Dietary Patterns in Runners with Gastrointestinal Disorders
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Questionnaire
2.3. Statistical Analysis
3. Results
3.1. Participant Demographics
3.2. Foods Generally Not Well Tolerated
3.3. Food Avoidances Pre-Racing
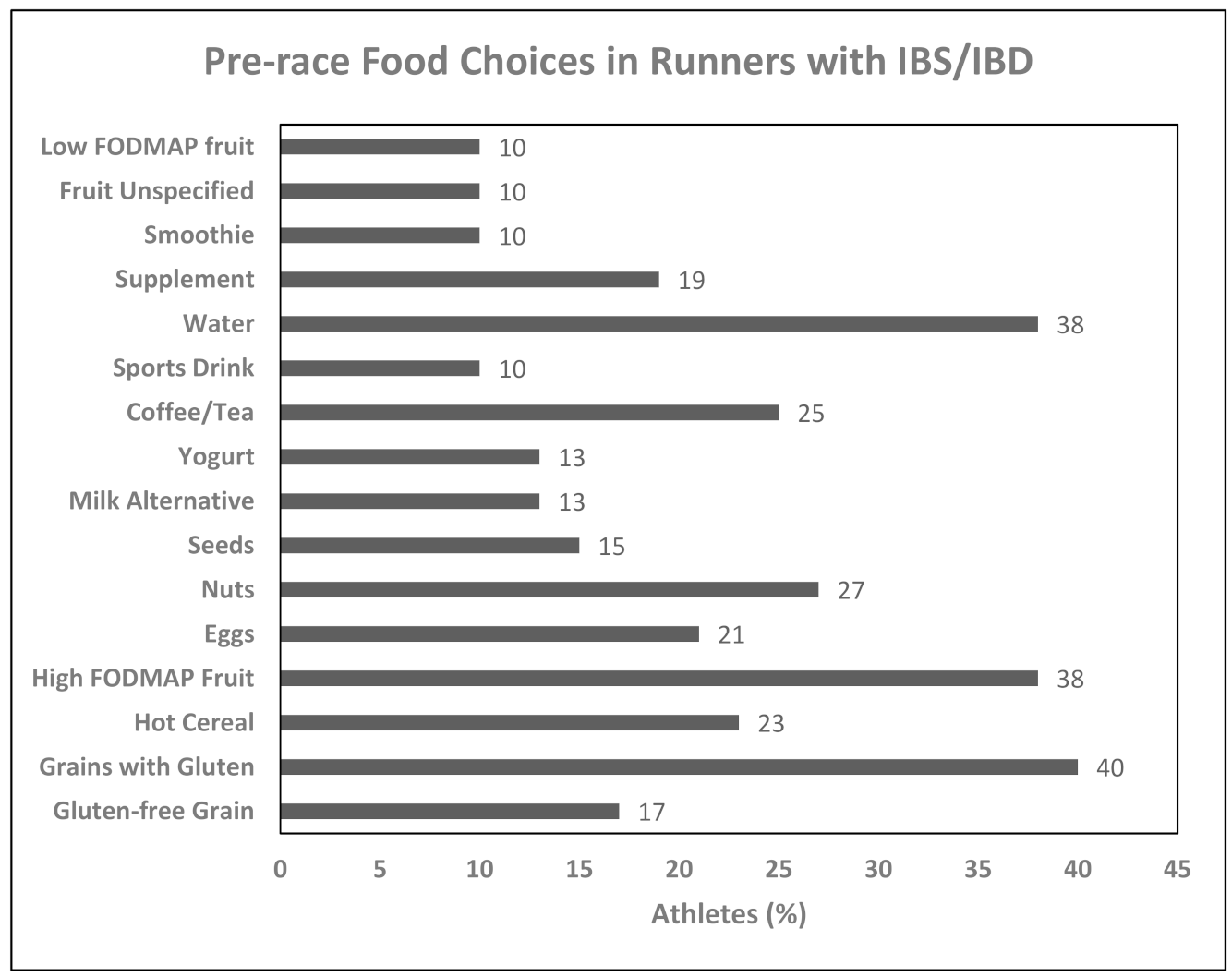
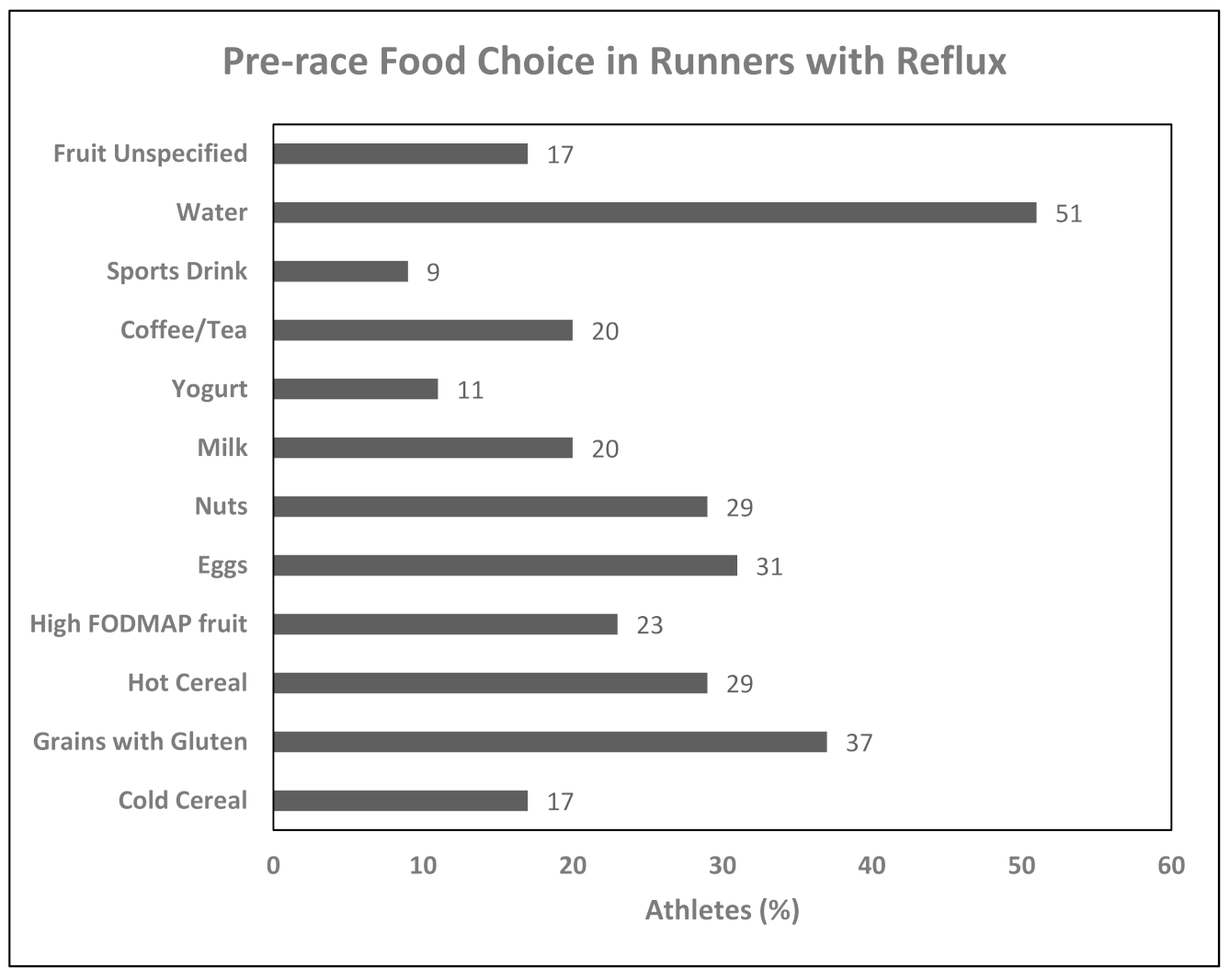
3.4. Foods Consumed Pre-Racing
3.5. Exercise-Induced Gastrointestinal Symptoms
3.6. Sources of Nutrition Information
4. Discussion
4.1. Characteristics of Runners with Medical Conditions
4.2. Food Avoidances in Runners with Medical Conditions
4.3. Foods Chosen Pre-Race in Runners with Gastrointestinal Diseases
4.4. Exercise-Induced Gastrointestinal Symptoms in Runners with Gastrointestinal Diseases
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Costa, R.J.S.; Snipe, R.M.J.; Kitic, C.M.; Gibson, P.R. Systematic review: Exercise-induced gastrointestinal syndrome—Implications for health and intestinal disease. Aliment. Pharmacol. Ther. 2017, 46, 246–265. [Google Scholar] [CrossRef]
- Wilson, P.B. Frequency of chronic gastrointestinal distress in runners: Validity and reliability of a retrospective questionnaire. Int. J. Sport Nutr. Exerc. Metab. 2017, 27, 370–376. [Google Scholar] [CrossRef]
- De Oliveira, E.P.; Burini, R.C.; Jeukendrup, A. Gastrointestinal complaints during exercise: Prevalence, etiology, and nutritional recommendations. Sport. Med. 2014, 44, S79–S85. [Google Scholar] [CrossRef]
- Hoogervorst, D.; van der Burg, N.; Versteegen, J.J.; Lambrechtse, K.J.; Redegeld, M.I.; Cornelissen, L.A.J.; Wardenaar, F.C. Gastrointestinal complaints and correlations with self-reported macronutrient intake in independent groups of (ultra) marathon runners competing at different distances. Sports 2019, 7, 1–18. [Google Scholar] [CrossRef]
- Clark, A.; Mach, N. Exercise-induced stress behavior, gut-microbiota-brain axis and diet: A systematic review for athletes. J. Int. Soc. Sports Nutr. 2016, 13, 1–21. [Google Scholar] [CrossRef]
- Ter Steege, R.W.F.; Kolkman, J.J. Review article: The pathophysiology and management of gastrointestinal symptoms during physical exercise, and the role of splanchinic blood flow. Aliment. Pharmacol. Ther. 2012, 35, 516–528. [Google Scholar] [CrossRef]
- Farmer, A.D.; Wood, E.; Ruffle, J.K. An approach to the care of patients with irritable bowel syndrome. CMAJ 2020, 192, E275–E282. [Google Scholar] [CrossRef]
- Bilski, J.; Mazur-Bialy, A.; Brzozowski, B.; Magierowski, M.; Zahradnik-Bilska, J.; Wojcik, D.; Magierowska, K.; Kwiecien, S.; Mach, T.; Brzozowski, T. Can exercise affect the course of inflammatory bowel disease? Experimental and clinical evidence. Pharmacol. Rep. 2016, 68, 827–836. [Google Scholar] [CrossRef]
