Abstract
The endocannabinoid system (ECS) is an endogenous signaling system formed by specific receptors (cannabinoid type 1 and type 2 (CB1 and CB2)), their endogenous ligands (endocannabinoids), and enzymes involved in their synthesis and degradation. The ECS, centrally and peripherally, is involved in various physiological processes, including regulation of energy balance, promotion of metabolic process, food intake, weight gain, promotion of fat accumulation in adipocytes, and regulation of body homeostasis; thus, its overactivity may be related to obesity. In this review, we try to explain the role of the ECS and the impact of genetic factors on endocannabinoid system modulation in the pathogenesis of obesity, which is a global and civilizational problem affecting the entire world population regardless of age. We also emphasize that the search for potential new targets for health assessment, treatment, and the development of possible therapies in obesity is of great importance.
1. Introduction
According to the World Health Organization (WHO), obesity is defined by a body mass index (BMI) higher than or equal to 30 kg/m2. Although the BMI is not an ideal diagnostic tool, it is widely used in clinical practice as well as in assessing the prevalence of obesity worldwide. However, it should be noted that the BMI uses only height and body weight, which could be misleading when muscle tissue is overgrown [1]. Therefore, the waist-to-hip ratio (WHR) should be measured to assess the location of adipose tissue [2]. In recent years, more accurate techniques, such as bioelectrical impedance analysis (BIA) or gold-standard dual-energy X-ray absorptiometry (DXA), have become more common, allowing a more precise evaluation of adipose tissue [3].
Within a few decades, obesity has become a global problem. Currently, almost 2 billion individuals worldwide suffer from overweight, and over 650 million are obese (Figure 1) [4]. In Poland, 21.3% of adults suffered from obesity in 2016, with a slight predominance of men. On the other hand, in the U.S., 36.2% of the population, predominantly women, suffer from obesity [5]. In fact, the prevalence of obesity has almost tripled since 1975 [6], and it is estimated that by 2030, half of the world’s population will be overweight [7]. Currently, obesity, especially among children, is vastly increasing in developing countries, particularly in urban areas. Interestingly, the prevalence of obesity is more than 30% higher among children living in developing countries than among children living in developed countries [8]. It is essential to note that 75% of people with excessive body weight in childhood will suffer from overweight or obesity in adult life [9]. The pathogenesis of obesity is complex and has not been investigated thoroughly enough, although it is accepted that behavioral, genetic, and biological factors, including intestinal microbiota or even intrauterine growth, have been associated with the development of obesity [8,10,11].
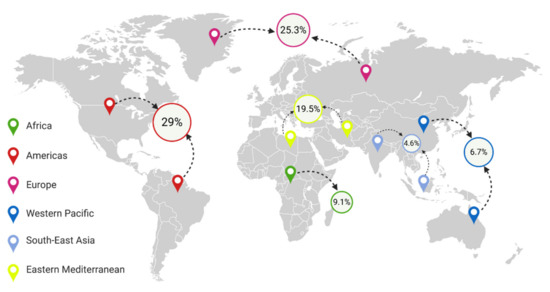
Figure 1.
Percentage of people with obesity in different regions of the world [13,14,15,16,17].
There is evidence of a link between intestinal microbiota and obesity. It has been discovered that microbiological changes in the intestine constitute a risk factor for obesity among humans [12]. In addition, bariatric surgery partly improves excessive body weight, associated with intestinal dysbiosis, and the changes in the intestinal microbiota composition have been associated with positive results following the surgery, i.e., with weight loss or metabolism improvement [11].
However, the direct cause of obesity is excessive calorie intake. Nearly 3 million people in the world die of obesity-related comorbidities each year [5]. Furthermore, obesity is associated with a higher incidence of cardiovascular disease, including heart failure, which is the main cause of death globally.
One of the elements responsible for the body’s nutrition and metabolic state is the food-intake-regulating system, involving numerous hormones, cytokines, and other transmitters, such as insulin, leptin, ghrelin, glucocorticosteroids, and endocannabinoids [18]. Food intake is regulated at both central and peripheral levels [19]. Central regulation is responsible for nutritional (pro-nutritional) behavior and the resulting feeling of pleasure, whereas peripheral regulation is based on the modification of lipogenesis, adipogenesis, glucose metabolism, and lipoprotein metabolism, in which the endocannabinoid system (ECS) plays a significant role [4,20].
The isolation of Δ9-tetrahydrocannabinol (Δ9-THC) in 1964 was a milestone in discovering the endocannabinoid system [21]. Studies on Δ9-THC led to the identification of the first cannabinoid receptor, i.e., cannabinoid receptor type 1 (CB1R) in the rat brain, which was classified as a G-protein-coupled receptor (GPCR) [22]. In the following years, CB1R was found in many species, including humans [23]. In 1993, a second cannabinoid receptor, cannabinoid receptor type 2 (CB2R), also classified as a GPCR, was discovered in spleen macrophages [24]. It is worth mentioning that other types of cannabinoid receptors, nonCB1 and nonCB2 orphan GPR55 and TRPV1 receptors, have been reported so far, which may explain the pathway that has not been fully understood [25,26,27]. However, to date, no genetic polymorphism changes in GPR55 and TRPV receptors have been identified in terms of their role in determining obesity. Only in vivo studies on the role of GPR55 in energy and glucose homeostasis have been performed in GPR55-/- mice, which revealed that GPR55 knockout, at least partially, increased adiposity and insulin resistance due to reduced physical activity [28]. A similar observation was confirmed for the TRPV receptor, where the authors evaluated the effect of capsaicin on the browning program in white adipose tissue (WAT) by the activation of TRPV1 channels to prevent diet-induced obesity in wild-type and TRPV1(-/-) mouse models. They successfully demonstrated that activation of TRPV1 channels by dietary capsaicin results in the browning of WAT, thus prevent obesity, which implies that TRPV could become a promising new target to combat obesity [29]. This fact was confirmed by Christie et al. in 2018, which indicates that TRPV may be involved in energy homeostasis and the control of food intake, appetite, and energy expenditure. This, in turn, strongly suggests that its dysregulation may be involved in the development of obesity. The mechanisms causing dysregulation have not been fully understood, but interactions with the ECS may, to some extent, explain the role of TRPV in this dysregulation [30].
The discovery of cannabinoid receptors allowed one to identify its endogenous cannabinoids, such as the endogenous partial agonist anandamide (AEA) and the endogenous full agonist 2-arachidonylglycerol (2-AG) [31], with a greater affinity for CB1 and CB2 than AEA [32,33], or virodhamine (CB1 receptor antagonist and CB2 receptor agonist) derived from arachidonic acid and ethanolamine [34].
The abovementioned AEA and 2-AG are the best-known endocannabinoids, although other ECS neurotransmitters, such as 2-arachidonyl glyceryl ether (2-AGE), N-arachidonoyl dopamine (NADA), oleamide (cis-9,10-octadecanoamide (ODA)), N-arachidonylglycine (NAGLy), palmitoylethanolamide (PEA), stearoylethanolamide (SEA), and oleoylethanolamine (OEA) [33], should also be mentioned, since they all have an affinity for cannabinoid-like G-coupled receptors. The endocannabinoid system is also formed by synthesizing and degrading enzymes, such as AEA-synthesizing enzymes (N- acylotransferase (NAT), N-acyl phosphatidylethanolamine phospholipase D (NAPE-PLD), and fatty acid amide hydrolase (FAAH)) and 2-AG-regulating enzymes (diacylglycerol lipase (DAGL) and monoacylglycerol lipase (MAGL)) [33,35]. Moreover, it has been recently discovered that glycerophosphodiester phosphodiesterase 3 (GDE3) acts as an ecto-enzyme and converts bioactive lysophosphadylinositol (LPI) to monoacyloglycerols (MG), including 2-AG, and activates CB1R as well as CB2R signaling in mammalian cultured cells [36,37].
CB1R is primarily located in the central and peripheral nervous systems, i.e., in the cerebral cortex (neocortex), with a high accumulation in the cingulate cortex, and the frontal and motor cortex. It is also present in the olfactory structures of the brain and the hippocampus, where the accumulation is exceptionally high, as well as in the amygdala, striatum, cortex, deep cerebellar nuclei, brain stem, spinal cord, diencephalon, and hypothalamus, where, in contrast, its accumulation is relatively low [38]. It should be noted that CB1R is the most common receptor of GPCRs in the mammalian central nervous system (CNS) [39,40]. Besides, CB1R is found in adipocytes and muscles, adrenals, pancreas, liver, gastrointestinal cells, and other tissues [41]. CB2R is formerly considered a peripheral receptor due to its location in spleen macrophages. However, cannabinoid receptor type 2 has also been found in some parts of the brain, such as the striatum, hypothalamus, cerebral cortex, hippocampus, amygdala, and substantia nigra [41,42]. Nevertheless, the immune system is the primary location of the CB2 receptor. The CB2 receptor was found in macrophages, including osteocytes, osteoclasts, Kupffer cells, and B lymphocytes, and in each organ with immune cells, including the cardiovascular system, gastrointestinal tract, and reproductive system, and plays an important role in inflammatory processes (Table 1) [43,44,45,46].

Table 1.
Presence of CB1R and CB2R in human tissues [47,48,49].
2. Role of the Endocannabinoid System in Metabolic Process Regulation
Endocannabinoids are involved in the physiological regulation of the body’s homeostasis, stimulating food intake and hunger, as well as shifting energy balance toward energy storage [50], by means of acting on peripheral tissues, such as adipocytes, hepatocytes, islet cells, the gastrointestinal tract, and skeletal muscles (Figure 2).

Figure 2.
Schematic illustration of the endocannabinoid system role in the regulation of metabolic processes. CB1R—cannabinoid receptor type 1; CB2R—cannabinoid receptor type 2; CNR1—endocannabinoid type 1 receptor gene; CNR2—endocannabinoid type 2 receptor gene; FAAH—fatty acid amide hydrolase; NAPE-PLD—N-acyl phosphatidylethanolamine phospholipase D.
2.1. Adipose Tissue
The ECS promotes fat storage in adipocytes by intensifying adipogenesis and acts directly by increasing triacylglyceride (TAG) production. It has been shown that the blockage of CB1R decreases adipocyte proliferation, while adipocyte differentiation is directly preceded by multiple increases in AEA and 2-AG levels in mice [51,52]. CB1R stimulation is accompanied by an increase in peroxisome proliferator-activated receptor gamma (PPAR-γ) receptors, which play an essential role in adipocyte proliferation and increase the size and quantity of TAG in adipocytes of diet-induced obese mice [51,53]. Additionally, CB1R activation decreases adiponectin expression and increases leptin expression in mouse white adipose tissue (WAT) [54].
2.2. Lipogenesis and Lipolysis
CB1R activation in mice stimulates the expression of PPAR-γ and lipoprotein lipase, which increases the availability of substrate for TAG production, stored in adipocytes [55]. Moreover, CB1 inhibits adenylate cyclase activity, which inhibits the activity of 5′AMP-activated protein kinase (AMPK), and further of AMPK-associated lipolysis, which reduces fatty acid synthase (FAS) inhibition and lipolysis. CB1R stimulation also directly increases FAS expression. On the other hand, CB1R increases glucose uptake into the adipose tissue by directly affecting glucose transporter type 4 (GLUT4) in adipocytes. These activities under physiological conditions are regulated by autocrine mechanisms in the adipose tissue. However, under pathological conditions, these actions cause dyslipidemia, i.e., mainly an increase in TAG and low-density lipoprotein (LDL) in the serum, and play a crucial role in developing insulin resistance (IR) [20].
2.3. Brown Adipose Tissue
CB1R is present in brown adipose tissue (BAT) adipocytes. Previous studies suggest that CB1R activation in BAT is based on the inhibition of signals from the sympathetic nervous system (SNS), which decreases thermogenesis [56]. Moreover, peripheral CB1R blockade in BAT can provide a new approach to treating obesity and lowering cardiovascular risk. In fact, chronic CB1R antagonism has been associated with activation of BAT thermogenesis and weight loss in diet-induced obese mice and rats by both peripheral and CNS-located CB1R [56,57]. As Eriksson et al. demonstrated, CB1R can be a promising surrogate biomarker for BAT, which would be helpful in further investigation of the activation and regulation of BAT and energy expenditure [58]. Similar results were obtained in the study by Boon et al., where CB1R blockade with rimonabant in mice enhanced energy expenditure and reduced dyslipidemia [59]. However, EC signaling via CB1R could also provide new approaches to treating obesity and improving metabolism in humans [60].
2.4. Liver
As mentioned earlier, CB1R is expressed in the liver, promoting the synthesis and storage of TAG [61]. The activation of CB1R in wild-type mice resulted in increased expression of sterol regulatory element-binding protein-1c (SREBP-1c) and subsequent expression of related lipogenic enzymes, e.g., FAS and acetyl-CoA carboxylase. Under pathological conditions, it significantly contributes to the development of non-alcoholic steatohepatitis (NASH), further hepatic fibrosis, and dyslipidemia or dyslipoproteinemia [62,63,64]. Moreover, CB1R activation causes an expansion of the adipose tissue in the liver, which causes IR [65]. In contrast, the ECS inhibits adiponectin expression, which stimulates liver AMPK and fatty acid entrance into mitochondrial oxidation pathways. It proves that in addition to the direct effect on liver metabolism, the ECS also indirectly decreases the oxidation of fatty acids in the liver in vivo [66]. Furthermore, CB2 is also expressed in hepatocytes, and CB1R antagonists and CB2 agonists protect the liver from toxic failure [67].
2.5. Skeletal Muscles
The action effect of CB1 in the muscles is associated with the regulation of glucose uptake through the modulation of insulin sensitivity. Under physiological conditions, the activation of CB1 in mice results in a decrease in glucose uptake and oxygen consumption by inhibiting fatty acid oxidation [68,69].
2.6. Pancreas
It has been demonstrated that CB1R and CB2 are present in alpha and beta islet cells, although their stimulation has a different result. The activation of CB1 increases insulin secretion from beta cells and glucagon from alpha cells in mice. CB2 stimulation decreases insulin secretion from beta cells and glucagon from alpha cells. These data suggest, therefore, that the glucose plasma concentrations induced by the ECS are not directly associated with pancreatic hormones; however, they are associated to a greater extent with the modulation of peripheral insulin sensitivity dependent upon the ECS [20,70,71].
