Association of Household Food Insecurity with Nutritional Status and Mental Health of Pregnant Women in Rural Bangladesh
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting, Population, and Data Source
2.2. Household Food Insecurity
2.3. Mental Health
2.4. Anthropometry
2.5. Outcomes
2.6. Covariates
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Anderson, S.A. (Ed.) Core indicators of nutritional state for difficult-to-sample populations. J. Nutr. 1990, 120 (Suppl. 11), 1559–1600. [Google Scholar] [CrossRef]
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2020. Transforming Food Systems for Affordable Healthy Diets; FAO: Rome, Italy, 2020. [Google Scholar] [CrossRef]
- USAID. Food Assistance Fact Sheet—Bangladesh (12 March 2020). Available online: https://www.usaid.gov/bangladesh/food-assistance (accessed on 8 August 2021).
- Mathur, A. Women and Food Security: A Comparison of South Asia and Southeast Asia. South Asian Surv. 2011, 18, 181–206. [Google Scholar] [CrossRef]
- Picciano, M.F. Pregnancy and lactation: Physiological adjustments, nutritional requirements and the role of dietary supplements. J. Nutr. 2003, 133, 1997s–2002s. [Google Scholar] [CrossRef] [PubMed]
- Cheu, L.A.; Yee, L.M.; Kominiarek, M.A. Food insecurity during pregnancy and gestational weight gain. Am. J. Obstet. Gynecol. MFM 2020, 2, 100068. [Google Scholar] [CrossRef]
- Hadley, C.; Tessema, F.; Muluneh, A.T. Household food insecurity and caregiver distress: Equal threats to child nutritional status? Am. J. Hum. Biol. Off. J. Hum. Biol. Counc. 2012, 24, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Hojaji, E.; Aghajani, M.; Zavoshy, R.; Noroozi, M.; Jahanihashemi, H.; Ezzeddin, N. Household food insecurity associations with pregnancy hypertension, diabetes mellitus and infant birth anthropometric measures: A cross-sectional study of Iranian mothers. Hypertens. Pregnancy 2021, 40, 109–117. [Google Scholar] [CrossRef]
- Richterman, A.; Raymonville, M.; Hossain, A.; Millien, C.; Joseph, J.P.; Jerome, G.; Franke, M.F.; Ivers, L.C. Food insecurity as a risk factor for preterm birth: A prospective facility-based cohort study in rural Haiti. BMJ Glob. Health 2020, 5, e002341. [Google Scholar] [CrossRef]
- Victora, C.G.; Christian, P.; Vidaletti, L.P.; Gatica-Domínguez, G.; Menon, P.; Black, R.E. Revisiting maternal and child undernutrition in low-income and middle-income countries: Variable progress towards an unfinished agenda. Lancet 2021, 397, 1388–1399. [Google Scholar] [CrossRef]
- Hamadani, J.D.; Hasan, M.I.; Baldi, A.J.; Hossain, S.J.; Shiraji, S.; Bhuiyan, M.S.A.; Mehrin, S.F.; Fisher, J.; Tofail, F.; Tipu, S.; et al. Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: An interrupted time series. Lancet. Glob. Health 2020, 8, e1380–e1389. [Google Scholar] [CrossRef]
- Townsend, R.; Chmielewska, B.; Barratt, I.; Kalafat, E.; van der Meulen, J.; Gurol-Urganci, I.; O’Brien, P.; Morris, E.; Draycott, T.; Thangaratinam, S.; et al. Global changes in maternity care provision during the COVID-19 pandemic: A systematic review and meta-analysis. EClinicalMedicine 2021, 37, 100947. [Google Scholar] [CrossRef]
- Picchioni, F.; Goulao, L.F.; Roberfroid, D. The impact of COVID-19 on diet quality, food security and nutrition in low and middle income countries: A systematic review of the evidence. Clin. Nutr. 2021, 43, 1–40. [Google Scholar] [CrossRef] [PubMed]
