Trajectories of Energy Intake Distribution and Risk of Dyslipidemia: Findings from the China Health and Nutrition Survey (1991–2018)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Participants
2.3. Calculation of Proportions of Energy Intake from Breakfast, Lunch and Dinner
2.4. Outcome Measures
2.5. Assessment of Covariates
2.6. Statistical Analysis
3. Results
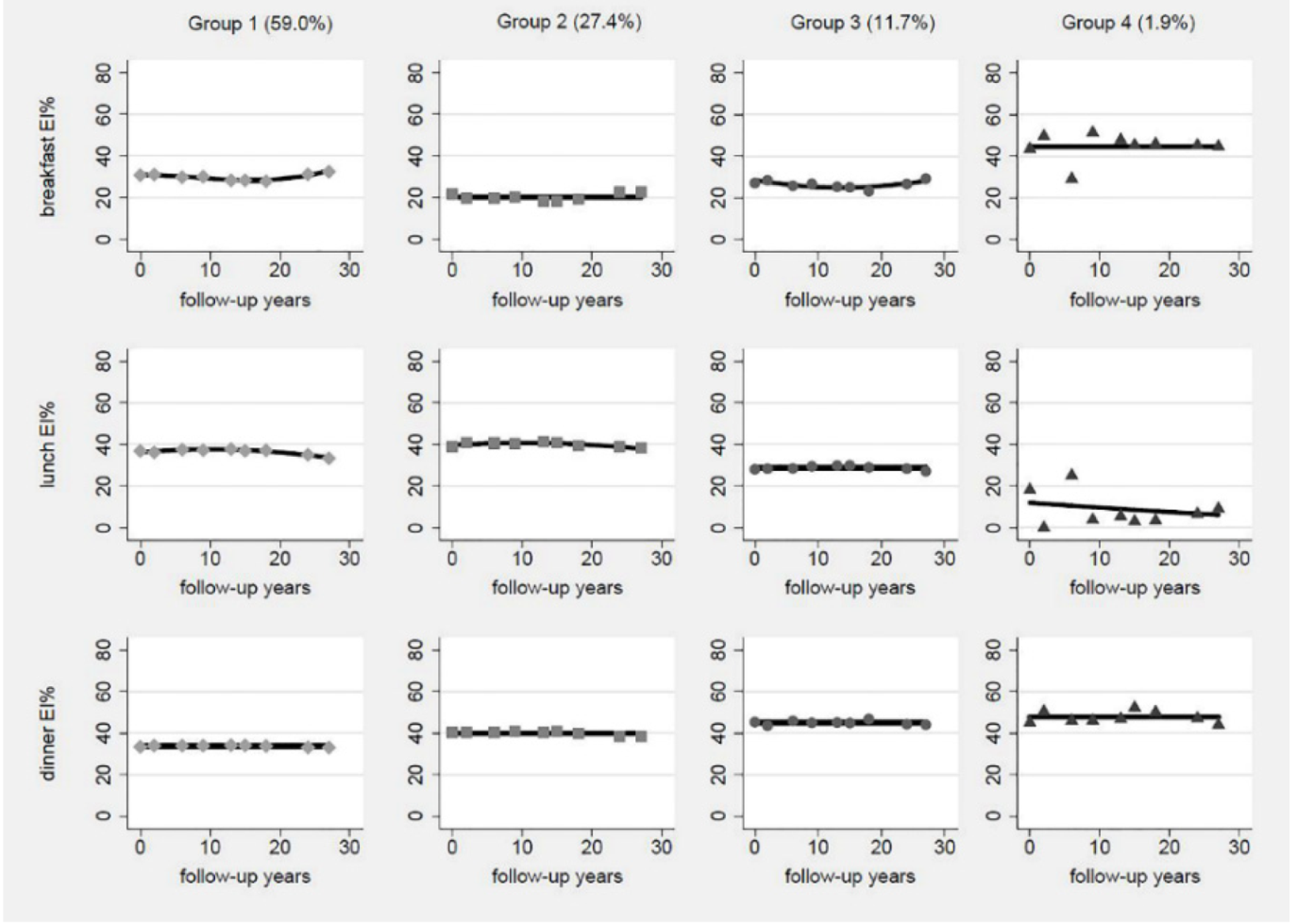
3.1. Trajectory Groups of Energy Intake Distribution
3.2. Baseline Characteristics by Trajectory Groups
3.3. Trajectory Groups of Energy Intake Distribution and Dyslipidemia
3.4. Cumulative Averages of Proportions of Energy from Breakfast, Lunch, Dinner and Dyslipidemia
3.5. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ference, B.A.; Ginsberg, H.N.; Graham, I.; Ray, K.K.; Packard, C.J.; Bruckert, E.; Hegele, R.A.; Krauss, R.M.; Raal, F.J.; Schunkert, H.; et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2017, 38, 2459–2472. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Zeng, F.F.; Liu, Z.M.; Zhang, C.X.; Ling, W.H.; Chen, Y.M. Effects of blood triglycerides on cardiovascular and all-cause mortality: A systematic review and meta-analysis of 61 prospective studies. Lipids Health Dis. 2013, 12, 159. [Google Scholar] [CrossRef] [Green Version]
- Nagasawa, S.Y.; Okamura, T.; Iso, H.; Tamakoshi, A.; Yamada, M.; Watanabe, M.; Murakami, Y.; Miura, K.; Ueshima, H. Evidence for Cardiovascular Prevention from Observational Cohorts in Japan Research, G. Relation between serum total cholesterol level and cardiovascular disease stratified by sex and age group: A pooled analysis of 65 594 individuals from 10 cohort studies in Japan. J. Am. Heart Assoc. 2012, 1, e001974. [Google Scholar] [CrossRef] [Green Version]
- Di Angelantonio, E.; Sarwar, N.; Perry, P.; Kaptoge, S.; Ray, K.; Thompson, A.; Wood, A.; Lewington, S.; Sattar, N.; Packard, C.; et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA 2009, 302, 1993–2000. [Google Scholar] [CrossRef] [Green Version]
- Kopin, L.; Lowenstein, C. Dyslipidemia. Ann. Intern. Med. 2017, 167, ITC81–ITC96. [Google Scholar] [CrossRef]
- Gomez-Delgado, F.; Katsiki, N.; Lopez-Miranda, J.; Perez-Martinez, P. Dietary habits, lipoprotein metabolism and cardiovascular disease: From individual foods to dietary patterns. Crit. Rev. Food Sci. Nutr. 2021, 61, 1651–1669. [Google Scholar] [CrossRef]
- Kim, D.; Hanzawa, F.; Sun, S.; Laurent, T.; Ikeda, S.; Umeki, M.; Mochizuki, S.; Oda, H. Delayed Meal Timing, a Breakfast Skipping Model, Increased Hepatic Lipid Accumulation and Adipose Tissue Weight by Disintegrating Circadian Oscillation in Rats Fed a High-Cholesterol Diet. Front. Nutr. 2021, 8, 681436. [Google Scholar] [CrossRef]
