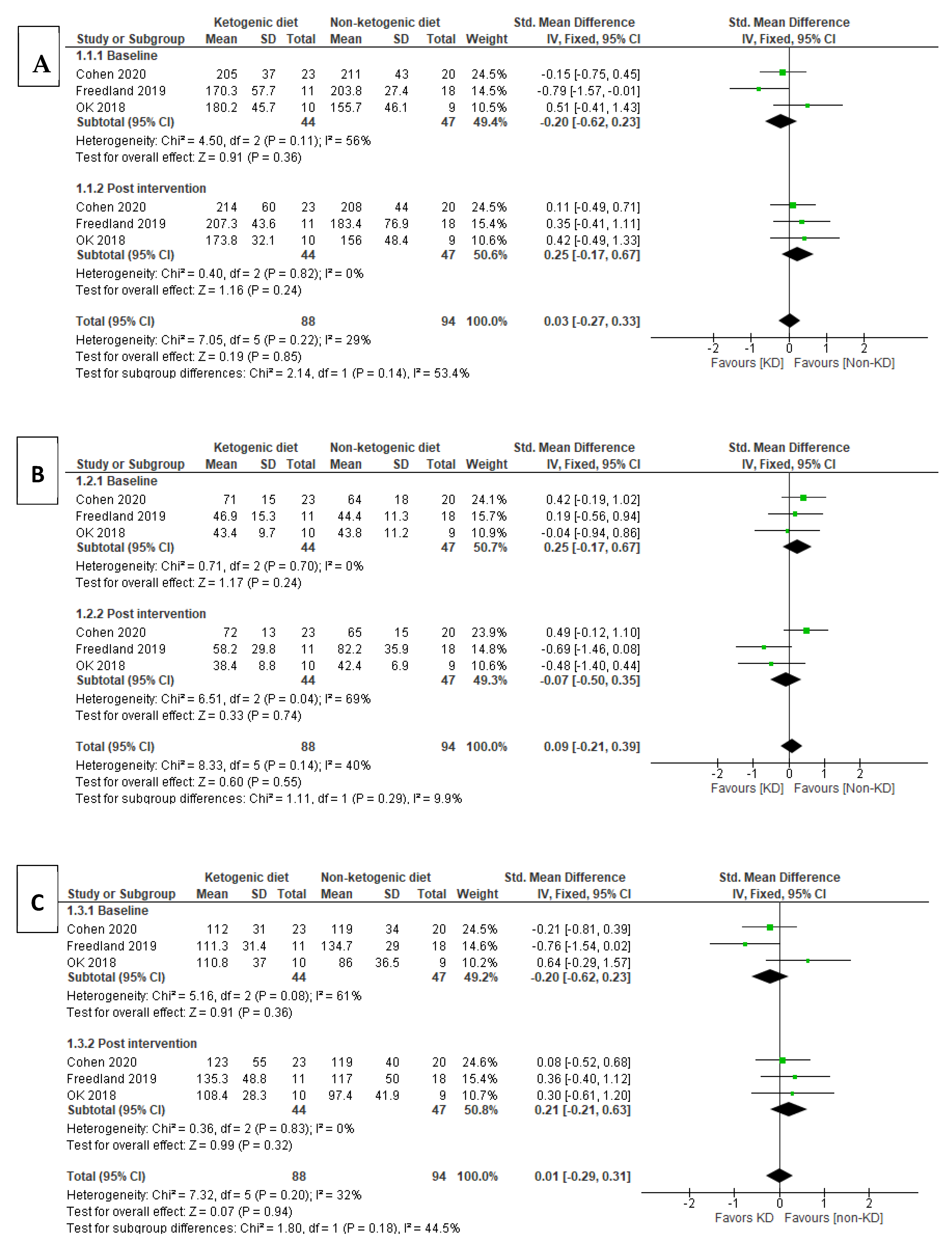
3.4.1. Lipid Profile
Total Cholesterol (TC)
HDL-Cholesterol
LDL-Cholesterol
Triglyceride (TG)
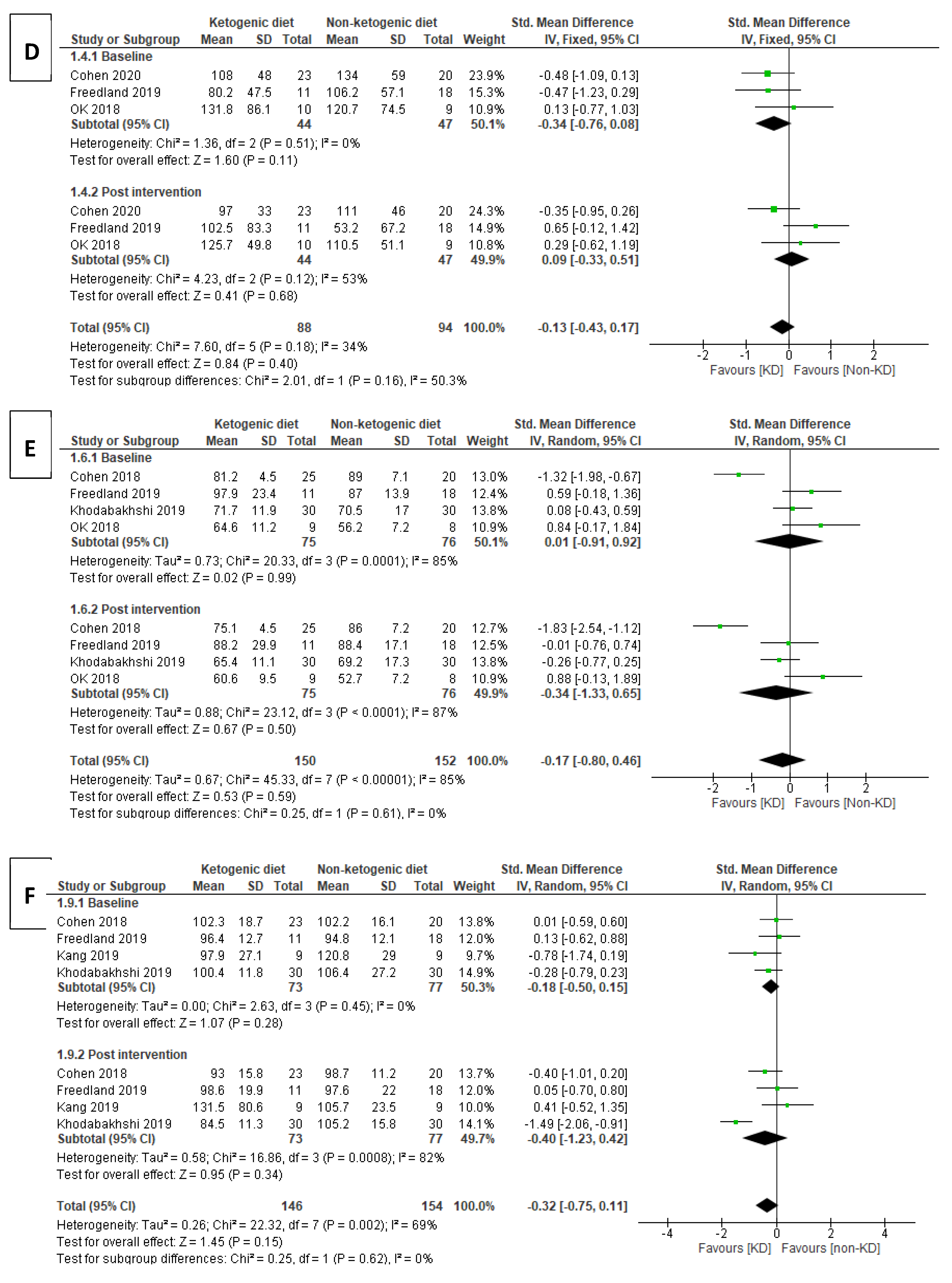
3.4.2. Body Weight (BW)
3.4.3. Fasting Blood Glucose (FBG)
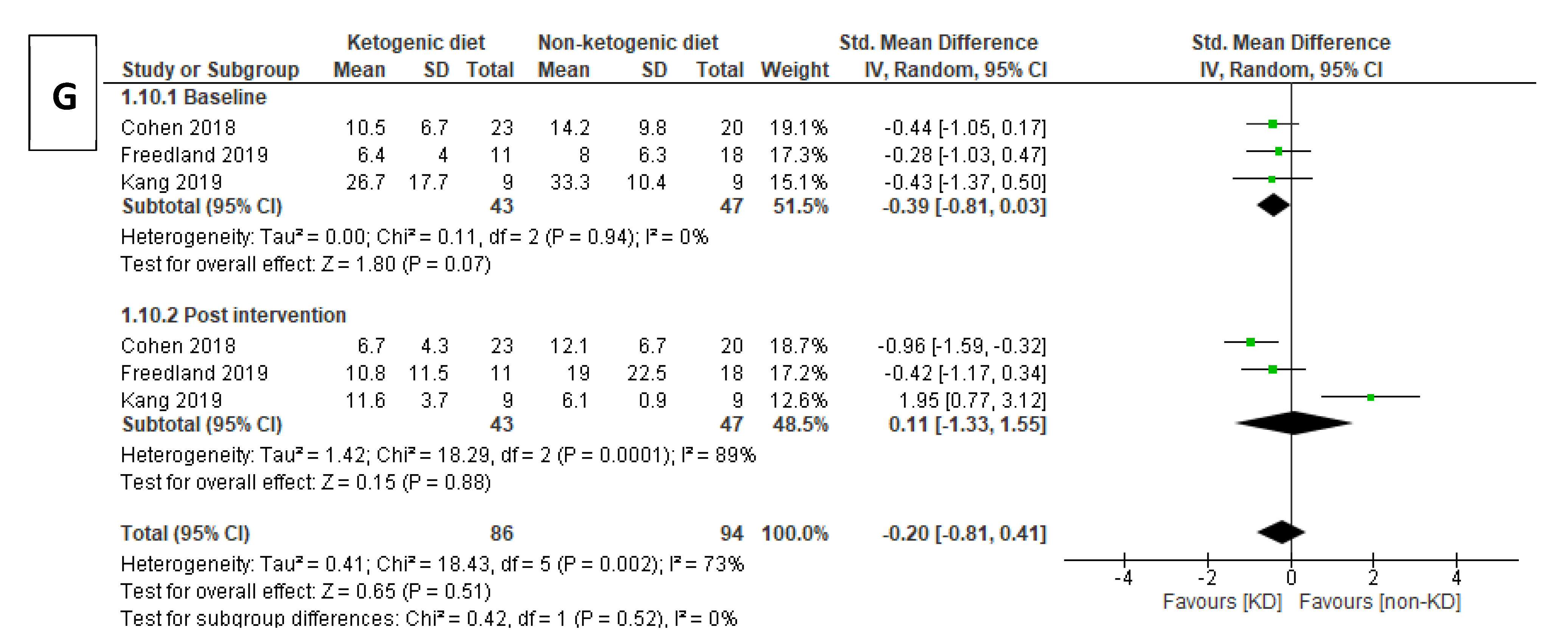
3.4.4. Insulin
3.4.5. Tumor Marker Levels (CEA, CA19-9) and Prostate-Specific Antigen (PSA) Test
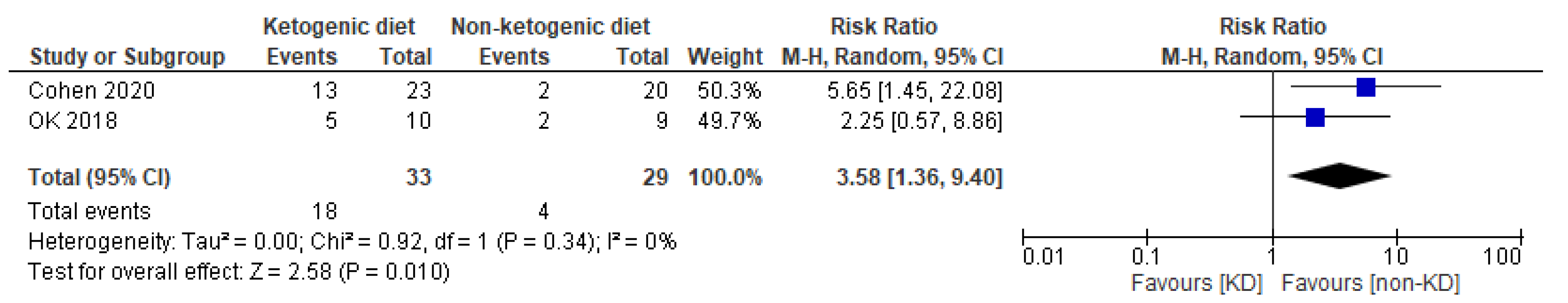
3.4.6. Ketosis
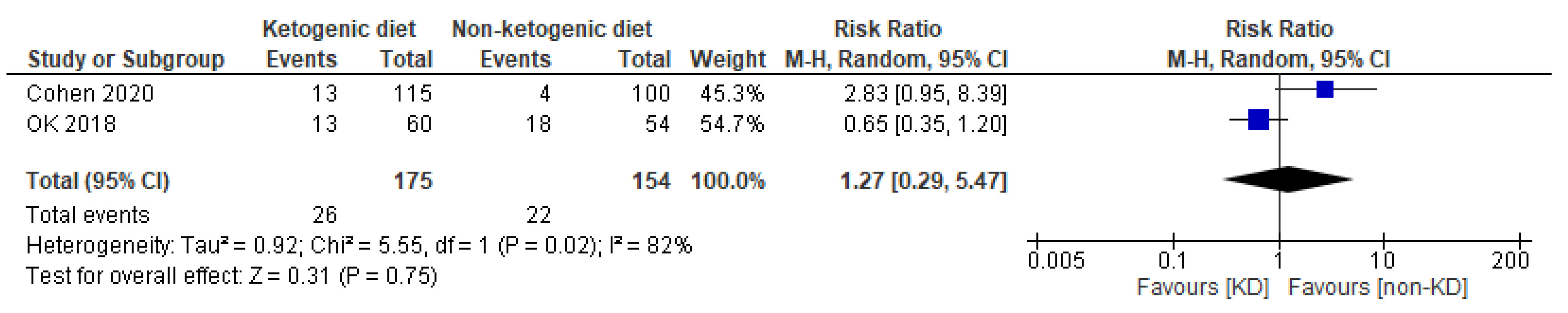
3.4.7. Adverse Event
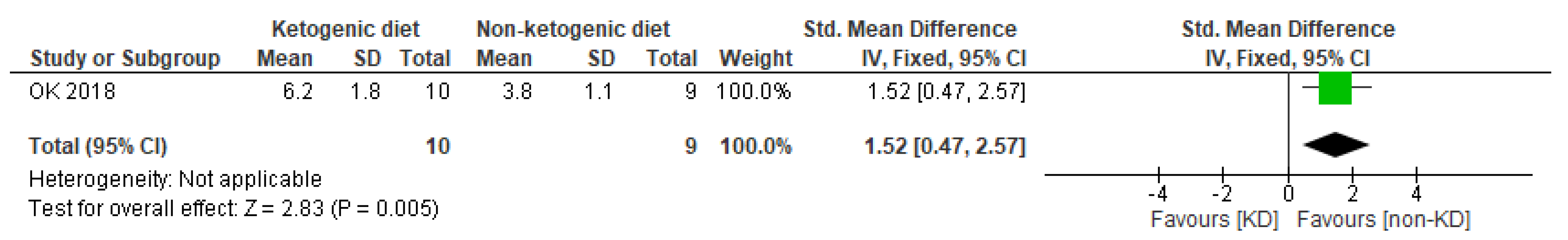
3.4.8. Satisfaction
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Westman, E.C.; Mavropoulos, J.; Yancy, W.S.; Volek, J.S. A review of low-carbohydrate ketogenic diets. Curr. Atheroscler. Rep. 2003, 5, 476–483. [Google Scholar] [CrossRef]
