Relationship between Persistent Gastrointestinal Symptoms and Duodenal Histological Findings after Adequate Gluten-Free Diet: A Gray Area of Celiac Disease Management in Adult Patients
Abstract
1. Introduction
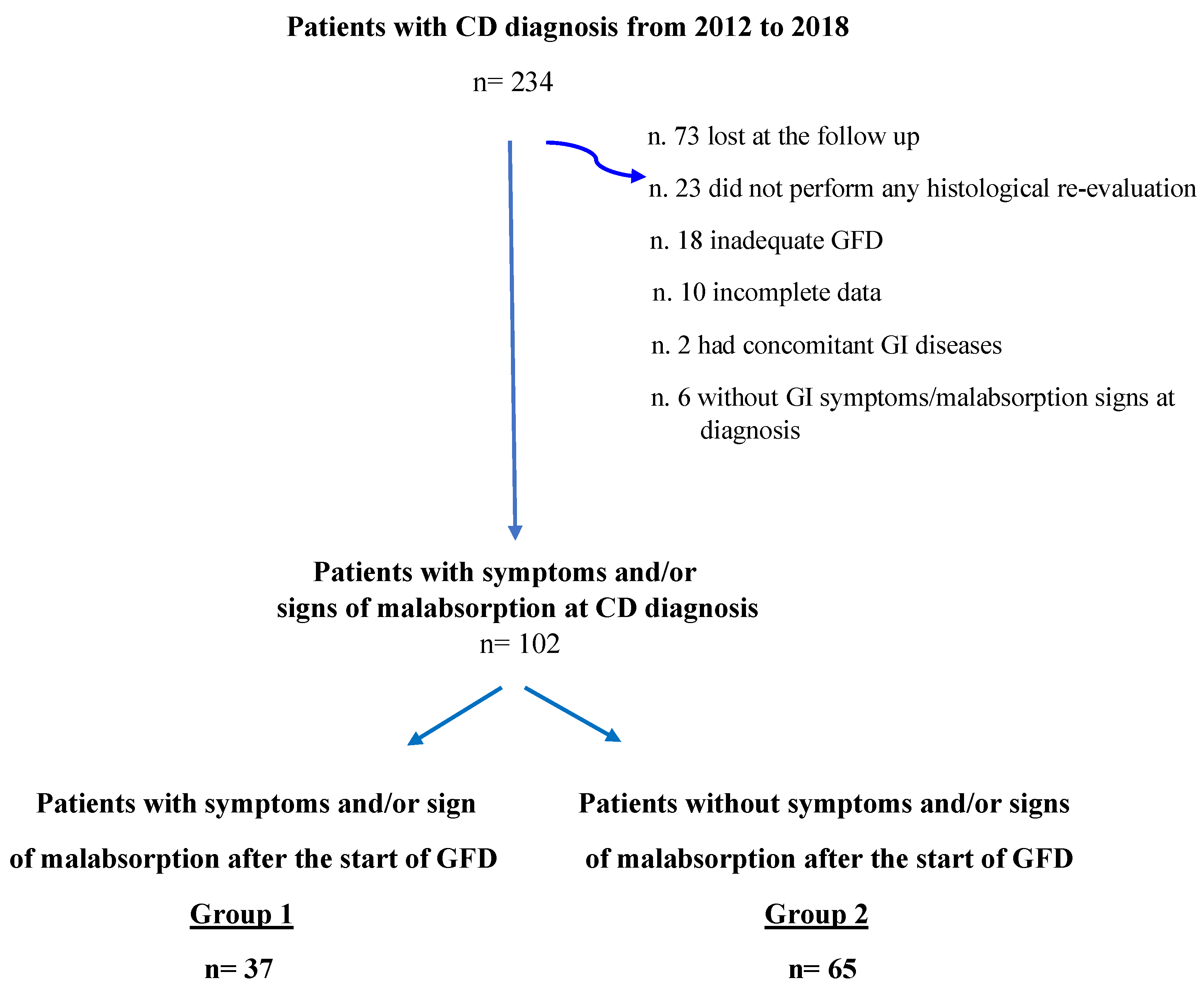
2. Materials and Methods
2.1. Endoscopic Procedures and Histological Classification
2.2. Serological Assays
2.3. GI Symptoms and GFD Assessment
2.4. Statistical Analyses
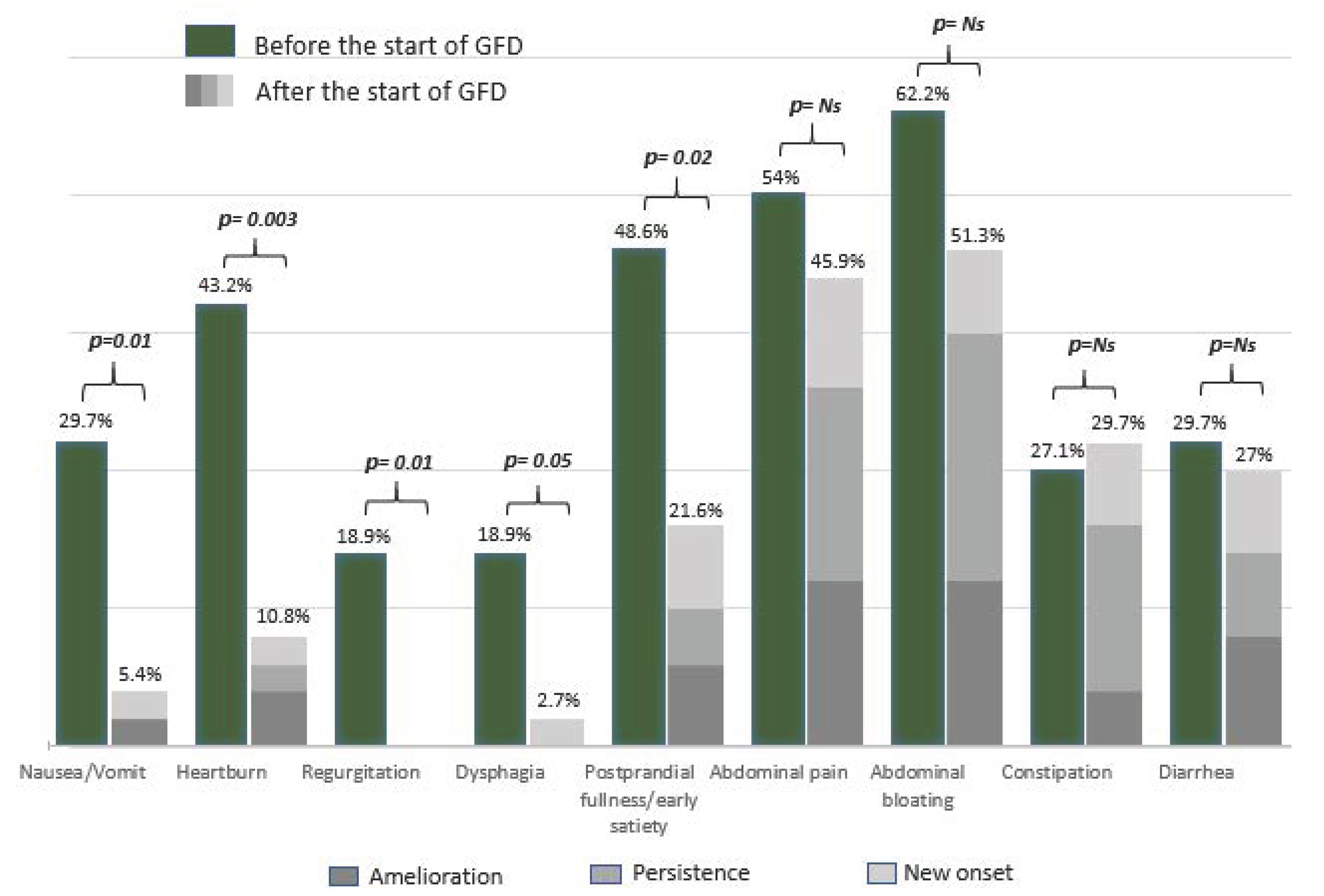
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al-Toma, A.; Volta, U.; Auricchio, R.; Castillejo, G.; Sanders, D.S.; Cellier, C.; Mulder, C.J.; Lundin, K.E.A. European Society for the Study of Coeliac Disease (ESsCD) Guideline for Coeliac Disease and Other Gluten-Related Disorders. United Eur. Gastroenterol. J. 2019, 7, 583–613. [Google Scholar] [CrossRef] [PubMed]
- Lebwohl, B.; Sanders, D.S.; Green, P.H.R. Coeliac Disease. Lancet Lond. Engl. 2018, 391, 70–81. [Google Scholar] [CrossRef]
- Fasano, A.; Catassi, C. Clinical Practice. Celiac Disease. N. Engl. J. Med. 2012, 367, 2419–2426. [Google Scholar] [CrossRef]
- Lee, S.K.; Lo, W.; Memeo, L.; Rotterdam, H.; Green, P.H.R. Duodenal Histology in Patients with Celiac Disease after Treatment with a Gluten-Free Diet. Gastrointest. Endosc. 2003, 57, 187–191. [Google Scholar] [CrossRef]
- Abdulkarim, A.S.; Burgart, L.J.; See, J.; Murray, J.A. Etiology of Nonresponsive Celiac Disease: Results of a Systematic Approach. Am. J. Gastroenterol. 2002, 97, 2016–2021. [Google Scholar] [CrossRef]
- Stasi, E.; Marafini, I.; Caruso, R.; Soderino, F.; Angelucci, E.; Del Vecchio Blanco, G.; Paoluzi, O.A.; Calabrese, E.; Sedda, S.; Zorzi, F.; et al. Frequency and Cause of Persistent Symptoms in Celiac Disease Patients on a Long-Term Gluten-Free Diet. J. Clin. Gastroenterol. 2016, 50, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Murray, J.A.; Watson, T.; Clearman, B.; Mitros, F. Effect of a Gluten-Free Diet on Gastrointestinal Symptoms in Celiac Disease. Am. J. Clin. Nutr. 2004, 79, 669–673. [Google Scholar] [CrossRef] [PubMed]
- Wahab, P.J.; Meijer, J.W.R.; Mulder, C.J.J. Histologic Follow-up of People with Celiac Disease on a Gluten-Free Diet: Slow and Incomplete Recovery. Am. J. Clin. Pathol. 2002, 118, 459–463. [Google Scholar] [CrossRef] [PubMed]
