Web-Based Personalized Nutrition System for Delivering Dietary Feedback Based on Behavior Change Techniques: Development and Pilot Study among Dietitians
Abstract
:1. Introduction
2. Materials and Methods
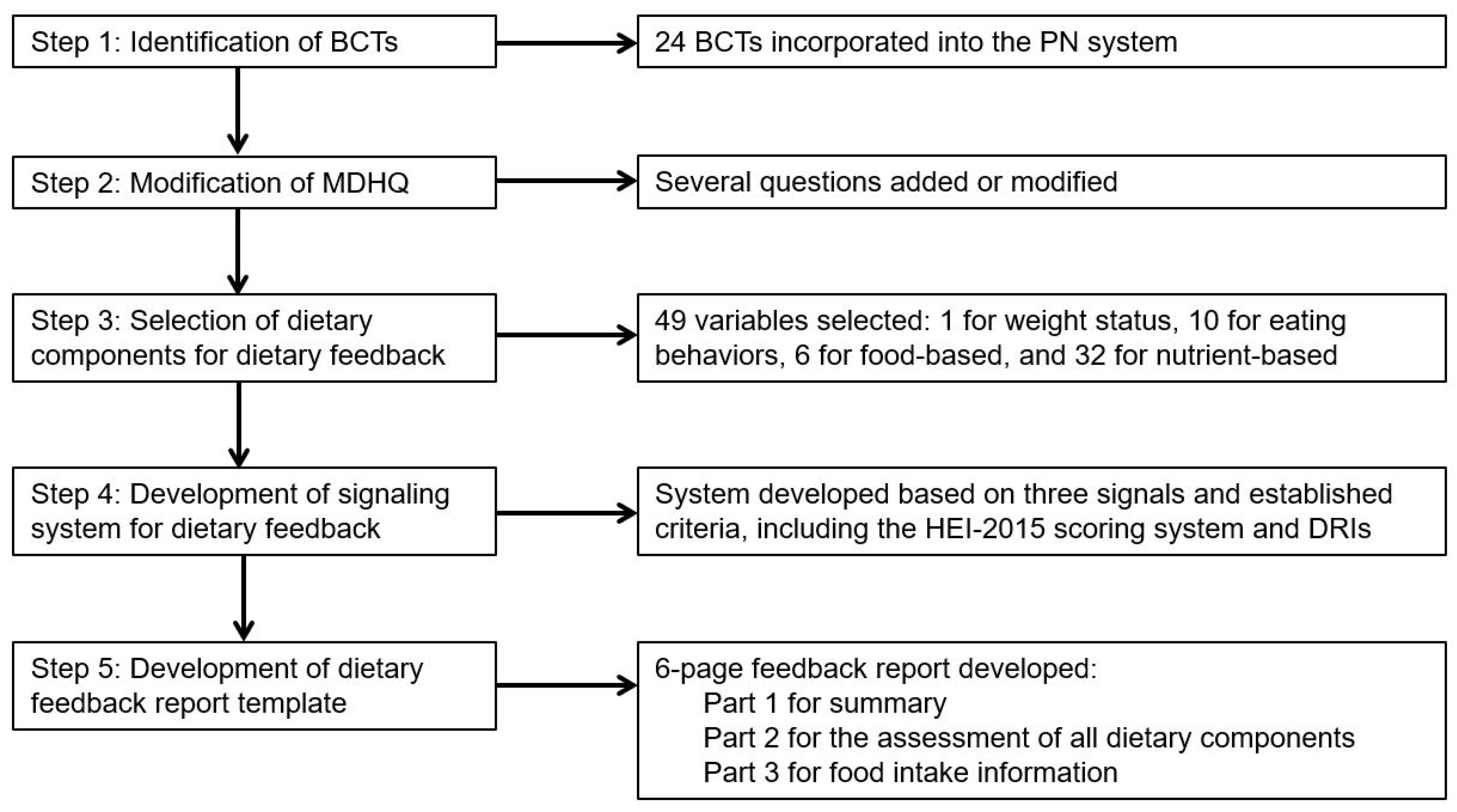
2.1. Development of Web-Based Personalized Nutrition System
2.1.1. Step 1: Identification of Behavior Change Techniques
2.1.2. Step 2: Modification of Dietary Assessment Method
2.1.3. Step 3: Selection of Dietary Components for Dietary Feedback
2.1.4. Step 4: Development of Signaling System for Dietary Feedback
2.1.5. Step 5: Development of Dietary Feedback Report Template
2.2. Pilot Study
2.2.1. Overview and Study Population
2.2.2. Survey Procedure
2.2.3. Assessment of Acceptability of the Dietary Feedback Report
2.2.4. Statistical Analysis
3. Results
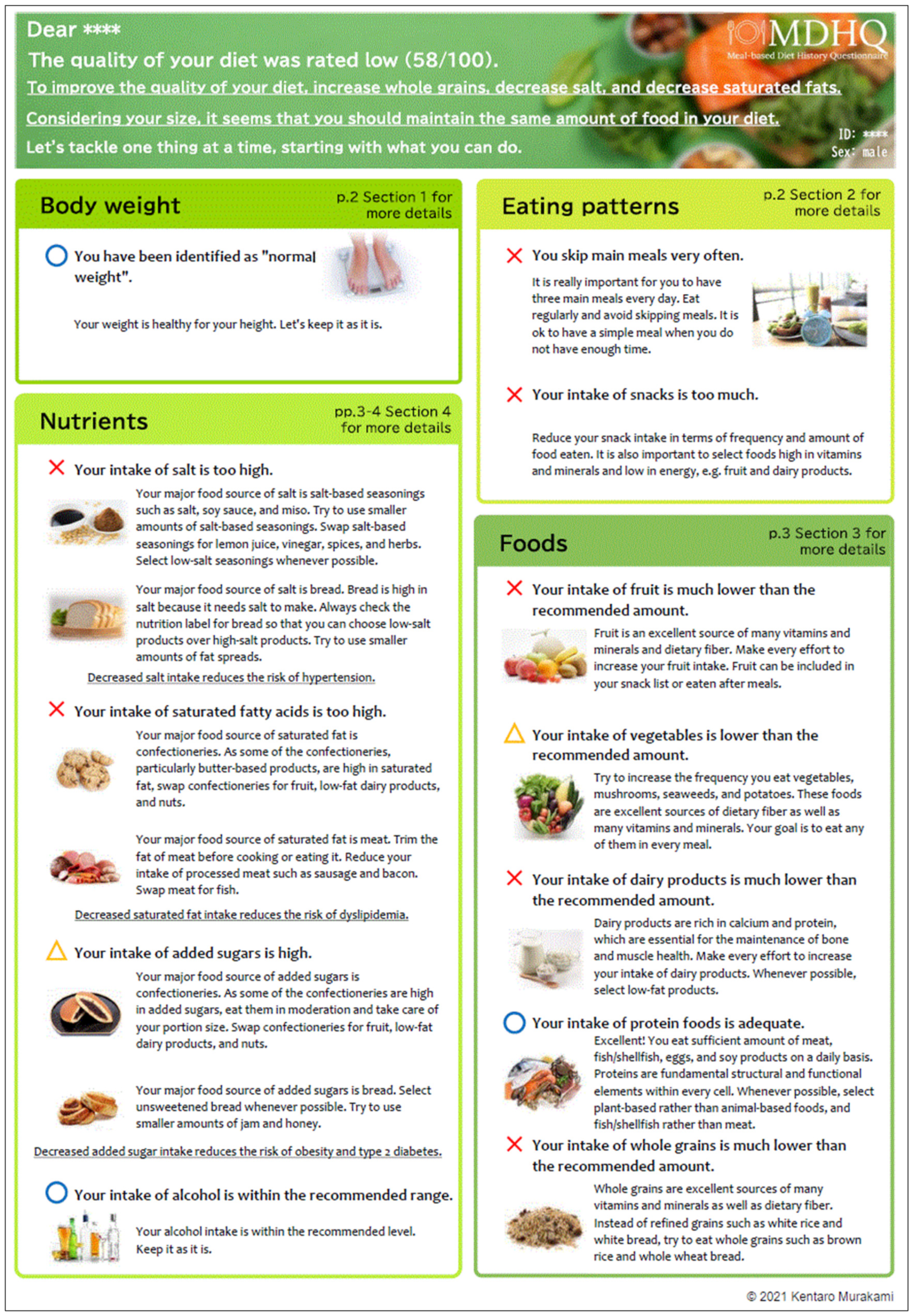
3.1. Dietary Feedback Report
3.1.1. Part 1 of Dietary Feedback Report
- “You have been identified as overweight.” (main assessment message)
- “You will become healthier if you succeed in a slight decrease in your body weight. Gradually decrease the amount of food you eat and become more physically active.” (more specific sub messages)
- “You skip main meals very often.” (main assessment message)