- Zhang, X.; Wu, Y.; Na, M.; Lichtenstein, A.H.; Xing, A.; Chen, S.; Wu, S.; Gao, X. Habitual Night Eating Was Positively Associated With Progress of Arterial Stiffness in Chinese Adults. J. Am. Heart Assoc. 2020, 9, e016455. [Google Scholar] [CrossRef]
- Wang, J.B.; Patterson, R.E.; Ang, A.; Emond, J.A.; Shetty, N.; Arab, L. Timing of energy intake during the day is associated with the risk of obesity in adults. J. Hum. Nutr. Diet. 2014, 27, 255–262. [Google Scholar] [CrossRef]
- Chen, H.J.; Chuang, S.Y.; Chang, H.Y.; Pan, W.H. Energy intake at different times of the day: Its association with elevated total and LDL cholesterol levels. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 390–397. [Google Scholar] [CrossRef]
- Pot, G.K.; Hardy, R.; Stephen, A.M. Irregularity of energy intake at meals: Prospective associations with the metabolic syndrome in adults of the 1946 British birth cohort. Br. J. Nutr. 2016, 115, 315–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pot, G.K.; Hardy, R.; Stephen, A.M. Irregular consumption of energy intake in meals is associated with a higher cardiometabolic risk in adults of a British birth cohort. Int. J. Obes. (Lond.) 2014, 38, 1518–1524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leech, R.M.; Timperio, A.; Livingstone, K.M.; Worsley, A.; McNaughton, S.A. Temporal eating patterns: Associations with nutrient intakes, diet quality, and measures of adiposity. Am. J. Clin. Nutr. 2017, 106, 1121–1130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eicher-Miller, H.A.; Khanna, N.; Boushey, C.J.; Gelfand, S.B.; Delp, E.J. Temporal Dietary Patterns Derived among the Adult Participants of the National Health and Nutrition Examination Survey 1999–2004 Are Associated with Diet Quality. J. Acad. Nutr. Diet. 2016, 116, 283–291. [Google Scholar] [CrossRef] [Green Version]
- Aqeel, M.M.; Guo, J.; Lin, L.; Gelfand, S.B.; Delp, E.J.; Bhadra, A.; Richards, E.A.; Hennessy, E.; Eicher-Miller, H.A. Temporal Dietary Patterns Are Associated with Obesity in US Adults. J. Nutr. 2020, 150, 3259–3268. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Zhai, F.Y.; Du, S.F.; Popkin, B.M. The China Health and Nutrition Survey, 1989–2011. Obes. Rev. 2014, 15 (Suppl. S1), 2–7. [Google Scholar] [CrossRef] [Green Version]
- Joint Committee on Revision of Guidelines for Prevention and Treatment of Dyslipidemia in Chinese Adults. Chinese guideline for the management of dyslipidemia (2016). Chin. Circ. J. 2016, 31, 937–953. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R., Jr.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000, 32, S498–S504. [Google Scholar] [CrossRef] [Green Version]