- O’Mahony, S.; Howdle, P.D.; Losowsky, M.S. Review Article: Management of Patients with Non-Responsive Coeliac Disease. Aliment. Pharmacol. Ther. 1996, 10, 671–680. [Google Scholar] [CrossRef] [PubMed]
- Hill, P.; Austin, A.; Forsyth, J.; Holmes, G. British Society of Gastroenterology Guidelines on the Diagnosis and Management of Coeliac Disease. Gut 2015, 64, 691–692. [Google Scholar] [CrossRef]
- Mahadev, S.; Murray, J.A.; Wu, T.-T.; Chandan, V.S.; Torbenson, M.S.; Kelly, C.P.; Maki, M.; Green, P.H.R.; Adelman, D.; Lebwohl, B. Factors Associated with Villus Atrophy in Symptomatic Coeliac Disease Patients on a Gluten-Free Diet. Aliment. Pharmacol. Ther. 2017, 45, 1084–1093. [Google Scholar] [CrossRef]
- Bardella, M.T.; Velio, P.; Cesana, B.M.; Prampolini, L.; Casella, G.; Di Bella, C.; Lanzini, A.; Gambarotti, M.; Bassotti, G.; Villanacci, V. Coeliac Disease: A Histological Follow-up Study. Histopathology 2007, 50, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Kaukinen, K.; Peräaho, M.; Lindfors, K.; Partanen, J.; Woolley, N.; Pikkarainen, P.; Karvonen, A.-L.; Laasanen, T.; Sievänen, H.; Mäki, M.; et al. Persistent Small Bowel Mucosal Villous Atrophy without Symptoms in Coeliac Disease. Aliment. Pharmacol. Ther. 2007, 25, 1237–1245. [Google Scholar] [CrossRef]
- Lanzini, A.; Lanzarotto, F.; Villanacci, V.; Mora, A.; Bertolazzi, S.; Turini, D.; Carella, G.; Malagoli, A.; Ferrante, G.; Cesana, B.M.; et al. Complete Recovery of Intestinal Mucosa Occurs Very Rarely in Adult Coeliac Patients despite Adherence to Gluten-Free Diet. Aliment. Pharmacol. Ther. 2009, 29, 1299–1308. [Google Scholar] [CrossRef] [PubMed]
- Collin, P.; Mäki, M.; Kaukinen, K. Complete Small Intestine Mucosal Recovery Is Obtainable in the Treatment of Celiac Disease. Gastrointest. Endosc. 2004, 59, 158–159, author reply in 159–160. [Google Scholar] [CrossRef]
- Galli, G.; Esposito, G.; Lahner, E.; Pilozzi, E.; Corleto, V.D.; Di Giulio, E.; Aloe Spiriti, M.A.; Annibale, B. Histological Recovery and Gluten-Free Diet Adherence: A Prospective 1-Year Follow-up Study of Adult Patients with Coeliac Disease. Aliment. Pharmacol. Ther. 2014, 40, 639–647. [Google Scholar] [CrossRef]
