Plant-Based Dietary Patterns and Breast Cancer Recurrence and Survival in the Pathways Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Plant-Based Diet Indices
2.3. Ascertainment of Breast Cancer Recurrence and Survival
2.4. Covariate Selection
2.5. Statistical Analysis
3. Results
3.1. Study Population
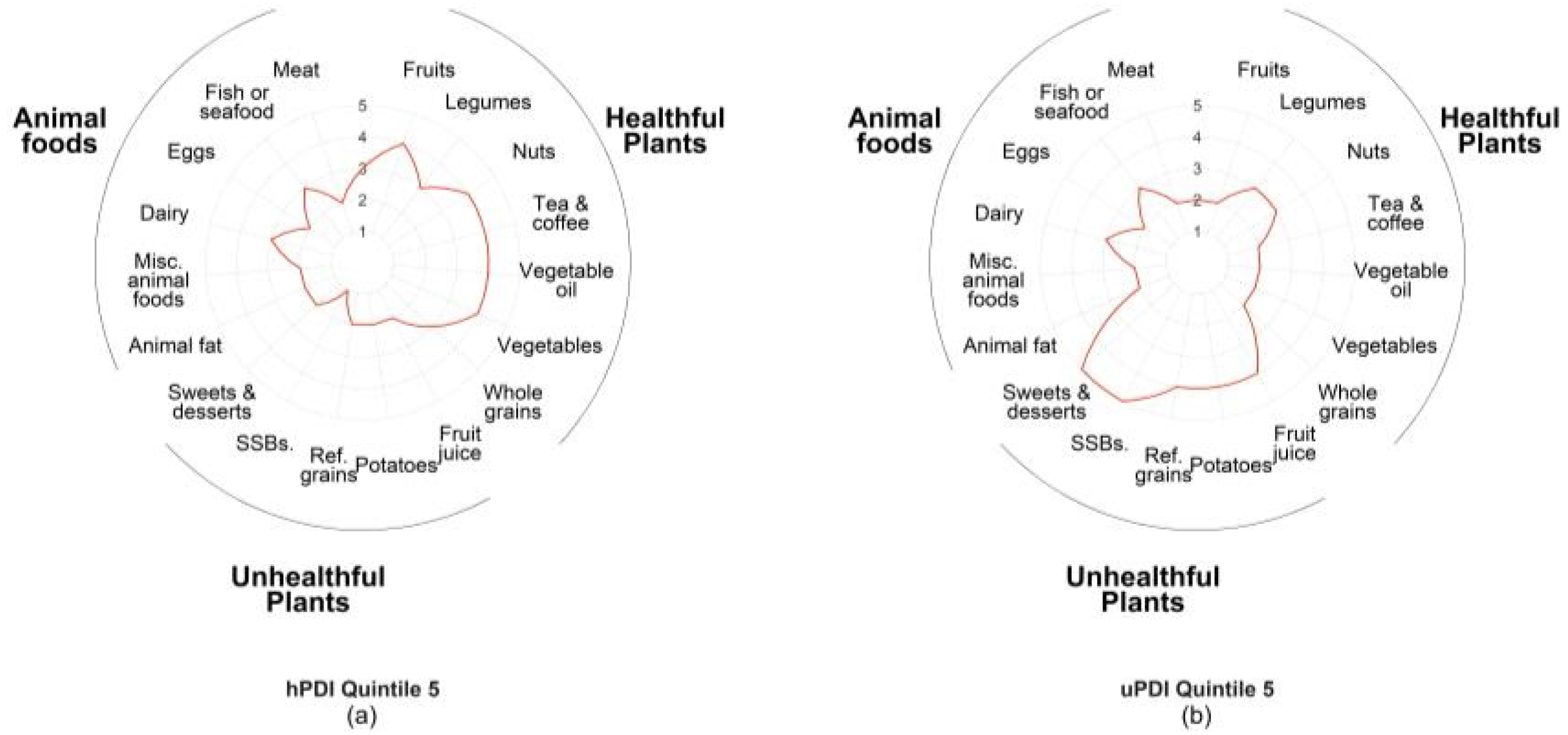
3.2. Food Consumption Patterns
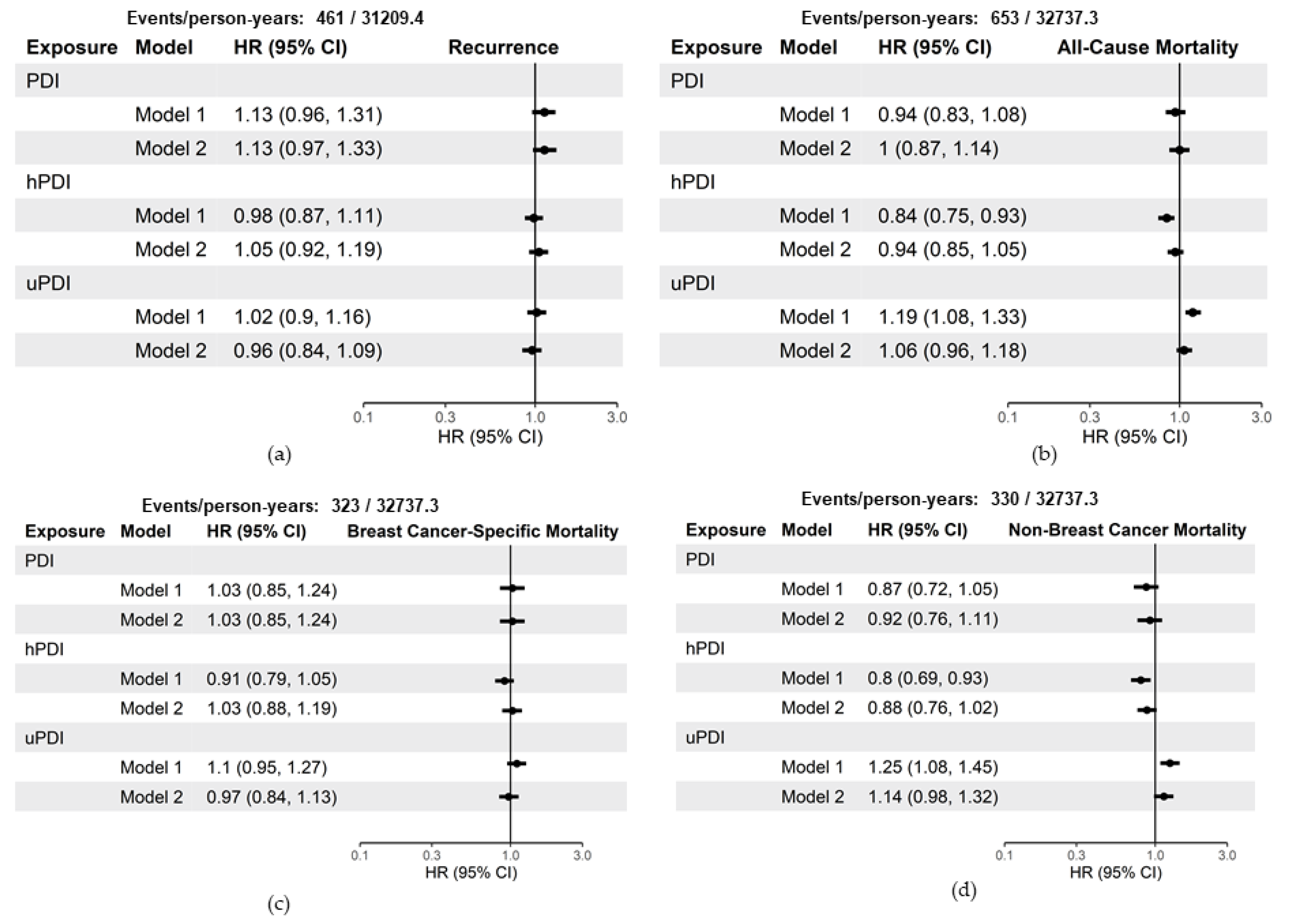
3.3. Plant-Based Indices and Breast Cancer Recurrence and Survival
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Miller, K.D.; Nogueira, L.; Mariotto, A.B.; Rowland, J.H.; Yabroff, K.R.; Alfano, C.M.; Jemal, A.; Kramer, J.L.; Siegel, R.L. Cancer treatment and survivorship statistics. CA A Cancer J. Clin. 2019, 69, 363–385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Cancer Research Fund International/American Institute for Cancer Research. Diet, Nutrition, Physical Activity, and Breast Cancer Survivors; World Cancer Research Fund International/American Institute for Cancer Research: London, UK, 2014. [Google Scholar]
- Kushi, L.H.; Doyle, C.; McCullough, M.; Rock, C.L.; Demark-Wahnefried, W.; Bandera, E.V.; Gapstur, S.; Patel, A.V.; Andrews, K.; Gansler, T. American Cancer Society guidelines on nutrition and physical activity for cancer prevention. CA A Cancer J. Clin. 2012, 62, 30–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cespedes, E.M.; Hu, F.B. Dietary patterns: From nutritional epidemiologic analysis to national guidelines. Am. J. Clin. Nutr. 2015, 101, 899–900. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martínez-González, M.A.; Sánchez-Tainta, A.; Corella, D.; Salas-Salvadó, J.; Ros, E.; Arós, F.; Gómez-Gracia, E.; Fiol, M.; Lamuela-Raventós, R.M.; Schröder, H.; et al. A provegetarian food pattern and reduction in total mortality in the Prevención con Dieta Mediterránea (PREDIMED) study. Am. J. Clin. Nutr. 2014, 100, 320S–328S. [Google Scholar] [CrossRef] [Green Version]