- Wolfson, J.A.; Garcia, T.; Leung, C.W. Food Insecurity Is Associated with Depression, Anxiety, and Stress: Evidence from the Early Days of the COVID-19 Pandemic in the United States. Health Equity 2021, 5, 64–71. [Google Scholar] [CrossRef]
- Abdu, J.; Kahssay, M.; Gebremedhin, M. Household Food Insecurity, Underweight Status, and Associated Characteristics among Women of Reproductive Age Group in Assayita District, Afar Regional State, Ethiopia. J. Environ. Public Health 2018, 2018, 7659204. [Google Scholar] [CrossRef]
- Castañeda, J.; Caire-Juvera, G.; Sandoval, S.; Castañeda, P.A.; Contreras, A.D.; Portillo, G.E.; Ortega-Vélez, M.I. Food Security and Obesity among Mexican Agricultural Migrant Workers. Int. J. Environ. Res. Public Health 2019, 16, 4171. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, D.C.; Reesor, L.M.; Murillo, R. Food insecurity and adult overweight/obesity: Gender and race/ethnic disparities. Appetite 2017, 117, 373–378. [Google Scholar] [CrossRef]
- Jones, A.D.; Mundo-Rosas, V.; Cantoral, A.; Levy, T.S. Household food insecurity in Mexico is associated with the co-occurrence of overweight and anemia among women of reproductive age, but not female adolescents. Matern. Child Nutr. 2017, 13, e12396. [Google Scholar] [CrossRef]
- Smith, T.M.; Colón-Ramos, U.; Pinard, C.A.; Yaroch, A.L. Household food insecurity as a determinant of overweight and obesity among low-income Hispanic subgroups: Data from the 2011–2012 California Health Interview Survey. Appetite 2016, 97, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Weigel, M.M.; Armijos, R.X.; Racines, M.; Cevallos, W. Food Insecurity Is Associated with Undernutrition but Not Overnutrition in Ecuadorian Women from Low-Income Urban Neighborhoods. J. Environ. Public Health 2016, 2016, 8149459. [Google Scholar] [CrossRef] [PubMed]
- Motbainor, A.; Worku, A.; Kumie, A. Household food insecurity is associated with both body mass index and middle upper-arm circumference of mothers in northwest Ethiopia: A comparative study. Int. J. Women’s Health 2017, 9, 379–389. [Google Scholar] [CrossRef]
- Tikuye, H.H.; Gebremedhin, S.; Mesfin, A.; Whiting, S. Prevalence and Factors Associated with Undernutrition among Exclusively Breastfeeding Women in Arba Minch Zuria District, Southern Ethiopia: A Cross-sectional Community-Based Study. Ethiop. J. Health Sci. 2019, 29, 913–922. [Google Scholar] [CrossRef]
- Young, S.L.; Plenty, A.H.; Luwedde, F.A.; Natamba, B.K.; Natureeba, P.; Achan, J.; Mwesigwa, J.; Ruel, T.D.; Ades, V.; Osterbauer, B.; et al. Household food insecurity, maternal nutritional status, and infant feeding practices among HIV-infected Ugandan women receiving combination antiretroviral therapy. Matern. Child Health J. 2014, 18, 2044–2053. [Google Scholar] [CrossRef]
- Jomaa, L.; Naja, F.; Cheaib, R.; Hwalla, N. Household food insecurity is associated with a higher burden of obesity and risk of dietary inadequacies among mothers in Beirut, Lebanon. BMC Public Health 2017, 17, 567. [Google Scholar] [CrossRef] [PubMed]
- Chaparro, C.; Oot, L.; Sethuraman, K. Overview of the Nutrition Situation in Four Countries in South and Central Asia; Food and Nutrition Technical Assistance III Project (FANTA): Washington, DC, USA, 2014. [Google Scholar]