- “It is really important for you to have three main meals every day. Eat regularly and avoid skipping meals. It is ok to have a simple meal when you do not have enough time.” (more specific sub messages)
3.1.2. Part 2 of Dietary Feedback Report
3.1.3. Part 3 of Dietary Feedback Report
3.2. Pilot Study
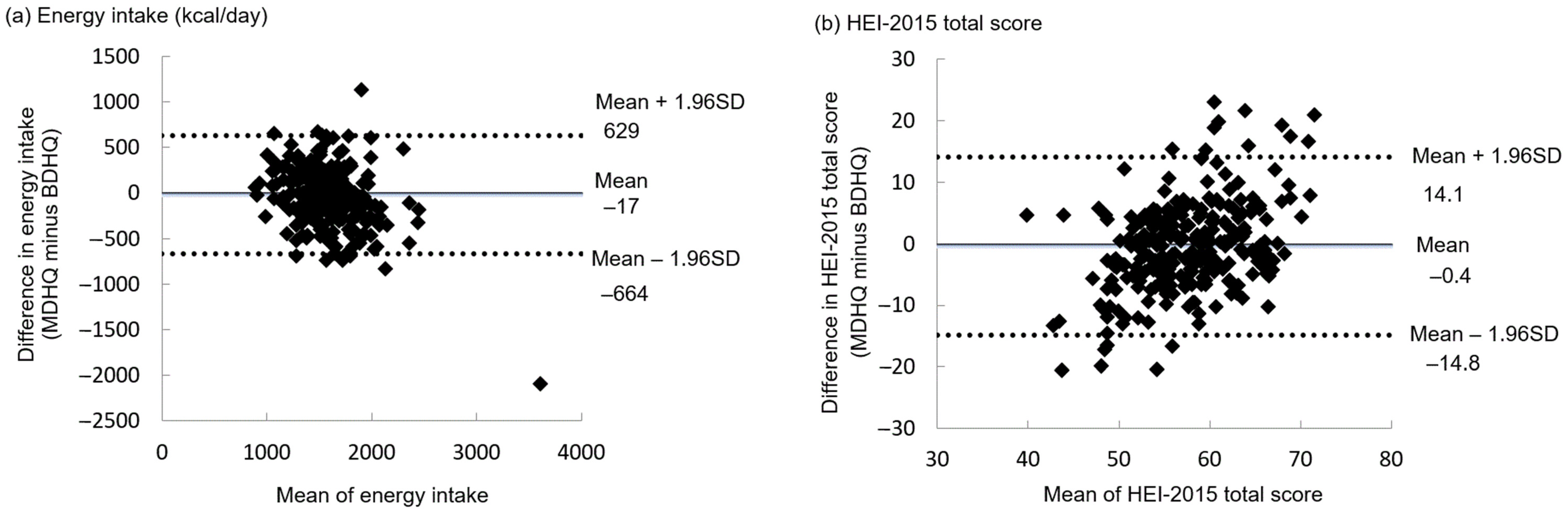
3.2.1. Comparability of the MDHQ with the BDHQ
3.2.2. Acceptability of the Dietary Feedback Report
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Willett, W.; Rockstrom, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- Jinnette, R.; Narita, A.; Manning, B.; McNaughton, S.A.; Mathers, J.C.; Livingstone, K.M. Does personalized nutrition advice improve dietary intake in healthy adults? A systematic review of randomized controlled trials. Adv. Nutr. 2021, 12, 657–669. [Google Scholar] [CrossRef] [PubMed]
- Ordovas, J.M.; Ferguson, L.R.; Tai, E.S.; Mathers, J.C. Personalised nutrition and health. BMJ 2018, 361, k2173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murakami, K.; Shinozaki, N.; McCaffrey, T.A.; Livingstone, M.B.E.; Sasaki, S. Data-driven development of the Meal-based Diet History Questionnaire for Japanese adults. Br. J. Nutr. 2021, 126, 1056–1064. [Google Scholar] [CrossRef] [PubMed]
