Food Insecurity Prevalence, Severity and Determinants in Australian Households during the COVID-19 Pandemic from the Perspective of Women
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
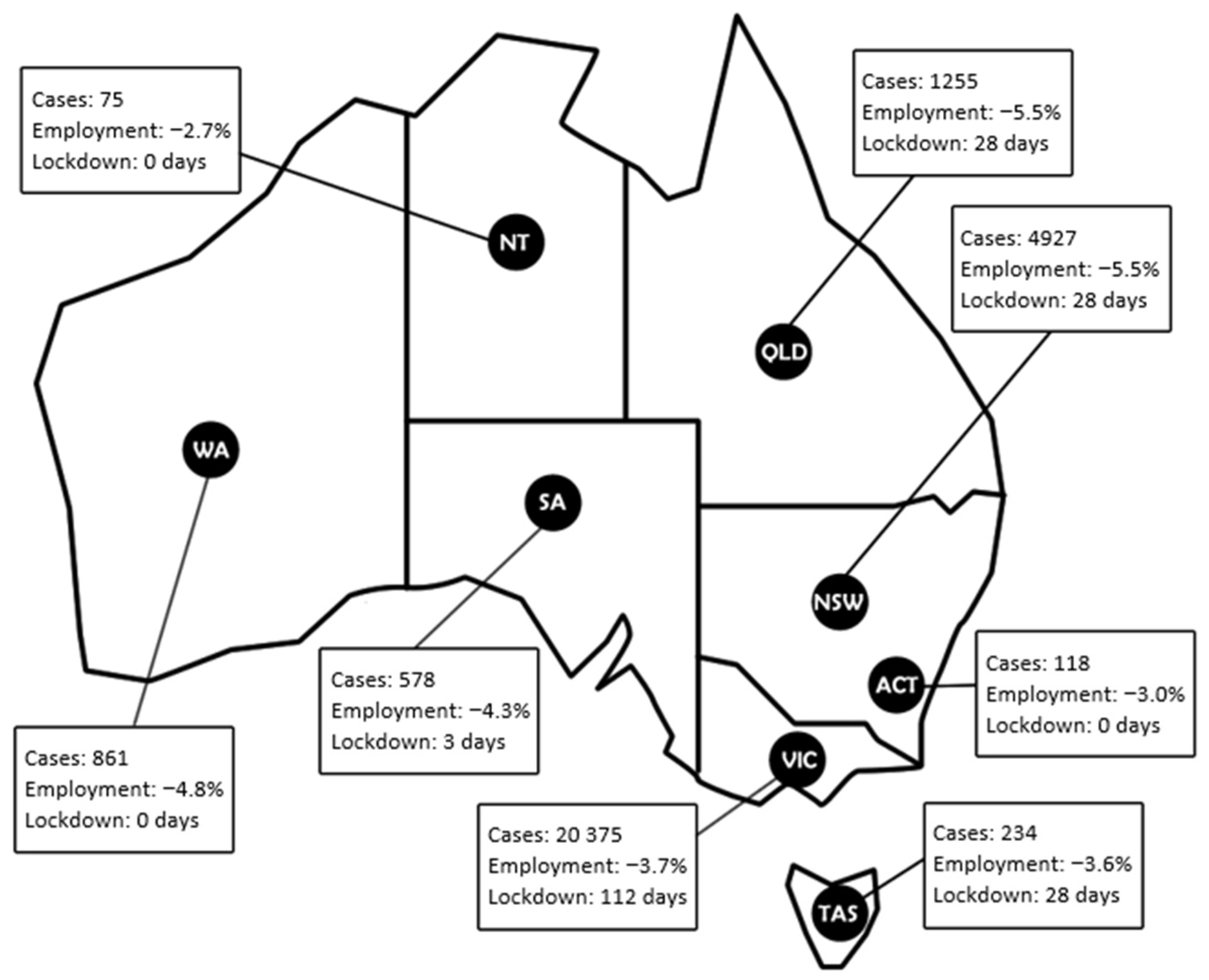
2.2. Participants and Sampling Strategy
2.3. Survey Variables
2.4. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Food Security Status
3.3. Factors Associated with Food Security
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The Committee on Economic Social and Cultural Rights. General Comment No. 12 on the Right to Adequate Food; United Nations: Geneva, Switzerland, 1999. [Google Scholar]
- Food and Agriculture Organization; Committee on World Food Security. Coming to Terms with Terminology 2012. Available online: http://www.fao.org/3/MD776E/MD776E.pdf (accessed on 4 June 2021).
- Hamelin, A.-M.; Beaudry, M.; Habicht, J.-P. Characterization of household food insecurity in Quebec: Food and feelings. Soc. Sci. Med. 2002, 54, 119–132. [Google Scholar] [CrossRef]
- Radimer, K.L.; Olson, C.M.; Campbell, C.C. Development of indicators to assess hunger. J. Nutr. 1990, 120 (Suppl. S11), 1544–1548. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Australian Health Survey: Nutrition—State and Territory Results 2011–2012 Cat No. 4364.0.55.009. 2015. Available online: www.abs.gov.au/ausstats/abs@.nsf/Lookup/1F1C9AF1C156EA24CA257B8E001707B5?opendocument (accessed on 4 June 2021).