2.7. Gastrointestinal Tract
The ECS reduces the feeling of satiety, which increases the frequency and quantity of food intake. Simultaneously, the ECS decreases gastric juice secretion, intestinal peristalsis, and bowel content passage. This, in turn, results in a higher absorption of nutrients, which could lead to weight gain and further obesity. These processes are influenced by receptors located in the gastrointestinal tract (GT) and the peripheral nervous system [72,73,74]. In fact, a high-fat diet-specific increase of AEA and 2-AG in the jejunum suggests the presence of positive feedback loops. The inhibition of this loop could reduce the consumption of fat-rich products, thus providing a therapeutic solution [75,76]. Furthermore, endocannabinoids are also produced in the gastrointestinal tract, e.g., in the small intestine. On the basis of the mice model, it has been indicated that after 24 h fasting, the level of AEA in the GT increases sevenfold, which can affect the nutritional status, energy balance, lipoprotein metabolism, glucose homeostasis, and even nutritional behavior [39,72].
3. Mechanisms of Hunger and Satiety in Obesity
Obesity and its comorbidities, such as coronary heart disease, hypertension, gout, diabetes, or several types of cancers, result from excessive accumulation of adipose tissue, which stems from consuming much more energy than is necessary [77]. However, specific homeostasis helps to maintain proper body weight for a longer period. An increased calorie density of widely available foods can disrupt homeostasis, hence leading to obesity [78]. Interestingly, the balance system is more sensitive to hunger than to satiety, since in the past it was difficult to predict whether and when the next meal will be consumed. Therefore, a tolerance for excessive caloric intake is essential for the development of obesity and metabolic disorders. In fact, appetite is regulated by a system of central and peripheral signals that can modulate the individual reaction to the provided nutrients. A central control of food intake is controlled by the hypothalamus, brain stem, neuropeptide signaling systems, and monoaminergic, and endocannabinoid systems. A peripheral control of food intake involves gastrointestinal satiation signals through hormones like cholecystokinin (CCK), glucagon-like peptide 1 (GLP-1), and neuropeptide Y (NPY). Signals are transmitted to the solitary nucleus (SN) in the brain stem through the vagus nerve. Satiety, associated with a portion size, suppresses hunger and ends food intake. Physiological and psychological mechanisms release signals from different gastrointestinal tract locations, including the stomach, proximal and distal parts of the small intestine, and colon, to the brain [79]. Generally, satiety is defined as a period between meals without the feeling of hunger [80], which is impacted by both long-term signals from body energy storage and short-term signals from the gastrointestinal tract [81]. NPY constitutes an essential neurotransmitter in the brain, increasing during hunger and decreasing during a meal [82]. In the course of weight regain among people with obesity, its role is particularly essential, since body weight reduction reduces leptin concentrations and activates NPY, which is associated with hyperphagia and decreased energy usage. On the other hand, proopiomelanocortin (POMC) has an anorexigenic effect. Therefore, mutations in POMC are associated with increased food consumption and the development of obesity [83].
Endocannabinoids (EC) are anabolic lipid mediators responsible for increased food consumption, energy storage, and lower energy expenditure. They are essential in regulating hormonal and metabolic changes in obesity. For instance, in the mice brain, a selective CB1 receptor agonist suppressed food intake [84]. Additionally, the amount of CB1in the hypothalamus decreased following exposure to leptin. Thus, the orexigenic effect of CB1has been associated with the function of the peripheral neuronal system, regulated by leptin and associated with the development of overweight and obesity [85]. In fact, leptin reduces calcium inflow and further inhibits EBC synthesis, which reduces appetite [86]. Moreover, EC can also modulate energy intake through peripheral mechanisms not associated with appetite. This confirms the resistance to weight gain induced by diet in CB1 −/− mice as compared to wild-type mice fed with the same diet [62].
Taste, flavor, or texture stimulates food intake, but they are also essential in achieving the feeling of satiety. As food consumption progresses, signals from the GT (extending stomach wall, ghrelin, peptide hormones) and an increase in glucose levels lead to food consumption termination. However, food palatability stimulates further consumption and can increase a portion intake by 40% in comparison to taste-neutral products [87]. Waiting for a meal or eating time is associated with faster satiety [88]. Furthermore, mental work and sleep deprivation negatively affect satiety and increase the amount of consumed food by means of unstable glycemia and cortisol levels [89]. Moreover, the low*satiety phenotype, i.e., one of the phenotypes of appetite, which favors obesity has been found [90]. In addition, meal composition affects satiety, and according to research data, high-protein meals ensure higher satiety during body weight reduction [91]. In healthy, normal-weight individuals, the consumption of a high-protein diet is associated with higher and longer satiety during the day than the consumption of a diet with a regular amount of protein [92]. In fact, the consumption of protein products with carbohydrates stimulates GLP-1, which increases insulin secretion. Additionally, satiety following high-protein consumption is also associated with increased energy expenditure, which further increases oxygen consumption and body temperature, as well as promoting satiety [93].
4. Microbiota, Hunger, and Satiety in Obesity
Intestinal microbiota are a complex population of various microorganisms that can positively affect the human body. However, microbial changes may promote the development of several diseases, in particular metabolic diseases. Microbial changes affect the mechanisms of hunger and satiety, produce neuroactive substances and short-chain fatty acids (SCFA), and thus regulate nutritional behaviors associated with food consumption. Lactobacillus and Bifidobacterium strains are known to produce gamma-aminobutyric acid (GABA) [94], whereas L. reuteri produces histamine, and L. plantarum produces acetylcholine [95]. Furthermore, intestinal microorganisms can also moderate intestinal permeability and bile acid metabolism. In fact, studies on mice have shown that probiotic supplementation decreases hunger [96]. The brain–gut axis affects appetite and, therefore, affects the energy state of the host [97,98]. The concentration of catecholamines increases under the influence of β-glucuronidase, produced by bacteria, which can also affect satiety [99]. Additionally, gut bacteria can also modulate serotonin production, which affects gastrointestinal motility and intestinal peptide secretion [99].
A lower response to sweet and greasy flavor was observed in obesity, resulting in increased appetite for these flavors and their higher consumption [100]. Saccharine-sensitive rats have a different intestinal microbiota composition than rats less vulnerable to saccharine [101]. The activation of the immune system causes a decrease in taste receptor cells and taste buds in the tongue [102]. These changes in people with dysbiosis are initiated by the Toll-like receptor and interferon receptor (IFN) types I and II [103], and a similar effect is observed following the influence of lipopolysaccharides (LPS). On the other hand, the administration of LPS to mice results in lower expression of sweet taste receptors and a lower response for saccharose [104]. Moreover, dysbiosis among individuals with obesity increases intestinal permeability, serum lipopolysaccharide levels, and enhances the synthesis of CB1R and the expression of macrophages [105]. Furthermore, it increases the inflammatory state, the infiltration of pro-inflammatory macrophages in the adipose tissue, and the accumulation of adipose tissue. Conversely, the antagonists of CB1R decrease intestinal permeability and LPS levels [106].
In a study by Maria Isabel Queipo-Ortuñ, higher amounts of Proteobacteria and Bacteroidetes and lower amounts of Actinobacteria and Firmicutes were observed in rats fed a restrictive diet. Additionally, an increase in Lactobacillus and Bifidobacterium was observed in the group with physical activity. In fact, a positive correlation between the amount of Bifidobacterium, Lactobacillus, and leptin and a negative correlation between Clostridium, Bacteroidetes, Prevotella, and leptin were observed. On the other hand, ghrelin was negatively associated with the number of Bifidobacterium and Lactobacillus and positively associated with Bacteroidetes and Prevotella [107].
5. Cannabinoids/Endocannabinoid Control of Food Intake
ECS activity in the central nervous system—mostly in the limbic system and hypothalamus—is well documented. The endocannabinoid system plays an essential role in connecting gastrointestinal tract activity and the body’s energy economy [50]. The ECS works by increasing both appetite and the motivation to seek food. This mechanism is regulated by nourishment and anorexigenic transmitters produced by the hypothalamus, e.g., corticotropin-releasing hormone (CRH), melanin-concentrating hormone (MCH), and hypocretin [108,109].
It is assumed that the ECS operates at the cellular level by inhibiting neuronal stimulation and transmitters secretion into the synaptic gap [110]. The EC level in the hypothalamus is physiologically regulated by hormones reflecting the organism’s metabolic conditions, e.g., leptin, ghrelin, cholecystokinin, and glucocorticosteroids. The use of cannabinoids increases food intake [111]. Studies on rodents have indicated that those with 60% deficiency of CB1R in the hypothalamus are less sensitive to a non-nutritive effect of rimonabant (a selective agonist of CB1R, previously used as an anti-obesity treatment and then excluded due to multiple adverse reactions, mostly psychiatric). Interestingly, it has been suggested that the leptin effect in the hypothalamus is mostly associated with ECS signaling, since no leptin-induced appetite suppression effect was observed in rodents. Moreover, in another study, ghrelin also reduced this effect [54,112].
It has been suggested that several neuronal connections, directly related to eating behaviors, change their function from stimulation to obesity inhibition. Therefore, EC’s presynaptic inhibiting effect on the expression of transmitters stimulates the expression of pro-nourishing transmitters [54]. Considering that leptin negatively regulates the expression of CB1R in the hypothalamus and the fact that leptin resistance is common, leptin resistance impairs negative leptin control of the ECS at the hypothalamus level, causing an increase in subsequent pro-nourishing behaviors [4,85,113]. Moreover, the administration of the reverse CB1R agonist restores leptin sensitivity and has an anti-obesity effect in mice [114]. Other rodent studies revealed an increase of 2-AG in the hypothalamus following a high-fat diet (regardless of chronic or acute stimulation). The selective activation of CB1R in the central nervous system resulted in resistance to obesity induced by a high-fat diet. Moreover, the inactivation of CB1R in the central and sympathetic nervous systems caused an increase of thermogenesis [54,74,85,115,116].
The role of the limbic system in the control of food intake is mainly based on hedonistic fulfilment and needs—in this case, the estimation of taste and related behaviors. The nucleus accumbens, where endocannabinoid and opioid receptors are found, plays the most crucial role in assessing food type. Additionally, the nucleus accumbens has a unique link with the lateral hypothalamus, where the ECS performs a significant function [117,118]. In fact, it has been proven that dopamine activity in the nucleus accumbens is associated with the classification of hedonistic impulses and that CB1R blockage in this structure inhibits dopamine expression in response to pleasurable food [117,119]. Furthermore, the vagus nerve contains CB1R, CCK, and leptin receptors and is also responsible for maintaining homeostasis. It transfers information from organs to the locus coeruleus concerned with the regulation of digestive processes. CCK is secreted from the duodenum during eating and reduces food intake via the vagus nerve. In addition, leptin negatively regulates CB1R levels, also in vagus nerve endings, which suggests another theoretical ECS-related mechanism of reducing food consumption [85].
Moreover, chronic activation of CB1R may increase processes associated with hyperlipidemia, diabetes, or cardiovascular events among hedonic patients with obesity [20,120]. Furthermore, several dietary factors, e.g., dietary secondary metabolites, can affect the ECS, and high-calorie and high-fat diets can modulate the CB1/CB2 ratio and, thus, enhance food intake in several cases [121,122]. EC can also moderate food reward, whereas EC agonists can increase the palatability and hedonic value of food [123]. Interestingly, there is a possible 6-n-propylthiouracil (PROP) taste sensitivity association with the BMI, lipid parameters, and circulating endocannabinoids. Therefore, lower concentrations of AEA or 2-AG in normal-weight nontasters versus normal-weight supertasters can counteract the excess adipose tissue accumulation. In contrast, obesity can disrupt the abovementioned adaptive mechanism, since Carta et al. also noted an opposite correlation between plasma AEA and 2-AG concentrations, as well as the PROP phenotype. As a result, nontasters had 62% higher levels of endocannabinoids than supertasters [124]. It is worth mentioning that the ECS is also dysregulated in eating disorders, and EC dysregulation can be a modulating factor of rewarding binge-eating or self-starvation; however, data regarding this issue remains limited [125].
6. Genetic Determinants of Obesity in the Context of the Endocannabinoid System
The endocannabinoid system contributes to food control consumption through central and peripheral mechanisms. The ECS is involved in lipid and glucose metabolism control, lipogenesis stimulation, and visceral fat accumulation [126,127,128,129]. Since genetic factors modified by the environmental factors control body weight maintenance, genetic variants affecting the ECS may be essential subjects in the pathophysiology of obesity.
It is frequently suggested that the main factor contributing to varying degrees of obesity susceptibility may be epigenetics and gene expression [130,131,132]. First studies concerning the role of DNA methylation in obesity were conducted in 2013 by Xu et al., in which the authors identified several CpG sites and DNA methylation variances associated with obesity in young African Americans [133]. Most importantly, it was demonstrated that differential methylation and differential variability can determine the risk of obesity in approximately 70%in humans. Since then, research regarding the role of DNA methylation and histone modification in obesity has been initiated [133,134,135,136,137,138,139].
On the basis of these studies, researchers managed to identify tissues (adipose tissue, blood, skeletal muscle stem cells) and genes (ABCC3, GRB10, H19, MOGAT1, PDGFA, PRDM16, PRKCE, ATP10A, IRS1, JARID2, KCNQ1, ABCG1, FAM123C, FHL2, KLF14, PHOSPHO1, ZNF518B, ADCY5, CDKN1A, FTO, INS, KCNQ1, PDE7B, PDX1, PPARGC1A, SEPT9, SOCS2, TCF7L2) associated with obesity and related phenotypes (BMI, waist circumference). The determination of obesity susceptibility genes can contribute to the explanation of weight regulation mechanisms, food intake control, and fat distribution, potentially indicating new approaches to preventing and treating obesity [140].
Recent studies have shown that the endocannabinoid system can also be epigenetically modulated by drugs, alcohol, and diet. These modulations mainly include the CNR1 gene but also the hydrolyzing enzyme FAAH. The epigenetic modulations mechanisms concern global and gene-specific DNA methylation changes, histone acetylation and deacetylation, and the production of specific miRNAs [141,142,143,144,145,146].