- Pekki, H.; Kurppa, K.; Mäki, M.; Huhtala, H.; Sievänen, H.; Laurila, K.; Collin, P.; Kaukinen, K. Predictors and Significance of Incomplete Mucosal Recovery in Celiac Disease After 1 Year on a Gluten-Free Diet. Am. J. Gastroenterol. 2015, 110, 1078–1085. [Google Scholar] [CrossRef] [PubMed]
- Malamut, G.; Cellier, C. Refractory Celiac Disease. Gastroenterol. Clin. North Am. 2019, 48, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Pekki, H.; Kurppa, K.; Mäki, M.; Huhtala, H.; Laurila, K.; Ilus, T.; Kaukinen, K. Performing Routine Follow-up Biopsy 1 Year after Diagnosis Does Not Affect Long-Term Outcomes in Coeliac Disease. Aliment. Pharmacol. Ther. 2017, 45, 1459–1468. [Google Scholar] [CrossRef] [PubMed]
- Marsh, M.N. Gluten, Major Histocompatibility Complex, and the Small Intestine. A Molecular and Immunobiologic Approach to the Spectrum of Gluten Sensitivity (‘celiac Sprue’). Gastroenterology 1992, 102, 330–354. [Google Scholar] [CrossRef]
- Biagi, F.; Andrealli, A.; Bianchi, P.I.; Marchese, A.; Klersy, C.; Corazza, G.R. A Gluten-Free Diet Score to Evaluate Dietary Compliance in Patients with Coeliac Disease. Br. J. Nutr. 2009, 102, 882–887. [Google Scholar] [CrossRef] [PubMed]
- Oberhuber, G.; Granditsch, G.; Vogelsang, H. The Histopathology of Coeliac Disease: Time for a Standardized Report Scheme for Pathologists. Eur. J. Gastroenterol. Hepatol. 1999, 11, 1185–1194. [Google Scholar] [CrossRef]
- Dixon, M.F.; Genta, R.M.; Yardley, J.H.; Correa, P. Classification and Grading of Gastritis. The Updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am. J. Surg. Pathol. 1996, 20, 1161–1181. [Google Scholar] [CrossRef]
- Carabotti, M.; Lahner, E.; Esposito, G.; Sacchi, M.C.; Severi, C.; Annibale, B. Upper Gastrointestinal Symptoms in Autoimmune Gastritis: A Cross-Sectional Study. Medicine (Baltimore) 2017, 96, e5784. [Google Scholar] [CrossRef] [PubMed]
- Lewis, S.J.; Heaton, K.W. Stool Form Scale as a Useful Guide to Intestinal Transit Time. Scand. J. Gastroenterol. 1997, 32, 920–924. [Google Scholar] [CrossRef]
- Vakil, N.; van Zanten, S.V.; Kahrilas, P.; Dent, J.; Jones, R.; Global Consensus Group. The Montreal Definition and Classification of Gastroesophageal Reflux Disease: A Global Evidence-Based Consensus. Am. J. Gastroenterol. 2006, 101, 1900–1920. [Google Scholar] [CrossRef] [PubMed]