- Weber, D.D.; Aminzadeh-Gohari, S.; Tulipan, J.; Catalano, L.; Feichtinger, R.G.; Kofler, B. Ketogenic diet in the treatment of cancer—Where do we stand? Mol. Metab. 2020, 33, 102–121. [Google Scholar] [CrossRef] [PubMed]
- Stafstrom, C.E.; Rho, J.M. The Ketogenic Diet as a Treatment Paradigm for Diverse Neurological Disorders. Front. Pharmacol. 2012, 3, 59. [Google Scholar] [CrossRef] [PubMed]
- Yancy, W.S.; Foy, M.; Chalecki, A.M.; Vernon, M.C.; Westman, E.C. A low-carbohydrate, ketogenic diet to treat type 2 diabetes. Nutr. Metab. 2005, 2, 34. [Google Scholar] [CrossRef] [PubMed]
- Paoli, A.; Mancin, L.; Giacona, M.C.; Bianco, A.; Caprio, M. Effects of a ketogenic diet in overweight women with polycystic ovary syndrome. J. Transl. Med. 2020, 18, 1–11. [Google Scholar] [CrossRef]
- Klement, R.J. Beneficial effects of ketogenic diets for cancer patients: A realist review with focus on evidence and confirmation. Med. Oncol. 2017, 34, 132. [Google Scholar] [CrossRef] [PubMed]
- Klement, R.J. Calorie or Carbohydrate Restriction? The Ketogenic Diet as Another Option for Supportive Cancer Treatment. Oncologist 2013, 18, 1056. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liberti, M.V.; Locasale, J.W. The Warburg Effect: How Does it Benefit Cancer Cells? Trends Biochem. Sci. 2016, 41, 211–218. [Google Scholar] [CrossRef]
- Weber, D.D.; Aminazdeh-Gohari, S.; Kofler, B. Ketogenic diet in cancer therapy. Aging 2018, 10, 164–165. [Google Scholar] [CrossRef]