- Killian, L.A.; Lee, S.-Y. Irritable bowel syndrome is underdiagnosed and ineffectively managed among endurance athletes. Appl. Physiol. Nutr. Metab. 2019, 44, 1329–1338. [Google Scholar] [CrossRef]
- Lustyk, K.; Jarrett, M.; Bennett, J.; Heitkemper, M. Does a physically active lifestyle improve symptoms in women with irritable bowel syndrome? Gastroenterol. Nurs. 2001, 24, 129–137. [Google Scholar] [CrossRef]
- Engels, M.; Cross, R.K.; Long, M.D. Exercise in patients with inflammatory bowel diseases: Current perspectives. Clin. Exp. Gastroenterol. 2018, 11, 1–11. [Google Scholar] [CrossRef]
- Maleki, B.H.; Tartibian, B.; Mooren, F.C.; FitzGerald, L.H.; Kruger, K.; Chehrzai, M.; Malandish, A. Low-to-moderate intensity aerobic exercise training modulates irritable bowel syndrome through antioxidative and inflammatory mechanisms in women: Results of a randomized controlled trial. Cytokine 2018, 102, 18–25. [Google Scholar] [CrossRef]
- Badillo, R.; Francis, D. Diagnosis and treatment of gastroesophageal reflux disease. World J. Gastrointest. Pharmacol. Ther. 2014, 5, 105–112. [Google Scholar] [CrossRef]
- Collings, K.L.; Pratt, F.P.; Rodriguez-Stanley, S.; Bemben, M.; Miner, P.B. Esophageal reflux in conditioned runners, cyclists, and weightlifters. Med. Sci. Sport. Exerc. 2003, 35, 730–735. [Google Scholar] [CrossRef]
- Parnell, J.A.; Wagner-Jones, K.; Madden, R.F.; Erdman, K.A. Dietary restrictions in endurance runners to mitigate exercise-induced gastrointestinal symptoms. J. Int. Society Sports Nutr. 2020, 17, 1–10. [Google Scholar] [CrossRef]
- Lis, D.M. Exit gluten-free and enter low FODMAPs: A novel dietary strategy to reduce gastrointestinal symptoms in athletes. Sports Med. 2019, 49, S87–S97. [Google Scholar] [CrossRef]
- Mckenzie, Y.A.; Bowyer, R.K.; Leach, H.; Gulia, P.; Horobin, J.; O’Sullivan, N.A.; Pettitt, C.; Reeves, L.B.; Seamark, L.; Williams, M.; et al. British Dietetic Association systematic review and evidence-based practice guidelines for the dietary management of irritable bowel syndrome in adults (2016 update). J. Hum. Nutr. Diet. 2016, 29, 549–575. [Google Scholar] [CrossRef]
- Varju, P.; Farkas, N.; Hegyi, P.; Garami, A.; Szabo, I.; Illes, A.; Solymar, M.; Vincze, A.; Balasko, M.; Par, G.; et al. Low fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP) diet improves symptoms in adults suffering from irritable bowel syndrome (IBS) compared to standard IBS diet: A meta-analysis of clinical studies. PLoS ONE 2017, 12, 1–15. [Google Scholar] [CrossRef]