- Mearin, F.; Lacy, B.E.; Chang, L.; Chey, W.D.; Lembo, A.J.; Simren, M.; Spiller, R. Bowel Disorders. Gastroenterology 2016. [Google Scholar] [CrossRef]
- Dewar, D.H.; Donnelly, S.C.; McLaughlin, S.D.; Johnson, M.W.; Ellis, H.J.; Ciclitira, P.J. Celiac Disease: Management of Persistent Symptoms in Patients on a Gluten-Free Diet. World J. Gastroenterol. 2012, 18, 1348–1356. [Google Scholar] [CrossRef] [PubMed]
- Comino, I.; Fernández-Bañares, F.; Esteve, M.; Ortigosa, L.; Castillejo, G.; Fambuena, B.; Ribes-Koninckx, C.; Sierra, C.; Rodríguez-Herrera, A.; Salazar, J.C.; et al. Fecal Gluten Peptides Reveal Limitations of Serological Tests and Food Questionnaires for Monitoring Gluten-Free Diet in Celiac Disease Patients. Am. J. Gastroenterol. 2016, 111, 1456–1465. [Google Scholar] [CrossRef] [PubMed]
- Elli, L.; Bascuñán, K.; di Lernia, L.; Bardella, M.T.; Doneda, L.; Soldati, L.; Orlando, S.; Ferretti, F.; Lombardo, V.; Barigelletti, G.; et al. Safety of Occasional Ingestion of Gluten in Patients with Celiac Disease: A Real-Life Study. BMC Med. 2020, 18, 42. [Google Scholar] [CrossRef] [PubMed]
- Elli, L.; Villalta, D.; Roncoroni, L.; Barisani, D.; Ferrero, S.; Pellegrini, N.; Bardella, M.T.; Valiante, F.; Tomba, C.; Carroccio, A.; et al. Nomenclature and Diagnosis of Gluten-Related Disorders: A Position Statement by the Italian Association of Hospital Gastroenterologists and Endoscopists (AIGO). Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2017, 49, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Carroccio, A.; Ambrosiano, G.; Di Prima, L.; Pirrone, G.; Iacono, G.; Florena, A.M.; Porcasi, R.; Noto, D.; Fayer, F.; Soresi, M.; et al. Clinical Symptoms in Celiac Patients on a Gluten-Free Diet. Scand. J. Gastroenterol. 2008, 43, 1315–1321. [Google Scholar] [CrossRef] [PubMed]
- Elli, L.; Zini, E.; Tomba, C.; Bardella, M.T.; Bosari, S.; Conte, D.; Runza, L.; Roncoroni, L.; Ferrero, S. Histological Evaluation of Duodenal Biopsies from Coeliac Patients: The Need for Different Grading Criteria during Follow-Up. BMC Gastroenterol. 2015, 15, 133. [Google Scholar] [CrossRef]
- Tan, I.L.; Withoff, S.; Kolkman, J.J.; Wijmenga, C.; Weersma, R.K.; Visschedijk, M.C. Non-Classical Clinical Presentation at Diagnosis by Male Celiac Disease Patients of Older Age. Eur. J. Intern. Med. 2020. [Google Scholar] [CrossRef]