- Kleve, S.; Booth, S.; Davidson, Z.E.; Palermo, C. Walking the food security tightrope—Exploring the experiences of low-to-middle income Melbourne households. Int. J. Environ. Res. Public Health 2018, 15, 2206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Temple, J.B. The association between stressful events and food insecurity: Cross-sectional evidence from Australia. Int. J. Environ. Res. Public Health 2018, 15, 2333. [Google Scholar] [CrossRef] [Green Version]
- Gallegos, D.; Ellies, P.; Wright, J. Still there’s no food! Food insecurity in a refugee population in Perth, Western Australia. Nutr. Diet. 2008, 65, 78–83. [Google Scholar] [CrossRef]
- McKay, F.H.; Dunn, M. Food security among asylum seekers in Melbourne. Aust. N. Z. J. Public Health 2015, 39, 344–349. [Google Scholar] [CrossRef] [Green Version]
- Ramsey, R.; Giskes, K.; Turrell, G.; Gallegos, D. Food insecurity among Australian children: Potential determinants, health and developmental consequences. J. Child. Health Care 2011, 15, 401–416. [Google Scholar] [CrossRef]
- Ramsey, R.; Giskes, K.; Turrell, G.; Gallegos, D. Food insecurity among adults residing in disadvantaged urban areas: Potential health and dietary consequences. Public Health Nutr. 2012, 15, 227–237. [Google Scholar] [CrossRef] [Green Version]
- Australian Bureau of Statistics. Australian Aboriginal and Torres Strait Islander Health Survey: Nutrition Results—Food and Nutrients, 2012–2013 (4727.0.55.005). 2015. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4727.0.55.005main+features12012–13 (accessed on 22 June 2021).
- The Hon Greg Hunt MP. First Confirmed Case of Novel Coronavirus in Australia: Department of Health. 2020. Available online: https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/first-confirmed-case-of-novel-coronavirus-in-australia (accessed on 29 July 2021).
- Australian Taxation Office. JobKeeper Payment. 2021. Available online: https://www.ato.gov.au/general/jobkeeper-payment/ (accessed on 22 June 2021).
- Cluver, L.; Lachman, J.M.; Sherr, L.; Wessels, I.; Krug, E.; Rakotomalala, S.; Blight, S.; Hillis, S.; Bachman, G.; Green, O. Parenting in a time of COVID-19. Lancet 2020, 395, e64. [Google Scholar] [CrossRef]
- Mehta, K.; Booth, S.; Coveney, J.; Strazdins, L. Feeding the Australian family: Challenges for mothers, nutrition and equity. Health Promot. Int. 2020, 35, 771–778. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Labour Force, Australia. 2020. Available online: https://www.abs.gov.au/statistics/labour/employment-and-unemployment/labour-force-australia/may-2020 (accessed on 7 July 2021).
- Matheson, J.; McIntyre, L. Women respondents report higher household food insecurity than do men in similar Canadian households. Public Health Nutr. 2014, 17, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Ho, S.K.; Singh, S.; Choi, M.Y. Gender disparities in food security, dietary intake, and nutritional health in the United States. Off. J. Am. Coll. Gastroenterol. ACG 2021, 116, 584–592. [Google Scholar] [CrossRef] [PubMed]
- Connor, J.; Madhavan, S.; Mokashi, M.; Amanuel, H.; Johnson, N.R.; Pace, L.E.; Bartz, D. Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: A review. Soc. Sci. Med. 2020, 266, 113364. [Google Scholar] [CrossRef] [PubMed]
- Neff, L.M. Hidden hunger: Food insecurity in the age of coronavirus. Am. J. Clin. Nutr. 2020, 112, 1160–1161. [Google Scholar] [CrossRef] [PubMed]
- Lamarche, B.; Brassard, D.; Lapointe, A.; Laramée, C.; Kearney, M.; Côté, M.; Bélanger-Gravel, A.; Desroches, S.; Lemieux, S.; Plante, C. Changes in diet quality and food security among adults during the COVID-19–related early lockdown: Results from NutriQuébec. Am. J. Clin. Nutr. 2021, 113, 984–992. [Google Scholar] [CrossRef]
- Fitzpatrick, K.M.; Harris, C.; Drawve, G.; Willis, D.E. Assessing food insecurity among US adults during the COVID-19 pandemic. J. Hunger. Environ. Nutr. 2020, 16, 1–18. [Google Scholar] [CrossRef]
- Kent, K.; Murray, S.; Penrose, B.; Auckland, S.; Visentin, D.; Godrich, S.; Lester, E. Prevalence and socio-demographic predictors of food insecurity in Australia during the COVID-19 pandemic. Nutrients 2020, 12, 2682. [Google Scholar] [CrossRef]
- Online Research Unit. ORU Panels. Available online: https://www.theoru.com/panels.htm (accessed on 10 November 2021).
- Australian Bureau of Statistics. Australian Demographics Statistics 2020. cat. no. 3101.0. 2020. Available online: https://www.abs.gov.au/statistics/people/population/national-state-and-territory-population/latest-release (accessed on 29 July 2021).