It has been demonstrated that peripheral ECS activity is epigenetically modulated by diet. It turns out that the compound affecting the epigenetic modulation of CNR1 expression in vivo and in vitro is the commonly used extra virgin olive oil (EVOO), as evidenced by the ~50% reduction in CpG methylation status of the CNR1 promoter and expression of CB1R modulators, i.e., miR23A and mir-301a (involved in the pathogenesis of colorectal cancer) in rats exposed to short- and long-term dietary EVOO. Moreover, Francesco et al. showed that EVOO and its phenolic components were able to selectively regulate CNR1 gene expression in Caco-2 cells due to the hypermethylation of the CNR1 promoter. Interestingly, the frequency of CNR1 methylation is also quite high in human colorectal cancer and reaches about 77% and seems to be a relevant mechanism for cancer progression [147]. A study by Pucci et al. revealed a significant and selective increase in CNR1 gene expression in high-fat-diet rats at the beginning of obesity development and after 21 weeks of high dietary exposure, with a simultaneous selective and significant decrease in DNA methylation at specific CpG sites in both gene promoters in overweight rats [148]. In fact, CB1R is present in human subcutaneous adipocytes, encoded by the CNR1 gene, alterations in which, related to obesity traits, are frequently described in the literature. It is well established that CB1R activation leads to an increase in energy storage, which occurs via an increased motivation to consume food and to decreased satiety [149]. Increased levels of CB1R and endocannabinoids are observed during adipocyte differentiation. According to Ravinet Trillou et al., CNR1-deficient mice were lean and resilient to diet-induced obesity [150]. The dysregulation of the endocannabinoid system seems to play a crucial role in human obesity [149], which can be demonstrated by significant abdominal fat accumulation [151], as well as the fact that CNR1 gene variants are associated with an increased appetite, BMI, waist circumference, and skin-fold thickness, and even the appearance of metabolic syndrome [152,153]. The important role of the ECS in the pathophysiology of obesity can be proven by the fact that a blockade of CNR1 by means of rimonabant leads to a significant reduction in food intake and weight loss [154,155]. Moreover, these findings indicate that CNR1 gene antagonists improve glucose and lipid homeostasis, which occurs independently of weight loss, implying that CNR1 gene variability may contribute to obesity-related metabolic disorders in view of human obesity.
Benzinou et al. studied 26 single-nucleotide polymorphisms of CNR1, in which 12 showed nominal evidence of association with childhood obesity, class I and class II, and class III adult obesity. The study was conducted on 5750 patients and demonstrated that CNR1 gene variants increases the risk of obesity and modulates the BMI in the European population [152]. The impact of CNR1 genetic diversity on the BMI was also confirmed by other researches, who demonstrated that the rs1049353 mutant allele is associated with a lower BMI in European populations [156,157,158]. Moreover, it was found that in Caucasians suffering from anorexia or bulimia, the T allele is much more frequent in both homo- and heterozygous individuals than in healthy individuals [159]. Interestingly, homozygotes with the rs1049353-mutated allele correlated with a higher WHR and waist circumference (WC) in obese men and were associated with an increase in childhood obesity [160]. Consequently, it may suggest that CNR1-specific variants may constitute key elements in the understanding of the CB1R impact on feeding, fat accumulation, and susceptibility to increased adiposity. A previous review paper [143] regarding the role of ECS genetic polymorphisms in relation to obesity and diabetes was already published in 2019 by Doris et al. On the basis of the data from their review, we attempted to present an up-to-date table describing the associations between ECS obesity-related genes’ single-nucleotide polymorphism (Table 2) However, it is important to bear in mind research reports, such as Muller’s group, investigating eight polymorphic sites of the CNR1 gene (rs9353527, rs754387, rs6454676, rs806379, rs1535255, rs2023239, rs806370 and rs1049353), which do not confirm any association of the variants studied with regard to obesity in children and adolescents [161].

Table 2.
Associations found between a single-nucleotide polymorphism in ECS obesity-related genes.
The fact that the endocannabinoid system is closely related to the control of metabolism and energy balance has already been well documented. Due to the pressure in the brain, the CB1 receptor has been mainly considered as controlling glucose and lipid metabolism. Although its level of expression in peripheral cells was deficient, it appeared to influence increasing obesity. It can also be evidenced by the fact that the genetic ablation of CNR1 leads to weight loss, as well as selective blocking of the CB1 receptor, which leads to reduced food intake and body weight loss. Nevertheless, following the CB2 discovery as a peripheral receptor and its identification in different brain regions, including the hippocampus, the approach was changed [42,180,181]. CNR2 was rarely examined in view of obesity, since its locations in the liver, adipose tissue, and pancreatic islet cells have only recently been defined [4]. Romero-Zerbo et al. showed that the overexpression of cerebral CB2R affects body weight modulation, leading to a lean phenotype in mice [182]. Additionally, CB2 agonists can reduce food intake in lean mice, simultaneously improving weight gain and obesity-related inflammation in diet-induced obese mice [183]. It turns out that the frequently studied variant CB2, Q63R, which affects the reduction in CB2R function, is also associated with human nutrition disorders, eating behavior, and energy homeostasis.
Moreover, its genetic ablation leads to adiposity development [184]. Rossi et al. analyzed the effect of rs35761398 (Q63R) on CB2Ron obesity modulation in Italian children and adolescents. They found that the less functional missense variant R63 was significantly associated with a high z-score body mass index. Additionally, they showed that the CB2R reverse agonist AM630 increased inflammatory adipokine release and fat storage, whereas the JWH-133 agonist reversed all effects related to obesity [185]. In turn, Ketterer et al. investigated five tagging SNPs of the CNR2 locus (rs2229579, rs3123554, rs9424398, rs4625225, rs2501392) concerning the association with the BMI, weight, total body fat as a measure for adiposity, and the WHR as an estimation of body fat distribution. They observed a significant association of rs3123554 with weight (P additive inheritance model = 0.0062), as well as a lower BMI and body fat. Interestingly, the association with the BMI was limited to females, which may constitute evidence of the identified interactions between the ECS and sex hormones [186]. Other studies have also highlighted the role of the rs3123554 minor allele in the body weight, insulin and leptin higher levels, triglycerides, and homeostatic model assessment—insulin resistance (HOMA-IR) based on the example of the Spanish cohort [187]. Summarizing all the reports described above, we can conclude that CB2R may constitute a new pharmacological target for the treatment of obesity in the future. However, as the role of CB2 is still not fully understood, it requires intensive research.
Analyzing genes encoding enzymes involved in the synthesis or the degradation of endocannabinoids (FAAH, MAGL, DAGL, and NAPE-PLD), we found that any available studies described the association of MAGL and DAGL polymorphism and their role in the incidence of obesity, whereas FAAH was defined as an obesity-related factor. Sipe et al. showed that a naturally occurring missense polymorphism rs324420 (c.C385A) and the A/A genotype were associated with overweight and obesity in 2667 white (P = 0.005) and black (P = 0.05) subjects but not in Asians [174]. Yagin’s findings confirmed these results and demonstrated that the prevalence of the c.385A allele was more frequent in overweight/obese individuals, and the changes in the FAAH gene were associated with higher anthropometric indices, as well as the A/A genotype, which significantly increased the risk of obesity in Iranian women [176]. Moreover, the association of rs324420 with an increased risk of obesity and higher triglyceride levels was demonstrated in different European cohorts [175,187,188,189,190]. Additionally, Balsevich et al. demonstrated that an endocannabinoid-dependent signaling mechanism contributes to the hyperphagic actions of leptin, which increases FAAH activity and reduces AEA signaling in hypothalamic regions, leading to a reduced food demand. This mechanism is also modulated by the genetic variant C385A of the FAAH gene. It follows, therefore, that reducing leptin susceptibility to leptin in individuals with a mutated 385A allele may lead to an increased risk of developing obesity with the related metabolic complications [191].
On the other hand, we found reports that presented contradictory results, suggesting that FAAH gene polymorphism and mutant allele carrying were not related to overweight or obesity. Jansen et al. found no correlation between FAAH 385A allele Danish subjects and the BMI, WHR, WC, and HOMA-IR [192], as well as Papazoglou et al., who did not confirm the link to severe obesity with or without the diagnosis of metabolic syndrome in Greeks [193]. Nevertheless, rs324420 was associated with elevated anandamide levels in the Brazilian population, which may prove to support the cannabinoid antagonist treatment strategies in overweight-related disorders [194].
NAPE-PLD encodes one of the enzymes of endocannabinoid synthesis and participates in the production of anandamide, a CNR1 agonist. NAPE-PLD and other ECS components are the subject of research in terms of drug targets in the treatment of several diseases, including obesity and metabolic comorbidities. Wangensteen et al. showed strong evidence that a common haplotype in NAPE-PLD (rs13232194, rs17605251, rs11487077, rs12540583, rs6465903) was associated with severe obesity. Additionally, they observed that one SNP, rs17605251, in NAPE-PLD was nominally associated with BMI in Norwegians [195].
7. Summary and Conclusions
The importance of the endocannabinoid system in regulating metabolic pathways in the human body is increasingly becoming the subject of research. The discovery of CB1 and CB2 receptors, their agonists, and their antagonists has enabled research on the potential role of the EC system in various physiological and pathological processes, such as appetite regulation, energy balance, food intake, fat deposition, hepatic lipogenesis, and glucose homeostasis. This indicates that the ECS can be overactive in obese patients, thus promoting metabolic processes resulting in weight gain, lipogenesis, insulin resistance, and dyslipidemia. Therefore, innovative new obesity treatments are highly desirable, and blocking the endocannabinoid system seems to be a crucial solution. Studies demonstrated that selective CB1R agonists can be used for the pharmacological treatment of obesity. Rimonabant was introduced in the European Union in 2006 and was tested in three randomized clinical trials. The study was entitled Rimonabant in Obesity (RIO), in which its influence on body weight reduction among 5588 overweight (BMI > 27 ) and obese patients with comorbidities (dyslipidemia and hypertension) was assessed [196]. A significant weight reduction, an improvement in the serum lipid profile (RIO-lipids), an increase in HDL cholesterol, and a decrease in TG were observed [197]. Furthermore, in the RIO-Diab clinical trial, an improvement in insulin sensitivity and glycemic control and a decrease in fasting glucose levels, the HOMA-IR index, and glycated hemoglobin levels were also demonstrated [198]. Although RIO trials proved the safety of rimonabant, the approval was rejected, since it induced symptoms of depression as well as anxiety and resulted in other side effects (nausea, emesis, diarrhea, vertigo, and headaches). The negative influence of rimonabant on the gastrointestinal tract is associated with the blockade of CB1R [199]. At this point, it is worth mentioning that individuals with obesity have an increased risk of the more severe course of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection [200,201]. The use of rimonabant in order to decrease inflammation, a vital hallmark of obesity and SARS-CoV-2 infection, could provide a potential beneficial treatment in terms of a severe COVID-19 course [202]. Therefore, rimonabant use should be considered in clinical trials for patients with SARS-CoV-2 infection [203]. Although rimonabant was withdrawn from the market, attempts on testing other CB1R second-generation antagonists were made. URB447, i.e., a CB1R and CB2R antagonist, decreased the intake of food and body weight in mice (also peripherally) and was similar to rimonabant with regard to the polar surface and other physicochemical properties [204]. AM6545 was referred to as the neutral antagonist due its limited penetration to the brain [205], and its administration increased leptin sensitivity and the metabolic profile in obese mice, although it presented limited oral bioavailability. BPR697, reported by studies in the Health Research Institutes (NHRI) in Taiwan, exhibits a low brain-to-plasma concentration ratio (B/P = 1/23), similar to rimonabant [206]. BPR697 induced weight loss in diet-induced obese mice, without altered food intake, and decreased hepatic lipid accumulation. N-cyclohexyl-4-[1-(2,4-dichlorophenyl)-1-(p-Ttolyl)methyl]piperazine-1-carbo amide exhibited a lower B/P ratio than rimonabant, although it presented a similar effect on weight loss in diet-induced obese mice [207]. AJ5012 and AJ5018 were created due to a structural change in rimonabant. Nevertheless, although their B/P ratio was significantly lower than rimonabant, their ability to decrease adipose tissue inflammation was similar to rimonabant. However, their oral bioavailability remains to be investigated [208]. According to Matthews et al., a peripherally selective tetrahydroindazole derivative (2p compound), used in diet-induced obese mice, showed a beneficial effect on plasma glucose [209]. Zhang et al. discovered a new class of 6-benzhydryl-4-amino-quinolin-2-ones [210]. The 6a compound presented a long half-life following oral and intravenous administration; however, due to high affinity to rimonabant, it presented time-dependent brain accumulation. Nevertheless, this observation could be understated due to the use of non-perfused brains. The administration of the 6a compound resulted in weight loss and increased insulin sensitivity, even when lower doses were administered. These results are promising, although the neuropsychiatric safety of these compounds should be investigated further.
Taranabant is a CB1R inverse agonist the effectiveness of which was proven in preclinical trials—it resulted in effective weight loss in diet-induced obese rats when 30% of CB1R was occupied [211]. Phase III clinical trials on humans were stopped in 2008 due to the high level of CNS side effects, mainly depression and anxiety [212,213]. In recent years, many CB1R-selective drugs have been withdrawn at different phases of clinical trials. Drinabant, a highly selective CB1R agonist, presented anti-depression and food-limiting effects in animal models and reached phase IIb clinical trials, but it was shortly withdrawn since it induced symptoms of severe psychiatric disorders in humans [211,214,215]. Failures of clinical trials limited the studies on humans, and currently, CB1R agonist are usually tested in laboratory conditions.
In the study by Radiszewska et al. on Wistar rats, a stimulation of peripheral CB1R by its agonist (WIN 55,212-2) had an anorexigenic effect and induced activity of exendin-4, a peptide agonist of the glucagon-like-peptide 1 [216]. It suggests a double activity of the ECS and could be used in the pharmacotherapy of obesity.
Studies conducted by Palomba et al. indicated that the activation of CB1R resulted in overexpression of PPAR-γ in adipocytes, thus suggesting a potential role of thiazolidinediones in this mechanism [51,217].
Taking into consideration the undeniable role of CB1R in the development of obesity and the role of CB1R agonists in obesity treatment, it is essential to further develop the research on CB1R-active substances, which have great potential in the treatment of obesity and obesity-related comorbidities.
It has been proven that exogenous factors are not the only elements responsible for the dysregulation of nutritional homeostasis. Our review presented evidence that there is a link between ECS gene polymorphisms and the risk of obesity. Research on ECS dysfunction could provide more precise knowledge of both the pathogenesis and the mechanisms of obesity, as well as provide new therapeutic programs. Previously introduced ECS-related therapeutic programs have been withdrawn due to mental disorders they resulted in; however, the endocannabinoid system remains the subject of numerous research studies.