- Hungin, A.P.S.; Mitchell, C.R.; Whorwell, P.; Mulligan, C.; Cole, O.; Agreus, L.; Fracasso, P.; Lionis, C.; Mendive, C.; Philippart de Foy, J.-M.; et al. Systematic review: Probiotics in the management of lower gastrointestinal symptoms—An updated evidence-based international consensus. Aliment. Pharmacol. Ther. 2018, 47, 1054–1070. [Google Scholar] [CrossRef]
- Lamb, C.A.; Kennedy, N.A.; Raine, T.; Hendy, P.A.; Smith, P.J.; Limdi, J.K.; Hayee, B.; Lomer, M.C.E.; Parkes, G.C.; Selinger, C.; et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut 2019, 68, s1–s106. [Google Scholar] [CrossRef]
- Uranga, J.A.; Lopez-Miranda, V.; Lombo, F.; Abalo, R. Food, nutrients and nutraceuticals affecting the course of inflammatory bowel disease. Pharmacol. Rep. 2016, 68, 816–826. [Google Scholar] [CrossRef]
- Thomas, D.T.; Erdman, K.A.; Burke, L.M. Position of the Academy of Nutrition and Dietetics, Dietitians of Canada, and the American College of Sports Medicine: Nutrition and athletic performance. J. Acad. Nutr. Diet. 2016, 116, 501–528. [Google Scholar] [CrossRef]
- Lis, D.M.; Stellingwerff, T.; Shing, C.M.; Ahuja, K.D.K.; Fell, J.W. Exploring the popularily, experiences, and beliefs surrounding gluten-free diets in nonceliac athletes. Int. J. Sport Nutr. Exerc. Metab. 2015, 25, 37–45. [Google Scholar] [CrossRef]
- Wiffin, M.; Smith, L.; Antonio, J.; Johnstone, J.; Beasley, L.; Roberts, J. Effect of a short-term low fermentable oligosaccharide, disaccharide, monosaccharide and polyol (FODMAP) diet on exercise-related gastrointestinal symptoms. J. Int. Soc. Sports Nutr. 2019, 16, 1–9. [Google Scholar] [CrossRef]
- Gaskell, S.K.; Costa, R.J.S. Applying a low-FODMAP dietary intervention to a female ultraendurance runner with irritable bowel syndrome during a multistage ultramarathon. Int. J. Sport Nutr. Exerc. Metab. 2019, 29, 61–67. [Google Scholar] [CrossRef]
- Gaskell, S.K.; Taylor, B.; Muir, J.; Costa, R.J.S. Impact of 24-h high and low fermentable oligo-, di, monosaccharide and polyol diets on markers of exercise-induced gastrointestinal syndrome in response to exertional heat stress. Appl. Physiol. Nutr. Metab. 2020, 45, 569–580. [Google Scholar] [CrossRef]
- Lis, D.; Ahuja, K.D.K.; Stellingwerff, T.; Kitic, C.M.; Fell, J. Food avoidance in athletes: FODMAP foods on the list. Appl. Physiol. Nutr. Metab. 2016, 41, 1002–1004. [Google Scholar] [CrossRef]
- Mehta, R.S.; Song, M.; Staller, K.; Chan, A.T. Association between beverage intake and incidence of gastroesophageal reflux symptoms. Clin. Gastroenterol. Hetapol. 2020, 18, 2226–2233. [Google Scholar] [CrossRef]