- Webb, P.; Bain, C.; Page, A. Essential Epidemiology: An Introduction for Students and Health Professionals, 3rd ed.; Cambridge University Press: Cambridge, UK, 2017. [Google Scholar]
- Bickel, G.; Nord, M.; Price, C.; Hamilton, W.; Cook, J. Guide to Measuring Household Food Security; U.S. Department of Agriculture: Alexandria, VA, USA, 2000; Revised; pp. 1–75.
- Kessler, R.C.; Barker, P.R.; Colpe, L.J.; Epstein, J.F.; Gfroerer, J.C.; Hiripi, E.; Howes, M.J.; Normand, S.-L.T.; Manderscheid, R.W.; Walters, E.E. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 2003, 60, 184–189. [Google Scholar] [CrossRef]
- Andrews, G.; Slade, T. Interpreting scores on the Kessler psychological distress scale (K10). Aust. N. Z. J. Public Health 2001, 25, 494–497. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Household Financial Resources. 2021. Available online: https://www.abs.gov.au/statistics/economy/finance/household-financial-resources/latest-release (accessed on 14 June 2021).
- Niles, M.T.; Bertmann, F.; Belarmino, E.H.; Wentworth, T.; Biehl, E.; Neff, R. The early food insecurity impacts of COVID-19. Nutrients 2020, 12, 2096. [Google Scholar] [CrossRef]
- Statcan. Food Insecurity during the COVID-19 Pandemic, May 2020 Ottawa, Canada: Statcan 2020. Available online: https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00039-eng.htm (accessed on 22 June 2021).
- Loopstra, R. Vulnerability to food insecurity since the COVID-19 lockdown. Lond. Food Found. 2020, 1–4. [Google Scholar]
- Chilton, M.; Knowles, M.; Bloom, S.L. The Intergenerational Circumstances of Household Food Insecurity and Adversity. J. Hunger. Environ. Nutr. 2017, 12, 269–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martin, M.A.; Lippert, A.M. Feeding her children, but risking her health: The intersection of gender, household food insecurity and obesity. Soc. Sci. Med. 2012, 74, 1754–1764. [Google Scholar] [CrossRef] [Green Version]
- Australian Research Alliance for Children and Youth. Report Card 2018: The Wellbeing of Young Australians; Australian Research Alliance for Children and Youth: Canberra, Australia, 2018. [Google Scholar]
- Godrich, S.; Lo, J.; Davies, C.; Darby, J.; Devine, A. Prevalence and socio-demographic predictors of food insecurity among regional and remote Western Australian children. Aust. N. Z. J. Public Health 2017, 41, 585–590. [Google Scholar] [CrossRef]
- Seivwright, A.; Callis, Z.; Flatau, P. Entrenched Disadvantage in Western Australia: Health, Economic and Social Impacts; 100 Families WA: Perth, Australia, 2019. [Google Scholar]
- Velardo, S.; Pollard, C.; Shipman, J.; Booth, S. How Do Disadvantaged Children Perceive, Understand and Experience Household Food Insecurity? Int. J. Environ. Res. Public Health 2021, 18, 4039. [Google Scholar] [CrossRef]
- Thomas, M.; Miller, D.P.; Morrissey, T.W. Food insecurity and child health. Pediatrics 2019, 144, e20190397. [Google Scholar] [CrossRef] [Green Version]
- Perez-Escamilla, F.; de Toledo Vianna, R.P. Food Insecurity and the Behavioral and Intellectual Development of Children: A Review of the Evidence. J. Appl. Res. Child. 2012, 3, 9. [Google Scholar]
- Carroll, N.; Sadowski, A.; Laila, A.; Hruska, V.; Nixon, M.; Ma, D.W.; Haines, J. The impact of COVID-19 on health behavior, stress, financial and food security among middle to high income Canadian families with young children. Nutrients 2020, 12, 2352. [Google Scholar] [CrossRef]
- Ettman, C.K.; Abdalla, S.M.; Cohen, G.H.; Sampson, L.; Vivier, P.M.; Galea, S. Low assets and financial stressors associated with higher depression during COVID-19 in a nationally representative sample of US adults. J. Epidemiol. Community Health 2021, 75, 501–508. [Google Scholar] [CrossRef]
- Maynard, M.; Andrade, L.; Packull-McCormick, S.; Perlman, C.M.; Leos-Toro, C.; Kirkpatrick, S.I. Food insecurity and mental health among females in high-income countries. Int. J. Environ. Res. Public Health 2018, 15, 1424. [Google Scholar] [CrossRef] [Green Version]
- Chang, Y.; Chatterjee, S.; Kim, J. Household finance and food insecurity. J. Fam. Econ. Issues 2014, 35, 499–515. [Google Scholar] [CrossRef]
- Guo, B. Household assets and food security: Evidence from the survey of program dynamics. J. Fam. Econ. Issues 2011, 32, 98–110. [Google Scholar] [CrossRef]
- Victorian Government. Financial and Other Support for COVID-19. 2021. Available online: https://www.coronavirus.vic.gov.au/financial-and-other-support-coronavirus-covid-19 (accessed on 22 June 2021).
