The Equity and Effectiveness of Achieving Canada’s Voluntary Sodium Reduction Guidance Targets: A Modelling Study Using the 2015 Canadian Community Health Survey—Nutrition
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Sodium Intake
2.3. Socioeconomic Position
2.4. Covariates
2.5. Modelling the Impact of Health Canada’s Sodium Reduction Guidance on Sodium Intake
2.6. Statistical Analyses
3. Results
SRG Targets and Social Inequities in Sodium Intake
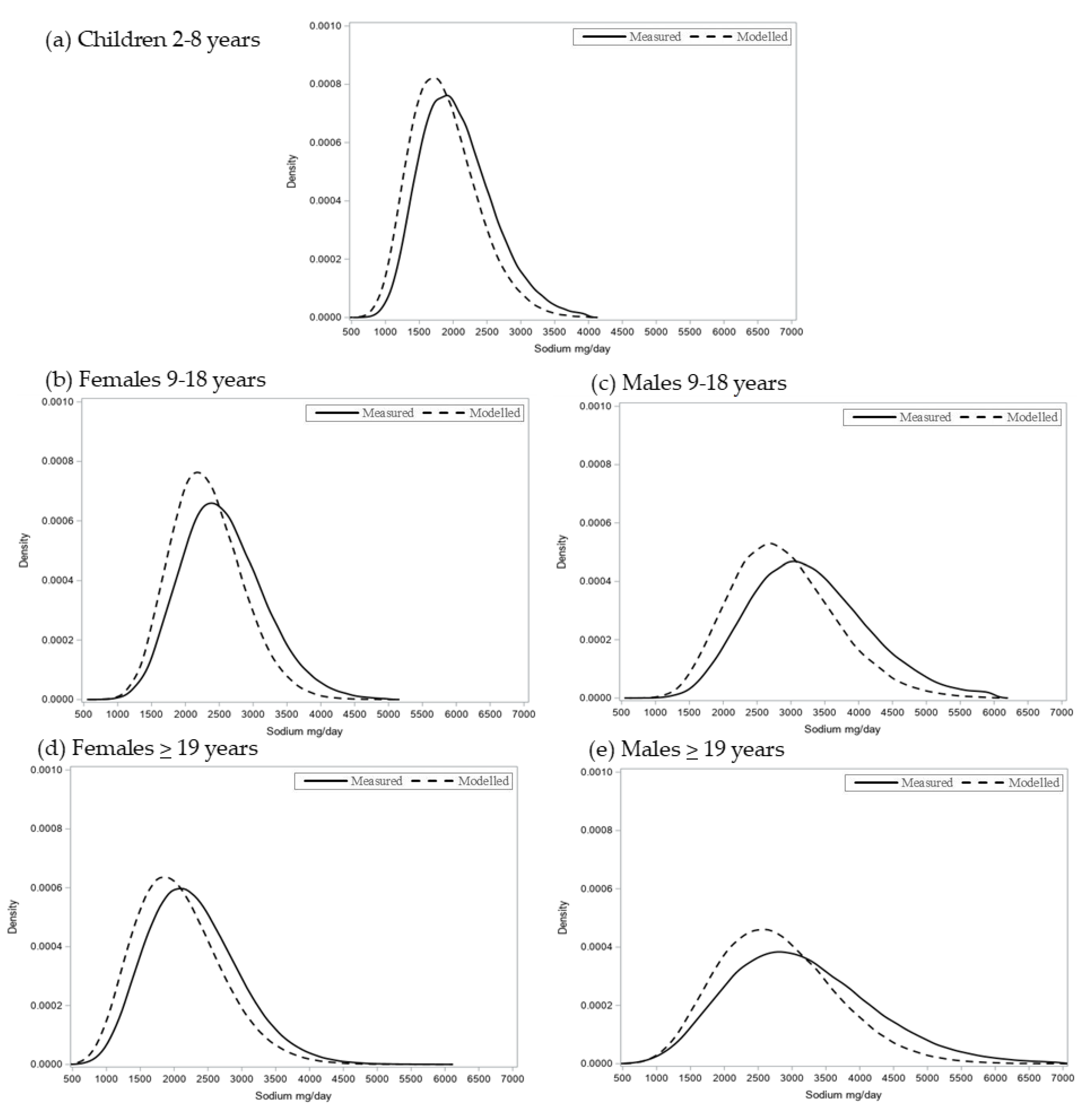
SRG Targets and Usual Sodium Intake Distributions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Global Burden of Disease Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Arcand, J.; Webster, J.; Johnson, C.; Raj, T.S.; Neal, B.; McLean, R.; Trieu, K.; Wong, M.M.; Leung, A.A.; Campbell, N.R. Announcing “Up to Date in the Science of Sodium”. J. Clin. Hypertens. 2016, 18, 85–88. [Google Scholar] [CrossRef]
- World Health Organization. A Comprehensive Global Monitoring Framework Including Indicators and a Set of Voluntary Global Targets for the Prevention and Control of Non-Communicable Diseases. 2012. Available online: http://www.who.int/nmh/events/2012/discussion_paper2_20120322.pdf. (accessed on 7 January 2021).