- Forster, H.; Walsh, M.C.; O’Donovan, C.B.; Woolhead, C.; McGirr, C.; Daly, E.J.; O’Riordan, R.; Celis-Morales, C.; Fallaize, R.; Macready, A.L.; et al. A dietary feedback system for the delivery of consistent personalized dietary advice in the Web-based multicenter Food4Me study. J. Med. Internet Res. 2016, 18, e150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wright, J.L.; Sherriff, J.L.; Dhaliwal, S.S.; Mamo, J.C. Tailored, iterative, printed dietary feedback is as effective as group education in improving dietary behaviours: Results from a randomised control trial in middle-aged adults with cardiovascular risk factors. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 43. [Google Scholar] [CrossRef] [Green Version]
- Forster, H.; Walsh, M.C.; Gibney, M.J.; Brennan, L.; Gibney, E.R. Personalised nutrition: The role of new dietary assessment methods. Proc. Nutr. Soc. 2016, 75, 96–105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef] [Green Version]
- Reedy, J.; Lerman, J.L.; Krebs-Smith, S.M.; Kirkpatrick, S.I.; Pannucci, T.E.; Wilson, M.M.; Subar, A.F.; Kahle, L.L.; Tooze, J.A. Evaluation of the Healthy Eating Index-2015. J. Acad. Nutr. Diet. 2018, 118, 1622–1633. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare, Japan. Dietary Reference Intakes for Japanese. 2020. Available online: https://www.mhlw.go.jp/stf/newpage_08517.html (accessed on 18 August 2021). (In Japanese).