- O’Kane, G. COVID-19 puts the spotlight on food insecurity in rural and remote Australia. Aust. J. Rural. Health 2020, 28, 319. [Google Scholar] [CrossRef] [PubMed]
- Horne, R.; Willand, N.; Dorignon, L.; Middha, B. The Lived Experience of COVID-19: Housing and Household Resilience: AHURI Final Report No. 345 Melbourne: Australian Housing and Urban Research Institute Limited. 2020. Available online: https://www.ahuri.edu.au/research/finalreports/345 (accessed on 25 June 2021).
| Demographic | Category | Food Security Status n (%) n = 1005 | p-Value * | |||
|---|---|---|---|---|---|---|
| High (n = 670) | Marginal (n = 138) | Low (n = 119) | Very Low (n = 78) | |||
| State/Territory | Australian Capital Territory | 20 (95.2) | 0 (0.0) | 0 (0.0) | 1 (4.8) | 0.058 |
| New South Wales | 202 (65.0) | 44 (14.1) | 44 (14.1) | 21 (6.8) | ||
| Northern Territory | 2 (66.7) | 0 (0.0) | 0 (0.0) | 1 (33.3) | ||
| Queensland | 128 (64.6) | 36 (18.2) | 22 (11.1) | 12 (6.1) | ||
| South Australia | 47 (69.1) | 5 (7.4) | 12 (17.6) | 4 (5.9) | ||
| Tasmania | 21 (72.4) | 3 (10.3) | 5 (17.2) | 0 (0) | ||
| Victoria | 180 (64.7) | 40 (14.4) | 29 (10.4) | 29 (10.4) | ||
| Western Australia | 70 (72.2) | 10 (10.3) | 7 (7.2) | 10 (10.3) | ||
| Regional/Remote | Inner Regional Australia | 67 (64.4) | 17 (16.3) | 10 (9.6) | 10 (9.6) | 0.705 |
| Major Cities of Australia | 563 (66.5) | 118 (13.9) | 102 (12.0) | 64 (7.6) | ||
| Outer Regional Australia | 30 (71.4) | 3 (7.1) | 5 (11.9) | 4 (9.5) | ||
| Remote Australia | 9 (81.8) | 0 (0) | 2 (18.2) | 0 (0) | ||
| Age | 18–24 | 108(68.4) | 21 (13.3) | 14 (8.9) | 15(9.5) | 0.215 |
| 25–34 | 228 (65.3) | 44 (12.6) | 45 (12.9) | 32 (9.2) | ||
| 35–44 | 219 (66.6) | 49 (14.9) | 46 (14.0) | 15 (4.6) | ||
| 45–50 | 115 (68.0) | 24 (14.2) | 14 (8.3) | 16 (9.5) | ||
| Current Marital Status | Single | 254 (61.2) | 58 (14.0) | 57 (13.7) | 46 (11.1) | 0.005 |
| Married or de facto | 402 (70.0) | 80 (13.9) | 61 (10.6) | 31 (5.4) | ||
| I prefer not to say | 14 (87.5) | 0 (0) | 1 (6.3) | 1(6.3) | ||
| Number of Children | 0 children | 419 (73.1) | 65 (11.3) | 46 (8.0) | 43 (7.5) | <0.01 |
| 1 child | 89 (56.3) | 26 (16.5) | 26 (16.5) | 17 (10.8) | ||
| 2 children | 116 (61.1) | 27(14.2) | 31 (16.3) | 16 (8.4) | ||
| 3 or more children | 46 (55.4) | 19 (22.9) | 16 (19.3) | 2 (2.4) | ||
| Highest Level of Completed Education | Primary/elementary school or less | 2 (40.0) | 0 (0) | 1 (20.0) | 2 (40.0) | 0.003 |
| Secondary/high school | 112 (58.0) | 27 (14.0) | 29 (15.0) | 25 (13.0) | ||
| TAFE | 156 (65.0) | 37 (15.4) | 32 (13.3) | 15 (6.3) | ||
| University/Post-graduate degree | 397 (70.8) | 71 (12.7) | 57 (10.2) | 36 (6.4) | ||
| Self-identified cultural/ethnic group | Oceanian (Australian peoples, New Zealand peoples, Pacific Islanders) | 367 (65.4) | 75 (13.4) | 68 (12.1) | 51 (9.1) | 0.830 |
| North-west European (British, Irish, Western European, Northern European) | 106 (66.7) | 25 (15.7) | 17 (10.7) | 11 (6.9) | ||
| South East Asian | 56 (70.0) | 11 (13.8) | 11 (13.8) | 2 (2.5) | ||
| Southern and Eastern European (Southern European, South Eastern European, Eastern European) | 47 (65.3) | 13 (18.1) | 9 (12.5) | 3 (4.2) | ||
| North East Asian | 21 (60.0) | 5 (14.3) | 5 (14.3) | 4 (11.4) | ||
| North African and Middle Eastern (Arab, Jewish, Peoples of the Sudan, other North African and Middle Eastern) | 13 (72.2) | 1 (5.6) | 3 (16.7) | 1 (5.6) | ||
| North American | 10 (90.9) | 1 (9.1) | 0 (0) | 0 (0) | ||