- Satija, A.; Bhupathiraju, S.N.; Rimm, E.B.; Spiegelman, D.; Chiuve, S.E.; Borgi, L.; Willett, W.C.; Manson, J.E.; Sun, Q.; Hu, F.B. Plant-Based Dietary Patterns and Incidence of Type 2 Diabetes in US Men and Women: Results from Three Prospective Cohort Studies. PLoS Med. 2016, 13, e1002039. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Satija, A.; Bhupathiraju, S.N.; Spiegelman, D.; Chiuve, S.E.; Manson, J.E.; Willett, W.; Rexrode, K.M.; Rimm, E.B.; Hu, F.B. Healthful and Unhealthful Plant-Based Diets and the Risk of Coronary Heart Disease in U.S. Adults. J. Am. Coll. Cardiol. 2017, 70, 411–422. [Google Scholar] [CrossRef] [PubMed]
- Romanos-Nanclares, A.; Toledo, E.; Sánchez-Bayona, R.; Sánchez-Quesada, C.; Martínez-González, M.Á.; Gea, A. Healthful and unhealthful provegetarian food patterns and the incidence of breast cancer: Results from a Mediterranean cohort. Nutrition 2020, 79–80. [Google Scholar] [CrossRef] [PubMed]
- Rigi, S.; Mousavi, S.M.; Benisi-Kohansal, S.; Azadbakht, L.; Esmaillzadeh, A. The association between plant-based dietary patterns and risk of breast cancer: A case-control study. Sci. Rep. 2021, 9, 3391. [Google Scholar] [CrossRef] [PubMed]
- Sasanfar, B.; Toorang, F.; Booyani, Z.; Vassalami, F.; Mohebbi, E.; Azadbakht, L.; Zendehdel, K. Adherence to plant-based dietary pattern and risk of breast cancer among Iranian women. Eur. J. Clin. Nutr. 2021, 1–10. [Google Scholar] [CrossRef]