- Macready, A.L.; Fallaize, R.; Butler, L.T.; Ellis, J.A.; Kuznesof, S.; Frewer, L.J.; Celis-Morales, C.; Livingstone, K.M.; Araujo-Soares, V.; Fischer, A.R.; et al. Application of behavior change techniques in a personalized nutrition electronic health intervention study: Protocol for the web-based Food4Me randomized controlled trial. JMIR Res. Protoc. 2018, 7, e87. [Google Scholar] [CrossRef] [Green Version]
- Celis-Morales, C.; Livingstone, K.M.; Marsaux, C.F.; Macready, A.L.; Fallaize, R.; O’Donovan, C.B.; Woolhead, C.; Forster, H.; Walsh, M.C.; Navas-Carretero, S.; et al. Effect of personalized nutrition on health-related behaviour change: Evidence from the Food4Me European randomized controlled trial. Int. J. Epidemiol. 2017, 46, 578–588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Celis-Morales, C.; Livingstone, K.M.; Petermann-Rocha, F.; Navas-Carretero, S.; San-Cristobal, R.; O’Donovan, C.B.; Moschonis, G.; Manios, Y.; Traczyk, I.; Drevon, C.A.; et al. Frequent nutritional feedback, personalized advice, and behavioral changes: Findings from the European Food4Me Internet-Based RCT. Am. J. Prev. Med. 2019, 57, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, K.M.; Celis-Morales, C.; Navas-Carretero, S.; San-Cristobal, R.; Macready, A.L.; Fallaize, R.; Forster, H.; Woolhead, C.; O’Donovan, C.B.; Marsaux, C.F.; et al. Effect of an Internet-based, personalized nutrition randomized trial on dietary changes associated with the Mediterranean diet: The Food4Me Study. Am. J. Clin. Nutr. 2016, 104, 288–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Celis-Morales, C.; Livingstone, K.M.; Marsaux, C.F.; Forster, H.; O’Donovan, C.B.; Woolhead, C.; Macready, A.L.; Fallaize, R.; Navas-Carretero, S.; San-Cristobal, R.; et al. Design and baseline characteristics of the Food4Me study: A web-based randomised controlled trial of personalised nutrition in seven European countries. Genes Nutr. 2015, 10, 450. [Google Scholar] [CrossRef] [PubMed]
- Fallaize, R.; Forster, H.; Macready, A.L.; Walsh, M.C.; Mathers, J.C.; Brennan, L.; Gibney, E.R.; Gibney, M.J.; Lovegrove, J.A. Online dietary intake estimation: Reproducibility and validity of the Food4Me food frequency questionnaire against a 4-day weighed food record. J. Med. Internet. Res. 2014, 16, e190. [Google Scholar] [CrossRef]
- Michie, S.; Ashford, S.; Sniehotta, F.F.; Dombrowski, S.U.; Bishop, A.; French, D.P. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: The CALO-RE taxonomy. Psychol. Health 2011, 26, 1479–1498. [Google Scholar] [CrossRef]
- Michie, S.; Hyder, N.; Walia, A.; West, R. Development of a taxonomy of behaviour change techniques used in individual behavioural support for smoking cessation. Addict. Behav. 2011, 36, 315–319. [Google Scholar] [CrossRef]
- Abraham, C.; Michie, S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008, 27, 379–387. [Google Scholar] [CrossRef] [Green Version]
- Carver, C.S.; Scheier, M.F. Control theory: A useful conceptual framework for personality-social, clinical, and health psychology. Psychol. Bull. 1982, 92, 111–135. [Google Scholar] [CrossRef]
- Fisher, J.D.; Fisher, W.A.; Bryan, A.D.; Misovich, S.J. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychol. 2002, 21, 177–186. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behaviour. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Bandura, A. Health promotion from the perspective of social cognitive theory. Psychol. Health 1998, 13, 623–649. [Google Scholar] [CrossRef]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Murakami, K.; Shinozaki, N.; Livingstone, M.B.E.; Fujiwara, A.; Asakura, K.; Masayasu, S.; Sasaki, S. Meal and snack frequency in relation to diet quality in Japanese adults: A cross-sectional study using different definitions of meals and snacks. Br. J. Nutr. 2020, 124, 1219–1228. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.B. Review of whole grain and dietary fiber recommendations and intake levels in different countries. Nutr. Rev. 2020, 78 (Suppl. 1), 29–36. [Google Scholar] [CrossRef] [PubMed]