| Southern and Central Asian | 9 (81.8) | 1 (9.1) | 1 (9.1) | 0 (0) | ||
| Southern and East African | 6 (100.0) | 0 (0) | 0 (0) | 0 (0) | ||
| South American | 3 (42.9) | 1 (14.3) | 2 (28.6) | 1 (14.3) | ||
| I prefer not to say | 32(71.1) | 5 (11.1) | 3 (6.7) | 5 (11.1) | ||
| Housing status | Own home | 350 (71.1) | 62 (12.6) | 54 (11.0) | 26 (5.3) | 0.006 |
| Rented home | 178 (58.6) | 46 (15.1) | 41 (13.5) | 39 (12.8) | ||
| Living with family | 136 (68.7) | 27 (13.6) | 22 (11.1) | 13 (6.6) | ||
| Emergency accommodation (hostel, B&B, hotel) | 0 (0) | 1 (50.0) | 1 (50.0) | 0 (0) | ||
| I prefer not to say | 6 (66.7) | 2 (22.2) | 1 (11.1) | 0 (0) | ||
| Mental Health Score (K10) | K10 ≥ 20 | 257 (52.4) | 88 (18.0) | 81 (16.5) | 64 (13.1) | <0.001 |
| Pre COVID-19 employment | Full-time employment | 372 (72.8) | 57 (11.2) | 47 (9.2) | 35 (6.8) | 0.014 |
| Casual employment | 47 (65.3) | 9 (12.5) | 8 (11.1) | 8 (11.1) | ||
| Government assistance | 18 (62.1) | 4 (13.8) | 5 (17.2) | 2 (6.9) | ||
| Government disability support | 9 (50.0) | 4 (22.2) | 2 (11.1) | 3 (16.7) | ||
| Homemaker | 57 (56.4) | 18 (17.8) | 13 (12.9) | 13 (12.9) | ||
| Part-time employment | 115 (62.2) | 34 (18.4) | 29 (15.7) | 7 (3.8) | ||
| Retired | 2 (50.0) | 0 (0.0) | 1 (25.0) | 1 (25.0) | ||
| Student | 42 (62.7) | 7 (10.4) | 12 (17.9) | 6 (9.0) | ||
| Pref not say | 8 (44.4) | 5 (27.8) | 2 (11.1) | 3 (16.7) | ||
| Pre COVID-19 household income (AUD) | 0–24,999 | 19 (32.2) | 15 (25.4) | 12 (20.3) | 13 (22.0) | <0.001 |
| 25,000–49,999 | 42 (46.2) | 15 (16.5) | 21 (23.1) | 13 (14.3) | ||
| 50,000–74,999 | 70 (54.7) | 17 (13.3) | 23 (18.0) | 18 (14.1) | ||
| 75,00–99,999 | 103 (65.2) | 26 (16.5) | 14 (8.9) | 15 (9.5) | ||
| 100,000–124,999 | 86 (69.4) | 18 (14.5) | 14 (11.3) | 6 (4.8) | ||
| 125,000–149,999 | 72 (76.6) | 11 (11.7) | 7 (7.4) | 4 (4.3) | ||
| >150,000 | 178 (84.4) | 19 (9.0) | 9 (4.3) | 5 (2.4) | ||
| Change in employment status due to COVID-19 | Yes | 127 (50.4) | 39 (15.5) | 43 (17.1) | 43 (17.1) | <0.001 |
| No | 543 (72.1) | 99 (13.1) | 76 (10.1) | 35 (4.6) | ||
| Employment status due to COVID-19 | Full-time employment | 27(54.0) | 3 (6.0) | 7 (14.0) | 13 (26.0) | 0.602 |
| Casual employment | 19 (46.3) | 11 (26.8) | 6 (14.6) | 5 (12.2) | ||
| Government assistance e.g., family payments | 1 (11.10) | 3 (33.3) | 1 (11.1) | 4 (44.4) | ||
| Government assistance e.g., Job Keeper | 10 (45.5) | 4 (18.2) | 6 (27.3) | 2 (9.1) | ||
| Government assistance e.g., Job Seeker | 17 (53.1) | 5 (15.6) | 5 (15.6) | 5 (15.6) | ||
| Government disability support | 2 (50.0) | 1 (25.0) | 0 (0.0) | 1 (25.0) | ||
| Homemaker | 5 (50.0) | 2 (20.0) | 2 (20.0) | 1 (10.0) | ||
| Part-time employment | 30 (53.6) | 8 (14.3) | 11 (19.6) | 7 (12.5) | ||
| Retired | 1 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0) | ||
| Student | 9 (50.0) | 1 (5.6) | 4 (22.2) | 4 (22.2) | ||
| I don’t know/I prefer not to answer | 6 (66.7) | 1 (11.1) | 1 (11.1) | 1 (11.1) | ||
| USDA Household Food Security Survey Module Question | Response Option | Food Security Status n (%) | p Value * | |||
|---|---|---|---|---|---|---|
| High | Marginal | Low | Very Low | |||
| Adult Question Items in the Last 6 Months | ||||||
| (I/We) worried whether (my/our) food would run out before (I/we) got money to buy more | Sometimes true/often true | 0 (0.0) | 73 (9.9) | 10 (1.4) | 4 (0.5) | <0.001 |
| Never true | 652 (88.2) | 19 (11.3) | 78 (46.4) | 71 (42.30) | ||
| I don’t know/I prefer not to answer | 18 (78.3) | 2 (8.7) | 3 (13.0) | 0 (0.0) | ||