Author Contributions
Conceptualization, I.K.-K., S.H. and P.S.; writing—original draft preparation, P.S., S.H. and A.M.R.; writing—review and editing—P.S., S.H., A.M.R., A.Z., R.S., A.D. and I.K.-K.; visualization—A.M.R., S.H., A.Z. and I.K.-K.; supervision—I.K.-K.; project administration—I.K.-K., A.D. and R.S.; and funding acquisition—I.K.-K. and A.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available in a publicly accessible. The data presented in this study are openly available in Medline and PubMed databases and on the publisher’s website. The keywords that were used: endocannabinoid system; ECS, obesity; cannabinoid receptors; obesity pathogenesis, and epigenetics of obesity. All data in the text are quoted and all works used are listed in the bibliography along with doi and reference numbers.
Acknowledgments
Figures were created with BioRender.com.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Batsis, J.A.; Villareal, D.T. Sarcopenic obesity in older adults: Aetiology, epidemiology and treatment strategies. Nat. Rev. Endocrinol. 2018, 14, 513–537. [Google Scholar] [CrossRef]
- Neeland, I.J.; Poirier, P.; Després, J.-P. Cardiovascular and metabolic heterogeneity of obesity: Clinical challenges and implications for management. Circulation 2018, 137, 1391–1406. [Google Scholar] [CrossRef] [PubMed]
- Martin-Calvo, N.; Moreno-Galarraga, L.; Martinez-Gonzalez, M.A. Association between body mass index, waist-to-height ratio and adiposity in children: A systematic review and meta-analysis. Nutrients 2016, 8, 512. [Google Scholar] [CrossRef] [PubMed]
- Rossi, F.; Punzo, F.; Umano, G.R.; Argenziano, M.; Miraglia Del Giudice, E. Role of cannabinoids in obesity. Int. J. Mol. Sci. 2018, 19, 2690. [Google Scholar] [CrossRef] [PubMed]
- WHO (World Health Organization). Available online: https://www.who.int/ (accessed on 2 August 2020).
- Schetz, M.; De Jong, A.; Deane, A.M.; Druml, W.; Hemelaar, P.; Pelosi, P.; Pickkers, P.; Reintam-Blaser, A.; Roberts, J.; Sakr, Y.; et al. Obesity in the critically ill: A narrative review. Intensive Care Med. 2019, 45, 757–769. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, E.A.; Khavjou, O.A.; Thompson, H.; Trogdon, J.G.; Pan, L.; Sherry, B.; Dietz, W. Obesity and severe obesity forecasts through. Am. J. Prev. Med. 2012, 42, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Di Cesare, M.; Sorić, M.; Bovet, P.; Miranda, J.J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.-P.; Bentham, J. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019, 17. [Google Scholar] [CrossRef]
- Freedman, D.S.; Khan, L.K.; Dietz, W.H.; Srinivasan, S.R.; Berenson, G.S. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: The bogalusa heart study. Pediatrics 2001, 108, 712–718. [Google Scholar] [CrossRef]
- Taveras, E.M.; Rifas-Shiman, S.L.; Belfort, M.B.; Kleinman, K.P.; Oken, E.; Gillman, M.W. Weight status in the first 6 months of life and obesity at 3 years of age. Pediatrics 2009, 123, 1177–1183. [Google Scholar] [CrossRef]
- Debédat, J.; Clément, K.; Aron-Wisnewsky, J. Gut microbiota dysbiosis in human obesity: Impact of bariatric surgery. Curr. Obes. Rep. 2019, 8, 229–242. [Google Scholar] [CrossRef]
- Abenavoli, L.; Scarpellini, E.; Colica, C.; Boccuto, L.; Salehi, B.; Sharifi-Rad, J.; Aiello, V.; Romano, B.; De Lorenzo, A.; Izzo, A.A.; et al. Gut microbiota and obesity: A role for probiotics. Nutrients 2019, 11, 2690. [Google Scholar] [CrossRef] [PubMed]
- Prevalence of Obesity among Adults, BMI >= 30 (Crude Estimate) (%). Available online: https://www.who.int/data/maternal-newborn-child-adolescent/monitor (accessed on 2 August 2020).
- Smith, K.B.; Smith, M.S. Obesity statistics. Prim. Care 2016, 43, 121–135. [Google Scholar] [CrossRef] [PubMed]
- Chooi, Y.C.; Ding, C.; Magkos, F. The epidemiology of obesity. Metab. Clin. Exp. 2019, 92, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Yumuk, V.; Tsigos, C.; Fried, M.; Schindler, K.; Busetto, L.; Micic, D.; Toplak, H. Obesity management task force of the European Association for the study of obesity European guidelines for obesity management in adults. Obes. Facts 2015, 8, 402–424. [Google Scholar] [CrossRef] [PubMed]
- Misra, A.; Jayawardena, R.; Anoop, S. Obesity in South Asia: Phenotype, morbidities, and mitigation. Curr. Obes. Rep. 2019, 8, 43–52. [Google Scholar] [CrossRef]
- Ahima, R.S.; Antwi, D.A. Brain regulation of appetite and satiety. Endocrinol. Metab. Clin. North Am. 2008, 37, 811–823. [Google Scholar] [CrossRef]
- Lenard, N.R.; Berthoud, H.-R. Central and peripheral regulation of food intake and physical activity: Pathways and genes. Obesity (Silver Spring) 2008, 16, S11–S22. [Google Scholar] [CrossRef]
- Di Marzo, V. The endocannabinoid system in obesity and type 2 diabetes. Diabetologia 2008, 51, 1356. [Google Scholar] [CrossRef]
- Crocq, M.-A. History of cannabis and the endocannabinoid system. Dialogues Clin. Neurosci 2020, 22, 223–228. [Google Scholar] [CrossRef]
- Matsuda, L.A.; Lolait, S.J.; Brownstein, M.J.; Young, A.C.; Bonner, T.I. Structure of a cannabinoid receptor and functional expression of the cloned CDNA. Nature 1990, 346, 561–564. [Google Scholar] [CrossRef]
- Gérard, C.M.; Mollereau, C.; Vassart, G.; Parmentier, M. Molecular cloning of a human cannabinoid receptor which is also expressed in testis. Biochem. J. 1991, 279, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Munro, S.; Thomas, K.L.; Abu-Shaar, M. Molecular characterization of a peripheral receptor for cannabinoids. Nature 1993, 365, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Bisogno, T.; Hanus, L.; De Petrocellis, L.; Tchilibon, S.; Ponde, D.E.; Brandi, I.; Moriello, A.S.; Davis, J.B.; Mechoulam, R.; Di Marzo, V. Molecular targets for cannabidiol and its synthetic analogues: Effect on vanilloid VR1 receptors and on the cellular uptake and enzymatic hydrolysis of anandamide. Br. J. Pharm. 2001, 134, 845–852. [Google Scholar] [CrossRef] [PubMed]
- Ryberg, E.; Larsson, N.; Sjögren, S.; Hjorth, S.; Hermansson, N.-O.; Leonova, J.; Elebring, T.; Nilsson, K.; Drmota, T.; Greasley, P.J. The orphan receptor GPR55 is a novel cannabinoid receptor. Br. J. Pharm. 2007, 152, 1092–1101. [Google Scholar] [CrossRef] [PubMed]
- Befort, K. Interactions of the opioid and cannabinoid systems in reward: Insights from knockout studies. Front. Pharm. 2015, 6. [Google Scholar] [CrossRef]
- Meadows, A.; Lee, J.H.; Wu, C.-S.; Wei, Q.; Pradhan, G.; Yafi, M.; Lu, H.-C.; Sun, Y. Deletion of G-protein-coupled receptor 55 promotes obesity by reducing physical activity. Int. J. Obes. (London) 2016, 40, 417–424. [Google Scholar] [CrossRef]
- Baskaran, P.; Krishnan, V.; Ren, J.; Thyagarajan, B. Capsaicin induces browning of white adipose tissue and counters obesity by activating TRPV1 channel-dependent mechanisms. Br. J. Pharm. 2016, 173, 2369–2389. [Google Scholar] [CrossRef]
- Christie, S.; Wittert, G.A.; Li, H.; Page, A.J. Involvement of TRPV1 channels in energy homeostasis. Front. Endocrinol. 2018, 9, 420. [Google Scholar] [CrossRef]
- Hryhorowicz, S.; Kaczmarek-Ryś, M.; Andrzejewska, A.; Staszak, K.; Hryhorowicz, M.; Korcz, A.; Słomski, R. Allosteric modulation of cannabinoid receptor 1—Current challenges and future opportunities. Int. J. Mol. Sci. 2019, 20, 5874. [Google Scholar] [CrossRef]
- Mechoulam, R.; Ben-Shabat, S.; Hanus, L.; Ligumsky, M.; Kaminski, N.E.; Schatz, A.R.; Gopher, A.; Almog, S.; Martin, B.R.; Compton, D.R. Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochem. Pharm. 1995, 50, 83–90. [Google Scholar] [CrossRef]
- Biernacki, M.; Skrzydlewska, E. Metabolizm endokannabinoidów. Postepy Hig. Med. Dosw. 2016, 70, 830–843. [Google Scholar] [CrossRef] [PubMed]
- Porter, A.C.; Sauer, J.-M.; Knierman, M.D.; Becker, G.W.; Berna, M.J.; Bao, J.; Nomikos, G.G.; Carter, P.; Bymaster, F.P.; Leese, A.B.; et al. Characterization of a novel endocannabinoid, virodhamine, with antagonist activity at the CB1 receptor. J. Pharm. Exp. 2002, 301, 1020–1024. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Pang, Z. Endocannabinoids and obesity. Vitam. Horm. 2013, 91, 325–368. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumi, T.; Matsuda, R.; Morito, K.; Kawabata, K.; Yokota, M.; Nikawadori, M.; Inoue-Fujiwara, M.; Kawashima, S.; Hidaka, M.; Yamamoto, T.; et al. Identification of human glycerophosphodiesterase 3 as an ecto phospholipase C that converts the G protein-coupled receptor 55 agonist lysophosphatidylinositol to bioactive monoacylglycerols in cultured mammalian cells. Biochim. Biophys Acta Mol. Cell Biol. Lipids 2020, 1865, 158761. [Google Scholar] [CrossRef] [PubMed]
- Briand-Mésange, F.; Pons, V.; Allart, S.; Masquelier, J.; Chicanne, G.; Beton, N.; Payrastre, B.; Muccioli, G.G.; Ausseil, J.; Davignon, J.-L.; et al. Glycerophosphodiesterase 3 (GDE3) is a lysophosphatidylinositol-specific ectophospholipase C acting as an endocannabinoid signaling switch. J. Biol. Chem. 2020, 295, 15767–15781. [Google Scholar] [CrossRef]
- Mackie, K. Distribution of Cannabinoid Receptors in the Central and Peripheral Nervous System; Handbook Experimental Pharmacology; Springer: Berlin, Germany, 2005; pp. 299–325. [Google Scholar] [CrossRef]
- Perkins, J.M.; Davis, S.N. Endocannabinoid System overactivity and the metabolic syndrome: Prospects for treatment. Curr. Diab. Rep. 2008, 8, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Kendall, D.A.; Yudowski, G.A. Cannabinoid receptors in the central nervous system: Their signaling and roles in disease. Front. Cell Neurosci. 2017, 10. [Google Scholar] [CrossRef]
- Matias, I.; Di Marzo, V. Endocannabinoids and the control of energy balance. Trends Endocrinol. Metab. 2007, 18, 27–37. [Google Scholar] [CrossRef]
- Onaivi, E.S.; Ishiguro, H.; Gong, J.-P.; Patel, S.; Perchuk, A.; Meozzi, P.A.; Myers, L.; Mora, Z.; Tagliaferro, P.; Gardner, E.; et al. Discovery of the presence and functional expression of cannabinoid CB2 receptors in brain. Ann. N. Y. Acad. Sci. 2006, 1074, 514–536. [Google Scholar] [CrossRef]
- Zou, S.; Kumar, U. Cannabinoid receptors and the endocannabinoid system: Signaling and function in the central nervous system. Int. J. Mol. Sci. 2018, 19, 833. [Google Scholar] [CrossRef]
- Ye, L.; Cao, Z.; Wang, W.; Zhou, N. New insights in cannabinoid receptor structure and signaling. Curr. Mol. Pharm. 2019, 12, 239–248. [Google Scholar] [CrossRef] [PubMed]
- Bie, B.; Wu, J.; Foss, J.F.; Naguib, M. An overview of the cannabinoid type 2 receptor system and its therapeutic potential. Curr. Opin. Anaesthesiol. 2018, 31, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Dhopeshwarkar, A.; Mackie, K. CB2 Cannabinoid receptors as a therapeutic target-what does the future hold? Mol. Pharm. 2014, 86, 430–437. [Google Scholar] [CrossRef] [PubMed]
- Home-Gene-NCBI. Available online: https://www.ncbi.nlm.nih.gov/gene (accessed on 2 August 2020).