- World Health Organization. Global Status Report on Noncommunicable Diseases 2010. 2010. Available online: http://whqlibdoc.who.int/publications/2011/9789240686458_eng.pdf?ua=1 (accessed on 7 January 2021).
- Barberio, A.M.; Sumar, N.; Trieu, K.; Lorenzetti, D.L.; Tarasuk, V.; Webster, J.; Campbell, N.R.C.; McLaren, L. Population-level interventions in government jurisdictions for dietary sodium reduction: A Cochrane Review. Int. J. Epidemiol. 2017, 46, 1551. [Google Scholar] [CrossRef]
- Trieu, K.; Neal, B.; Hawkes, C.; Dunford, E.; Campbell, N.; Rodriguez-Fernandez, R.; Legetic, B.; McLaren, L.; Barberio, A.; Webster, J. Salt Reduction Initiatives around the World—A Systematic Review of Progress towards the Global Target. PLoS ONE 2015, 10, e0130247. [Google Scholar] [CrossRef] [PubMed]
- Santos, J.A.; Sparks, E.; Thout, S.R.; McKenzie, B.; Trieu, K.; Hoek, A.; Johnson, C.; McLean, R.; Arcand, J.; Campbell, N.R.C.; et al. The Science of Salt: A global review on changes in sodium levels in foods. J. Clin. Hypertens. 2019, 21, 1043–1056. [Google Scholar] [CrossRef] [PubMed]
- Health Canada. Sodium intake of Canadians in 2017; Health Canada: Ottawa, ON, Canada, 2017.
- The National Academies of Science Engineering Medicine. Dietary Reference Intakes for Sodium and Potassium (2019); The National Academic Press: Washington, DC, USA, 2019. [Google Scholar]
- Health Canada. Guidance for the Food Industry on Reducing Sodium in Processed Foods. In Bureau of Nutritional Sciences Food Directorate; Health Products and Food Branch, Ed.; Health Canada: Ottawa, ON, Canada, 2012. [Google Scholar]
- Health Canada. Sodium Reduction in Processed Foods in Canada: An Evaluation of Progress toward Voluntary Targets from 2012 to 2016; Health Canada: Ottawa, ON, Canada, 2018.