- Parnell, J.A.; Lafave, H.; Wagner-Jones, K.; Madden, R.F.; Erdman, K.A. Development of a questionnaire to assess dietary restrictions runners use to mitigate gastrointestinal symptoms. J. Int. Soc. Sports Nutr. 2019, 16, 1–9. [Google Scholar] [CrossRef]
- Hungin, A.P.S.; Chang, L.; Locke, G.R.; Dennis, E.H.; Barghout, V. Irritable bowel syndrome in the United States: Prevalence, symptom patterns and impact. Aliment. Pharmacol. Ther. 2005, 21, 1365–1375. [Google Scholar] [CrossRef]
- Lovell, R.M.; Ford, A.C. Global prevalence of and risk factors for irritable bowel syndrome: A meta-analysis. Clin. Gastroenterol. Hepatol. 2012, 10, 712–721. [Google Scholar] [CrossRef] [PubMed]
- Fedorak, R.N.; Vanner, S.J.; Paterson, W.G.; Bridges, R.J. Canadian Digestive Health Foundation Public Impact Series 3: Irritable bowel syndrome in Canada. Incidence, prevalence, and direct and indirect economic impact. Can. J. Gastroenterol. 2012, 26, 252–257. [Google Scholar] [CrossRef] [PubMed]
- MacDermott, R.P. Treatment of irritable bowel syndrome in outpatients with inflammatory bowel disease using a food and beverage intolerance, food and beverage avoidance diet. Inflamm. Bowel Dis. 2007, 13, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Borghini, R.; Donato, G.; Alvaro, D.; Picarelli, A. New insights in IBS-like disorders: Pandora’s box has been opened; a review. Gastroenterol. Hepatol. Bed Bench 2017, 10, 79–89. [Google Scholar] [PubMed]
- Croall, I.D.; Trott, N.; Rej, A.; Aziz, I.; O’Brien, D.J.; George, H.A.; Hossain, M.Y.; Marks, L.J.S.; Richardson, J.I.; Rigby, R.; et al. A population survey of dietary attitudes towards gluten. Nutrients 2019, 11, 1–8. [Google Scholar] [CrossRef]
- Burke, L.M.; Jones, A.M.; Jeukendrup, A.E.; Mooses, M. Contemporary nutrition strategies to optimize performance in distance runners and race walkers. Int. J. Sport Nutr. Exerc. Metab. 2019, 29, 117–129. [Google Scholar] [CrossRef]
- Tiller, N.B.; Roberts, J.D.; Beasley, L.; Chapman, S.; Pinto, J.M.; Smith, L.; Wiffin, M.; Russell, M.; Sparks, S.A.; Duckworth, L.; et al. International Society of Sports Nutrition Position Stand: Nutritional considerations for single-stage ultra-marathon training and racing. J. Int. Soc. Sports Nutr. 2019, 16, 1–23. [Google Scholar] [CrossRef]
- James, S.C.; Fraser, K.; Young, W.; McNabb, W.C.; Roy, N.C. Gut microbial metabolites and biochemical pathways involved in irritable bowel syndrome: Effects of diet and nutrition on the microbiome. J. Nutr. 2020, 150, 1012–1021. [Google Scholar] [CrossRef]