- Murakami, K.; Livingstone, M.B.E.; Fujiwara, A.; Sasaki, S. Application of the Healthy Eating Index-2015 and the Nutrient-Rich Food Index 9.3 for assessing overall diet quality in the Japanese context: Different nutritional concerns from the US. PLoS ONE 2020, 15, e0228318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murakami, K.; Shinozaki, N.; Livingstone, M.B.E.; Fujiwara, A.; Asakura, K.; Masayasu, S.; Sasaki, S. Characterisation of breakfast, lunch, dinner and snacks in the Japanese context: An exploratory cross-sectional analysis. Public Health Nutr. 2020, 10, 1–13, Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Panizza, C.E.; Shvetsov, Y.B.; Harmon, B.E.; Wilkens, L.R.; Le Marchand, L.; Haiman, C.; Reedy, J.; Boushey, C.J. Testing the predictive validity of the Healthy Eating Index-2015 in the Multiethnic Cohort: Is the score associated with a reduced risk of all-cause and cause-specific mortality? Nutrients 2018, 10, 452. [Google Scholar] [CrossRef] [Green Version]
- Hu, E.A.; Steffen, L.M.; Coresh, J.; Appel, L.J.; Rebholz, C.M. Adherence to the Healthy Eating Index-2015 and other dietary patterns may reduce risk of cardiovascular disease, cardiovascular mortality, and all-cause mortality. J. Nutr. 2020, 150, 312–321. [Google Scholar] [CrossRef]
- Morze, J.; Danielewicz, A.; Hoffmann, G.; Schwingshackl, L. Diet quality as assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and health outcomes: A second update of a systematic review and meta-analysis of cohort studies. J. Acad. Nutr. Diet. 2020, 120, 1998–2031. [Google Scholar] [CrossRef]
- Report of the Subdivision on Resources, The Council for Science and Technology, Ministry of Education, Culture, Sports, Science and Technology, Japan. Standard Tables of Food Composition in Japan-2020-(Eighth Revised Edition). 2020. Available online: https://www.mext.go.jp/a_menu/syokuhinseibun/mext_01110.html (accessed on 18 August 2021). (In Japanese).
- Murakami, K.; Livingstone, M.B.E.; Fujiwara, A.; Sasaki, S. Reproducibility and relative validity of the Healthy Eating Index-2015 and Nutrient-Rich Food Index 9.3 estimated by comprehensive and brief diet history questionnaires in Japanese adults. Nutrients 2019, 11, 2540. [Google Scholar] [CrossRef] [Green Version]
- Bowman, S.A.; Clemens, J.C.; Friday, J.E.; Thoerig, R.C.; Moshfegh, A. Food Patterns Equivalents Database 2011-12: Methodology and User Guide. Food Surveys Research Group. Beltsville Human Nutrition Research Center, Agricultural Research Service, U.S. Department of Agriculture, Beltsville, MD. 2014. Available online: http://www.ars.usda.gov/nea/bhnrc/fsrg (accessed on 18 August 2021).
- Murakami, K.; Sasaki, S.; Uenishi, K. The degree of misreporting of the energy-adjusted intake of protein, potassium, and sodium does not differ among under-, acceptable, and over-reporters of energy intake. Nutr. Res. 2012, 32, 741–750. [Google Scholar] [CrossRef]
- World Health Organization. Nutrition Landscape Information System (NLiS) country profile indicators: Interpretation guide, 2nd ed. World Health Organization. 2019. Available online: https://apps.who.int/iris/handle/10665/332223 (accessed on 18 August 2021).
- Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. 2011. Available online: https://www.nap.edu/resource/13050/Vitamin-D-and-Calcium-2010-Report-Brief.pdf (accessed on 17 August 2021).