- Tayie, F.A.; Zizza, C.A. Height differences and the associations between food insecurity, percentage body fat and BMI among men and women. Public Health Nutr. 2009, 12, 1855–1861. [Google Scholar] [CrossRef][Green Version]
- Weigel, M.M.; Armijos, M.M. Food insufficiency in the households of reproductive-age Ecuadorian women: Association with food and nutritional status indicators. Ecol. Food Nutr. 2015, 54, 20–42. [Google Scholar] [CrossRef] [PubMed]
- Laraia, B.; Vinikoor-Imler, L.C.; Siega-Riz, A.M. Food insecurity during pregnancy leads to stress, disordered eating, and greater postpartum weight among overweight women. Obesity 2015, 23, 1303–1311. [Google Scholar] [CrossRef] [PubMed]
- Jebena, M.G.; Taha, M.; Nakajima, M.; Lemieux, A.; Lemessa, F.; Hoffman, R.; Tesfaye, M.; Belachew, T.; Workineh, N.; Kebede, E.; et al. Household food insecurity and mental distress among pregnant women in Southwestern Ethiopia: A cross sectional study design. BMC Pregnancy Childbirth 2015, 15, 250. [Google Scholar] [CrossRef]
- Abrahams, Z.; Lund, C.; Field, S.; Honikman, S. Factors associated with household food insecurity and depression in pregnant South African women from a low socio-economic setting: A cross-sectional study. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 363–372. [Google Scholar] [CrossRef]
- Richards, M.; Weigel, M.; Li, M.; Rosenberg, M.; Ludema, C. Household food insecurity and antepartum depression in the National Children’s Study. Ann. Epidemiol. 2020, 44, 38–44.e31. [Google Scholar] [CrossRef]
- Sparling, T.M.; Waid, J.L.; Wendt, A.S.; Gabrysch, S. Depression among women of reproductive age in rural Bangladesh is linked to food security, diets and nutrition. Public Health Nutr. 2020, 23, 660–673. [Google Scholar] [CrossRef]
- Woldetensay, Y.K.; Belachew, T.; Biesalski, H.K.; Ghosh, S.; Lacruz, M.E.; Scherbaum, V.; Kantelhardt, E.J. The role of nutrition, intimate partner violence and social support in prenatal depressive symptoms in rural Ethiopia: Community based birth cohort study. BMC Pregnancy Childbirth 2018, 18, 374. [Google Scholar] [CrossRef]
- Moafi, F.; Kazemi, F.; Samiei Siboni, F.; Alimoradi, Z. The relationship between food security and quality of life among pregnant women. BMC Pregnancy Childbirth 2018, 18, 319. [Google Scholar] [CrossRef] [PubMed]
- Weigel, M.M.; Armijos, R.X.; Racines, M.; Cevallos, W.; Castro, N.P. Association of Household Food Insecurity with the Mental and Physical Health of Low-Income Urban Ecuadorian Women with Children. J. Environ. Public Health 2016, 2016, 5256084. [Google Scholar] [CrossRef]
- Whittle, H.J.; Sheira, L.A.; Wolfe, W.R.; Frongillo, E.A.; Palar, K.; Merenstein, D.; Wilson, T.E.; Adedimeji, A.; Weber, K.M.; Adimora, A.A.; et al. Food insecurity is associated with anxiety, stress, and symptoms of posttraumatic stress disorder in a cohort of women with or at risk of HIV in the United States. J. Nutr. 2019, 149, 1393–1403. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, S.; Ali, I. Maternal food insecurity in low-income countries: Revisiting its causes and consequences for maternal and neonatal health. J. Agric. Food Res. 2021, 3, 100091. [Google Scholar] [CrossRef]
- Institute of Medicine. Weight Gain during Pregnancy: Reexamining the Guidelines; National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Hasan, S.M.T.; Khan, M.A.; Ahmed, T. Inadequate maternal weight gain in the third trimester increases the risk of intrauterine growth restriction in rural Bangladesh. PLoS ONE 2019, 14, e0212116. [Google Scholar] [CrossRef] [PubMed]