- Mengyu, F.; Jun, L.; Pingping, H. Chinese guildline for data processing and analysis concerning the International Physical Activity Questionnaire. Chin. J. Epidemiol. 2014, 35, 961–964. [Google Scholar]
- Su, C.; Song, X.; Hu, H.; Du, W.; Wang, H.; Zhang, B. Longitudinal Association between Urbanicity and Total Dietary Fat Intake in Adults in Urbanizing China from 1991 to 2015: Findings from the CHNS. Nutrients 2020, 12, 1597. [Google Scholar] [CrossRef]
- Huang, F.; Wang, Z.; Wang, L.; Wang, H.; Zhang, J.; Du, W.; Su, C.; Jia, X.; Ouyang, Y.; Wang, Y.; et al. Evaluating adherence to recommended diets in adults 1991–2015: Revised China dietary guidelines index. Nutr. J. 2019, 18, 70. [Google Scholar] [CrossRef]
- Nagin, D.S.; Jones, B.L.; Passos, V.L.; Tremblay, R.E. Group-based multi-trajectory modeling. Stat. Methods Med. Res. 2018, 27, 2015–2023. [Google Scholar] [CrossRef]
- van der Nest, G.; Lima Passos, V.; Candel, M.J.J.M.; van Breukelen, G.J.P. An overview of mixture modelling for latent evolutions in longitudinal data: Modelling approaches, fit statistics and software. Adv. Life Course Res. 2020, 43, 100323. [Google Scholar] [CrossRef]
- Zou, G. A modified poisson regression approach to prospective studies with binary data. Am. J. Epidemiol. 2004, 159, 702–706. [Google Scholar] [CrossRef]
- Hu, F.; Stampfer, M.; Rimm, E.; Ascherio, A.; Rosner, B.; Spiegelman, D.; Willett, W. Dietary fat and coronary heart disease: A comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am. J. Epidemiol. 1999, 149, 531–540. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almoosawi, S.; Winter, J.; Prynne, C.J.; Hardy, R.; Stephen, A.M. Daily profiles of energy and nutrient intakes: Are eating profiles changing over time? Eur. J. Clin. Nutr. 2012, 66, 678–686. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, Y.; Li, Y.; Yang, X.; Hemler, E.C.; Fang, Y.; Zhao, L.; Zhang, J.; Yang, Z.; Wang, Z.; He, L.; et al. The dietary transition and its association with cardiometabolic mortality among Chinese adults, 1982–2012: A cross-sectional population-based study. Lancet Diabetes Endocrinol. 2019, 7, 540–548. [Google Scholar] [CrossRef]
- Zhai, F.; Wang, H.; Du, S.; He, Y.; Wang, Z.; Ge, K.; Popkin, B.M. Prospective study on nutrition transition in China. Nutr. Rev. 2009, 67 (Suppl. S1), S56–S61. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Zhai, F.; Du, S.; Popkin, B. Dynamic shifts in Chinese eating behaviors. Asia Pac. J. Clin. Nutr. 2008, 17, 123–130. [Google Scholar]