- World Health Organization. Guideline: Sugars Intake for Adults and Children. Geneva, Switzerland: World Health Organization. 2015. Available online: http://apps.who.int/iris/bitstream/10665/149782/1/9789241549028_eng.pdf?ua=1 (accessed on 18 August 2021).
- Wood, A.M.; Kaptoge, S.; Butterworth, A.S.; Willeit, P.; Warnakula, S.; Bolton, T.; Paige, E.; Paul, D.S.; Sweeting, M.; Burgess, S.; et al. Risk thresholds for alcohol consumption: Combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet 2018, 391, 1513–1523. [Google Scholar] [CrossRef] [Green Version]
- Public Health Agency. Enjoy Healthy Eating. 2012. Available online: https://www.nidirect.gov.uk/information-and-services/healthy-lives/healthy-eating (accessed on 17 August 2021).
- British Dietetic Association. Food Fact Sheets. 2013. Available online: https://www.bda.uk.com/food-health/food-facts.html (accessed on 17 August 2021).
- Food Saftey Authority Ireland. Healthy Eating Guidelines. 2011. Available online: https://www.fsai.ie/science_and_health/healthy_eating.html (accessed on 17 August 2021).
- Office of Disease Prevention and Health Promotion. Cut Down on Saturated Fats. 2016. Available online: https://health.gov/sites/default/files/2019-10/DGA_Cut-Down-On-Saturated-Fats.pdf (accessed on 17 August 2021).
- National Health Service. How to Eat Less Saturated Fat. 2020. Available online: https://www.nhs.uk/live-well/eat-well/eat-less-saturated-fat/ (accessed on 17 August 2021).
- Office of Disease Prevention and Health Promotion. Cut Down on Added Sugars. 2016. Available online: https://health.gov/sites/default/files/2019-10/DGA_Cut-Down-On-Added-Sugars.pdf (accessed on 17 August 2021).
- Makino, N. Food and Cooking Data for Salt; Kagawa Nutrition University Press: Tokyo, Japan, 2013. (In Japanese) [Google Scholar]
- World Cancer Research Fund. Easy Ways to Eat Less Fat, Sugar and Salt. Available online: https://www.wcrf-uk.org/uk/recipes/easy-ways-cut-sugar-fat-salt (accessed on 17 August 2021).
- Ministry of Health, Labour and Welfare, Japan. E-health Net. Available online: https://www.e-healthnet.mhlw.go.jp/ (accessed on 17 August 2021). (In Japanese).
- Kobayashi, S.; Murakami, K.; Sasaki, S.; Okubo, H.; Hirota, N.; Notsu, A.; Fukui, M.; Date, C. Comparison of relative validity for food group intake estimated by comprehensive and brief-type self-administered diet history questionnaires against 16 d dietary records in Japanese adults. Public Health Nutr. 2011, 14, 1200–1211. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, S.; Honda, S.; Murakami, K.; Sasaki, S.; Okubo, H.; Hirota, N.; Notsu, A.; Fukui, M.; Date, C. Both comprehensive and brief self-administered diet history questionnaires satisfactorily rank nutrient intakes in Japanese adults. J. Epidemiol. 2012, 22, 151–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murakami, K.; Mizoue, T.; Sasaki, S.; Ohta, M.; Sato, M.; Matsushita, Y.; Mishima, N. Dietary intake of folate, other B vitamins, and ω-3 polyunsaturated fatty acids in relation to depressive symptoms in Japanese adults. Nutrition 2008, 24, 140–147. [Google Scholar] [CrossRef]
- Kobayashi, S.; Asakura, K.; Suga, H.; Sasaki, S. High protein intake is associated with low prevalence of frailty among old Japanese women: A multicenter cross-sectional study. Nutr. J. 2013, 12, 164. [Google Scholar] [CrossRef] [Green Version]
- Inomaki, R.; Murakami, K.; Livingstone, M.B.; Okubo, H.; Kobayashi, S.; Suga, H.; Sasaki, S. A Japanese diet with low glycaemic index and glycaemic load is associated with both favourable and unfavourable aspects of dietary intake patterns in three generations of women. Public Health Nutr. 2017, 20, 649–659. [Google Scholar] [CrossRef] [Green Version]