- Hasan, S.M.T.; Khan, M.A.; Ahmed, T. Institute of Medicine Recommendations on the Rate of Gestational Weight Gain and Perinatal Outcomes in Rural Bangladesh. Int. J. Environ. Res. Public Health 2021, 18, 6519. [Google Scholar] [CrossRef]
- Hasan, S.M.T.; Rahman, S.; Locks, L.M.; Rahman, M.; Hore, S.K.; Saqeeb, K.N.; Khan, M.A.; Ahmed, T. Magnitude and determinants of inadequate third-trimester weight gain in rural Bangladesh. PLoS ONE 2018, 13, e0196190. [Google Scholar] [CrossRef]
- International Centre for Diarrhoeal Disease Research. Health and Demographic Surveillance System–Matlab, v. 53. Registration of Health and Demographic Events 2018; Scientific Report No. 141; International Centre for Diarrhoeal Disease Research: Dhaka, Bangladesh, 2020. [Google Scholar]
- Hasan, S.M.T.; Ahmed, S.I.; Khan, M.A.; Sarker, S.A.; Ahmed, T. Achieving Optimal Gestational Weight Gain, Birth Weight, and Perinatal Outcomes Among Pregnant Women at Risk of Hypertension: Protocol for a Pilot Randomized Controlled Trial. JMIR Res. Protoc. 2020, 9, e16676. [Google Scholar] [CrossRef]
- Jennifer, C.; Swindale, A.; Bilinsky, P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Household Food Access: Indicator Guide (v. 3); FHI 360/FANTA: Washington, DC, USA, 2007. [Google Scholar]
- Das, S.; Rasul, M.G.; Hossain, M.S.; Khan, A.R.; Alam, M.A.; Ahmed, T.; Clemens, J.D. Acute food insecurity and short-term coping strategies of urban and rural households of Bangladesh during the lockdown period of COVID-19 pandemic of 2020: Report of a cross-sectional survey. BMJ Open 2020, 10, e043365. [Google Scholar] [CrossRef]
- Lovibond, S.H.; Lovibond, P.F. Manual for the Depression Anxiety Stress Scales, 2nd ed.; Psychology Foundation: Sydney, Australia, 1995; ISBN 7334-1423-0. [Google Scholar]
- Clout, D.; Brown, R. Sociodemographic, pregnancy, obstetric, and postnatal predictors of postpartum stress, anxiety and depression in new mothers. J. Affect. Disord. 2015, 188, 60–67. [Google Scholar] [CrossRef]
- Rallis, S.; Skouteris, H.; McCabe, M.; Milgrom, J. A prospective examination of depression, anxiety and stress throughout pregnancy. Women Birth J. Aust. Coll. Midwives 2014, 27, e36–e42. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Alim, S.M.A.H.M.; Kibria, S.M.E.; Lslam, J.; Uddin, Z.; Nessa, M.; Wahab, A.; Lslam, M. Translation of DASS 21 into Bangla and validation among medical students. Bangladesh J. Psychiatry 2017, 28, 67–70. [Google Scholar] [CrossRef]
- Bailey, K.V.; Ferro-Luzzi, A. Use of body mass index of adults in assessing individual and community nutritional status. Bull. World Health Organ. 1995, 73, 673–680. [Google Scholar] [PubMed]
- Ververs, M.T.; Antierens, A.; Sackl, A.; Staderini, N.; Captier, V. Which anthropometric indicators identify a pregnant woman as acutely malnourished and predict adverse birth outcomes in the humanitarian context? PLoS Curr. 2013, 5. [Google Scholar] [CrossRef]
- Kolovos, S.; Zavala, G.A.; Leijen, A.S.; Melgar-Quiñonez, H.; van Tulder, M. Household food insecurity is associated with depressive symptoms: Results from a Mexican population-based survey. Food Secur. 2020, 12, 407–416. [Google Scholar] [CrossRef]