- Adams, J.; Mytton, O.; White, M.; Monsivais, P. Why Are Some Population Interventions for Diet and Obesity More Equitable and Effective Than Others? The Role of Individual Agency. PLoS Med. 2016, 13, e1001990. [Google Scholar]
- McLaren, L.; Heidinger, S.; Dutton, D.J.; Tarasuk, V.; Campbell, N.R. A repeated cross-sectional study of socio-economic inequities in dietary sodium consumption among Canadian adults: Implications for national sodium reduction strategies. Int. J. Equity Health 2014, 13, 44. [Google Scholar] [CrossRef] [PubMed]
- McGill, R.; Anwar, E.; Orton, L.; Bromley, H.; Lloyd-Williams, F.; O’Flaherty, M.; Taylor-Robinson, D.; Guzman-Castillo, M.; Gillespie, D.; Moreira, P.; et al. Are interventions to promote healthy eating equally effective for all? Systematic review of socioeconomic inequalities in impact. BMC Public Health 2015, 15, 457. [Google Scholar]
- Gillespie, D.O.; Allen, K.; Guzman-Castillo, M.; Bandosz, P.; Moreira, P.; McGill, R.; Anwar, E.; Lloyd-Williams, F.; Bromley, H.; Diggle, P.J.; et al. The Health Equity and Effectiveness of Policy Options to Reduce Dietary Salt Intake in England: Policy Forecast. PLoS ONE 2015, 10, e0127927. [Google Scholar]
- Center for Science in the Public Interest. International Action on Salt; Center for Science in the Public Interest: Washington, DC, USA, 2016. [Google Scholar]
- Collins, M.; Mason, H.; O’Flaherty, M.; Guzman-Castillo, M.; Critchley, J.; Capewell, S. An economic evaluation of salt reduction policies to reduce coronary heart disease in England: A policy modeling study. Value Health 2014, 17, 517–524. [Google Scholar] [CrossRef]
- Hyseni, L.; Elliot-Green, A.; Lloyd-Williams, F.; Kypridemos, C.; O’Flaherty, M.; McGill, R.; Orton, L.; Bromley, H.; Cappuccio, F.P.; Capewell, S. Systematic review of dietary salt reduction policies: Evidence for an effectiveness hierarchy? PLoS ONE 2017, 12, e0177535. [Google Scholar] [CrossRef]
- Pearson-Stuttard, J.; Kypridemos, C.; Collins, B.; Mozaffarian, D.; Huang, Y.; Bandosz, P.; Capewell, S.; Whitsel, L.; Wilde, P.; O’Flaherty, M.; et al. Estimating the health and economic effects of the proposed US Food and Drug Administration voluntary sodium reformulation: Microsimulation cost-effectiveness analysis. PLoS Med. 2018, 15, e1002551. [Google Scholar] [CrossRef]
- De Mestral, C.; Mayen, A.L.P.D.; Marques-Vidal, P.; Bochud, M.; Stringhini, S. Socioeconomic Determinants of Sodium Intake in Adult Populations of High-Income Countries: A Systematic Review and Meta-Analysis. Am. J. Public. Health 2017, 107, e1–e12. [Google Scholar] [CrossRef] [PubMed]
- Tugwell, P.; de Savigny, D.; Hawker, G.; Robinson, V. Applying clinical epidemiological methods to health equity: The equity effectiveness loop. BMJ 2006, 332, 358–361. [Google Scholar] [CrossRef] [PubMed]
- Health Canada. 2015 Canadian Community Health Survey (CCHS)—Nutrition User Guide; Government of Canada: Ottawa, ON, Canada, 2017.
- Health Canada. Canadian Community Health Survey, Cycle 2.2, Nutrition (2004): Income-Related Household Food Security in Canada; Health Canada: Ottawa, ON, Canada, 2008.
- Jessri, M.; Lou, W.Y.; L’Abbe, M.R. Evaluation of different methods to handle misreporting in obesity research: Evidence from the Canadian national nutrition survey. Br. J. Nutr. 2016, 115, 147–159. [Google Scholar] [CrossRef]
- McCrory, M.A.H.C.; Roberts, S.B. Procedures for screening out inaccurate reports of dietary energy intake. Public Health Nutr. 2002, 5, 873–882. [Google Scholar] [CrossRef] [PubMed]
- Hack, S.; Jessri, M.; L’Abbe, M.R. Evaluating Diet Quality of Canadian Adults Using Health Canada’s Surveillance Tool Tier System: Findings from the 2015 Canadian Community Health Survey-Nutrition. Nutrients 2020, 12, 1113. [Google Scholar] [CrossRef]
- National Cancer Institute. Usual Dietary Intakes: SAS Macros for the NCI Method; National Cancer Institute: Bethesda, MA, USA. Available online: https://epi.grants.cancer.gov/diet/usualintakes/macros.html (accessed on 7 January 2019).