- Allen, B.G.; Bhatia, S.K.; Anderson, C.M.; Eichenberger-Gilmore, J.M.; Sibenaller, Z.A.; Mapuskar, K.A.; Schoenfeld, J.D.; Buatti, J.M.; Spitz, D.R.; Fath, M.A. Ketogenic diets as an adjuvant cancer therapy: History and potential mechanism. Redox Biol. 2014, 2, 963–970. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Masood, W.; Annamaraju, P.; Uppaluri, K.R. Ketogenic Diet. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Kang, C.M.; Yun, B.; Kim, M.; Song, M.; Kim, Y.-H.; Lee, S.H.; Lee, H.; Lee, S.M.; Lee, S.-M. Postoperative serum metabolites of patients on a low carbohydrate ketogenic diet after pancreatectomy for pancreatobiliary cancer: A nontargeted metabolomics pilot study. Sci. Rep. 2019, 9, 1–11. [Google Scholar] [CrossRef]
- Ok, J.H.; Lee, H.; Chung, H.-Y.; Lee, S.H.; Choi, E.J.; Kang, C.M.; Lee, S.M. The Potential Use of a Ketogenic Diet in Pancreatobiliary Cancer Patients After Pancreatectomy. Anticancer. Res. 2018, 38, 6519–6527. [Google Scholar] [CrossRef]
- Heinemann, L. Insulin Assay Standardization: Leading to Measures of Insulin Sensitivity and Secretion for Practical Clinical Care: Response to Staten et al. Diabetes Care 2010, 33, e83. [Google Scholar] [CrossRef] [PubMed]
- Rohatgi, A. WebPlotDigitizer: Web Based Tool to Extract Data from Plots, Images, and Maps. USA: WebPlotDigitizer. 2019. Available online: https://automeris.io/WebPlotDigitizer (accessed on 15 September 2020).