- Kargl, J.; Balenga, N.; Parzmair, G.P.; Brown, A.J.; Heinemann, A.; Waldhoer, M. The cannabinoid receptor CB1 modulates the signaling properties of the lysophosphatidylinositol receptor GPR55. Biol. Chem. 2012, 287, 44234–44248. [Google Scholar] [CrossRef]
- Atwood, B.K.; Mackie, K. CB2: A Cannabinoid receptor with an identity crisis. Br. J. Pharm. 2010, 160, 467–479. [Google Scholar] [CrossRef]
- Kirkham, T.C.; Williams, C.M.; Fezza, F.; Di Marzo, V. Endocannabinoid levels in rat limbic forebrain and hypothalamus in relation to fasting, feeding and satiation: Stimulation of eating by 2-arachidonoyl glycerol. Br. J. Pharm. 2002, 136, 550–557. [Google Scholar] [CrossRef]
- Matias, I.; Gonthier, M.-P.; Orlando, P.; Martiadis, V.; De Petrocellis, L.; Cervino, C.; Petrosino, S.; Hoareau, L.; Festy, F.; Pasquali, R.; et al. Regulation, function, and dysregulation of endocannabinoids in models of adipose and beta-pancreatic cells and in obesity and hyperglycemia. J. Clin. Endocrinol. Metab. 2006, 91, 3171–3180. [Google Scholar] [CrossRef]
- Gary-Bobo, M.; Elachouri, G.; Scatton, B.; Le Fur, G.; Oury-Donat, F.; Bensaid, M. The cannabinoid CB1 receptor antagonist rimonabant (SR141716) inhibits cell proliferation and increases markers of adipocyte maturation in cultured mouse 3T3 F442A preadipocytes. Mol. Pharm. 2006, 69, 471–478. [Google Scholar] [CrossRef]
- Pagano, C.; Pilon, C.; Calcagno, A.; Urbanet, R.; Rossato, M.; Milan, G.; Bianchi, K.; Rizzuto, R.; Bernante, P.; Federspil, G.; et al. The endogenous cannabinoid system stimulates glucose uptake in human fat cells via phosphatidylinositol 3-kinase and calcium-dependent mechanisms. J. Clin. Endocrinol. Metab. 2007, 92, 4810–4819. [Google Scholar] [CrossRef]
- Silvestri, C.; Di Marzo, V. The endocannabinoid system in energy homeostasis and the etiopathology of metabolic disorders. Cell Metab. 2013, 17, 475–490. [Google Scholar] [CrossRef]
- Cota, D.; Marsicano, G.; Tschöp, M.; Grübler, Y.; Flachskamm, C.; Schubert, M.; Auer, D.; Yassouridis, A.; Thöne-Reineke, C.; Ortmann, S.; et al. The endogenous cannabinoid system affects energy balance via central orexigenic drive and peripheral lipogenesis. J. Clin. Investig. 2003, 112, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Bajzer, M.; Olivieri, M.; Haas, M.K.; Pfluger, P.T.; Magrisso, I.J.; Foster, M.T.; Tschöp, M.H.; Krawczewski-Carhuatanta, K.A.; Cota, D.; Obici, S. Cannabinoid receptor 1 (CB1) antagonism enhances glucose utilisation and activates brown adipose tissue in diet-induced obese mice. Diabetologia 2011, 54, 3121–3131. [Google Scholar] [CrossRef] [PubMed]
- Verty, A.N.A.; Allen, A.M.; Oldfield, B.J. The Effects of rimonabant on brown adipose tissue in rat: Implications for energy expenditure. Obesity 2009, 17, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, O.; Mikkola, K.; Espes, D.; Tuominen, L.; Virtanen, K.; Forsback, S.; Haaparanta-Solin, M.; Hietala, J.; Solin, O.; Nuutila, P. The cannabinoid receptor-1 is an imaging biomarker of brown adipose tissue. J. Nucl. Med. 2015, 56, 1937–1941. [Google Scholar] [CrossRef]
- Boon, M.R.; Kooijman, S.; van Dam, A.D.; Pelgrom, L.R.; Berbée, J.F.P.; Visseren, C.A.R.; Aggele, R.C.v.; van den Hoek, A.M.; Sips, H.C.M.; Lombès, M.; et al. Peripheral cannabinoid 1 receptor blockade activates brown adipose tissue and diminishes dyslipidemia and obesity. FASEB J. 2014, 28, 5361–5375. [Google Scholar] [CrossRef]
- Lahesmaa, M.; Eriksson, O.; Gnad, T.; Oikonen, V.; Bucci, M.; Hirvonen, J.; Koskensalo, K.; Teuho, J.; Niemi, T.; Taittonen, M.; et al. Cannabinoid type 1 receptors are upregulated during acute activation of brown adipose tissue. Diabetes 2018, 67, 1226–1236. [Google Scholar] [CrossRef]
- Woods, S.C. Role of the endocannabinoid system in regulating cardiovascular and metabolic risk factors. Am. J. Med. 2007, 120, S19–S25. [Google Scholar] [CrossRef]
- Osei-Hyiaman, D.; DePetrillo, M.; Pacher, P.; Liu, J.; Radaeva, S.; Bátkai, S.; Harvey-White, J.; Mackie, K.; Offertáler, L.; Wang, L.; et al. Endocannabinoid activation at hepatic CB1 receptors stimulates fatty acid synthesis and contributes to diet-induced obesity. J. Clin. Investig. 2005, 115, 1298–1305. [Google Scholar] [CrossRef]
- Medina, J.; Fernández-Salazar, L.I.; García-Buey, L.; Moreno-Otero, R. Approach to the pathogenesis and treatment of nonalcoholic steatohepatitis. Diabetes Care 2004, 27, 2057–2066. [Google Scholar] [CrossRef]
- Jeong, W.; Osei-Hyiaman, D.; Park, O.; Liu, J.; Bátkai, S.; Mukhopadhyay, P.; Horiguchi, N.; Harvey-White, J.; Marsicano, G.; Lutz, B.; et al. Paracrine activation of hepatic CB1 receptors by stellate cell-derived endocannabinoids mediates alcoholic fatty liver. Cell Metab. 2008, 7, 227–235. [Google Scholar] [CrossRef]
- Ruby, M.A.; Nomura, D.K.; Hudak, C.S.S.; Barber, A.; Casida, J.E.; Krauss, R.M. Acute overactive endocannabinoid signaling induces glucose intolerance, hepatic steatosis, and novel cannabinoid receptor 1 responsive genes. PLoS ONE 2011, 6, e26415. [Google Scholar] [CrossRef] [PubMed]
- Yamauchi, T.; Kamon, J.; Minokoshi, Y.; Ito, Y.; Waki, H.; Uchida, S.; Yamashita, S.; Noda, M.; Kita, S.; Ueki, K.; et al. Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating amp-activated protein kinase. Nat. Med. 2002, 8, 1288–1295. [Google Scholar] [CrossRef] [PubMed]
- Trebicka, J.; Racz, I.; Siegmund, S.V.; Cara, E.; Granzow, M.; Schierwagen, R.; Klein, S.; Wojtalla, A.; Hennenberg, M.; Huss, S.; et al. Role of cannabinoid receptors in alcoholic hepatic injury: Steatosis and fibrogenesis are increased in CB2 receptor-deficient mice and decreased in CB1 receptor knockouts. Liver Int. 2011, 31, 860–870. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.L.; Connoley, I.P.; Wilson, C.A.; Stock, M.J. Effects of the cannabinoid CB1 receptor antagonist SR141716 on oxygen consumption and soleus muscle glucose uptake in Lep(Ob)/Lep(Ob) mice. Int. J. Obes. (London) 2005, 29, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Song, D.; Bandsma, R.H.J.; Xiao, C.; Xi, L.; Shao, W.; Jin, T.; Lewis, G.F. Acute cannabinoid receptor type 1 (CB1R) modulation influences insulin sensitivity by an effect outside the central nervous system in mice. Diabetologia 2011, 54, 1181–1189. [Google Scholar] [CrossRef]
- Juan-Picó, P.; Fuentes, E.; Bermúdez-Silva, F.J.; Javier Díaz-Molina, F.; Ripoll, C.; Rodríguez de Fonseca, F.; Nadal, A. Cannabinoid receptors regulate Ca(2+) signals and insulin secretion in pancreatic beta-cell. Cell Calcium 2006, 39, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Starowicz, K.M.; Cristino, L.; Matias, I.; Capasso, R.; Racioppi, A.; Izzo, A.A.; Di Marzo, V. Endocannabinoid dysregulation in the pancreas and adipose tissue of mice fed with a high-fat diet. Obesity (Silver Spring) 2008, 16, 553–565. [Google Scholar] [CrossRef]
- Gómez, R.; Navarro, M.; Ferrer, B.; Trigo, J.M.; Bilbao, A.; Arco, I.D.; Cippitelli, A.; Nava, F.; Piomelli, D.; de Fonseca, F.R. A peripheral mechanism for CB1 cannabinoid receptor-dependent modulation of feeding. J. Neurosci. 2002, 22, 9612–9617. [Google Scholar] [CrossRef]
- Coutts, A.A.; Izzo, A.A. The gastrointestinal pharmacology of cannabinoids: An update. Curr. Opin. Pharm. 2004, 4, 572–579. [Google Scholar] [CrossRef]
- Pang, Z.; Wu, N.N.; Zhao, W.; Chain, D.C.; Schaffer, E.; Zhang, X.; Yamdagni, P.; Palejwala, V.A.; Fan, C.; Favara, S.G.; et al. The central cannabinoid CB1 receptor is required for diet-induced obesity and rimonabant’s antiobesity effects in mice. Obesity (Silver Spring) 2011, 19, 1923–1934. [Google Scholar] [CrossRef]
- DiPatrizio, N.V.; Astarita, G.; Schwartz, G.; Li, X.; Piomelli, D. Endocannabinoid signal in the gut controls dietary fat intake. Proc. Natl. Acad. Sci. USA 2011, 108, 12904–12908. [Google Scholar] [CrossRef] [PubMed]
- Argueta, D.A.; DiPatrizio, N.V. Peripheral endocannabinoid signaling controls hyperphagia in western diet-induced obesity. Physiol. Behav. 2017, 171, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Iyengar, N.M.; Gucalp, A.; Dannenberg, A.J.; Hudis, C.A. Obesity and cancer mechanisms: Tumor microenvironment and inflammation. J. Clin. Oncol. 2016, 34, 4270–4276. [Google Scholar] [CrossRef] [PubMed]
- Bray, G.A.; Smith, S.R.; DeJonge, L.; de Souza, R.; Rood, J.; Champagne, C.M.; Laranjo, N.; Carey, V.; Obarzanek, E.; Loria, C.M.; et al. Effect of diet composition on energy expenditure during weight loss: The pounds lost study. Int. J. Obes. (London) 2012, 36, 448–455. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Keenan, G.S.; Brunstrom, J.M.; Ferriday, D. Effects of meal variety on expected satiation: Evidence for a ‘Perceived Volume’ heuristic. Appetite 2015, 89, 10–15. [Google Scholar] [CrossRef]
- Strubbe, J.H.; Woods, S.C. The timing of meals. Psychol. Rev. 2004, 111, 128–141. [Google Scholar] [CrossRef]
- Woods, S.C. Signals that influence food intake and body weight. Physiol. Behav. 2005, 86, 709–716. [Google Scholar] [CrossRef]
- Wynne, K.; Stanley, S.; McGowan, B.; Bloom, S. Appetite control. J. Endocrinol. 2005, 184, 291–318. [Google Scholar] [CrossRef]
- Krude, H.; Biebermann, H.; Luck, W.; Horn, R.; Brabant, G.; Grüters, A. Severe early-onset obesity, adrenal insufficiency and red hair pigmentation caused by POMC mutations in humans. Nat. Genet. 1998, 19, 155–157. [Google Scholar] [CrossRef]
- Colombo, G.; Agabio, R.; Diaz, G.; Lobina, C.; Reali, R.; Gessa, G.L. Appetite suppression and weight loss after the cannabinoid antagonist SR. Life Sci. 1998, 63, PL113–PL117. [Google Scholar] [CrossRef]
- Di Marzo, V.; Goparaju, S.K.; Wang, L.; Liu, J.; Bátkai, S.; Járai, Z.; Fezza, F.; Miura, G.I.; Palmiter, R.D.; Sugiura, T.; et al. Leptin-regulated endocannabinoids are involved in maintaining food intake. Nature 2001, 410, 822–825. [Google Scholar] [CrossRef] [PubMed]
- Jo, Y.-H.; Chen, Y.-J.J.; Chua, S.C.; Talmage, D.A.; Role, L.W. Integration of endocannabinoid and leptin signaling in an appetite-related neural circuit. Neuron 2005, 48, 1055–1066. [Google Scholar] [CrossRef] [PubMed]
- De Castro, J.M.; Bellisle, F.; Dalix, A.M.; Pearcey, S.M. Palatability and intake relationships in free-living humans. characterization and independence of influence in North Americans. Physiol. Behav. 2000, 70, 343–350. [Google Scholar] [CrossRef]
- Brunstrom, J.M. The Control of meal size in human subjects: A role for expected satiety, expected satiation and premeal planning. Proc. Nutr. Soc. 2011, 70, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.-P.; Drapeau, V.; Poirier, P.; Teasdale, N.; Tremblay, A. Glycemic instability and spontaneous energy intake: Association with knowledge-based work. Psychosom. Med. 2008, 70, 797–804. [Google Scholar] [CrossRef]
- Müller, M.J.; Geisler, C.; Hübers, M.; Pourhassan, M.; Bosy-Westphal, A. body composition-related functions: A problem-oriented approach to phenotyping. Eur. J. Clin. Nutr. 2019, 73, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Westerterp-Plantenga, M.S.; Nieuwenhuizen, A.; Tomé, D.; Soenen, S.; Westerterp, K.R. Dietary protein, weight loss, and weight maintenance. Annu. Rev. Nutr. 2009, 29, 21–41. [Google Scholar] [CrossRef] [PubMed]
- Hochstenbach-Waelen, A.; Veldhorst, M.A.B.; Nieuwenhuizen, A.G.; Westerterp-Plantenga, M.S.; Westerterp, K.R. Comparison of 2 diets with either 25% or 10% of energy as casein on energy expenditure, substrate balance, and appetite profile. Am. J. Clin. Nutr. 2009, 89, 831–838. [Google Scholar] [CrossRef]
- Westerterp-Plantenga, M.S.; Lejeune, M.P.G.M.; Smeets, A.J.P.G.; Luscombe-Marsh, N.D. Sex differences in energy homeostatis following a diet relatively high in protein exchanged with carbohydrate, assessed in a respiration chamber in humans. Physiol. Behav. 2009, 97, 414–419. [Google Scholar] [CrossRef]