| The food that (I/we) bought just didn’t last and (I/we) didn’t have money to get more | Sometimes true/often true | 0 (0.0) | 19 (11.3) | 78 (46.4) | 71 (42.3) | <0.001 |
| Never true | 655 (80.3) | 116 (14.2) | 39 (4.8) | 6 (0.7) | ||
| I don’t know/I prefer not to answer | 15 (71.4) | 3 (14.3) | 2 (9.5) | 1 (4.8) | ||
| (I/we) couldn’t afford to eat balanced meals | Sometimes true/often true | 0 (0.0) | 60 (25.9) | 98 (42.2) | 74 (31.9) | <0.001 |
| Never true | 653 (86.7) | 76 (10.1) | 21 (2.8) | 3 (0.4) | ||
| I don’t know/I prefer not to answer | 17 (85.0) | 2 (10.0) | 0 (0.0) | 1 (5.0) | ||
| In the last 6 months since last did you or other adults in your household ever cut the size of your meals or skip meals because there wasn’t enough money for food | Yes | N/A | 1 (0.9) | 34 (31.5) | 73 (67.6) | <0.001 |
| No | N/A | 111 (57.5) | 78 (40.4) | 4 (2.1) | ||
| I don’t know/I prefer not to answer | N/A | 4 (54.5) | 6 (9.1) | 1 (36.4) | ||
| How often did this happen—almost every month some months but not every month or in only 1 or 2 months | Only 1 or 2 months | N/A | 1 (3.7) | 17 (63.0) | 9 (33.3) | 0.002 |
| Almost every month/Some months but not every month | N/A | 0 (0.0) | 16 (20.3) | 63 (79.7) | ||
| I don’t know/I prefer not to answer | N/A | 0 (0.0) | 1 (50.0) | 1 (50.0) | ||
| In the last 6 months did you ever eat less than you felt you should because there wasn’t enough money for food? | Yes | N/A | 7 (5.7) | 44 (36.1) | 71 (58.2) | <0.001 |
| No | N/A | 106 (58.6) | 69 (38.1) | 6 (3.3) | ||
| I don’t know/I prefer not to answer | N/A | 3 (33.3) | 5 (55.6) | 1 (11.1) | ||
| In the last 6 months were you every hungry but didn’t eat because there wasn’t enough money for food? | Yes | N/A | 1 (1.1) | 27(29.0) | 65 (69.9) | <0.001 |
| No | N/A | 114 (54.00) | 86 (40.8) | 11 (5.2) | ||
| I don’t know/I prefer not to answer | N/A | 1 (12.5) | 5 (62.5) | 2 (25.0) | ||
| In the last 6 months did you lose weight because there wasn’t enough money for food? | Yes | N/A | 1 (1.7) | 10 (16.9) | 48 (81.4) | <0.001 |
| No | N/A | 115 (48.9) | 99 (42.1) | 21 (8.9) | ||
| I don’t know/I prefer not to answer | N/A | 0 (0.0) | 9 (50.0) | 9 (50.0) | ||
| In the last 6 months did (you/you or other adults in your household) ever not eat for a whole day because there wasn’t enough money for food? | Yes | N/A | 0 (0.0) | 2 (4.7) | 41 (95.3) | <0.001 |
| No | N/A | 9 (8.5) | 60 (56.6) | 37 (34.9) | ||
| I don’t know/I prefer not to answer | N/A | 1 (25.0) | 3 (75.0) | 0 (0.0) | ||
| How often did this happen—almost every month some months but not every month or in only 1 or 2 months? | Only 1 or 2 months | N/A | N/A | 2 (22.2) | 7 (77.8) | 0.004 |
| Almost every month/Some months but not every month | N/A | N/A | 0 (0.00) | 34 (100) | ||
| Child Question Items in the last 6 months | ||||||
| I relied on only a few kinds of low-cost food to feed my child/the children because we were running out of money to buy food. | Often true/Sometimes true | 0 (0.0) | 35 (28.0) | 56 (44.8) | 34 (27.2) | <0.001 |
| Never true | 245 (82.5) | 36 (12.1) | 15 (5.1) | 1 (0.3) | ||
| I don’t know/I prefer not to answer | 6 (66.7) | 1 (11.1) | 2 (22.2) | 0 (0.0) | ||
| I couldn’t feed my child/the children a balanced meal because we couldn’t afford that. | Often true/Sometimes true | 0 (0.0) | 2 (7.4) | 13 (48.1) | 12 (44.0) | <0.001 |
| Never true | 87 (68.5) | 24 (18.9) | 12 (9.4) | 4 (3.1) | ||
| I don’t know/I prefer not to answer | 2 (50.0) | 0 (0.0) | 1 (25.0) | 1 (25.0) | ||