- Leech, R.M.; Timperio, A.; Worsley, A.; McNaughton, S.A. Eating patterns of Australian adults: Associations with blood pressure and hypertension prevalence. Eur. J. Nutr. 2019, 58, 1899–1909. [Google Scholar] [CrossRef] [Green Version]
- Almoosawi, S.; Vingeliene, S.; Karagounis, L.G.; Pot, G.K. Chrono-nutrition: A review of current evidence from observational studies on global trends in time-of-day of energy intake and its association with obesity. PLoS Comput. Biol. 2016, 75, 487–500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoshida, J.; Eguchi, E.; Nagaoka, K.; Ito, T.; Ogino, K. Association of night eating habits with metabolic syndrome and its components: A longitudinal study. BMC Public Health 2018, 18, 1366. [Google Scholar] [CrossRef] [PubMed]
- Gu, C.; Brereton, N.; Schweitzer, A.; Cotter, M.; Duan, D.; Børsheim, E.; Wolfe, R.R.; Pham, L.V.; Polotsky, V.Y.; Jun, J.C. Metabolic Effects of Late Dinner in Healthy Volunteers-A Randomized Crossover Clinical Trial. J. Clin. Endocrinol. Metab. 2020, 105, 2789–2802. [Google Scholar] [CrossRef] [PubMed]
- Hibi, M.; Masumoto, A.; Naito, Y.; Kiuchi, K.; Yoshimoto, Y.; Matsumoto, M.; Katashima, M.; Oka, J.; Ikemoto, S. Nighttime snacking reduces whole body fat oxidation and increases LDL cholesterol in healthy young women. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2013, 304, R94–R101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, L.; Li, X.; Du, X.; Liu, W.; Du, J.; Guo, L.; Xia, S.; Yuan, Y.; Zheng, Y.; Wu, S.; et al. Cross-sectional association of meal skipping with lipid profiles and blood glucose in Chinese adults. Nutrition 2021, 90, 111245. [Google Scholar] [CrossRef] [PubMed]
- Cella, L.K.; Cauter, E.V.; Schoeller, D. Diurnal rhythmicity of human cholesterol synthesis: Normal pattern and adaptation to simulated. Am. J. Physiol. 1995, 269, E489. [Google Scholar] [CrossRef]
- Jones, P.J.; Schoeller, D.A. Evidence for diurnal periodicity in human cholesterol synthesis. J. Lipid Res. 1990, 31, 667–673. [Google Scholar] [CrossRef]
- Galman, C.; Angelin, B.; Rudling, M. Bile acid synthesis in humans has a rapid diurnal variation that is asynchronous with cholesterol synthesis. Gastroenterology 2005, 129, 1445–1453. [Google Scholar] [CrossRef]
- Arasaradnam, M.; Morgan, L.; Wright, J.; Gama, R. Diurnal variation in lipoprotein lipase activity. Ann. Clin. Biochem. 2002, 39, 136–139. [Google Scholar] [CrossRef]
- Huang, Y.; Li, X.; Wang, M.; Ning, H.; A, L.; Li, Y.; Sun, C. Lipoprotein lipase links vitamin D, insulin resistance, and type 2 diabetes: A cross-sectional epidemiological study. Cardiovasc. Diabetol. 2013, 12, 17. [Google Scholar] [CrossRef] [Green Version]

| Baseline Characteristics | Group 1 | Group 2 | Group 3 | Group 4 | p Value |
|---|---|---|---|---|---|