- Barrett, E.; Ross, R.P.; O’Toole, P.W.; Fitzgerald, G.F.; Stanton, C. γ-Aminobutyric acid production by culturable bacteria from the human intestine. J. Appl. Microbiol. 2012, 113, 411–417. [Google Scholar] [CrossRef]
- Hemarajata, P.; Spinler, J.K.; Balderas, M.A.; Versalovic, J. Identification of a proton-chloride antiporter (EriC) by himar1 transposon mutagenesis in lactobacillus reuteri and its role in histamine production. Antonie Van Leeuwenhoek 2014, 105, 579–592. [Google Scholar] [CrossRef] [PubMed]
- Dock, D.B.; Latorraca, M.Q.; Aguilar-Nascimento, J.E.; Gomes-da-Silva, M.H.G. Probiotics enhance recovery from malnutrition and lessen colonic mucosal atrophy after short-term fasting in rats. Nutrition 2004, 20, 473–476. [Google Scholar] [CrossRef] [PubMed]
- Bauer, P.V.; Hamr, S.C.; Duca, F.A. Regulation of energy balance by a gut-brain axis and involvement of the gut microbiota. Cell. Mol. Life Sci. 2016, 73, 737–755. [Google Scholar] [CrossRef] [PubMed]
- Foster, J.A.; Lyte, M.; Meyer, E.; Cryan, J.F. Gut microbiota and brain function: An evolving field in neuroscience. Int. J. Neuropsychopharmacol. 2016, 19. [Google Scholar] [CrossRef] [PubMed]
- Asano, Y.; Hiramoto, T.; Nishino, R.; Aiba, Y.; Kimura, T.; Yoshihara, K.; Koga, Y.; Sudo, N. Critical role of gut microbiota in the production of biologically active, free catecholamines in the gut lumen of mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2012, 303, G1288–G1295. [Google Scholar] [CrossRef]
- Berthoud, H.-R.; Zheng, H. Modulation of taste responsiveness and food preference by obesity and weight loss. Physiol. Behav. 2012, 107, 527–532. [Google Scholar] [CrossRef]
- Lyte, M.; Fodor, A.A.; Chapman, C.D.; Martin, G.G.; Perez-Chanona, E.; Jobin, C.; Dess, N.K. Gut microbiota and a selectively bred taste phenotype: A novel model of microbiome-behavior relationships. Psychosom. Med. 2016, 78, 610–619. [Google Scholar] [CrossRef]
- Kim, K.-A.; Yoo, H.H.; Gu, W.; Yu, D.-H.; Jin, M.J.; Choi, H.-L.; Yuan, K.; Guerin-Deremaux, L.; Kim, D.-H. Effect of a soluble prebiotic fiber, NUTRIOSE, on the absorption of ginsenoside Rd in rats orally administered ginseng. J. Ginseng Res. 2014, 38, 203–207. [Google Scholar] [CrossRef]
- Wang, H.; Zhou, M.; Brand, J.; Huang, L. Inflammation and taste disorders. Ann. N. Y. Acad. Sci. 2009, 1170, 596–603. [Google Scholar] [CrossRef]
- Zhu, X.; He, L.; McCluskey, L.P. Ingestion of bacterial lipopolysaccharide inhibits peripheral taste responses to sucrose in mice. Neuroscience 2014, 258, 47–61. [Google Scholar] [CrossRef]
- Muccioli, G.G.; Naslain, D.; Bäckhed, F.; Reigstad, C.S.; Lambert, D.M.; Delzenne, N.M.; Cani, P.D. The endocannabinoid system links gut microbiota to adipogenesis. Mol. Syst. Biol. 2010, 6, 392. [Google Scholar] [CrossRef] [PubMed]
- Mehrpouya-Bahrami, P.; Chitrala, K.N.; Ganewatta, M.S.; Tang, C.; Murphy, E.A.; Enos, R.T.; Velazquez, K.T.; McCellan, J.; Nagarkatti, M.; Nagarkatti, P. Blockade of CB1 cannabinoid receptor alters gut microbiota and attenuates inflammation and diet-induced obesity. Sci. Rep. 2017, 7, 15645. [Google Scholar] [CrossRef] [PubMed]
- Queipo-Ortuño, M.I.; Seoane, L.M.; Murri, M.; Pardo, M.; Gomez-Zumaquero, J.M.; Cardona, F.; Casanueva, F.; Tinahones, F.J. Gut microbiota composition in male rat models under different nutritional status and physical activity and its association with serum leptin and ghrelin levels. PLoS ONE 2013, 8, e65465. [Google Scholar] [CrossRef]
- Di Marzo, V.; Matias, I. Endocannabinoid control of food intake and energy balance. Nat. Neurosci. 2005, 8, 585–589. [Google Scholar] [CrossRef] [PubMed]
- Horvath, T.L. Endocannabinoids and the regulation of body fat: The smoke is clearing. J. Clin. Investig. 2003, 112, 323–326. [Google Scholar] [CrossRef]
- Ohno-Shosaku, T.; Tanimura, A.; Hashimotodani, Y.; Kano, M. Endocannabinoids and Retrograde modulation of synaptic transmission. Neuroscientist 2012, 18, 119–132. [Google Scholar] [CrossRef]
- Kim, J.; Li, Y.; Watkins, B.A. Endocannabinoid signaling and energy metabolism: A target for dietary intervention. Nutrition 2011, 27, 624–632. [Google Scholar] [CrossRef]
- Cardinal, P.; Bellocchio, L.; Clark, S.; Cannich, A.; Klugmann, M.; Lutz, B.; Marsicano, G.; Cota, D. Hypothalamic CB1 Cannabinoid receptors regulate energy balance in mice. Endocrinology 2012, 153, 4136–4143. [Google Scholar] [CrossRef]
- Myers, M.G.; Heymsfield, S.B.; Haft, C.; Kahn, B.B.; Laughlin, M.; Leibel, R.L.; Tschöp, M.H.; Yanovski, J.A. Challenges and opportunities of defining clinical leptin resistance. Cell Metab. 2012, 15, 150–156. [Google Scholar] [CrossRef]
- Tam, J.; Cinar, R.; Liu, J.; Godlewski, G.; Wesley, D.; Jourdan, T.; Szanda, G.; Mukhopadhyay, B.; Chedester, L.; Liow, J.-S.; et al. Peripheral cannabinoid-1 receptor inverse agonism reduces obesity by reversing leptin resistance. Cell Metab. 2012, 16, 167–179. [Google Scholar] [CrossRef]
- Bisogno, T.; Mahadevan, A.; Coccurello, R.; Chang, J.-W.; Allarà, M.; Chen, Y.; Giacovazzo, G.; Lichtman, A.; Cravatt, B.; Moles, A.; et al. A novel fluorophosphonate inhibitor of the biosynthesis of the endocannabinoid 2-arachidonoylglycerol with potential anti-obesity effects. Br. J. Pharm. 2013, 169, 784–793. [Google Scholar] [CrossRef] [PubMed]
- Quarta, C.; Bellocchio, L.; Mancini, G.; Mazza, R.; Cervino, C.; Braulke, L.J.; Fekete, C.; Latorre, R.; Nanni, C.; Bucci, M.; et al. CB(1) Signaling in forebrain and sympathetic neurons is a key determinant of endocannabinoid actions on energy balance. Cell Metab. 2010, 11, 273–285. [Google Scholar] [CrossRef] [PubMed]
- Alén, F.; Ramírez-López, M.T.; Gómez de Heras, R.; Rodríguez de Fonseca, F.; Orio, L. Cannabinoid receptors and cholecystokinin in feeding inhibition. Vitam. Horm. 2013, 92, 165–196. [Google Scholar] [CrossRef] [PubMed]
- Bermudez-Silva, F.J.; Cardinal, P.; Cota, D. The role of the endocannabinoid system in the neuroendocrine regulation of energy balance. J. Psychopharmacol. 2012, 26, 114–124. [Google Scholar] [CrossRef]
- Melis, T.; Succu, S.; Sanna, F.; Boi, A.; Argiolas, A.; Melis, M.R. The cannabinoid antagonist SR 141716A (Rimonabant) reduces the increase of extra-cellular dopamine release in the rat nucleus accumbens induced by a novel high palatable food. Neurosci. Lett. 2007, 419, 231–235. [Google Scholar] [CrossRef]
- Janero, D.R. Cannabinoid-1 receptor (CB1R) blockers as medicines: Beyond obesity and cardiometabolic disorders to substance abuse/drug addiction with CB1R neutral antagonists. Expert Opin. Emerg. Drugs 2012, 17, 17–29. [Google Scholar] [CrossRef]
- DiPatrizio, N.V.; Piomelli, D. The thrifty lipids: Endocannabinoids and the neural control of energy conservation. Trends Neurosci. 2012, 35, 403–411. [Google Scholar] [CrossRef]
- Naughton, S.S.; Mathai, M.L.; Hryciw, D.H.; McAinch, A.J. Fatty acid modulation of the endocannabinoid system and the effect on food intake and metabolism. Int. J. Endocrinol. 2013, 2013, 361895. [Google Scholar] [CrossRef]
- Jager, G.; Witkamp, R.F. The endocannabinoid system and appetite: Relevance for food reward. Nutr. Res. Rev. 2014, 27, 172–185. [Google Scholar] [CrossRef]
- Carta, G.; Melis, M.; Pintus, S.; Pintus, P.; Piras, C.A.; Muredda, L.; Demurtas, D.; Di Marzo, V.; Banni, S.; Barbarossa, I.T. Participants with normal weight or with obesity show different relationships of 6-n-propylthiouracil (PROP) taster status with BMI and plasma endocannabinoids. Sci. Rep. 2017, 7, 1361. [Google Scholar] [CrossRef]
- Marco, E.M.; Romero-Zerbo, S.Y.; Viveros, M.-P.; Bermudez-Silva, F.J. The role of the endocannabinoid system in eating disorders: Pharmacological implications. Behav. Pharm. 2012, 23, 526–536. [Google Scholar] [CrossRef] [PubMed]
- De Miguel-Yanes, J.M.; Manning, A.K.; Shrader, P.; McAteer, J.B.; Goel, A.; Hamsten, A.; Fox, C.S.; Florez, J.C.; Dupuis, J.; Meigs, J.B. Variants at the endocannabinoid receptor CB1 gene (CNR1) and insulin sensitivity, type 2 diabetes and coronary heart disease. Obesity (Silver Spring) 2011, 19, 2031–2037. [Google Scholar] [CrossRef] [PubMed]
- Engeli, S. Peripheral metabolic effects of endocannabinoids and cannabinoid receptor blockade. Obes. Facts 2008, 1, 8–15. [Google Scholar] [CrossRef]
- Pagotto, U.; Marsicano, G.; Cota, D.; Lutz, B.; Pasquali, R. The emerging role of the endocannabinoid system in endocrine regulation and energy balance. Endocr. Rev. 2006, 27, 73–100. [Google Scholar] [CrossRef]
- Russo, P.; Strazzullo, P.; Cappuccio, F.; Trégouët, D.-A.; Lauria, F.; Loguercio, M.; Barba, G.; Versiero, M.; Siani, A. Genetic variations at the endocannabinoid type 1 receptor gene (CNR1) are associated with obesity phenotypes in men. J. Clin. Endocrinol. Metab. 2007, 92, 2382–2386. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gallardo-Escribano, C.; Buonaiuto, V.; Ruiz-Moreno, M.I.; Vargas-Candela, A.; Vilches-Perez, A.; Benitez-Porres, J.; Romance-Garcia, A.R.; Ruiz-Moreno, A.; Gomez-Huelgas, R.; Bernal-Lopez, M.R. Epigenetic approach in obesity: DNA methylation in a prepubertal population which underwent a lifestyle modification. Clin. Epigenet. 2020, 12, 144. [Google Scholar] [CrossRef] [PubMed]
- Ouni, M.; Schürmann, A. Epigenetic contribution to obesity. Mamm. Genome 2020, 31, 134–145. [Google Scholar] [CrossRef] [PubMed]
- Koh, I.-U.; Choi, N.-H.; Lee, K.; Yu, H.-Y.; Yun, J.H.; Kong, J.-H.; Kim, H.J.; Lee, S.; Kim, S.C.; Kim, B.-J.; et al. Obesity susceptible novel DNA methylation marker on regulatory region of inflammation gene: Results from the Korea Epigenome Study (KES). BMJ Open Diabetes Res. Care 2020, 8, e001338. [Google Scholar] [CrossRef]
- Xu, X.; Su, S.; Barnes, V.A.; De Miguel, C.; Pollock, J.; Ownby, D.; Shi, H.; Zhu, H.; Snieder, H.; Wang, X. A genome-wide methylation study on obesity: Differential variability and differential methylation. Epigenetics 2013, 8, 522–533. [Google Scholar] [CrossRef]
- Dick, K.J.; Nelson, C.P.; Tsaprouni, L.; Sandling, J.K.; Aïssi, D.; Wahl, S.; Meduri, E.; Morange, P.-E.; Gagnon, F.; Grallert, H.; et al. DNA methylation and body-mass index: A genome-wide analysis. Lancet 2014, 383, 1990–1998. [Google Scholar] [CrossRef]
- Aslibekyan, S.; Demerath, E.W.; Mendelson, M.; Zhi, D.; Guan, W.; Liang, L.; Sha, J.; Pankow, J.S.; Liu, C.; Irvin, M.R.; et al. Epigenome-Wide Study identifies novel methylation loci associated with body mass index and waist circumference. Obesity (Silver Spring) 2015, 23, 1493–1501. [Google Scholar] [CrossRef]
- Demerath, E.W.; Guan, W.; Grove, M.L.; Aslibekyan, S.; Mendelson, M.; Zhou, Y.-H.; Hedman, Å.K.; Sandling, J.K.; Li, L.-A.; Irvin, M.R.; et al. Epigenome-Wide Association Study (EWAS) of BMI, BMI change and waist circumference in African American adults identifies multiple replicated loci. Hum. Mol. Genet. 2015, 24, 4464–4479. [Google Scholar] [CrossRef]
- Mendelson, M.M.; Marioni, R.E.; Joehanes, R.; Liu, C.; Hedman, Å.K.; Aslibekyan, S.; Demerath, E.W.; Guan, W.; Zhi, D.; Yao, C.; et al. Association of body mass index with DNA methylation and gene expression in blood cells and relations to cardiometabolic disease: A Mendelian Randomization approach. PLoS Med. 2017, 14, e1002215. [Google Scholar] [CrossRef]
- Wang, X.; Pan, Y.; Zhu, H.; Hao, G.; Huang, Y.; Barnes, V.; Shi, H.; Snieder, H.; Pankow, J.; North, K.; et al. An Epigenome-Wide Study of obesity in African American youth and young adults: Novel findings, replication in neutrophils, and relationship with gene expression. Clin. Epigenetics 2018, 10, 3. [Google Scholar] [CrossRef]