- Corrao, G.; Corazza, G.R.; Bagnardi, V.; Brusco, G.; Ciacci, C.; Cottone, M.; Sategna Guidetti, C.; Usai, P.; Cesari, P.; Pelli, M.A.; et al. Mortality in Patients with Coeliac Disease and Their Relatives: A Cohort Study. Lancet Lond. Engl. 2001, 358, 356–361. [Google Scholar] [CrossRef]
- Green, P.H.R.; Stavropoulos, S.N.; Panagi, S.G.; Goldstein, S.L.; Mcmahon, D.J.; Absan, H.; Neugut, A.I. Characteristics of Adult Celiac Disease in the USA: Results of a National Survey. Am. J. Gastroenterol. 2001, 96, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, J.F.; Leffler, D.A.; Bai, J.C.; Biagi, F.; Fasano, A.; Green, P.H.R.; Hadjivassiliou, M.; Kaukinen, K.; Kelly, C.P.; Leonard, J.N.; et al. The Oslo Definitions for Coeliac Disease and Related Terms. Gut 2013, 62, 43–52. [Google Scholar] [CrossRef]
- Melini, V.; Melini, F. Gluten-Free Diet: Gaps and Needs for a Healthier Diet. Nutrients 2019, 11, 170. [Google Scholar] [CrossRef] [PubMed]
- Sanz, Y. Effects of a Gluten-Free Diet on Gut Microbiota and Immune Function in Healthy Adult Humans. Gut Microbes 2010, 1, 135–137. [Google Scholar] [CrossRef]
- Laurikka, P.; Salmi, T.; Collin, P.; Huhtala, H.; Mäki, M.; Kaukinen, K.; Kurppa, K. Gastrointestinal Symptoms in Celiac Disease Patients on a Long-Term Gluten-Free Diet. Nutrients 2016, 8, 429. [Google Scholar] [CrossRef]
- Bellini, M.; Tonarelli, S.; Mumolo, M.G.; Bronzini, F.; Pancetti, A.; Bertani, L.; Costa, F.; Ricchiuti, A.; de Bortoli, N.; Marchi, S.; et al. Low Fermentable Oligo- Di- and Mono-Saccharides and Polyols (FODMAPs) or Gluten Free Diet: What Is Best for Irritable Bowel Syndrome? Nutrients 2020, 12, 3368. [Google Scholar] [CrossRef] [PubMed]
- Roncoroni, L.; Elli, L.; Doneda, L.; Bascuñán, K.A.; Vecchi, M.; Morreale, F.; Scricciolo, A.; Lombardo, V.; Pellegrini, N. A Retrospective Study on Dietary FODMAP Intake in Celiac Patients Following a Gluten-Free Diet. Nutrients 2018, 10, 1769. [Google Scholar] [CrossRef] [PubMed]
- Usai-Satta, P.; Bassotti, G.; Bellini, M.; Oppia, F.; Lai, M.; Cabras, F. Irritable Bowel Syndrome and Gluten-Related Disorders. Nutrients 2020, 12, 1117. [Google Scholar] [CrossRef] [PubMed]