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Review of Interventions Version 5.1.0 [updated March 2011]. 2011. Available online: www.handbook.cochrane.org. (accessed on 15 September 2020).
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Luo, D.; Weng, H.; Zeng, X.; Lin, L.; Chu, H.; Tong, T. Optimally estimating the sample standard deviation from the five-number summary. Res. Synth. Methods 2020, 11, 641–654. [Google Scholar] [CrossRef] [PubMed]
- Luo, D.; Wan, X.; Liu, J.; Tong, T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat. Methods Med Res. 2018, 27, 1785–1805. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res. Methodol. 2014, 14, 1–13. [Google Scholar] [CrossRef]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef]
- Cohen, C.W.; Fontaine, K.R.; Arend, R.C.; Gower, B.A. A Ketogenic Diet Is Acceptable in Women with Ovarian and Endometrial Cancer and Has No Adverse Effects on Blood Lipids: A Randomized, Controlled Trial. Nutr. Cancer 2019, 72, 584–594. [Google Scholar] [CrossRef]
- Cohen, C.W.; Fontaine, K.R.; Arend, R.C.; Alvarez, R.D.; Iii, C.A.L.; Huh, W.K.; Bevis, K.S.; Kim, K.H.; Straughn, J.M.; A Gower, B. A Ketogenic Diet Reduces Central Obesity and Serum Insulin in Women with Ovarian or Endometrial Cancer. J. Nutr. 2018, 148, 1253–1260. [Google Scholar] [CrossRef] [PubMed]
- Freedland, S.J.; Howard, L.; Allen, J.; Smith, J.; Stout, J.; Aronson, W.; Inman, B.A.; Armstrong, A.J.; George, D.; Westman, E.; et al. A lifestyle intervention of weight loss via a low-carbohydrate diet plus walking to reduce metabolic disturbances caused by androgen deprivation therapy among prostate cancer patients: Carbohydrate and prostate study 1 (CAPS1) randomized controlled trial. Prostate Cancer Prostatic Dis. 2019, 22, 428–437. [Google Scholar] [CrossRef] [PubMed]
- Khodabakhshi, A.; Akbari, M.E.; Mirzaei, H.R.; Mehrad-Majd, H.; Kalamian, M.; Davoodi, S.H. Feasibility, Safety, and Beneficial Effects of MCT-Based Ketogenic Diet for Breast Cancer Treatment: A Randomized Controlled Trial Study. Nutr. Cancer 2019, 72, 627–634. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of Cancer: The Next Generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- Allen, B.G.; Bhatia, S.K.; Buatti, J.M.; Brandt, K.E.; Lindholm, K.E.; Button, A.M.; Szweda, L.I.; Smith, B.J.; Spitz, D.R.; Fath, M.A. Ketogenic Diets Enhance Oxidative Stress and Radio-Chemo-Therapy Responses in Lung Cancer Xenografts. Clin. Cancer Res. 2013, 19, 3905–3913. [Google Scholar] [CrossRef] [PubMed]
- Schieber, M.; Chandel, N.S. ROS Function in Redox Signaling and Oxidative Stress. Curr. Biol. 2014, 24, R453–R462. [Google Scholar] [CrossRef] [PubMed]
- Sengupta, S.; Peterson, T.R.; Laplante, M.; Oh, S.; Sabatini, D.M. mTORC1 controls fasting-induced ketogenesis and its modulation by ageing. Nat. Cell Biol. 2010, 468, 1100–1104. [Google Scholar] [CrossRef]