- Dhana, K.; Braun, K.V.E.; Nano, J.; Voortman, T.; Demerath, E.W.; Guan, W.; Fornage, M.; van Meurs, J.B.J.; Uitterlinden, A.G.; Hofman, A.; et al. An Epigenome-Wide Association Study of obesity-related traits. Am. J. Epidemiol. 2018, 187, 1662–1669. [Google Scholar] [CrossRef] [PubMed]
- González-Muniesa, P.; Mártinez-González, M.-A.; Hu, F.B.; Després, J.-P.; Matsuzawa, Y.; Loos, R.J.F.; Moreno, L.A.; Bray, G.A.; Martinez, J.A. Obesity. Nat. Rev. Dis. Primers 2017, 3, 17034. [Google Scholar] [CrossRef] [PubMed]
- Rotter, A.; Bayerlein, K.; Hansbauer, M.; Weiland, J.; Sperling, W.; Kornhuber, J.; Biermann, T. CB1 and CB2 Receptor expression and promoter methylation in patients with cannabis dependence. Eur. Addict. Res. 2013, 19, 13–20. [Google Scholar] [CrossRef]
- Subbanna, S.; Nagre, N.N.; Umapathy, N.S.; Pace, B.S.; Basavarajappa, B.S. Ethanol exposure induces neonatal neurodegeneration by enhancing CB1R exon1 histone H4K8 acetylation and up-regulating CB1R function causing neurobehavioral abnormalities in adult mice. Int. J. Neuropsychopharmacol. 2014, 18. [Google Scholar] [CrossRef]
- Di Francesco, A.; Falconi, A.; Di Germanio, C.; Micioni Di Bonaventura, M.V.; Costa, A.; Caramuta, S.; Del Carlo, M.; Compagnone, D.; Dainese, E.; Cifani, C.; et al. Extravirgin olive oil up-regulates CB1 tumor suppressor gene in human colon cancer cells and in rat colon via epigenetic mechanisms. J. Nutr. Biochem. 2015, 26, 250–258. [Google Scholar] [CrossRef]
- Chen, J.; Hutchison, K.E.; Bryan, A.D.; Filbey, F.M.; Calhoun, V.D.; Claus, E.D.; Lin, D.; Sui, J.; Du, Y.; Liu, J. Opposite epigenetic associations with alcohol use and exercise intervention. Front. Psychiatry 2018, 9, 594. [Google Scholar] [CrossRef]
- Pucci, M.; Micioni Di Bonaventura, M.V.; Zaplatic, E.; Bellia, F.; Maccarrone, M.; Cifani, C.; D’Addario, C. Transcriptional regulation of the endocannabinoid system in a rat model of binge-eating behavior reveals a selective modulation of the hypothalamic fatty acid amide hydrolase gene. Int. J. Eat. Disord. 2019, 52, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Almeida, M.M.; Dias-Rocha, C.P.; Reis-Gomes, C.F.; Wang, H.; Atella, G.C.; Cordeiro, A.; Pazos-Moura, C.C.; Joss-Moore, L.; Trevenzoli, I.H. Maternal high-fat diet impairs leptin signaling and up-regulates type-1 cannabinoid receptor with sex-specific epigenetic changes in the hypothalamus of newborn rats. Psychoneuroendocrinology 2019, 103, 306–315. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Wang, H.; Ning, W.; Backlund, M.G.; Dey, S.K.; DuBois, R.N. Loss of cannabinoid receptor 1 accelerates intestinal tumor growth. Cancer Res. 2008, 68, 6468–6476. [Google Scholar] [CrossRef] [PubMed]
- Pucci, M.; Micioni Di Bonaventura, M.V.; Vezzoli, V.; Zaplatic, E.; Massimini, M.; Mai, S.; Sartorio, A.; Scacchi, M.; Persani, L.; Maccarrone, M.; et al. Preclinical and clinical evidence for a distinct regulation of Mu opioid and type 1 cannabinoid receptor genes expression in obesity. Front. Genet. 2019, 10, 523. [Google Scholar] [CrossRef] [PubMed]
- Engeli, S.; Böhnke, J.; Feldpausch, M.; Gorzelniak, K.; Janke, J.; Bátkai, S.; Pacher, P.; Harvey-White, J.; Luft, F.C.; Sharma, A.M.; et al. Activation of the peripheral endocannabinoid system in human obesity. Diabetes 2005, 54, 2838–2843. [Google Scholar] [CrossRef]
- Ravinet Trillou, C.; Delgorge, C.; Menet, C.; Arnone, M.; Soubrié, P. CB1 cannabinoid receptor knockout in mice leads to leanness, resistance to diet-induced obesity and enhanced leptin sensitivity. Int. J. Obes. Relat. Metab. Disord. 2004, 28, 640–648. [Google Scholar] [CrossRef]
- Côté, M.; Matias, I.; Lemieux, I.; Petrosino, S.; Alméras, N.; Després, J.-P.; Di Marzo, V. Circulating endocannabinoid levels, abdominal adiposity and related cardiometabolic risk factors in obese men. Int. J. Obes. (London) 2007, 31, 692–699. [Google Scholar] [CrossRef]
- Benzinou, M.; Chèvre, J.-C.; Ward, K.J.; Lecoeur, C.; Dina, C.; Lobbens, S.; Durand, E.; Delplanque, J.; Horber, F.F.; Heude, B.; et al. Endocannabinoid receptor 1 gene variations increase risk for obesity and modulate body mass index in European populations. Hum. Mol. Genet. 2008, 17, 1916–1921. [Google Scholar] [CrossRef]
- Pawlak, M.; Łaczmański, Ł.; Milewicz, A. Rola układu endokannabinoidowego i polimorfizmów genu CNR1 w Powstawaniu otyłości. Endokrynologia Otyłość I Zaburzenia Przemiany Mater. 2011, 7, 192–196. [Google Scholar]
- Schleinitz, D.; Carmienke, S.; Böttcher, Y.; Tönjes, A.; Berndt, J.; Klöting, N.; Enigk, B.; Müller, I.; Dietrich, K.; Breitfeld, J.; et al. Role of genetic variation in the cannabinoid type 1 receptor gene (CNR1) in the pathophysiology of human obesity. Pharmacogenomics 2010, 11, 693–702. [Google Scholar] [CrossRef]
- Van Gaal, L.F.; Rissanen, A.M.; Scheen, A.J.; Ziegler, O.; Rössner, S. RIO-Europe Study Group. Effects of the cannabinoid-1 receptor blocker rimonabant on weight reduction and cardiovascular risk factors in overweight patients: 1-Year experience from the RIO-Europe Study. Lancet 2005, 365, 1389–1397. [Google Scholar] [CrossRef]
- Gazzerro, P.; Caruso, M.G.; Notarnicola, M.; Misciagna, G.; Guerra, V.; Laezza, C.; Bifulco, M. Association between cannabinoid type-1 receptor polymorphism and body mass index in a southern italian population. Int. J. Obes. (London) 2007, 31, 908–912. [Google Scholar] [CrossRef] [PubMed]
- De Luis, D.A.; Ovalle, H.F.; Soto, G.D.; Izaola, O.; de la Fuente, B.; Romero, E. Role of genetic variation in the cannabinoid receptor gene (CNR1) (G1359A Polymorphism) on weight loss and cardiovascular risk factors after liraglutide treatment in obese patients with diabetes mellitus type. J. Investig. Med. 2014, 62, 324–327. [Google Scholar] [CrossRef] [PubMed]
- Frost, M.; Nielsen, T.; Wraae, K.; Hagen, C.; Piters, E.; Beckers, S.; Freitas, F.; Brixen, K.; Van Hul, W.; Andersen, M. Polymorphisms in the endocannabinoid receptor 1 in relation to fat mass distribution. Eur. J. Endocrinol. Eur. Fed. Endocr. Soc. 2010, 163, 407–412. [Google Scholar] [CrossRef]
- Monteleone, P.; Bifulco, M.; Di Filippo, C.; Gazzerro, P.; Canestrelli, B.; Monteleone, F.; Proto, M.C.; Di Genio, M.; Grimaldi, C.; Maj, M. Association of CNR1 and FAAH endocannabinoid gene polymorphisms with anorexia nervosa and bulimia nervosa: Evidence for synergistic effects. Genes Brain Behav. 2009, 8, 728–732. [Google Scholar] [CrossRef]
- Col Araz, N.; Nacak, M.; Oguzkan Balci, S.; Benlier, N.; Araz, M.; Pehlivan, S.; Balat, A.; Aynacioglu, A.S. Childhood obesity and the role of dopamine D2 receptor and cannabinoid receptor-1 gene polymorphisms. Genet. Test. Mol. Biomark. 2012, 16, 1408–1412. [Google Scholar] [CrossRef]
- Müller, T.D.; Reichwald, K.; Wermter, A.K.; Brönner, G.; Nguyen, T.T.; Friedel, S.; Koberwitz, K.; Engeli, S.; Lichter, P.; Meitinger, T.; et al. No Evidence for an involvement of variants in the cannabinoid receptor gene (CNR1) in obesity in German children and adolescents. Mol. Genet. Metab. 2007, 90, 429–434. [Google Scholar] [CrossRef]
- De Luis, D.A.; Izaola, O.; Aller, R.; Lopez, J.J.; Torres, B.; Diaz, G.; Gomez, E.; Romero, E. Association of G1359A polymorphism of the cannabinoid receptor gene (CNR1) with macronutrient intakes in obese females. J. Hum. Nutr. Diet. 2016, 29, 118–123. [Google Scholar] [CrossRef]
- Milewicz, A.; Tworowska-Bardzińska, U.; Jędrzejuk, D.; Lwow, F.; Dunajska, K.; Łaczmański, Ł.; Pawlak, M. Are endocannabinoid type 1 receptor gene (CNR1) polymorphisms associated with obesity and metabolic syndrome in postmenopausal polish women? Int. J. Obes. (London) 2011, 35, 373–377. [Google Scholar] [CrossRef][Green Version]
- Peeters, A.; Beckers, S.; Mertens, I.; Van Hul, W.; Van Gaal, L. The G1422A Variant of the cannabinoid receptor gene (CNR1) is associated with abdominal adiposity in obese men. Endocrine 2007, 31, 138–141. [Google Scholar] [CrossRef]
- De Luis, D.A.; González Sagrado, M.; Aller, R.; Izaola, O.; Conde, R. Relation of C358A Polymorphism of the endocannabinoid degrading enzyme fatty acid amide hydrolase (FAAH) with obesity and insulin resistance. Nutr. Hosp. 2010, 25, 993–998. [Google Scholar] [PubMed]
- Jaeger, J.P.; Mattevi, V.S.; Callegari-Jacques, S.M.; Hutz, M.H. Cannabinoid type-1 receptor gene polymorphisms are associated with central obesity in a Southern Brazilian population. Dis. Markers 2008, 25, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Ceccarini, J.; Weltens, N.; Ly, H.G.; Tack, J.; Van Oudenhove, L.; Van Laere, K. Association between cerebral cannabinoid 1 receptor availability and body mass index in patients with food intake disorders and healthy subjects: A [(18)F]MK-9470 PET study. Transl. Psychiatry 2016, 6, e853. [Google Scholar] [CrossRef] [PubMed]
- Doris, J.M.; Millar, S.A.; Idris, I.; O’Sullivan, S.E. Genetic polymorphisms of the endocannabinoid system in obesity and diabetes. Diabetes Obes. Metab. 2019, 21, 382–387. [Google Scholar] [CrossRef]
- Tiwari, A.K.; Zai, C.C.; Likhodi, O.; Lisker, A.; Singh, D.; Souza, R.P.; Batra, P.; Zaidi, S.H.E.; Chen, S.; Liu, F.; et al. A common polymorphism in the cannabinoid receptor 1 (CNR1) gene is associated with antipsychotic-induced weight gain in schizophrenia. Neuropsychopharmacology 2010, 35, 1315–1324. [Google Scholar] [CrossRef]
- Vazquez-Roque, M.I.; Camilleri, M.; Vella, A.; Carlson, P.; Laugen, J.; Zinsmeister, A.R. Association of genetic variation in cannabinoid mechanisms and gastric motor functions and satiation in overweight and obesity. Neurogastroenterol. Motil. 2011, 23, 637-e257. [Google Scholar] [CrossRef]
- Dinu, I.R.; Popa, S.; Bîcu, M.; Moţa, E.; Moţa, M. The implication of CNR1 gene’s polymorphisms in the modulation of endocannabinoid system effects. Rom. J. Intern. Med. 2009, 47, 9–18. [Google Scholar]
- Mutombo, P.B.W.B.; Yamasaki, M.; Nabika, T.; Shiwaku, K. Cannabinoid receptor 1 (CNR1) 4895 C/T genetic polymorphism was associated with obesity in Japanese men. J. Atheroscler. Thromb. 2012, 19, 779–785. [Google Scholar] [CrossRef][Green Version]
- Baye, T.M.; Zhang, Y.; Smith, E.; Hillard, C.J.; Gunnell, J.; Myklebust, J.; James, R.; Kissebah, A.H.; Olivier, M.; Wilke, R.A. Genetic variation in cannabinoid receptor 1 (CNR1) is associated with derangements in lipid homeostasis, independent of body mass index. Pharmacogenomics 2008, 9, 1647–1656. [Google Scholar] [CrossRef]
- Sipe, J.C.; Waalen, J.; Gerber, A.; Beutler, E. Overweight and obesity associated with a missense polymorphism in fatty acid amide hydrolase (FAAH). Int. J. Obes. (London) 2005, 29, 755–759. [Google Scholar] [CrossRef]
- Monteleone, P.; Tortorella, A.; Martiadis, V.; Di Filippo, C.; Canestrelli, B.; Maj, M. The CDNA 385C to a missense polymorphism of the endocannabinoid degrading enzyme fatty acid amide hydrolase (FAAH) is associated with overweight/obesity but not with binge eating disorder in overweight/obese women. Psychoneuroendocrinology 2008, 33, 546–550. [Google Scholar] [CrossRef] [PubMed]
- Yagin, N.L.; Aliasgari, F.; Aliasgharzadeh, S.; Mahdavi, R.; Akbarzadeh, M. The Influence of the fatty acid amide hydrolase 385C>A single nucleotide polymorphisms on obesity susceptibility. Mol. Biol. Rep. 2019, 46, 5049–5055. [Google Scholar] [CrossRef] [PubMed]
- De Luis, D.A.; Gonzalez Sagrado, M.; Aller, R.; Izaola, O.; Conde, R. Effects of C358A missense polymorphism of the endocannabinoid degrading enzyme fatty acid amide hydrolase on weight loss after a hypocaloric diet. Metabolism 2011, 60, 730–734. [Google Scholar] [CrossRef] [PubMed]
- De Luis, D.A.; Izaola, O.; Aller, R.; de La Fuente, B.; Pacheco, D. Effects of C358A polymorphism of the endocannabinoid degrading enzyme fatty acid amide hydrolase (FAAH) on weight loss, adipocytokines levels, and insulin resistance after a high polyunsaturated fat diet in obese patients. J. Endocrinol. Investig. 2013, 36, 965–969. [Google Scholar] [CrossRef]