- Szilagyi, A.; Ishayek, N. Lactose intolerance, dairy avoidance, and treatment options. Nutrients 2018, 10, 1–30. [Google Scholar] [CrossRef]
- Lis, D.M.; Stellingwerff, T.; Kitic, C.M.; Fell, J.W.; Ahuja, K.D.K. Low FODMAP: A preliminary strategy to reduce gastrointestinal distress in athletes. Med. Sci. Sports Exerc. 2018, 50, 116–123. [Google Scholar] [CrossRef]
- Bronkowska, M.; Kosendiak, A.; Orzeł, D. Assessment of the frequency of intake of selected sources of dietary fibre among persons competing in marathons. Rocz. Państwowego Zakładu Hig. 2018, 69, 347–351. [Google Scholar] [CrossRef] [PubMed]
- Jang, L.G.; Choi, G.; Kim, S.W.; Kim, B.Y.; Lee, S.; Park, H. The combination of sport and sport-specific diet is associated with characteristics of gut microbiota: An observational study. J. Int. Soc. Sports Nutr. 2019, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Rehrer, N.J.; van Kemenade, M.; Meester, W.; Brouns, F.; Saris, W. Gastrointestinal complaints in relation to dietary intake in triathletes. Int. J. Sport Nutr. 1992, 2, 48–59. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.; Canfora, E.E.; Blaak, E.E. Gastrointestinal transit time, glucose homeostasis and metabolic health: Modulation by dietary fibers. Nutrients 2018, 10, 275. [Google Scholar] [CrossRef] [PubMed]
- Morozov, S.; Isakov, V.; Konovalova, M. Fiber-enriched diet helps to control symptoms and improves esophageal motility in patients with non-erosive gastroesophageal reflux disease. World J. Gastroenterol. 2018, 24, 2291–2299. [Google Scholar] [CrossRef]
- Martinucci, I.; Guidi, G.; Savarino, E.V.; Frazzoni, M.; Tolone, S.; Frazzoni, L.; Fuccio, L.; Bertani, L.; Bodini, G.; Ceccarelli, L.; et al. Vegetal and animal food proteins have a different impact in the first postprandial hour of impedance-pH analysis in patients with heartburn. Gastroenterol. Res. Pract. 2018, 1–7. [Google Scholar] [CrossRef]
- Rothschild, J.A.; Kilding, A.E.; Plews, D.J. Pre-exercise nutrition habits and beliefs of endurance athletes vary by sex, competitive level, and diet. J. Am. Coll. Nutr. 2020, 1–12. [Google Scholar] [CrossRef]
- Snipe, R.M.J.; Khoo, A.; Kitic, C.M.; Gibson, P.R.; Costa, R.J.S. Carbohydrate and protein intake during exertional heat stress ameliorates intestinal epithelial injury and small intestine permeability. Appl. Physiol. Nutr. Metab. 2017, 42, 1283–1292. [Google Scholar] [CrossRef]
- Forbes, A.; Escher, J.; Hebuterne, X.; Klek, S.; Krznaric, Z.; Schneider, S.; Shamir, R.; Stardelova, K.; Wierdsma, N.; Wiskin, A.E.; et al. ESPEN guideline: Clinical nutrition in inflammatory bowel disease. Clin. Nutr. 2017, 36, 321–347. [Google Scholar] [CrossRef]