- Maes, L.; Cook, T.L.; Ottovaere, C.; Matthijs, C.; Moreno, L.A.; Kersting, M.; Papadaki, A.; Manios, Y.; Dietrich, S.; Hallstrom, L.; et al. Pilot evaluation of the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) Food-O-Meter, a computer-tailored nutrition advice for adolescents: A study in six European cities. Public Health Nutr. 2011, 14, 1292–1302. [Google Scholar] [CrossRef]
- Vereecken, C.; Covents, M.; Maes, L.; Moyson, T. Formative evaluation of the feedback component of Children’s and Adolescents’ Nutrition Assessment and Advice on the Web (CANAA-W) among parents of schoolchildren. Public Health Nutr. 2013, 16, 15–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- Murakami, K.; Livingstone, M.B.E.; Shinozaki, N.; Sugimoto, M.; Fujiwara, A.; Masayasu, S.; Sasaki, S. Food combinations in relation to the quality of overall diet and individual meals in Japanese adults: A nationwide study. Nutrients 2020, 12, 327. [Google Scholar] [CrossRef] [Green Version]
- Cleghorn, C.L.; Harrison, R.A.; Ransley, J.K.; Wilkinson, S.; Thomas, J.; Cade, J.E. Can a dietary quality score derived from a short-form FFQ assess dietary quality in UK adult population surveys? Public Health Nutr. 2016, 19, 2915–2923. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schroder, H.; Fito, M.; Estruch, R.; Martinez-Gonzalez, M.A.; Corella, D.; Salas-Salvado, J.; Lamuela-Raventos, R.; Ros, E.; Salaverria, I.; Fiol, M.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef] [Green Version]
- van Lee, L.; Feskens, E.J.; Meijboom, S.; Hooft van Huysduynen, E.J.; van’t Veer, P.; de Vries, J.H.; Geelen, A. Evaluation of a screener to assess diet quality in the Netherlands. Br. J. Nutr. 2016, 115, 517–526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whitton, C.; Ho, J.C.Y.; Rebello, S.A.; van Dam, R.M. Relative validity and reproducibility of dietary quality scores from a short diet screener in a multi-ethnic Asian population. Public Health Nutr. 2018, 21, 2735–2743. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, M.B.; Robson, P.J.; Wallace, J.M. Issues in dietary intake assessment of children and adolescents. Br. J. Nutr. 2004, 92, S213–S222. [Google Scholar] [CrossRef] [PubMed]
- Murakami, K.; Livingstone, M.B.E.; Sasaki, S. Establishment of a meal coding system for the characterization of meal-based dietary patterns in Japan. J. Nutr. 2017, 147, 2093–2101. [Google Scholar] [CrossRef] [Green Version]
- Murakami, K.; Livingstone, M.B.E.; Sasaki, S. Meal-specific dietary patterns and their contribution to overall dietary patterns in the Japanese context: Findings from the 2012 National Health and Nutrition Survey, Japan. Nutrition 2019, 59, 108–115. [Google Scholar] [CrossRef]
- Murakami, K.; Livingstone, M.B.E.; Sasaki, S.; Hirota, N.; Notsu, A.; Miura, A.; Todoriki, H.; Fukui, M.; Date, C. Applying a meal coding system to 16-day weighed dietary record data in the Japanese context: Toward the development of simple meal-based dietary assessment tools. J. Nutr. Sci. 2018, 7, e29. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health, Labour and Welfare, Japan. Secular Trends in the Number of New Dietitians. Available online: https://www.mhlw.go.jp/content/000785418.pdf (accessed on 19 September 2021). (In Japanese).
| Variable | Value |
|---|---|
| Sex, n (%) | |
| Male | 6 (2.4) |
| Female | 249 (97.7) |
| Age (years) | 48.6 ± 10.8 |
| Body height (cm) 2 | 158.6 ± 5.8 |
| Body weight (kg) 2 | 55.5 ± 8.5 |
| BMI (kg/m2) 3 | 22.1 ± 3.2 |
| Weight status, n (%) | |
| Underweight (BMI < 18.5 kg/m2) | 27 (10.6) |