- Kirkpatrick, S.I.; Tarasuk, V. Food insecurity is associated with nutrient inadequacies among Canadian adults and adolescents. J. Nutr. 2008, 138, 604–612. [Google Scholar] [CrossRef]
- Krieger, N.; Williams, D.R.; Moss, N.E. Measuring social class in US public health research: Concepts, methodologies, and guidelines. Annu. Rev. Public Health 1997, 18, 341–378. [Google Scholar] [CrossRef] [PubMed]
- Dachner, N.; Ricciuto, L.; Kirkpatrick, S.I.; Tarasuk, V. Food purchasing and food insecurity among low-income families in Toronto. Can. J. Diet. Pract. Res. 2010, 71, e50–e56. [Google Scholar]
- Health Canada. Consultation Report: Restricting Marketing of Unhealthy Food and Beverages to Children in Canada; Health Canada: Ottawa, ON, Canada, 2017.
- Cogswell, M.E.; Patel, S.M.; Yuan, K.; Gillespie, C.; Juan, W.; Curtis, C.J.; Vigneault, M.; Clapp, J.; Roach, P.; Moshfegh, A.; et al. Modeled changes in US sodium intake from reducing sodium concentrations of commercially processed and prepared foods to meet voluntary standards established in North America: NHANES. Am. J. Clin. Nutr. 2017, 106, 530–540. [Google Scholar] [CrossRef] [PubMed]
- Lucko, A.M.; Doktorchik, C.; Woodward, M.; Cogswell, M.; Neal, B.; Rabi, D.; Anderson, C.; He, F.J.; MacGregor, G.A.; L’Abbe, M.; et al. Percentage of ingested sodium excreted in 24-hour urine collections: A systematic review and meta-analysis. J. Clin. Hypertens. 2018, 20, 1220–1229. [Google Scholar] [CrossRef] [PubMed]
| 2 to 18 Years | ≥19 Years | |||
|---|---|---|---|---|
| Sodium (mg/day) | Sodium (mg/day) | |||
| n | Mean (95% CI) (95% CI) | n | Mean (95% CI) (95% CI) | |
| Sex | ||||
| Males | 3072 | 2820 (2730, 2910) | 6414 | 3179 (3088, 3269) |
| Females | 3054 | 2324 (2253, 2394) | 7105 | 2295 (2238, 2352) |
| Dietary Reference Intake Groups | ||||
| Male and Female | ||||
| 2–3 years | 948 | 1750 (1634, 1865) | ||
| 4–8 years | 1223 | 2287 (2197, 2378) | ||
| Males | ||||
| 9–13 years | 1044 | 2937 (2807, 3067) | ||
| 14–18 years | 934 | 3520 (3327, 3713) | ||
| 19–30 years | 881 | 3560 (3300, 3821) | ||
| 31–50 years | 2070 | 3264 (3098, 3430) | ||
| 51–70 years | 2227 | 3046 (2919, 3174) | ||
| ≥71 years | 1236 | 2649 (2533, 2765) | ||
| Females | ||||
| 9–13 years | 966 | 2582 (2468, 2695) | ||
| 14–18 years | 1011 | 2498 (2353, 2644) | ||
| 19–30 years | 892 | 2387 (2185, 2588) | ||
| 31–50 years | 2273 | 2419 (2315, 2523) | ||
| 51–70 years | 2405 | 2194 (2121, 2267) | ||
| ≥71 years | 1535 | 2100 (2013, 2186) | ||
| Household Education | ||||
| Less than high school | 190 | 2738 (2391, 3085) | 1556 | 2670 (2502, 2838) |
| High school only | 939 | 2575 (2443, 2707) | 2722 | 2720 (2597, 2843) |