- Wilson, P.B. Dietary and non dietary correlates of gastrointestinal distress during the cycle and run of a triathlon. Eur. J. Sport Sci. 2016, 16, 448–454. [Google Scholar] [CrossRef]
- Pickering, C.; Grgic, J. Caffeine and exercise: What next? Sports Med. 2019, 49, 1007–1030. [Google Scholar] [CrossRef] [PubMed]
- Ali, F.; Rehman, H.; Babayan, Z.; Stapleton, D.; Joshi, D.-D. Energy drinks and their adverse health effects: A systematic review of the current evidence. Postgrad. Med. 2015, 127, 308–322. [Google Scholar] [CrossRef] [PubMed]
- Gunja, N.; Brown, J.A. Energy drinks: Health risks and toxicity. Med. J. Aust. 2012, 196, 46–49. [Google Scholar] [CrossRef] [PubMed]
- Helge, J.W. A high carbohydrate diet remains the evidence based choice for elite athletes to optimise performance. J. Physiol. 2017, 595, 2775. [Google Scholar] [CrossRef] [PubMed]
- Stellingwerff, T.; Cox, G.R. Systematic review: Carbohydrate supplementation on exercise performance or capacity of varying durations. Appl. Physiol. Nutr. Metab. 2014, 39, 998–1011. [Google Scholar] [CrossRef]
- Surdea-Blaga, T.; Negrutiu, D.E.; Palage, M.; Dumitrascu, D.L. Food and gastroesophageal reflux disease. Curr. Med. Chem. 2019, 26, 3497–3511. [Google Scholar] [CrossRef]
- Ten Haaf, D.S.M.; van der Worp, M.P.; Groenewoud, H.M.M.; Leij-halfwerk, S.; Nijhuis-van der Sanden, M.W.G.; Verbeek, A.L.M.; Staal, J.B. Nutritional indicators for gastrointestinal symptoms in female runners: The “Marikenloop study”. BMJ Open 2014, 4, 1–8. [Google Scholar] [CrossRef]
- Keeffe, E.B.; Lowe, D.K.; Goss, J.R.; Wayne, R. Gastrointestinal symptoms of marathon runners. West J. Med. 1984, 141, 481–484. [Google Scholar]
- Pugh, J.N.; Kirk, B.; Fearn, R.; Morton, J.P.; Close, G.L. Prevalence, severity and potential nutritional causes of gastrointestinal symptoms during a marathon in recreational runners. Nutrients 2018, 10, 1–7. [Google Scholar] [CrossRef]
- Ter Steege, R.W.F.; van der Palen, J.; Kolkman, J.J. Prevalence of gastrointestinal complaints in runners competing in a long distance run: An internet based observational study in 1281 subjects. Scand. J. Gastroenterol. 2008, 43, 1477–1482. [Google Scholar] [CrossRef]
- Pfeiffer, B.; Stellingwerff, T.; Hodgson, A.B.; Randell, R.; Pöttgen, K.; Res, P.; Jeukendrup, A.E. Nutritional intake and gastrointestinal problems during competitive endurance events. Med. Sci. Sports Exerc. 2012, 44, 344–351. [Google Scholar] [CrossRef] [PubMed]