- Silvester, J.A.; Graff, L.A.; Rigaux, L.; Bernstein, C.N.; Leffler, D.A.; Kelly, C.P.; Walker, J.R.; Duerksen, D.R. Symptoms of Functional Intestinal Disorders Are Common in Patients with Celiac Disease Following Transition to a Gluten-Free Diet. Dig. Dis. Sci. 2017, 62, 2449–2454. [Google Scholar] [CrossRef]
- Besterman, H.S.; Bloom, S.R.; Sarson, D.L.; Blackburn, A.M.; Johnston, D.I.; Patel, H.R.; Stewart, J.S.; Modigliani, R.; Guerin, S.; Mallinson, C.N. Gut-Hormone Profile in Coeliac Disease. Lancet Lond. Engl. 1978, 1, 785–788. [Google Scholar] [CrossRef]
- Barbara, G.; Stanghellini, V.; De Giorgio, R.; Corinaldesi, R. Functional Gastrointestinal Disorders and Mast Cells: Implications for Therapy. Neurogastroenterol. Motil. Off. J. Eur. Gastrointest. Motil. Soc. 2006, 18, 6–17. [Google Scholar] [CrossRef]
- Galli, G.; Purchiaroni, F.; Lahner, E.; Sacchi, M.C.; Pilozzi, E.; Corleto, V.D.; Di Giulio, E.; Annibale, B. Time Trend Occurrence of Duodenal Intraepithelial Lymphocytosis and Celiac Disease in an Open Access Endoscopic Population. United Eur. Gastroenterol. J. 2017, 5, 811–818. [Google Scholar] [CrossRef]
- Marsilio, I.; Maddalo, G.; Ghisa, M.; Savarino, E.V.; Farinati, F.; Zingone, F. The Coeliac Stomach: A Review of the Literature. Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2020, 52, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Lebwohl, B.; Green, P.H.R.; Genta, R.M. The Coeliac Stomach: Gastritis in Patients with Coeliac Disease. Aliment. Pharmacol. Ther. 2015, 42, 180–187. [Google Scholar] [CrossRef] [PubMed]
| N (%) | Patients with Persistent Sign/Symptoms Group 1 n = 37 | Patients without Persistent Signs/Symptoms Group 2 n = 65 | p |
|---|---|---|---|
| Median age at diagnosis, yrs (range) | 41 (18–76) | 38 (18–66) | 0.245 |
| Female gender (%) | 28 (75.7) | 45 (69.2) | 0.648 |
| Median BMI * Kg/m2 (range) | 23.4 (17.5–31.8) | 21.1 (16–30.8) | 0.168 |
| Comorbidities | |||
| Autoimmune | 9 (24.3) | 17 (26.5) | 1 |
| Others # | 8 (18.8) | 13 (20.3) | 1 |
| Family history of CD § | 8 (21.6) | 8 (12.3) | 0.261 |
| ≥5 years of duration of symptoms/signs before CD diagnosis | 13 (39.4) | 10 (18.8) | 0.045 |
| H. pylori infection | 10 (27%) | 17 (26.1%) | 1 |
| Clinical presentation | |||