| Trade, college, etc. | 2458 | 2670 (2571, 2769) | 4932 | 2810 (2710, 2911) |
| Bachelor degree, etc. | 2539 | 2477 (2390, 2563) | 4309 | 2685 (2596, 2775) |
| Income | ||||
| Quintile 1 | 1190 | 2499 (2379, 2618) | 2829 | 2566 (2406, 2726) |
| Quintile 2 | 1158 | 2509 (2397, 2621) | 2870 | 2632 (2528, 2736) |
| Quintile 3 | 1407 | 2644 (2510, 2778) | 2866 | 2800 (2692, 2908) |
| Quintile 4 | 1271 | 2496 (2366, 2625) | 2381 | 2758 (2636, 2879) |
| Quintile 5 | 1100 | 2764 (2601, 2926) | 2573 | 2916 (2784, 3049) |
| Food security | ||||
| Food insecure | 772 | 2753 (2531, 2976) | 1270 | 2679 (2484, 2873) |
| Food secure | 5354 | 2551 (2491, 2611) | 12,249 | 2742 (2683, 2801) |
| Misreporting | ||||
| Under reporter | 1144 | 1828 (1724, 1933) | 4374 | 1842 (1786, 1898) |
| Plausible reporter | 2530 | 2724 (2653, 2796) | 6551 | 3050 (2980, 3120) |
| Over reporter | 671 | 3658 (3478, 3838) | 846 | 4898 (4649, 5146) |
| Unclassified | 1781 | 2367 (2254, 2480) | 1748 | 2727 (2565, 2889) |
| Energy intake | ||||
| Males (kcal/day) | 3072 | 1995 (1943, 2046) | 6414 | 2173 (2123, 2223) |
| Females (kcal/day) | 3054 | 1674 (1626, 1721) | 7105 | 1590 (1559, 1621) |
| Measured Sodium Intake (mg/day) | Modelled Sodium Intake (mg/day) | |||
|---|---|---|---|---|
| Mean (95% CI) | Difference (95% CI) | Mean (95% CI) | Difference (95% CI) | |
| Household Education | ||||
| Less than high school | 2379 (1822, 2936) | 358 (−201, 916) | 1959 (1685, 2233) | 72 (−204, 347) |
| High school only | 2233 (2034, 2432) | 212 (5, 419) | 1949 (1843, 2055) | 61 (−48, 171) |
| Trade, college, etc. | 2126 (2045, 2208) | 105 (9, 201) | 1904 (1818, 1990) | 16 (−74, 106) |
| Bachelor degree, etc. | 2021 (1948, 2095) | Ref. | 1888 (1831, 1944) | Ref. |
| Income | ||||
| Quintile 1 | 2151 (2026, 2276) | 170 (−1, 342) | 1914 (1826, 2002) | 49 (−77, 175) |
| Quintile 2 | 2070 (1949, 2192) | 90 (−68, 249) | 1952 (1844, 2061) | 87 (−49, 224) |
| Quintile 3 | 2132 (2015, 2249) | 151 (3, 299) | 1917 (1822, 2011) | 52 (−71, 174) |
| Quintile 4 | 2060 (1981, 2140) | 80 (−54, 214) | 1842 (1774, 1911) | −23 (−141, 96) |
| Quintile 5 | 1980 (1863, 2098) | Ref. | 1865 (1767, 1963) | Ref. |
| Food Security | ||||
| Food insecure | 2335 (2140, 2531) | 271 (75, 468) | 1976 (1851, 2102) | 83 (−45, 212) |
| Food secure | 2064 (2004, 2124) | Ref. | 1893 (1837, 1949) | Ref. |
| Males | Females | |||||||
|---|---|---|---|---|---|---|---|---|
| Measured Sodium Intake (mg/day) | Modelled Sodium Intake (mg/day) | Measured Sodium Intake (mg/day) | Modelled Sodium Intake (mg/day) | |||||