| (n = 1676) | (n = 779) | (n = 334) | (n = 54) | ||
| Age (year, mean [SD]) | 53.63 (11.55) | 53.59 (12.38) | 52.36 (11.50) | 57.33 (9.25) | 0.028 |
| Sex (%) | |||||
| Male | 720 (42.96) | 376 (48.27) | 164 (49.10) | 26 (48.15) | 0.027 |
| Female | 956 (57.04) | 403 (51.73) | 170 (50.90) | 28 (51.85) | |
| Marriage status (%) | |||||
| In marriage | 1531 (91.35) | 710 (91.14) | 293 (87.72) | 49 (90.74) | 0.212 |
| Other status | 145 (8.65) | 69 (8.86) | 41 (12.28) | 5 (9.26) | |
| Education level (%) | |||||
| Primary school | 817 (48.75) | 330 (42.36) | 165 (49.40) | 39 (72.22) | <0.001 |
| Middle school | 573 (34.19) | 283 (36.33) | 130 (38.92) | 12 (22.22) | |
| High school and above | 286 (17.06) | 166 (21.31) | 39 (11.68) | 3 (5.56) | |
| Geographic region (%) | |||||
| Urban | 349 (20.82) | 282 (36.20) | 122 (36.53) | 0 (0.00) | <0.001 |
| Rural | 1327 (79.18) | 497 (63.80) | 212 (63.47) | 54 (100.00) | |
| Physical activity (%) | |||||
| Low | 1480 (88.31) | 725 (93.07) | 291 (87.13) | 47 (88.89) | 0.004 |
| Medium | 127 (7.58) | 39 (5.01) | 34 (10.18) | 4 (7.41) | |
| High | 69 (4.12) | 15 (1.93) | 9 (2.69) | 2 (3.70) | |
| Sleep duration (%) | |||||
| 6~9 h | 1467 (87.53) | 676 (86.78) | 300 (89.82) | 49 (90.74) | 0.341 |
| <6 h | 40 (2.39) | 18 (2.31) | 6 (1.80) | 3 (5.56) | |
| >9 h | 169 (10.08) | 85 (10.91) | 28 (8.38) | 2 (3.70) | |
| Smoking (%) | |||||
| Nonsmoker | 1240 (73.99) | 554 (71.12) | 231 (69.16) | 38 (70.37) | 0.273 |
| Current smoker | 436 (26.01) | 225 (28.88) | 103 (30.84) | 16 (29.63) | |
| Alcohol drinking (%) | |||||
| Nondrinker | 1151 (68.68) | 511 (65.60) | 206 (61.68) | 41 (75.93) | 0.029 |
| Current drinker | 525 (31.32) | 268 (34.40) | 128 (38.32) | 13 (24.07) | |
| Chronic disease history (%) | |||||
| Yes | 1463 (87.29) | 689 (88.45) | 303 (90.72) | 47 (87.04) | 0.343 |
| No | 213 (12.71) | 90 (11.55) | 31 (9.28) | 7 (12.96) | |
| Per capita household income (yuan/year, median [IQR]) | 22,007 (11,065–40,371) | 24,382 (11,579–48,569) | 21,198 (12,690–36,015) | 24,055 (12,991–37,231) | 0.058 |
| Urbanicity score (mean [SD]) | 62.37 (18.08) | 70.09 (18.00) | 59.72 (18.14) | 56.82 (9.73) | <0.001 |
| BMI (mg/kg, mean [SD]) | 23.37 (3.29) | 22.80 (3.34) | 22.06 (3.16) | 22.92 (2.84) | <0.001 |
| WC (cm, mean [SD]) | 80.00 (9.67) | 80.60 (9.58) | 77.89 (9.61) | 78.51 (10.01) | <0.001 |
| SBP (mmHg, mean [SD]) | 125.71 (18.46) | 123.00 (18.35) | 123.98 (18.05) | 131.00 (19.61) | 0.025 |
| DBP (mmHg, mean [SD]) | 81.44 (11.08) | 79.73 (10.39) | 79.91 (10.79) | 75.28 (12.46) | <0.001 |
| CDGI (mean [SD]) | 45.51 (11.70) | 45.30 (10.12) | 45.61 (10.05) | 43.34 (9.19) | 0.529 |