| My child was/The children were not eating enough because we just couldn’t afford enough food. | Often true/Sometimes true | 0 (0.00) | 0 (0.0) | 8 (47.1) | 9 (52.9) | <0.001 |
| Never true | 87 (64.00) | 26 (19.1) | 16 (11.8) | 7 (5.1) | ||
| In the last 6 months did you ever cut the size of your childs/any of the children’s meals because there wasn’t enough money for food? | Yes | N/A | 3 (15.8) | 2 (10.5) | 14 (73.7) | <0.001 |
| No | N/A | 34 (31.5) | 55 (50.9) | 19 (17.6) | ||
| In the last 6 months did any of the children ever skip meals because there wasn’t enough money for food? | Yes | N/A | 0 (0.0) | 0 (0.0) | 12 (100.0) | 0.001 |
| No | N/A | 37 (31.9) | 57 (49.1) | 22 (19.0) | ||
| How often did this happen—almost every month some months but not every month or in only 1 or 2 months? | Only 1 or 2 months | N/A | N/A | N/A | 2 (100.0) | <0.001 |
| Almost every month/Some months but not every month | N/A | N/A | N/A | 10 (100.0) | ||
| In the last 6 months was your child/were the children ever hungry but you just couldn’t afford more food? | Yes | 0 (0.00) | 0 (0.0) | 11 (100) | 0 (0.0) | <0.001 |
| No | 37 (31.9) | 56 (48.3) | 23 (19.8) | 37 (31.9) | ||
| I don’t know/I prefer not to answer | 0 (0.0) | 2 (100) | 0 (0.00) | 0 (0.0) | ||
| In the last 6 months did your child/any of the children ever not eat for a whole day because there wasn’t enough money for food? | Yes | 0 | 0 | 9 (100) | 0 | <0.001 |
| No | 37 (31.9) | 56 (48.3) | 23 (19.8) | 37 (31.9) | ||
| I don’t know/I prefer not to answer | 0 (0.0) | 2 (50.0) | 2 (50.0) | 0 (0.0) | ||
| Marginal Food Security | Low Food Security | Very Low Food Security | ||||
|---|---|---|---|---|---|---|
| OR (95%CI) | p-Value | OR (95%CI) | p-Value | OR (95%CI) | p-Value | |
| State | ||||||
| State (all other states) | Ref | Ref | Ref | Ref | Ref | Ref |
| NSW | 1.158 (0.643–1.934) | 0.576 | 1.144 (0.643–2.037) | 0.647 | 0.718 (0.339–1.522) | 0.388 |
| VIC | 1.090 (0.646–1.839) | 0.746 | 0.714 (0.384–2.135) | 0.285 | 1.171 (0.593–2.314) | 0.649 |
| Current marital status | ||||||
| Marital status (married/de facto) | Ref | Ref | Ref | Ref | Ref | Ref |
| Single | 0.910 (0.526–1.572) | 0.734 | 1.163 (0.628–2.153) | 0.631 | 1.516 (0.751–3.061) | 0.245 |
| I prefer not to say | N/A | N/A | N/A | N/A | 4.688 (0.299–73.591) | 0.271 |
| Number of children | ||||||
| No children | Ref | Ref | Ref | Ref | Ref | Ref |
| 1 child | 2.241 (1.238–4.055) | 0.008 | 3.938 (1.997–7.765) | <0.001 | 2.578 (1.172–5.675) | 0.019 |
| 2 children | 1.932 (1.034–3.608) | 0.039 | 3.811 (1.921–7.561) | <0.001 | 2.434 (1.045–5.673) | 0.039 |
| >3 children | 3.587 (1.677–7.672) | <0.001 | 6.243 (2.593–15.032) | <0.001 | 0.305 (0.034–2.715) | 0.287 |
| Education | ||||||
| Education (university/post-grad) | Ref | Ref | Ref | Ref | Ref | Ref |
| TAFE | 0.870 (0.509–1.486) | 0.609 | 0.911 (0.495–1.676) | 0.765 | 0.631 (0.294–1.352) | 0.236 |
| High School | 1.116 (0.623–2.003) | 0.712 | 1.188 (0.621–2.274) | 0.603 | 1.312 (0.621–2.774) | 0.477 |
| Primary school | N/A | N/A | 1.308 (0.056–30.476) | 0.867 | 2.002 (0.117–34.327) | 0.632 |
| Housing tenure | ||||||
| Own Home | Ref | Ref | Ref | Ref | Ref | Ref |
| Rented home | 1.238 (0.750–20.41) | 0.404 | 1.015 (0.578–1.782) | 0.959 | 2.102 (1.091–4.048) | 0.026 |
| Living with family | 1.505 (0.805–2.811) | 0.200 | 0.631 (0.290–1.374) | 0.246 | 0.711 (0.275–1.842) | 0.483 |
| Emergency accommodation | N/A | N/A | N/A | N/A | N/A | N/A |
| Mental health | ||||||