| Mean (95% CI) | Difference (95% CI) | Mean (95% CI) | Difference (95% CI) | Mean (95% CI) | Difference (95% CI) | Mean (95% CI) | Difference 95% CI) | |
| 9–18 Years | ||||||||
| Household Education | ||||||||
| Less than high school | 3249 (2949, 3550) | 148 (−161, 456) | 2562 (2272, 2853) | −211 (−509, 87) | 2740 (2498, 2981) | 246 (−1, 493) | 2442 (2202, 2682) | 96 (−149, 341) |
| High school only | 3115 (2939, 3290) | 13 (−175, 201) | 2785 (2643, 2926) | 12 (−129, 152) | 2523 (2394, 2652) | 29 (−127, 185) | 2256 (2146, 2365) | −90 (−227, 46) |
| Trade, college, etc. | 3223 (3084, 3362) | 121 (−34, 277) | 2780 (2655, 2905) | 7 (118, 131) | 2535 (2430, 2641) | 41 (−86, 169) | 2250 (2156, 2344) | −96 (−216, 24) |
| Bachelor degree, etc. | 3102 (2974, 3229) | Ref. | 2773 (2651, 2896) | Ref. | 2494 (2387, 2601) | Ref. | 2346 (2243, 2449) | Ref. |
| Income | ||||||||
| Quintile 1 | 3052 (2892, 3211) | −224 (−442, −5) | 2718 (2573, 2863) | −56 (−244, 133) | 2521 (2378, 2663) | 15 (−172, 201) | 2366 (2238, 2495) | 104 (−63, 271) |
| Quintile 2 | 3069 (2923, 3214) | −207 (−423, 10) | 2814 (2666, 2962) | 41 (−159, 240) | 2617 (2464, 2771) | 111 (−90, 312) | 2375 (2232, 2519) | 113 (−79, 304) |
| Quintile 3 | 3262 (3105, 3419) | −14 (−245, 217) | 2803 (2679, 2928) | 30 (153, 213) | 2532 (2403, 2660) | 26 (−143, 194) | 2267 (2153, 2382) | 5 (−149, 159) |
| Quintile 4 | 3118 (2947, 3290) | −157 (−391, 78) | 2731 (2550, 2912) | −43 (−245 160) | 2421 (2312, 2530) | −85 (−249, 79) | 2185 (2078, 2292) | −78 (−238, 83) |
| Quintile 5 | 3275 (3078, 3472) | Ref. | 2773 (2600, 2947) | Ref. | 2506 (2370, 2643) | Ref. | 2262 (2129, 2396) | Ref. |
| Food Security | ||||||||
| Food insecure | 3138 (2937, 3339) | −19 (−227, 189) | 2711 (2547, 2875) | −66 (−232, 100) | 2636 (2469, 2803) | 122 (−52, 296) | 2295 (2153, 2436) | −4 (−149, 140) |
| Food secure | 3157 (3052, 3263) | Ref. | 2777 (2670, 2883) | Ref. | 2514 (2434, 2593) | Ref. | 2299 (2224, 2374) | Ref. |
| ≥19 Years | ||||||||
| Household Education | ||||||||
| Less than high school | 3400 (3186, 3614) | 399 (172, 626) | 2918 (2748, 3087) | 148 (−30, 327) | 2412 (2306, 2517) | 122 (6, 239) | 2067 (1981, 2152) | −45 (−141, 51) |
| High school only | 3177 (3045, 3309) | 176 (26, 325) | 2751 (2641, 2861) | −18 (−143, 107) | 2358 (2266, 2451) | 69 (−42,180) | 2110 (2032, 2188) | −2 (−97, 94) |
| Trade, college, etc. | 3076 (2969, 3184) | 75 (−51, 201) | 2745 (2654, 2837) | −24 (−130, 82) | 2353 (2273, 2433) | 64 (−38, 166) | 2119 (2047, 2191) | 7 (−81, 94) |
| Bachelor degree, etc. | 3001 (2876, 3126) | Ref. | 2769 (2660, 2878) | Ref. | 2289 (2199, 2380) | Ref. | 2112 (2035, 2188) | Ref. |
| Income | ||||||||