| Only GI ° symptoms | 8 (21.6) | 15 (23.1) | 0.807 |
| Only malabsorption signs | 5 (13.5) | 5 (7.7) | 0.498 |
| Both symptoms and signs | 24(64.8) | 45 (69.2) | 0.665 |
| GI symptoms | |||
| Total pts with GI symptoms | 32 (86.5) | 54 (83.1) | 0.780 |
| Nausea/vomiting | 11 (29.7) | 17 (26.1) | 0.817 |
| Heartburn | 16 (43.2) | 29 (44.6) | 1 |
| Regurgitation | 7 (18.9) | 14 (21.5) | 0.804 |
| Dysphagia | 7 (18.9) | 7 (10.7) | 0.369 |
| Postprandial fullness/early satiety | 18 (48.6) | 37 (56.9) | 0.535 |
| Abdominal pain | 20 (54) | 39 (60) | 0.677 |
| Abdominal bloating | 23 (62.2) | 48 (73.8) | 0.264 |
| Constipation | 10 (27.1) | 7 (10.8) | 0.051 |
| Diarrhea | 11 (29.7) | 16 (24.6) | 0.643 |
| Diarrhea | |||
| Signs of malabsorption | 29 (78.4) | 49 (75.4) | 0.811 |
| Marsh 3C at diagnosis | 17 (45.9) | 39 (60) | 0.215 |
| N (%) | Patients with Persistent Sign/Symptoms Group 1 n = 37 | Patients without Persistent Signs/Symptoms Group 2 n = 65 | p |
|---|---|---|---|
| Median months of GFD *(range) | 14 (12–28) | 18 (12–28) | 0.211 |
| Clinical presentation | |||
| Only GI § symptoms | 18 (48.7) | 0 | na # |
| Only malabsorption signs | 10 (27) | 0 | na |
| Both symptoms and signs | 9 (24.3) | 0 | na |
| Antibody positivity | 8 (21.6) | 15 (23.1) | 1 |
| H. pylori infection | 1 (2.7) | 4 (6.1) | 0.650 |
| Marsh score | |||
| Marsh 0 | 26 (70.3) | 39 (60) | 0.392 |
| Marsh 1 | 1 (2.7) | 11 (17) | 0.052 |
| Marsh 2 | 0 | 0 | na |
| Marsh 3A | 7 (18.9) | 14 (21.5) | 0.804 |
| Marsh 3B | 2 (5.4) | 1 (1.5) | 0.290 |
| Marsh 3C | 1 (2.7) | 0 | na |
| N (%) | Pts with Marsh 3 at Histological Control n = 10 | Pts with Marsh 0–1 at Histological Control n = 27 | p |
|---|---|---|---|
| Median months of GFD * (range) | 14 (12–25) | 14 (12–28) | 0.63 |
| Clinical presentation | |||
| Only GI § symptoms | 5 (50%) | 13 (48.2%) | 1 |
| Only malabsorption signs | 4 (40%) | 9 (33.3%) | 0.715 |
| Both symptoms and signs | 1 (10%) | 5 (18.5%) | 0.347 |
| GI § symptoms | |||
| Nausea/vomiting | 0 | 2 (7.4) | 1 |
| Heartburn | 2 (20) | 2 (7.4) | 0.291 |
| Regurgitation | 0 (0) | 0 (0) | 1 |
| Dysphagia | 0 (0) | 1 (3.7) | 1 |
| Postprandial fullness/early satiety | 1 (10) | 7 (25.9) | 0.404 |
| Abdominal pain | 4 (40) | 13 (48.1) | 0.724 |