| Total energy (kcal, mean [SD]) | 2362.90 (774.13) | 2413.84 (780.73) | 2278.93 (693.68) | 2441.83 (878.01) | 0.124 |
| Trajectory Groups | n | Cumulative Number of Cases/Person-Year | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|---|---|
| Risk Ratio (95% CI) | Risk Ratio (95% CI) | Risk Ratio (95% CI) | Risk Ratio (95% CI) | |||
| Dyslipidemia | ||||||
| Group 1 | 1676 | 606/18,225 | 1 | 1 | 1 | 1 |
| Group 2 | 779 | 298/8397 | 1.06 (0.93, 1.21) | 1.02 (0.89, 1.16) | 1.03 (0.90, 1.18) | 1.12 (0.98, 1.29) |
| Group 3 | 334 | 152/3702 | 1.25 (1.06, 1.47) ** | 1.32 (1.11, 1.56) ** | 1.31 (1.11, 1.56) ** | 1.48 (1.26, 1.75) *** |
| Group 4 | 54 | 17/555 | 0.90 (0.55, 1.47) | 0.93 (0.56, 1.54) | 0.90 (0.54, 1.49) | 0.99 (0.60, 1.63) |
| Hypercholesterolemia | ||||||
| Group 1 | 1676 | 158/18,225 | 1 | 1 | 1 | 1 |
| Group 2 | 779 | 72/8397 | 0.99 (0.73, 1.33) | 1.04 (0.76, 1.41) | 1.07 (0.78, 1.45) | 1.13 (0.83, 1.54) |
| Group 3 | 334 | 51/3702 | 1.62 (1.15, 2.27) ** | 1.86 (1.30, 2.65) ** | 1.87 (1.31, 2.66) ** | 1.96 (1.37, 2.81) *** |
| Group 4 | 54 | 4/555 | 0.83 (0.31, 2.18) | 0.82 (0.30, 2.18) | 0.83 (0.31, 2.20) | 0.87 (0.33, 2.31) |
| Hypertriglyceridemia | ||||||
| Group 1 | 1676 | 239/18,225 | 1 | 1 | 1 | 1 |
| Group 2 | 779 | 124/8397 | 1.12 (0.89, 1.40) | 1.06 (0.84, 1.34) | 1.09 (0.86, 1.37) | 1.25 (0.99, 1.59) |
| Group 3 | 334 | 49/3702 | 1.02 (0.75, 1.39) | 1.03 (0.75, 1.40) | 1.02 (0.74, 1.39) | 1.23 (0.90, 1.68) |
| Group 4 | 54 | 10/555 | 1.36 (0.71, 2.58) | 1.48 (0.77, 2.86) | 1.44 (0.75, 2.77) | 1.72 (0.91, 3.26) |
| Low HDL-C | ||||||
| Group 1 | 1676 | 254/18,225 | 1 | 1 | 1 | 1 |
| Group 2 | 779 | 136/8397 | 1.15 (0.93, 1.43) | 1.03 (0.84, 1.28) | 1.04 (0.84, 1.28) | 1.14 (0.92, 1.41) |
| Group 3 | 334 | 45/3702 | 0.88 (0.64, 1.21) | 0.89 (0.66, 1.22) | 0.88 (0.64, 1.20) | 1.02 (0.74, 1.38) |
| Group 4 | 54 | 6/555 | 0.76 (0.35, 1.67) | 0.80 (0.36, 1.79) | 0.74 (0.33, 1.66) | 0.83 (0.38, 1.83) |
| High LDL-C | ||||||
| Group 1 | 1676 | 207/18,225 | 1 | 1 | 1 | 1 |
| Group 2 | 779 | 97/8397 | 1.01 (0.78–1.30) | 0.98 (0.75–1.28) | 1.02 (0.78–1.32) | 1.08 (0.83–1.41) |
| Group 3 | 334 | 80/3702 | 1.92 (1.47–2.51) *** | 2.21 (1.67–2.92) *** | 2.23 (1.68–2.95) *** | 2.41 (1.82–3.20) *** |
| Group 4 | 54 | 5/255 | 0.78 (0.34–1.80) | 0.77 (0.33–1.80) | 0.79 (0.34–1.83) | 0.83 (0.36–1.95) |
| n | Cumulative Number of Cases/Person-Year | Model 1 | Model 2 | Model 3 | Model 4 | ||
|---|---|---|---|---|---|---|---|
| Risk Ratio (95% CI) | Risk Ratio (95% CI) | Risk Ratio (95% CI) | Risk Ratio (95% CI) | ||||
| Breakfast | |||||||
| Q1 | <22.9% | 710 | 276/7761 | 1 | 1 | 1 | 1 |