- D’Agostino, R.B.; Chase, W.; Belanger, A. The Appropriateness of Some Common Procedures for Testing the Equality of Two Independent Binomial Populations. Am. Stat. 1988, 42, 198–202. [Google Scholar] [CrossRef]
- Upton, G.J.G. A Comparison of Alternative Tests for the 2 × 2 Comparative Trial. J. R. Stat. Soc. Ser. A Gen. 1982, 145, 86–105. [Google Scholar] [CrossRef]
- Schafer, J.L.; Kang, J. Average causal effects from nonrandomized studies: A practical guide and simulated example. Psychol. Methods 2008, 13, 279–313. [Google Scholar] [CrossRef]
- Austin, P.C. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef]
- Caliendo, M.; Kopeinig, S. Some Practical Guidance for the Implementation of Propensity Score Matching. J. Econ. Surv. 2008, 22, 31–72. [Google Scholar] [CrossRef]
- Ho, D.E.; Imai, K.; King, G.; Stuart, E.A. Matching as Nonparametric Preprocessing for Reducing Model Dependence in Parametric Causal Inference. Political Anal. 2007, 15, 199–236. [Google Scholar] [CrossRef]
- Pooler, J.A.; Srinivasan, M. Association Between Supplemental Nutrition Assistance Program Participation and Cost-Related Medication Nonadherence Among Older Adults with Diabetes. JAMA Intern. Med. 2019, 179, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Stuart, E.A. Matching methods for causal inference: A review and a look forward. Stat. Sci. 2010, 25, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.R.; Rubin, D.B. Constructing a Control Group Using Multivariate Matched Sampling Methods That Incorporate the Propensity Score. Am. Stat. 1985, 39, 33–38. [Google Scholar] [CrossRef]
- Leuven, E.; Sianesi, B. “PSMATCH2: Stata Module to Perform Full Mahalanobis and Propensity Score Matching, Common Support Graphing, and Covariate Imbalance Testing” Version 4.0.12 30 January 2016. 2003. Available online: http://ideas.repec.org/c/boc/bocode/s432001.html (accessed on 14 July 2021).
- Commission on the Nutrition Challenges of the 21st Century. Ending Malnutrition by 2020: An Agenda for Change in the Millennium. ACC/SCN, 2000. Available online: https://www.unscn.org/uploads/web/news/2000-FEB-Ending-Malnutrition-by-2020-Agenda-for-Change-in-the-Millennium-Report.pdf (accessed on 19 July 2021).
- Toh-Adam, R.; Srisupundit, K.; Tongsong, T. Short stature as an independent risk factor for cephalopelvic disproportion in a country of relatively small-sized mothers. Arch. Gynecol. Obstet. 2012, 285, 1513–1516. [Google Scholar] [CrossRef] [PubMed]
- Mogren, I.; Lindqvist, M.; Petersson, K.; Nilses, C.; Small, R.; Granåsen, G.; Edvardsson, K. Maternal height and risk of caesarean section in singleton births in Sweden-A population-based study using data from the Swedish Pregnancy Register 2011 to 2016. PLoS ONE 2018, 13, e0198124. [Google Scholar] [CrossRef]
- Khanam, R.; Lee, A.C.; Mitra, D.K.; Ram, M.; Das Gupta, S.; Quaiyum, A.; Choudhury, A.; Christian, P.; Mullany, L.C.; Baqui, A.H. Maternal short stature and under-weight status are independent risk factors for preterm birth and small for gestational age in rural Bangladesh. Eur. J. Clin. Nutr. 2019, 73, 733–742. [Google Scholar] [CrossRef]
- Martorell, R.; Zongrone, A. Intergenerational influences on child growth and undernutrition. Paediatr. Perinat. Epidemiol. 2012, 26 (Suppl. 1), 302–314. [Google Scholar] [CrossRef]