- Grabacka, M.; Pierzchalska, M.; Reiss, K. Peroxisome proliferator activated receptor α ligands as anticancer drugs targeting mitochondrial metabolism. Curr. Pharm. Biotechnol. 2013, 14, 342–356. [Google Scholar] [CrossRef]
- Klement, R.J.; Champ, C.E. Calories, carbohydrates, and cancer therapy with radiation: Exploiting the five R’s through dietary manipulation. Cancer Metastasis Rev. 2014, 33, 217–229. [Google Scholar] [CrossRef]
- McDaniel, S.S.; Rensing, N.R.; Thio, L.L.; Yamada, K.A.; Wong, M. The ketogenic diet inhibits the mammalian target of rapamycin (mTOR) pathway. Epilepsia 2011, 52, e7–e11. [Google Scholar] [CrossRef]
| Parameter | Inclusion Criteria |
|---|---|
| Population | Cancer patients |
| Intervention/exposures | Dietary intake of ketogenic diet; low-carbohydrate diet |
| Comparison | Any comparison |
| Outcomes | Effectiveness, weight change, glucose level, insulin, lipid profiles, adverse outcome |
| Type of study | Randomized controlled trials |
| 1. KD * | 21. Tumo * |
| 2. Ketogenic * | 22. Carcinoma * |
| 3. Keto * | 23. Malignan * |
| 4. Low carb * | 24. Ongolog * |
| 5. Low-carb * | 25. Metastas * |
| 6. High fat * | 26. Lymphoma * |
| 7. High-fat * | 27. leukemia |
| 8. medium chain tryglyceride * | 28. Adenoma * |
| 9. medium chain triglyceride * | 29. Adenocarcinoma* |
| 10. MCT * | 30. Glioma * |
| 11. Atkin * | 31. Sarcoma * |
| 12. 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 | 32. 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 |
| 13. Diet * | 33. Randomized controlled trial * |
| 14. Plan * | 34. Controlled clinical trial * |
| 15. Treat * | 35. Random * |
| 16. 13 or 14 or 15 | 36. RCT * |
| 17. 12 and 16 | 37. 33 or 34 or 35 or 36 |
| 18. 1 or 17 | 38. 18 and 32 and 37 |
| 19. Neoplasm * | |
| 20. Cancer * |
| First Author/Year | Study Design | Types of Cancer | Concurrent Treatment | Interventions | Inclusion Criteria | Exclusion Criteria | Outcomes |
|---|---|---|---|---|---|---|---|
| OK (2018) | Prospective RCT |
| Operation | KD: 3–6% of carbohydrate and 1 g/kg of high-quality protein was provided daily. 70–80% of energy was given through fat to achieve a ketogenic ratio of 1.05–1.75:1 (fat: carbohydrate + protein). |
|
|
|
| Cohen (2018) | RCT | Ovarian/endometrial cancer | Chemotherapy | KD: ~5% pf energy from carbohydrate (≤20 g/d), 25% energy from protein (≤100 g/d) and 70% energy from fat (≥125 g/d) |
| Not mentioned |
|
| Cohen (2020) | RCT | Ovarian/endometrial cancer | Chemotherapy | KD: ~5% pf energy from carbohydrate (≤20 g/d), 25% energy from protein (≤100 g/d) and 70% energy from fat (≥125 g/d) |
| Serious cardiovascular disease and events. |
|
| Khodabakhshi (2019) | RCT | Breast cancer | Chemotherapy | KD: MCT-based KD containing 6% calorie from CHO, 19% protein, 20% MCT, 55% fat |