| Abdominal bloating | 5 (50) | 14 (51.8) | 1 |
| Constipation | 2 (20) | 9 (33.3) | 0.688 |
| Diarrhea | 3 (30) | 7 (25.9) | 1 |
| Signs of malabsorption | 6 (60) | 13 (48.1) | 0.714 |
| Antibody positivity | 2 (20) | 6 (22.2) | 1 |
| Odds Ratio | 95% CI | p | |
|---|---|---|---|
| Age >40 years | 1.9 | 0.63–5.72 | 0.25 |
| Female gender | 0.5 | 0.15–2.13 | 0.41 |
| ≥5 years duration of symptoms/signs before CD diagnosis | 5.3 | 1.32–21.78 | 0.01 |
| Duration of GFD * > 18 months | 0.9 | 0.83–1.02 | 0.15 |
| Associated autoimmune diseases | 0.6 | 0.18–2.32 | 0.51 |
| Constipation at CD § diagnosis | 7.4 | 1.33–41.99 | 0.02 |
| Antibody positivity at histological re-evaluation | 1.4 | 0.38–5.76 | 0.56 |
| Marsh 3C at histological re-evaluation | 0.5 | 0.18–1.86 | 0.36 |
| H. pylori infection at histological re-evaluation | 0.1 | 0.01–1.85 | 0.14 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galli, G.; Carabotti, M.; Pilozzi, E.; Lahner, E.; Annibale, B.; Conti, L. Relationship between Persistent Gastrointestinal Symptoms and Duodenal Histological Findings after Adequate Gluten-Free Diet: A Gray Area of Celiac Disease Management in Adult Patients. Nutrients 2021, 13, 600. https://doi.org/10.3390/nu13020600
Galli G, Carabotti M, Pilozzi E, Lahner E, Annibale B, Conti L. Relationship between Persistent Gastrointestinal Symptoms and Duodenal Histological Findings after Adequate Gluten-Free Diet: A Gray Area of Celiac Disease Management in Adult Patients. Nutrients. 2021; 13(2):600. https://doi.org/10.3390/nu13020600
Chicago/Turabian StyleGalli, Gloria, Marilia Carabotti, Emanuela Pilozzi, Edith Lahner, Bruno Annibale, and Laura Conti. 2021. "Relationship between Persistent Gastrointestinal Symptoms and Duodenal Histological Findings after Adequate Gluten-Free Diet: A Gray Area of Celiac Disease Management in Adult Patients" Nutrients 13, no. 2: 600. https://doi.org/10.3390/nu13020600
APA StyleGalli, G., Carabotti, M., Pilozzi, E., Lahner, E., Annibale, B., & Conti, L. (2021). Relationship between Persistent Gastrointestinal Symptoms and Duodenal Histological Findings after Adequate Gluten-Free Diet: A Gray Area of Celiac Disease Management in Adult Patients. Nutrients, 13(2), 600. https://doi.org/10.3390/nu13020600