- Black, M.M.; Cutts, D.B.; Frank, D.A.; Geppert, J.; Skalicky, A.; Levenson, S.; Casey, P.H.; Berkowitz, C.; Zaldivar, N.; Cook, J.T.; et al. Special Supplemental Nutrition Program for Women, Infants, and Children participation and infants’ growth and health: A multisite surveillance study. Pediatrics 2004, 114, 169–176. [Google Scholar] [CrossRef]
- El-Bastawissi, A.Y.; Peters, R.; Sasseen, K.; Bell, T.; Manolopoulos, R. Effect of the Washington Special Supplemental Nutrition Program for Women, Infants and Children (WIC) on pregnancy outcomes. Matern. Child Health J. 2007, 11, 611–621. [Google Scholar] [CrossRef]
- Bhattacharya, A.; Pal, B.; Mukherjee, S.; Roy, S.K. Assessment of nutritional status using anthropometric variables by multivariate analysis. BMC Public Health 2019, 19, 1045. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, A.; Butt, A.; Saha, T.K.; Basu, G.; Chattopadhyay, A.; Mukherjee, A. Assessment of Malnutrition Among Adolescents:Can BMI be Replaced by MUAC. Indian J. Community Med. 2010, 35, 276–279. [Google Scholar] [CrossRef] [PubMed]
- Frison, S.; Kerac, M.; Checchi, F.; Prudhon, C. Anthropometric indices and measures to assess change in the nutritional status of a population: A systematic literature review. BMC Nutr. 2016, 2, 76. [Google Scholar] [CrossRef]
- Irena, A.H.; Ross, D.A.; Salama, P.; Collins, S. Anthropometric predictors of mortality in undernourished adults in the Ajiep Feeding Programme in Southern Sudan. Am. J. Clin. Nutr. 2013, 98, 335–339. [Google Scholar] [CrossRef]
- Nowak-Szczepanska, N.; Gomula, A.; Koziel, S. Mid-upper arm circumference and body mass index as different screening tools of nutritional and weight status in Polish schoolchildren across socio-political changes. Sci. Rep. 2019, 9, 12399. [Google Scholar] [CrossRef]
- Powell-Tuck, J.; Hennessy, E.M. A comparison of mid upper arm circumference, body mass index and weight loss as indices of undernutrition in acutely hospitalized patients. Clin. Nutr. 2003, 22, 307–312. [Google Scholar] [CrossRef]
- Weng, C.-H.; Tien, C.-P.; Li, C.-I.; L’Heureux, A.; Liu, C.-S.; Lin, C.-H.; Lin, C.-C.; Lai, S.-W.; Lai, M.-M.; Lin, W.-Y. Mid-upper arm circumference, calf circumference and mortality in Chinese long-term care facility residents: A prospective cohort study. BMJ Open 2018, 8, e020485. [Google Scholar] [CrossRef]
- Hamelin, A.M.; Beaudry, M.; Habicht, J.P. Characterization of household food insecurity in Québec: Food and feelings. Soc. Sci. Med. 2002, 54, 119–132. [Google Scholar] [CrossRef]
- Weaver, L.J.; Hadley, C. Moving beyond hunger and nutrition: A systematic review of the evidence linking food insecurity and mental health in developing countries. Ecol. Food Nutr. 2009, 48, 263–284. [Google Scholar] [CrossRef]
- Hamelin, A.M.; Habicht, J.P.; Beaudry, M. Food insecurity: Consequences for the household and broader social implications. J. Nutr. 1999, 129, 525s–528s. [Google Scholar] [CrossRef] [PubMed]
- Tarasuk, V.S. Household food insecurity with hunger is associated with women’s food intakes, health and household circumstances. J. Nutr. 2001, 131, 2670–2676. [Google Scholar] [CrossRef]
- Nettle, D. Does Hunger Contribute to Socioeconomic Gradients in Behavior? Front. Psychol. 2017, 8, 358. [Google Scholar] [CrossRef] [PubMed]
- Lewis, A.J.; Austin, E.; Galbally, M. Prenatal maternal mental health and fetal growth restriction: A systematic review. J. Dev. Orig. Health Dis. 2016, 7, 416–428. [Google Scholar] [CrossRef]