| Quintile 1 | 3113 (2933, 3293) | 82 (−126, 290) | 2811 (2667, 2954) | 126 (−40, 292) | 2305 (2206, 2404) | −41 (−184, 103) | 2105 (2021, 2189) | 21 (−111, 154) |
| Quintile 2 | 3083 (2949, 3217) | 52 (−118, 222) | 2781 (2668, 2893) | 96 (−49, 241) | 2313 (2225, 2401) | −33 (−171, 106) | 2110 (2034, 2185) | 26 (−95, 146) |
| Quintile 3 | 3129 (2999, 3259) | 98 (−56, 252) | 2814 (2708, 2919) | 129 (−2, 260) | 2411 (2312, 2509) | 65 (−82, 211) | 2153 (2072, 2234) | 70 (−57, 195) |
| Quintile 4 | 3120 (2984, 3256) | 89 (−74, 251) | 2770 (2651, 2889) | 86 (−56, 227) | 2321 (2220, 2423) | −25 (−182, 133) | 2092 (2007, 2177) | 8 (−131, 147) |
| Quintile 5 | 3031 (2887, 3175) | Ref. | 2685 (2555, 2814) | Ref. | 2346 (2222, 2470) | Ref. | 2084 (1969, 2199) | Ref. |
| Food Security | ||||||||
| Food insecure | 3137 (2910, 3365) | 48 (−186, 282) | 2596 (2423, 2770) | −188 (−365, −11) | 2276 (2168, 2385) | −67 (−172, 38) | 2007 (1912, 2101) | −112 (−206, −18) |
| Food secure | 3089 (2996, 3182) | Ref. | 2784 (2703, 2865) | Ref. | 2343 (2280, 2406) | Ref. | 2119 (2064, 2175) | Ref. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smith, B.T.; Hack, S.; Jessri, M.; Arcand, J.; McLaren, L.; L’Abbé, M.R.; Anderson, L.N.; Hobin, E.; Hammond, D.; Manson, H.; et al. The Equity and Effectiveness of Achieving Canada’s Voluntary Sodium Reduction Guidance Targets: A Modelling Study Using the 2015 Canadian Community Health Survey—Nutrition. Nutrients 2021, 13, 779. https://doi.org/10.3390/nu13030779
Smith BT, Hack S, Jessri M, Arcand J, McLaren L, L’Abbé MR, Anderson LN, Hobin E, Hammond D, Manson H, et al. The Equity and Effectiveness of Achieving Canada’s Voluntary Sodium Reduction Guidance Targets: A Modelling Study Using the 2015 Canadian Community Health Survey—Nutrition. Nutrients. 2021; 13(3):779. https://doi.org/10.3390/nu13030779
Chicago/Turabian StyleSmith, Brendan T., Salma Hack, Mahsa Jessri, JoAnne Arcand, Lindsay McLaren, Mary R. L’Abbé, Laura N. Anderson, Erin Hobin, David Hammond, Heather Manson, and et al. 2021. "The Equity and Effectiveness of Achieving Canada’s Voluntary Sodium Reduction Guidance Targets: A Modelling Study Using the 2015 Canadian Community Health Survey—Nutrition" Nutrients 13, no. 3: 779. https://doi.org/10.3390/nu13030779
APA StyleSmith, B. T., Hack, S., Jessri, M., Arcand, J., McLaren, L., L’Abbé, M. R., Anderson, L. N., Hobin, E., Hammond, D., Manson, H., Rosella, L. C., & Manuel, D. G. (2021). The Equity and Effectiveness of Achieving Canada’s Voluntary Sodium Reduction Guidance Targets: A Modelling Study Using the 2015 Canadian Community Health Survey—Nutrition. Nutrients, 13(3), 779. https://doi.org/10.3390/nu13030779