- Bellini, G.; Grandone, A.; Torella, M.; Miraglia del Giudice, E.; Nobili, B.; Perrone, L.; Maione, S.; Rossi, F. The Cannabinoid receptor 2 Q63R variant modulates the relationship between childhood obesity and age at menarche. PLoS ONE 2015, 10, e0140142. [Google Scholar] [CrossRef]
- Brusco, A.; Tagliaferro, P.; Saez, T.; Onaivi, E.; Brusco, A.; Tagliaferro, P. Postsynaptic localization of CB2 cannabinoid receptors in the rat hippocampus. Synapse (New York) 2008, 62, 944–949. [Google Scholar] [CrossRef]
- Van Sickle, M.D.; Duncan, M.; Kingsley, P.J.; Mouihate, A.; Urbani, P.; Mackie, K.; Stella, N.; Makriyannis, A.; Piomelli, D.; Davison, J.S.; et al. Identification and functional characterization of brainstem cannabinoid CB2 receptors. Science 2005, 310, 329–332. [Google Scholar] [CrossRef]
- Romero-Zerbo, S.Y.; Garcia-Gutierrez, M.S.; Suárez, J.; Rivera, P.; Ruz-Maldonado, I.; Vida, M.; Rodriguez de Fonseca, F.; Manzanares, J.; Bermúdez-Silva, F.J. Overexpression of cannabinoid CB2 receptor in the brain induces hyperglycaemia and a lean phenotype in adult mice. J. Neuroendocr. 2012, 24, 1106–1119. [Google Scholar] [CrossRef]
- Verty, A.N.A.; Stefanidis, A.; McAinch, A.J.; Hryciw, D.H.; Oldfield, B. Anti-obesity effect of the CB2 receptor agonist JWH-015 in diet-induced obese mice. PLoS ONE 2015, 10, e0140592. [Google Scholar] [CrossRef]
- Ishiguro, H.; Carpio, O.; Horiuchi, Y.; Shu, A.; Higuchi, S.; Schanz, N.; Benno, R.; Arinami, T.; Onaivi, E.S. A nonsynonymous polymorphism in cannabinoid CB2 receptor gene is associated with eating disorders in humans and food intake is modified in mice by its ligands. Synapse 2010, 64, 92–96. [Google Scholar] [CrossRef]
- Rossi, F.; Bellini, G.; Luongo, L.; Manzo, I.; Tolone, S.; Tortora, C.; Bernardo, M.E.; Grandone, A.; Conforti, A.; Docimo, L.; et al. Cannabinoid receptor 2 as antiobesity target: Inflammation, fat storage, and browning modulation. J. Clin. Endocrinol. Metab. 2016, 101, 3469–3478. [Google Scholar] [CrossRef] [PubMed]
- Ketterer, C.; Heni, M.; Stingl, K.; Tschritter, O.; Linder, K.; Wagner, R.; Machicao, F.; Häring, H.-U.; Preissl, H.; Staiger, H.; et al. Polymorphism Rs3123554 in CNR2 reveals gender-specific effects on body weight and affects loss of body weight and cerebral insulin action. Obesity (Silver Spring) 2014, 22, 925–931. [Google Scholar] [CrossRef] [PubMed]
- De Luis, D.A.; Izaola, O.; Primo, D.; de la Fuente, B.; Aller, R. Polymorphism Rs3123554 in the cannabinoid receptor gene type 2 (CNR2) reveals effects on body weight and insulin resistance in obese subjects. Endocrinol. Diabetes Nutr. 2017, 64, 440–445. [Google Scholar] [CrossRef] [PubMed]
- De Luis, D.A.; Ballesteros, M.; Guzman, A.L.; Ruiz, E.; Muñoz, C.; Penacho, M.A.; Iglesias, P.; Maldonado, A.; Martin, L.S.; Izaola, O.; et al. Polymorphism G1359A of the cannabinoid receptor gene (CNR1): Allelic frequencies and influence on cardiovascular risk factors in a Multicentre Study of Castilla-Leon. J. Hum. Nutr. Diet. 2016, 29, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Müller, T.D.; Brönner, G.; Wandolski, M.; Carrie, J.; Nguyen, T.T.; Greene, B.H.; Scherag, A.; Grallert, H.; Vogel, C.I.; Scherag, S.; et al. Mutation screen and association studies for the fatty acid amide hydrolase (FAAH) gene and early onset and adult obesity. BMC Med. Genet. 2010, 11, 2. [Google Scholar] [CrossRef] [PubMed]
- Durand, E.; Lecoeur, C.; Delplanque, J.; Benzinou, M.; Degraeve, F.; Boutin, P.; Marre, M.; Balkau, B.; Charpentier, G.; Froguel, P.; et al. Evaluating the association of FAAH common gene variation with childhood, adult severe obesity and type 2 diabetes in the French population. Obes. Facts 2008, 1, 305–309. [Google Scholar] [CrossRef]
- Balsevich, G.; Sticht, M.; Bowles, N.P.; Singh, A.; Lee, T.T.Y.; Li, Z.; Chelikani, P.K.; Lee, F.S.; Borgland, S.L.; Hillard, C.J.; et al. Role for fatty acid amide hydrolase (FAAH) in the leptin-mediated effects on feeding and energy balance. Proc. Natl. Acad. Sci. USA 2018, 115, 7605–7610. [Google Scholar] [CrossRef]
- Jensen, D.P.; Andreasen, C.H.; Andersen, M.K.; Hansen, L.; Eiberg, H.; Borch-Johnsen, K.; Jørgensen, T.; Hansen, T.; Pedersen, O. The functional Pro129Thr variant of the FAAH gene is not associated with various fat accumulation phenotypes in a population-based cohort of 5,801 whites. J. Mol. Med. 2007, 85, 445–449. [Google Scholar] [CrossRef]
- Papazoglou, D.; Panagopoulos, I.; Papanas, N.; Gioka, T.; Papadopoulos, T.; Papathanasiou, P.; Kaitozis, O.; Papatheodorou, K.; Maltezos, E. The fatty acid amide hydrolase (FAAH) Pro129Thr polymorphism is not associated with severe obesity in greek subjects. Horm. Metab. Res. 2008, 40, 907–910. [Google Scholar] [CrossRef]
- De Martins, C.J.M.; Genelhu, V.; Pimentel, M.M.G.; Celoria, B.M.J.; Mangia, R.F.; Aveta, T.; Silvestri, C.; Marzo, V.D.; Francischetti, E.A. Circulating endocannabinoids and the polymorphism 385C>A in fatty acid amide hydrolase (FAAH) gene may identify the obesity phenotype related to cardiometabolic risk: A study conducted in a Brazilian population of complex interethnic admixture. PLoS ONE 2015, 10, e0142728. [Google Scholar] [CrossRef]
- Wangensteen, T.; Akselsen, H.; Holmen, J.; Undlien, D.; Retterstøl, L. A Common haplotype in NAPEPLD Is associated with severe obesity in a Norwegian population-based cohort (the HUNT Study). Obesity (Silver Spring) 2011, 19, 612–617. [Google Scholar] [CrossRef] [PubMed]
- Pi-Sunyer, F.; Aronne, L.; Heshmati, H.; Devin, J.; Rosenstock, J. Effect of rimonabant, a cannabinoid-1 receptor blocker, on weight and cardiometabolic risk factors in overweight or obese patients: RIO-North America: A Randomized Controlled Trial. JAMA 2006, 295, 761–775. [Google Scholar] [CrossRef]
- Jean-Pierre, D.; Alain, G.; Lars, S. Effects of rimonabant on metabolic risk factors in overweight patients with dyslipidemia. N. Engl. J. Med. 2005, 14. [Google Scholar]
- Scheen, A.J.; Finer, N.; Hollander, P.; Jensen, M.D.; Van Gaal, L.F. RIO Diabetes Study Group: Efficacy and tolerability of rimonabant in overweightor obese patients with type 2 diabetes: A randomised controlled study. Lancet 2006, 368, 1660–1672. [Google Scholar] [CrossRef]
- Wierzbicki, A.S. Rimonabant: Endocannabinoid inhibition for the metabolic syndrome. Int. J. Clin. Pract. 2006, 60, 1697–1706. [Google Scholar] [CrossRef]
- Rychter, A.M.; Zawada, A.; Ratajczak, A.E.; Dobrowolska, A.; Krela-Kaźmierczak, I. Should patients with obesity be more afraid of COVID-19? Obes. Rev. 2020, 21, 13083. [Google Scholar] [CrossRef]
- Popkin, B.M.; Du, S.; Green, W.D.; Beck, M.A.; Algaith, T.; Herbst, C.H.; Alsukait, R.F.; Alluhidan, M.; Alazemi, N.; Shekar, M. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes. Rev. 2020, 21, e13128. [Google Scholar] [CrossRef]
- Briand-Mésange, F.; Trudel, S.; Salles, J.; Ausseil, J.; Salles, J.-P.; Chap, H. Possible role of adipose tissue and the endocannabinoid system in coronavirus disease 2019 pathogenesis: Can rimonabant return? Obesity 2020, 28, 1580–1581. [Google Scholar] [CrossRef]
- Quarta, C.; Cota, D. Anti-obesity therapy with peripheral CB1 Blockers: From promise to safe(?) practice. Int. J. Obes. 2020, 44, 2179–2193. [Google Scholar] [CrossRef]
- LoVerme, J.; Duranti, A.; Tontini, A.; Spadoni, G.; Mor, M.; Stella, N.; Xu, C.; Tarzia, G.; Piomelli, D.; Tarzia, G. Synthesis and characterization of a peripherally restricted CB1 cannabinoid antagonist, URB447, that reduces feeding and body-weight gain in mice. Bioorganic Med. Chem. Lett. 2013, 11, 639–643. [Google Scholar] [CrossRef]
- Cluny, N.; Vemuri, V.; Chambers, A.; Limebeer, C.; Bedard, H.; Wood, J.; Lutz, B.; Zimmer, A.; Parker, L.; Makriyannis, A.; et al. A novel peripherally restricted cannabinoid receptor antagonist, AM6545, reduces food intake and body weight, but does not cause malaise, in rodents: Peripheral CB antagonist reduces food intake. Br. J. Pharmacol. 2010, 161, 629–642. [Google Scholar] [CrossRef] [PubMed]
- Vijayakumar, R.; Lin, Y.; Shia, K.-S.; Yeh, Y.-N.; Hsieh, W.-P.; Hsiao, W.-C.; Chang, C.-P.; Chao, Y.-S.; Hung, M.-S. Induction of fatty acid oxidation resists weight gain, ameliorates hepatic steatosis and reduces cardiometabolic risk factors. Int. J. Obes. 2012, 36, 999–1006. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Li, M.; Meng, T.; Peng, H.; Xie, X.; Zhang, Y.; Jin, Y.; Wang, X.; Zou, L.; Shen, J. Asymmetric synthesis and biological evaluation of N-Cyclohexyl-4-[1-(2,4-Dichlorophenyl)-1-(p-Tolyl)Methyl]Piperazine-1-Carboxamide as HCB1 receptor antagonists. Eur. J. Med. Chem. 2011, 46, 5310–5316. [Google Scholar] [CrossRef] [PubMed]
- Han, J.H.; Shin, H.; Park, J.-Y.; Rho, J.G.; Son, D.H.; Kim, K.W.; Seong, J.K.; Yoon, S.-H.; Kim, W. A novel peripheral cannabinoid 1 receptor antagonist, AJ5012, improves metabolic outcomes and suppresses adipose tissue inflammation in obese mice. FASEB J. 2019, 33, 4314–4326. [Google Scholar] [CrossRef] [PubMed]
- Matthews, J.M.; McNally, J.J.; Connolly, P.J.; Xia, M.; Zhu, B.; Black, S.; Chen, C.; Hou, C.; Liang, Y.; Tang, Y.; et al. Tetrahydroindazole derivatives as potent and peripherally selective Cannabinoid-1 (CB1) receptor inverse agonists. Bioorganic Med. Chem. Lett. 2016, 26, 5346–5349. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.-M.; Greco, M.N.; Macielag, M.J.; Teleha, C.A.; DesJarlais, R.L.; Tang, Y.; Ho, G.; Hou, C.; Chen, C.; Zhao, S.; et al. 6-Benzhydryl-4-Amino-Quinolin-2-Ones as potent cannabinoid type 1 (CB1) receptor inverse agonists and chemical modifications for peripheral selectivity. J. Med. Chem. 2018, 61, 10276–10298. [Google Scholar] [CrossRef]
- Vemuri, V.K.; Janero, D.R.; Makriyannis, A. Pharmacotherapeutic targeting of the endocannabinoid signaling system: Drugs for obesity and the metabolic syndrome. Physiol. Behav. 2008, 93, 671–686. [Google Scholar] [CrossRef]
- Aronne, L.J.; Tonstad, S.; Moreno, M.; Gantz, I.; Erondu, N.; Suryawanshi, S.; Molony, C.; Sieberts, S.; Nayee, J.; Meehan, A.G.; et al. A clinical trial assessing the safety and efficacy of taranabant, a CB1R inverse agonist, in obese and overweight patients: A high-dose study. Int. J. Obes. (London) 2010, 34, 919–935. [Google Scholar] [CrossRef]
- Kipnes, M.S.; Hollander, P.; Fujioka, K.; Gantz, I.; Seck, T.; Erondu, N.; Shentu, Y.; Lu, K.; Suryawanshi, S.; Chou, M.; et al. A one-year study to assess the safety and efficacy of the CB1R inverse agonist taranabant in overweight and obese patients with type 2 diabetes. Diabetes Obes. Metab. 2010, 12, 517–531. [Google Scholar] [CrossRef]
- Reggio, P.H. Toward the design of cannabinoid CB1 receptor inverse agonists and neutral antagonists. Drug Dev. Res. 2009, 70, 585–600. [Google Scholar] [CrossRef]
- Lee, H.-K.; Choi, E.B.; Pak, C.S. The current status and future perspectives of studies of cannabinoid receptor 1 antagonists as anti-obesity agents. Curr. Top. Med. Chem. 2009, 9, 482–503. [Google Scholar] [CrossRef] [PubMed]
- Radziszewska, E.; Bojanowska, E. Effects of glucagon-like Peptide-1 receptor stimulation and blockade on food consumption and body weight in rats treated with a cannabinoid CB1 receptor agonist WIN 55,212-2. Med. Sci. Monit. Basic Res. 2013, 19, 6–11. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Palomba, L.; Silvestri, C.; Imperatore, R.; Morello, G.; Piscitelli, F.; Martella, A.; Cristino, L.; Di Marzo, V. Negative regulation of leptin-induced reactive oxygen species (ROS) formation by cannabinoid CB1 receptor activation in hypothalamic neurons. J. Biol. Chem. 2015, 290, 13669–13677. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