| Q2 | 22.9–26.9% | 709 | 282/7839 | 1.01 (0.86, 1.18) | 1.04 (0.88, 1.22) | 1.04 (0.89, 1.22) | 1.01 (0.86, 1.19) |
| Q3 | 26.9–31.0% | 713 | 279/7797 | 1.01 (0.86, 1.18) | 1.04 (0.88, 1.23) | 1.03 (0.87, 1.21) | 0.93 (0.79, 1.10) |
| Q4 | ≥31.0% | 711 | 236/7482 | 0.86 (0.73, 1.02) | 0.95 (0.79, 1.14) | 0.91 (0.76, 1.09) | 0.82 (0.68, 0.98) * |
| p trend | 0.06 | 0.405 | 0.214 | 0.010 | |||
| Lunch | |||||||
| Q1 | <33.1% | 708 | 268/7761 | 1 | 1 | 1 | 1 |
| Q2 | 33.1–36.5% | 713 | 287/7839 | 1.07 (0.91, 1.25) | 1.01 (0.85, 1.18) | 1.01 (0.86, 1.19) | 0.99 (0.84, 1.17) |
| Q3 | 36.5–39.7% | 711 | 243/7797 | 0.91 (0.77, 1.07) | 0.84 (0.71, 1.00) | 0.87 (0.73, 1.03) | 0.85 (0.71, 1.01) |
| Q4 | ≥39.7% | 711 | 275/7482 | 1.03 (0.88, 1.20) | 0.97 (0.82, 1.14) | 1.01 (0.86, 1.19) | 1.00 (0.84, 1.18) |
| p trend | 0.841 | 0.38 | 0.743 | 0.598 | |||
| Dinner | |||||||
| Q1 | <33.3% | 710 | 258/7761 | 1 | 1 | 1 | 1 |
| Q2 | 33.3–36.5% | 711 | 238/7839 | 0.92 (0.78, 1.09) | 0.92 (0.77, 1.09) | 0.90 (0.75, 1.07) | 0.91 (0.77, 1.08) |
| Q3 | 36.5–40.5% | 708 | 268/7797 | 1.04 (0.88, 1.22) | 1.00 (0.95, 1.18) | 0.99 (0.83, 1.17) | 1.07 (0.90, 1.27) |
| Q4 | ≥40.5% | 714 | 309/7482 | 1.20 (1.02, 1.40) * | 1.22 (1.04, 1.44) * | 1.19 (1.01, 1.40) * | 1.35 (1.15, 1.59) ** |
| p trend | 0.002 | 0.005 | 0.013 | <0.001 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, X.; Wang, H.; Su, C.; Wang, Z.; Du, W.; Huang, F.; Zhang, J.; Jia, X.; Jiang, H.; Ouyang, Y.; et al. Trajectories of Energy Intake Distribution and Risk of Dyslipidemia: Findings from the China Health and Nutrition Survey (1991–2018). Nutrients 2021, 13, 3488. https://doi.org/10.3390/nu13103488
Song X, Wang H, Su C, Wang Z, Du W, Huang F, Zhang J, Jia X, Jiang H, Ouyang Y, et al. Trajectories of Energy Intake Distribution and Risk of Dyslipidemia: Findings from the China Health and Nutrition Survey (1991–2018). Nutrients. 2021; 13(10):3488. https://doi.org/10.3390/nu13103488
Chicago/Turabian StyleSong, Xiaoyun, Huijun Wang, Chang Su, Zhihong Wang, Wenwen Du, Feifei Huang, Jiguo Zhang, Xiaofang Jia, Hongru Jiang, Yifei Ouyang, and et al. 2021. "Trajectories of Energy Intake Distribution and Risk of Dyslipidemia: Findings from the China Health and Nutrition Survey (1991–2018)" Nutrients 13, no. 10: 3488. https://doi.org/10.3390/nu13103488
APA StyleSong, X., Wang, H., Su, C., Wang, Z., Du, W., Huang, F., Zhang, J., Jia, X., Jiang, H., Ouyang, Y., Li, L., Bai, J., Zhang, X., Ding, G., & Zhang, B. (2021). Trajectories of Energy Intake Distribution and Risk of Dyslipidemia: Findings from the China Health and Nutrition Survey (1991–2018). Nutrients, 13(10), 3488. https://doi.org/10.3390/nu13103488