|
|
|
| Kang (2019) | Prospective RC |
| Operation | LCKD: Energy content: 1500 kcal/d, provided 4% from carbohydrate, 16% from protein and 80% from fat. Ketogenic ratio of 1.75:1 (F: C + P w/w). |
|
|
|
| Freedland (2019) | Multi-center phase II RCT | Prostate cancer | ADT | LCD/walking arm: carbohydrate intake ≤ 20 g/d and walk ≥ 30 min/day for ≥5 days/week. List of LC foods to choose from and list of moderate/high carbohydrate foods to limit. Sample menus and recipes were given. Coaching by dietitian in person or by phone weekly for months 0–3 and biweekly for months 4–6. |
|
|
|
| First Author (Year) | Intervention | Number of Enrollment | Number of Completion | Mean (SD) Age at Baseline (Year) | BMI Mean (SD) In kg/m2 at Baseline | Duration (Mean Week) | Completion Rate on Diets at the End of Trial (%) |
|---|---|---|---|---|---|---|---|
| OK (2018) | KD GD | 20 10 | 10 9 | 57.8 (7.3) 66.3 (9.8) | 24.0 (2.2) 22.2 (2.6) | 4 | 50.0 90.0 |
| Cohen (2018) | KD ACS | 37 36 | 25 20 | 61.5 (8.5) 58.6 (11.7) | 30.7 (8.0) 33.0 (10.7) | 12 | 55.6 67.6 |
| Cohen (2020) | KD ACS | 37 36 | 25 20 | 61.5 (8.5) 58.6 (11.7) | 30.7 (8.0) 33.0 (10.7) | 12 | 55.6 67.6 |
| Khodabakhshi (2019) | KD SD | 40 37 | 30 30 | 44.8 (8.4) 45.2 (15.0) | 28.47 (4.1) 28.44 (5.8) | 12 | 75.0 81.1 |
| Kang (2019) | LCKD GD | 20 10 | 9 9 | 58.3 (7.6) 66.3 (9.8) | 24.0 (2.2) 22.2 (2.7) | 4 | 45.0 90.0 |
| Freedland (2019) | LCD GD | 20 22 | 11 18 | 67.8 (12.7) 63.8 (11.3) | 31.9 (9.5) 29.4 (4.0) | 24 | 55.0 81.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Y.-F.; Mattamel, P.B.; Joseph, T.; Huang, J.; Chen, Q.; Akinwunmi, B.O.; Zhang, C.J.P.; Ming, W.-K. Efficacy of Low-Carbohydrate Ketogenic Diet as an Adjuvant Cancer Therapy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2021, 13, 1388. https://doi.org/10.3390/nu13051388
Yang Y-F, Mattamel PB, Joseph T, Huang J, Chen Q, Akinwunmi BO, Zhang CJP, Ming W-K. Efficacy of Low-Carbohydrate Ketogenic Diet as an Adjuvant Cancer Therapy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients. 2021; 13(5):1388. https://doi.org/10.3390/nu13051388
Chicago/Turabian StyleYang, Ya-Feng, Preety Babychen Mattamel, Tanya Joseph, Jian Huang, Qian Chen, Babatunde O. Akinwunmi, Casper J. P. Zhang, and Wai-Kit Ming. 2021. "Efficacy of Low-Carbohydrate Ketogenic Diet as an Adjuvant Cancer Therapy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" Nutrients 13, no. 5: 1388. https://doi.org/10.3390/nu13051388
APA StyleYang, Y.-F., Mattamel, P. B., Joseph, T., Huang, J., Chen, Q., Akinwunmi, B. O., Zhang, C. J. P., & Ming, W.-K. (2021). Efficacy of Low-Carbohydrate Ketogenic Diet as an Adjuvant Cancer Therapy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients, 13(5), 1388. https://doi.org/10.3390/nu13051388