| Normal weight (BMI ≥ 18.5 to <25 kg/m2) | 183 (71.8) |
| Overweight (BMI ≥25 kg/m2) | 45 (17.7) |
| Dietary reporting status in the MDHQ, n (%) | |
| Implausible 4 | 65 (25.5) |
| Plausible 5 | 190 (74.5) |
| Whether the MDHQ feedback report was printed, n (%) | |
| No | 133 (52.2) |
| Yes | 122 (47.8) |
| Time spent reading the MDHQ feedback report, n (%) | |
| Less than 20 min | 162 (63.5) |
| 20 min or more | 93 (36.5) |
| Variable | Maximum Score | MDHQ | BDHQ | Pearson Correlation 2 | Mean Difference 3 | Limit of Agreement 4 |
|---|---|---|---|---|---|---|
| Energy intake (kcal/day) | --- | 1581 ± 283 | 1598 ± 392 | 0.56 **** | −17 | 629, −664 |
| HEI-2015 total score | 100 | 57.2 ± 8.1 | 57.5 ± 5.5 | 0.46 **** | −0.4 | 14.1, −14.8 |
| HEI-2015 component score | --- | --- | --- | --- | --- | --- |
| Total fruits | 5 | 2.2 ± 1.3 | 2.2 ± 1.3 | 0.65 **** | 0.0 | 2.1, −2.1 |
| Whole fruits | 5 | 3.4 ± 1.6 | 3.3 ± 1.6 | 0.71 **** | 0.1 | 2.5, −2.3 |
| Total vegetables | 5 | 4.8 ± 0.7 | 4.9 ± 0.4 | 0.31 **** | −0.1 | 1.3, −1.5 |
| Greens and beans | 5 | 3.7 ± 1.5 | 4.3 ± 1.2 *** | 0.39 **** | −0.7 | 2.3, −3.6 |
| Whole grains | 10 | 2.8 ± 2.6 | 0.4 ± 0.5 *** | −0.04 | 2.4 | 7.5, −2.8 |
| Dairy | 10 | 2.6 ± 1.5 | 2.5 ± 1.6 | 0.62 **** | 0.1 | 2.7, −2.5 |
| Total protein foods | 5 | 4.5 ± 0.6 | 5.0 ± 0.2 *** | 0.21 *** | −0.5 | 0.7, −1.6 |
| Seafood and plant proteins | 5 | 4.9 ± 0.5 | 5.0 ± 0.2 ** | 0.46 **** | −0.1 | 0.7, −0.9 |
| Fatty acids | 10 | 6.9 ± 2.4 | 8.3 ± 1.9 *** | 0.32 **** | −1.4 | 3.6, −6.4 |
| Refined grains | 10 | 1.6 ± 2.3 | 1.5 ± 2.1 | 0.32 **** | 0.1 | 5.2, −4.9 |
| Sodium | 10 | 1.5 ± 2.2 | 1.0 ± 1.8 ** | 0.43 **** | 0.5 | 4.8, −3.8 |
| Added sugars | 10 | 9.3 ± 1.1 | 9.8 ± 0.6 *** | 0.38 **** | −0.5 | 1.5, −2.5 |
| Saturated fats | 10 | 8.9 ± 1.4 | 9.4 ± 1.0 *** | 0.23 *** | −0.5 | 2.5, −3.5 |
| Variable | Value |
|---|---|
| Total score | 4.2 ± 0.4 |
| The report is believable | 4.1 ± 0.6 |
| The report is relevant | 4.3 ± 0.6 |
| The report is interesting | 4.6 ± 0.6 |
| The report is logical | 4.3 ± 0.7 |
| The report is understandable | 4.3 ± 0.7 |
| The report is well formulated | 4.4 ± 0.7 |
| The report is complete | 4.5 ± 0.6 |
| The report is too long | 3.3 ± 1.1 |
| The report is personal | 4.4 ± 0.7 |
| The report is correct | 3.9 ± 0.7 |
| I will use the report | 4.3 ± 0.7 |
| The report will help me to eat healthier | 4.5 ± 0.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murakami, K.; Shinozaki, N.; Masayasu, S.; Livingstone, M.B.E. Web-Based Personalized Nutrition System for Delivering Dietary Feedback Based on Behavior Change Techniques: Development and Pilot Study among Dietitians. Nutrients 2021, 13, 3391. https://doi.org/10.3390/nu13103391
Murakami K, Shinozaki N, Masayasu S, Livingstone MBE. Web-Based Personalized Nutrition System for Delivering Dietary Feedback Based on Behavior Change Techniques: Development and Pilot Study among Dietitians. Nutrients. 2021; 13(10):3391. https://doi.org/10.3390/nu13103391
Chicago/Turabian StyleMurakami, Kentaro, Nana Shinozaki, Shizuko Masayasu, and M. Barbara E. Livingstone. 2021. "Web-Based Personalized Nutrition System for Delivering Dietary Feedback Based on Behavior Change Techniques: Development and Pilot Study among Dietitians" Nutrients 13, no. 10: 3391. https://doi.org/10.3390/nu13103391
APA StyleMurakami, K., Shinozaki, N., Masayasu, S., & Livingstone, M. B. E. (2021). Web-Based Personalized Nutrition System for Delivering Dietary Feedback Based on Behavior Change Techniques: Development and Pilot Study among Dietitians. Nutrients, 13(10), 3391. https://doi.org/10.3390/nu13103391