- Kazemi, F.; Masoumi, S.Z.; Shayan, A.; Shahidi Yasaghi, S.Z. Prevalence of food insecurity in pregnant women and its association with gestational weight gain pattern, neonatal birth weight, and pregnancy complications in Hamadan County, Iran, in 2018. Agric. Food Secur. 2020, 9, 12. [Google Scholar] [CrossRef]
- Senarath, U.; Gunawardena, N.S. Women’s autonomy in decision making for health care in South Asia. Asia-Pac. J. Public Health 2009, 21, 137–143. [Google Scholar] [CrossRef]
- Miller, B.D. Social class, gender and intrahousehold food allocations to children in South Asia. Soc. Sci. Med. 1997, 44, 1685–1695. [Google Scholar] [CrossRef]
- Quisumbing, A.R.; Maluccio, J.A. Resources at Marriage and Intrahousehold Allocation: Evidence from Bangladesh, Ethiopia, Indonesia, and South Africa*. Oxf. Bull. Econ. Stat. 2003, 65, 283–327. [Google Scholar] [CrossRef]
- Patel, V.; Kirkwood, B.R.; Pednekar, S.; Pereira, B.; Barros, P.; Fernandes, J.; Datta, J.; Pai, R.; Weiss, H.; Mabey, D. Gender disadvantage and reproductive health risk factors for common mental disorders in women: A community survey in India. Arch. Gen. Psychiatry 2006, 63, 404–413. [Google Scholar] [CrossRef]
- International Centre for Diarrhoeal Disease Research. Health and Demographic Surveillance System—Matlab, v. 48. Household Socio-Economic Census 2014; International Centre for Diarrhoeal Disease Research: Dhaka, Bangladesh, 2016. [Google Scholar]
- DiClemente, K.; Grace, K.; Kershaw, T.; Bosco, E.; Humphries, D. Investigating the Relationship between Food Insecurity and Fertility Preferences in Tanzania. Matern. Child Health J. 2021, 25, 302–310. [Google Scholar] [CrossRef]
- Arora, A.; Jha, A.K.; Alat, P.; Das, S.S. Understanding coronaphobia. Asian J. Psychiatr. 2020, 54, 102384. [Google Scholar] [CrossRef] [PubMed]
- Tarasuk, V.; Mitchell, A.; McLaren, L.; McIntyre, L. Chronic physical and mental health conditions among adults may increase vulnerability to household food insecurity. J. Nutr. 2013, 143, 1785–1793. [Google Scholar] [CrossRef] [PubMed]
- Bruening, M.; Dinour, L.M.; Chavez, J.B.R. Food insecurity and emotional health in the USA: A systematic narrative review of longitudinal research. Public Health Nutr. 2017, 20, 3200–3208. [Google Scholar] [CrossRef]
- Institute of Medicine. Hunger and Obesity: Understanding a Food Insecurity Paradigm: Workshop Summary; The National Academies Press: Washington, DC, USA, 2011. [Google Scholar] [CrossRef]
- Pérez-Escamilla, R.; Vilar-Compte, M.; Gaitan-Rossi, P. Why identifying households by degree of food insecurity matters for policymaking. Glob. Food Secur. 2020, 26, 100459. [Google Scholar] [CrossRef]
- Stevens, B.; Watt, K.; Brimbecombe, J.; Clough, A.; Judd, J.; Lindsay, D. The role of seasonality on the diet and household food security of pregnant women living in rural Bangladesh: A cross-sectional study. Public Health Nutr. 2017, 20, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Owoo, N.S. Food insecurity and family structure in Nigeria. SSM-Popul. Health 2017, 4, 117–125. [Google Scholar] [CrossRef]
| Characteristic | Food-Insecure | Food-Secure | p |
|---|---|---|---|
| Before matching (n = 672) | |||
| Pregnant women, n | 71 | 601 | - |
| Age (years), mean (SD) | 26.6 (6.4) | 25.2 (5.8) | 0.056 |
| Religion, Muslim | 90.1 | 83.7 | 0.158 |