| Participants | IBS/IBD n (%) | Reflux n (%) | Control Runners n (%) |
|---|---|---|---|
| Gender | |||
| Male | 2 (4) (<0.001) | 11 (31) | 162 (45) |
| Female | 50 (96) | 25 (69) | 195 (55) |
| Performance Level | |||
| Lower Recreational | 25 (49) | 18 (50) | 128 (35) |
| Upper Recreational | 24 (47) | 16 (44) | 208 (56) |
| Competitive | 2 (4) | 2 (6) | 33 (9) |
| Run Distance | |||
| Don’t Compete | 1 (2) | 0 (0) | 0 (0) |
| 5 km | 13 (25) | 9 (26) | 63 (18) |
| 6–10 km | 16 (31) | 15 (43) | 123 (35) |
| Half-marathon | 14 (27) | 8 (23) | 130 (37) |
| Marathon | 8 (15) | 3 (9) | 40 (11) |
| Allergies | |||
| Tree Nuts | 4 (8) | 2 (5) | n/a |
| Milk | 12 (23) | 4 (11) | n/a |
| Soy | 2 (4) | 2 (5) | n/a |
| Sulfites | 3 (6) | 1 (3) | n/a |
| Whey | 5 (9) | 1 (3) | n/a |
| Eggs | 2 (4) | 0 (0) | n/a |
| Peanuts | 3 (6) | 1 (3) | n/a |
| Fish | 1 (2) | 5 (14) | n/a |
| Wheat | 6 (11) | 0 (0) | n/a |
| Gluten | 8 (15) | 1 (3) | n/a |
| Casein | 5 (9) | 1 (3) | n/a |
| Avocados | 1 (2) | 0 (0) | n/a |
| Corn & oats | 1 (2) | 0 (0) | n/a |
| Cranberries & pineapple | 1 (2) | 0 (0) | n/a |
| Garlic | 1 (2) | 0 (0) | n/a |
| Octopus | 1 (2) | 0 (0) | n/a |
| MSG | 0 (0) | 1 (3) | n/a |
| Oranges | 0 (0) | 1 (3) | n/a |
| Horseradish | 0 (0) | 1 (3) | n/a |
| Bananas & capers | 0 (0) | 1 (3) | n/a |
| Foods Not Well Tolerated | IBS/IBD n (%) | Reflux n (%) | Control Runners n (%) |
|---|---|---|---|
| Grains | 18 (34) (<0.001) | 6 (16) (0.014) | 18 (5) |
| Legumes | 8 (15) (<0.001) | 0 (0) | 4 (1) |
| Soy milk | 7 (13) (<0.001) | 2 (5) | 3 (1) |
| Starchy vegetable | 5 (9) (<0.001) | 0 (0) | 2 (0.5) |
| Cold cereal | 5 (9) (0.010) | 2 (5) | 7 (2) |
| Hot cereal | 7 (13) (<0.001) | 1 (3) | 3 (1) |
| Nuts | 4 (8) (0.006) | 2 (5) | 3 (1) |
| Coffee/tea | 6 (11) (0.001) | 3 (8) (0.039) | 6 (2) |
| Yogurt | 17(32) (<0.001) | 8 (22) (0.001) | 17 (5) |
| Eggs | 9 (17) (<0.001) | 1 (3) | 4 (1) |
| Cheese | 17 (32) (<0.001) | 11 (30) (<0.001) | 23 (6) |
| Milk | 26 (49) (<0.001) | 15 (41) (<0.001) | 52 (14) |
| Sports Bar/gel | 5 (9) (0.037) | 2 (5) | 11 (3) |
| Vegetable | 8 (15) (0.001) | 3 (8) | 12 (3) |
| Gluten-free grains | 7 (13) (0.001) | 1 (3) | 9 (2) |
| Energy drinks | 4 (8) (0.036) | 2 (5) | 7 (2) |
| Sports drink | 3 (6) | 1 (3) | 5 (1) |
| Fruit | 4 (8) (0.025) | 2 (5) | 6 (2) |
| Foods Avoided | IBS/IBD n (%) | Reflux n (%) | Control Runners n (%) |
|---|---|---|---|
| Meat | 16 (31) | 13 (36) | 121 (33) |
| Milk products | 21 (53) | 12 (38) | 135 (37) |
| Fish/seafood | 11 (22) | 6 (19) | 109 (30) |
| Poultry | 11 (21) | 9 (25) | 93 (25) |