| Mental health above 20 | 2.51 (1.612 -3.909) | <0.001 | 5.360 (3.097–9.278) | <0.001 | 7.065 (3.404–14.662) | <0.001 |
| Pre-COVID19 employment | ||||||
| Job (full time) | Ref | Ref | Ref | Ref | Ref | Ref |
| Casual | 0.508 (0.183–1.410) | 0.194 | 0.803 (0.278–0.316) | 0.684 | 0.939 (3.18–2.773) | 0.910 |
| Government assistance | 0.365 (0.091 (1.469) | 0.156 | 0.789 (0.212–2.941) | 0.724 | 0.383 (0.070–2.095) | 0.268 |
| Government disability support | 1.460 (0.296–7.207) | 0.643 | 1.050 (0.159–6.920) | 0.959 | 1.740 (0.266–11.383) | 0.563 |
| Homemaker | 0.825 (0.363–1.879) | 0.647 | 0.619 (0.226–1.691) | 0.349 | 2.212 (0.735 -6.656) | 0.158 |
| Part-time | 1.134 (0.641–2.008) | 0.666 | 1.293 (0.670–2.495) | 0.444 | 0.484 (0.184–1.271) | 0.141 |
| Retired | N/A | N/A | N/A | N/A | 1.927 (0.113–32.857) | 0.650 |
| Student | 0.636 (0.217–1.859) | 0.408 | 1.573 (0.553 -4.472) | 0.395 | 1.178 (0.346–4.013) | 0.793 |
| I don’t know/I prefer not to say | 0.833 (0.178–4.383) | 0.879 | 1.344 (0.219–8.257) | 0.750 | 0.435 (0.042–4517) | 0.485 |
| Pre-COVID19 income | ||||||
| Income > $150,000 | Ref | Ref | Ref | Ref | Ref | Ref |
| $125,000–149,999 | 1.510 (0.662–3.444) | 0.327 | 2.040 (0.645–6.449) | 0.225 | 1.312 (0.302–5.693) | 0.717 |
| $100,000–$124,999 | 2.064 (1.000–4.265) | 0.050 | 3.539 (1.355–9.242) | 0.010 | 1.867 (0.506–6.887) | 0.348 |
| $75,00–$99,999 | 2.187 (1.095–4.367) | 0.027 | 2.729 (10.35–7.195) | 0.042 | 3.036 (0.971–9.661) | 0.056 |
| $50,000–$74,999 | 2.198 (0.996–4.848) | 0.051 | 7.424 (2.871–19.195) | <0.001 | 4.407 (1.38–13.992) | 0.012 |
| $25,000–$49,999 | 4.371 (1.748–10.932) | 0.002 | 10.877 (3.692–32.042) | <0.001 | 6.166 (1.689–22.512) | 0.006 |
| $0–$24,999 | 8.896 (3.127–25.308) | <0.001 | 10.293 (2.836–37.359) | <0.001 | 8.976 (2.175–37.033) | 0.002 |
| Change in employment status | ||||||
| Has your employment status changed since COVID-19—Yes | 1.611 (0.985–2.636) | 0.57 | 2.222 (1.306–3.779) | 0.003 | 6.513 (3.475–12.207) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kleve, S.; Bennett, C.J.; Davidson, Z.E.; Kellow, N.J.; McCaffrey, T.A.; O’Reilly, S.; Enticott, J.; Moran, L.J.; Harrison, C.L.; Teede, H.; et al. Food Insecurity Prevalence, Severity and Determinants in Australian Households during the COVID-19 Pandemic from the Perspective of Women. Nutrients 2021, 13, 4262. https://doi.org/10.3390/nu13124262
Kleve S, Bennett CJ, Davidson ZE, Kellow NJ, McCaffrey TA, O’Reilly S, Enticott J, Moran LJ, Harrison CL, Teede H, et al. Food Insecurity Prevalence, Severity and Determinants in Australian Households during the COVID-19 Pandemic from the Perspective of Women. Nutrients. 2021; 13(12):4262. https://doi.org/10.3390/nu13124262
Chicago/Turabian StyleKleve, Sue, Christie J. Bennett, Zoe E. Davidson, Nicole J. Kellow, Tracy A. McCaffrey, Sharleen O’Reilly, Joanne Enticott, Lisa J. Moran, Cheryce L. Harrison, Helena Teede, and et al. 2021. "Food Insecurity Prevalence, Severity and Determinants in Australian Households during the COVID-19 Pandemic from the Perspective of Women" Nutrients 13, no. 12: 4262. https://doi.org/10.3390/nu13124262
APA StyleKleve, S., Bennett, C. J., Davidson, Z. E., Kellow, N. J., McCaffrey, T. A., O’Reilly, S., Enticott, J., Moran, L. J., Harrison, C. L., Teede, H., & Lim, S. (2021). Food Insecurity Prevalence, Severity and Determinants in Australian Households during the COVID-19 Pandemic from the Perspective of Women. Nutrients, 13(12), 4262. https://doi.org/10.3390/nu13124262