| Education (years), mean (SD) | 6.6 (3.0) | 8.4 (2.9) | <0.001 |
| Parity | |||
| Nulliparous | 21.1 | 35.8 | 0.014 |
| 1 previous birth | 45.1 | 38.9 | 0.318 |
| ≥2 previous births | 33.8 | 25.3 | 0.123 |
| Gestational age (weeks), mean (SD) | 9.4 (1.6) | 9.9 (1.8) | 0.063 |
| Chronic disease | 5.6 | 4.8 | 0.766 |
| Area | |||
| Block A | 32.4 | 27.6 | 0.398 |
| Block B | 39.4 | 29.8 | 0.096 |
| Block C | 14.1 | 22.6 | 0.099 |
| Block D | 14.1 | 20.0 | 0.236 |
| Period | |||
| Jan–Mar 2020 | 26.8 | 21.6 | 0.326 |
| Apr–Jun 2020 | 19.7 | 16.6 | 0.514 |
| Jul–Sep 2020 | 29.6 | 24.0 | 0.299 |
| Oct 2020–Jan 2021 | 23.9 | 37.8 | 0.022 |
| After matching (n = 665) | |||
| Pregnant women, n | 70 | 595 | - |
| Age (years), mean (SD) | 26.5 (6.5) | 26.2 (5.8) | 0.746 |
| Religion, Muslim | 90.0 | 89.7 | 0.959 |
| Education (years), mean (SD) | 6.7 (3.0) | 6.8 (3.2) | 0.837 |
| Parity | |||
| Nulliparous | 21.4 | 22.6 | 0.874 |
| 1 previous birth | 45.7 | 45.9 | 0.980 |
| ≥2 previous births | 32.9 | 31.5 | 0.867 |
| Gestational age (weeks), mean (SD) | 9.4 (1.6) | 9.5 (1.5) | 0.934 |
| Chronic disease | 5.7 | 5.1 | 0.871 |
| Area | |||
| Block A | 32.9 | 31.9 | 0.906 |
| Block B | 38.6 | 39.7 | 0.889 |
| Block C | 14.3 | 14.4 | 0.982 |
| Block D | 14.3 | 13.9 | 0.953 |
| Period | |||
| Jan–Mar 2020 | 27.1 | 24.3 | 0.707 |
| Apr–Jun 2020 | 20.0 | 21.6 | 0.819 |
| Jul–Sep 2020 | 28.6 | 31.0 | 0.751 |
| Oct 2020–Jan 2021 | 24.3 | 23.0 | 0.863 |
| Outcome | Unadjusted | Adjusted 1 | ||
|---|---|---|---|---|
| β (95% CI) | p | β (95% CI) | p | |
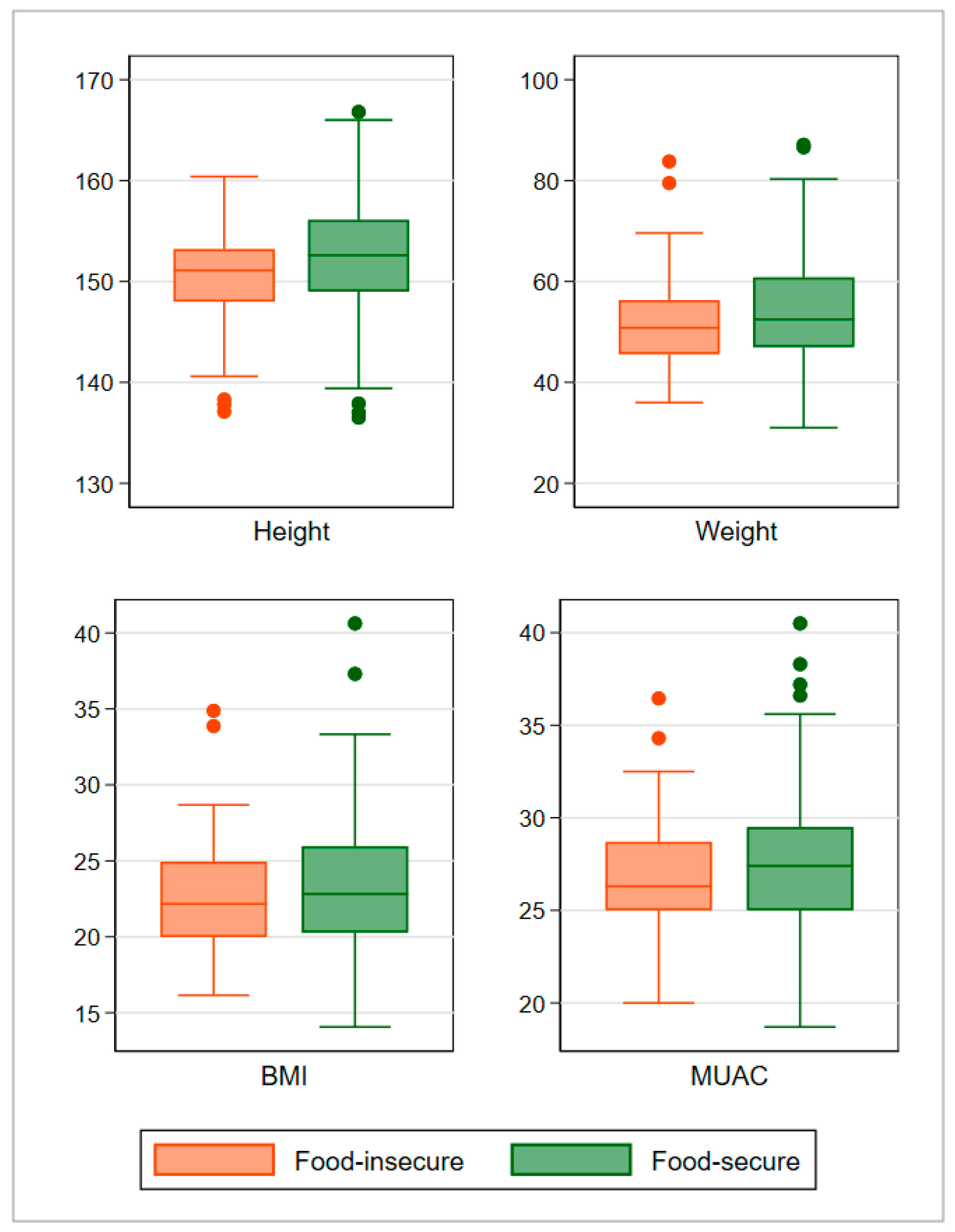
| Height (cm) | −2.0 (−2.8, −1.3) | <0.001 | −2.0 (−2.7, −1.2) | <0.001 |
| Weight (kg) | −2.0 (−3.4, −0.6) | 0.005 | −2.0 (−3.4, −0.7) | 0.003 |
| BMI (kg/m2) | −0.3 (−0.8, 0.3) | 0.365 | −0.3 (−0.8, 0.2) | 0.287 |
| MUAC (cm) | −0.6 (−1.1, −0.1) | 0.027 | −0.6 (−1.1, −0.1) | 0.010 |
| Outcome | Unadjusted | Adjusted 1 | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
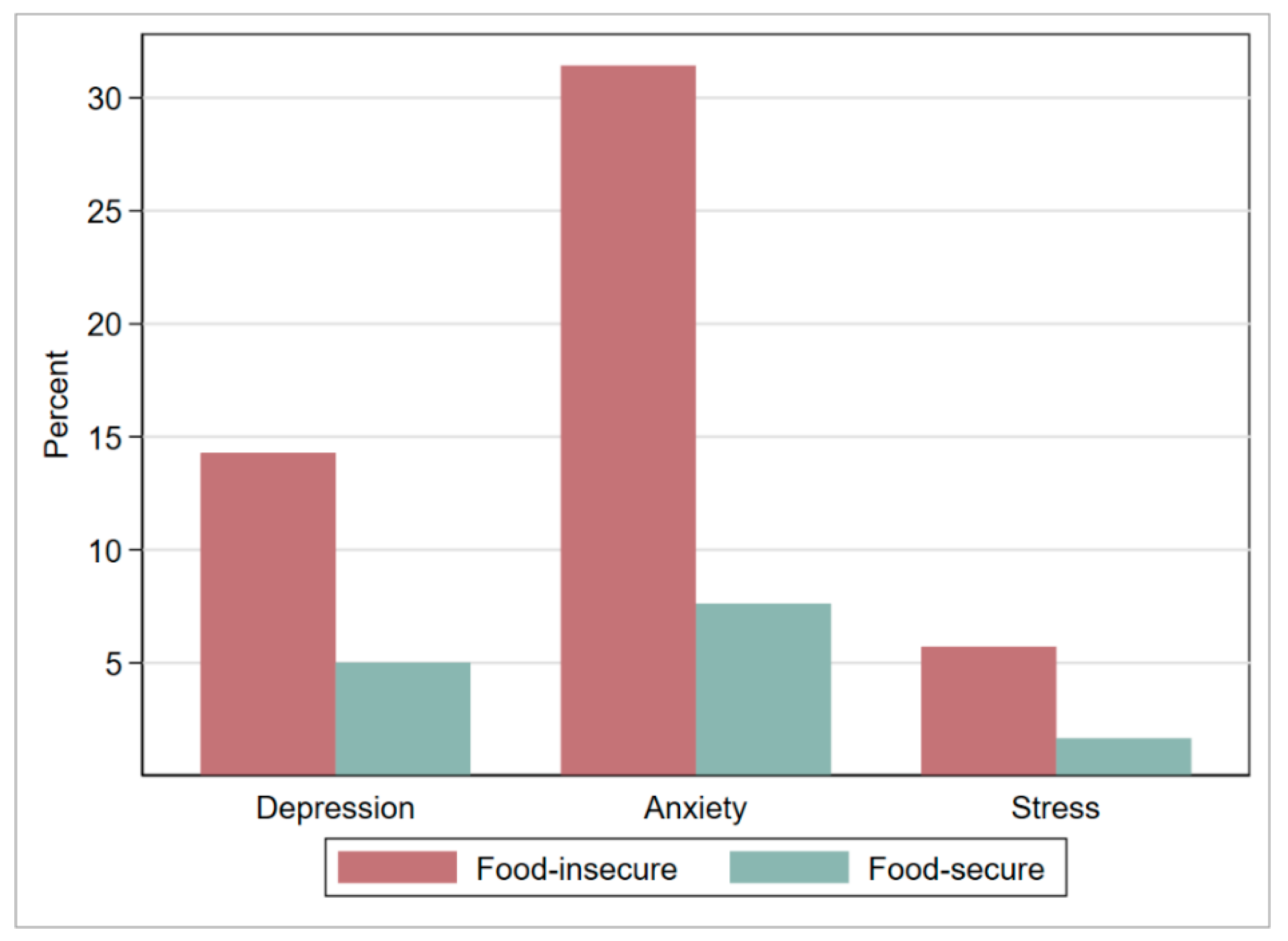
| Depression | 3.2 (1.8, 5.6) | <0.001 | 3.3 (1.8, 5.9) | <0.001 |
| Anxiety | 5.6 (3.5, 8.9) | <0.001 | 6.1 (3.7, 10.0) | <0.001 |
| Stress | 3.6 (1.4, 9.4) | 0.009 | 4.8 (1.6, 14.2) | 0.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hasan, S.M.T.; Hossain, D.; Ahmed, F.; Khan, M.A.; Begum, F.; Ahmed, T. Association of Household Food Insecurity with Nutritional Status and Mental Health of Pregnant Women in Rural Bangladesh. Nutrients 2021, 13, 4303. https://doi.org/10.3390/nu13124303
Hasan SMT, Hossain D, Ahmed F, Khan MA, Begum F, Ahmed T. Association of Household Food Insecurity with Nutritional Status and Mental Health of Pregnant Women in Rural Bangladesh. Nutrients. 2021; 13(12):4303. https://doi.org/10.3390/nu13124303
Chicago/Turabian StyleHasan, S. M. Tafsir, Daluwar Hossain, Faysal Ahmed, Md Alfazal Khan, Ferdousi Begum, and Tahmeed Ahmed. 2021. "Association of Household Food Insecurity with Nutritional Status and Mental Health of Pregnant Women in Rural Bangladesh" Nutrients 13, no. 12: 4303. https://doi.org/10.3390/nu13124303
APA StyleHasan, S. M. T., Hossain, D., Ahmed, F., Khan, M. A., Begum, F., & Ahmed, T. (2021). Association of Household Food Insecurity with Nutritional Status and Mental Health of Pregnant Women in Rural Bangladesh. Nutrients, 13(12), 4303. https://doi.org/10.3390/nu13124303