| High-fibre | 14 (27) | 12 (33) | 85 (23) |
| Chocolate | 12 (23) | 9 (25) | 83 (23) |
| Legumes | 19 (37) (0.006) | 11 (31) | 70 (19) |
| Coffee/tea | 13 (25) | 9 (25) | 71 (19) |
| Energy drinks | 11 (21) | 3 (8) | 61 (17) |
| Starchy vegetable | 8 (15) | 4 (11) | 56 (15) |
| Lactose-free milk | 4 (10) | 2 (7) | 55 (15) |
| Eggs | 9 (18) | 5 (14) | 54 (15) |
| Soy milk | 14 (28) (0.012) | 6 (18) | 50 (14) |
| Sports drink | 5 (10) | 1 (3) | 42 (11) |
| Vegetables | 7 (14) | 7 (19) | 44 (12) |
| Cold cereal | 7 (16) | 6 (17) | 44 (12) |
| Grain | 14 (32) (<0.001) | 6 (17) | 37 (10) |
| Hot cereal | 9 (21) (0.010) | 3 (9) | 28 (8) |
| Gluten-free grain | 6 (12) | 4 (11) | 28 (8) |
| Sports bar/gel | 6 (12) | 3 (8) | 39 (11) |
| Juice | 8 (15) | 3 (8) | 37 (10) |
| Smoothie | 6 (12) | 6 (17) | 33 (9) |
| Fruit | 6 (12) | 5 (14) | 30 (8) |
| Nuts | 6 (13) | 5 (15) | 40 (11) |
| Coconut milk | 7 (14) | 4 (11) | 44 (12) |
| Almond milk | 4 (9) | 3 (9) | 41 (11) |
| Symptoms | IBS/IBD n (%) | Reflux n (%) | Control Runners n (%) |
|---|---|---|---|
| Stomach pain/cramps | 40 (77) (<0.001) | 19 (53) | 157 (43) |
| Intestinal pain/discomfort | 30 (58) (<0.001) | 12 (33) | 85 (23) |
| Side ache/stitch | 12 (23) | 11 (31) | 81 (22) |
| Urge to defecate | 16 (31) | 13 (36) | 79 (21) |
| Bloating | 27 (52) (<0.001) | 18 (50) (<0.001) | 72 (20) |
| Diarrhea | 30 (58) (<0.001) | 14 (39) (0.007) | 66 (18) |
| Fullness/heaviness | 11 (24) | 7 (25) | 60 (18) |
| Burping/belching | 10 (19) | 7 (19) | 58 (16) |
| Gas | 18 (35) (0.003] | 11 (31) (0.039) | 60 (16) |
| Nausea/vomiting | 15 (29) (0.001] | 11 (31) (0.002) | 38 (10) |
| Reflux/heartburn | 6 (12) | 15 (42) (<0.001) | 26 (7) |
| Bleeding | 0 (0) | 0 (0) | 1 (0.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Erdman, K.A.; Jones, K.W.; Madden, R.F.; Gammack, N.; Parnell, J.A. Dietary Patterns in Runners with Gastrointestinal Disorders. Nutrients 2021, 13, 448. https://doi.org/10.3390/nu13020448
Erdman KA, Jones KW, Madden RF, Gammack N, Parnell JA. Dietary Patterns in Runners with Gastrointestinal Disorders. Nutrients. 2021; 13(2):448. https://doi.org/10.3390/nu13020448
Chicago/Turabian StyleErdman, Kelly Anne, Kim Wagner Jones, Robyn F. Madden, Nancy Gammack, and Jill A. Parnell. 2021. "Dietary Patterns in Runners with Gastrointestinal Disorders" Nutrients 13, no. 2: 448. https://doi.org/10.3390/nu13020448
APA StyleErdman, K. A., Jones, K. W., Madden, R. F., Gammack, N., & Parnell, J. A. (2021). Dietary Patterns in Runners with Gastrointestinal Disorders. Nutrients, 13(2), 448. https://doi.org/10.3390/nu13020448