- Kwan, M.L.; Ambrosone, C.B.; Lee, M.M.; Barlow, J.; Krathwohl, S.E.; Ergas, I.J.; Ashley, C.H.; Bittner, J.R.; Darbinian, J.; Stronach, K.; et al. The Pathways Study: A prospective study of breast cancer survivorship within Kaiser Permanente Northern California. Cancer Causes Control 2008, 19, 1065–1076. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ross, T.R.; Ng, D.; Brown, J.S.; Pardee, R.; Hornbrook, M.C.; Hart, G.; Steiner, J.F. The HMO Research Network Virtual Data Warehouse: A Public Data Model to Support Collaboration. EGEMS. EGEMS 2014, 2, 1049. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chubak, J.; Ziebell, R.; Greenlee, R.T.; Honda, S.; Hornbrook, M.C.; Epstein, M.; Nekhlyudov, L.; Pawloski, P.A.; Ritzwoller, D.P.; Ghai, N.R.; et al. The Cancer Research Network: A platform for epidemiologic and health services research on cancer prevention, care, and outcomes in large, stable populations. Cancer Causes Control 2016, 27, 1315–1323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Therneau, T.M. A Package for Survival Analysis in R; R Package Version 3.2-7. Available online: https://CRAN.R-project.org/package=survival (accessed on 21 January 2021).
- Sjoberg, D.D.; Curry, M.; Hannum, M.; Whiting, K.; Zabor, E.C. gtsummary: Presentation-Ready Data Summary and Analytic Result Tables; R Package Version 1.3.5. Available online: https://CRAN.R-project.org/package=gtsummary (accessed on 21 January 2021).
- Gohel, D. flextable: Functions for Tabular Reporting; R Package Version 0.6.1. Available online: https://CRAN.R-project.org/package=flextable (accessed on 21 January 2021).
- Wickham, H. ggplot2: Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2016. [Google Scholar]
- Auguie, B. gridExtra: Miscellaneous Functions for “Grid” Graphics; R Package Version 2.3. Available online: https://CRAN.R-project.org/package=gridExtra (accessed on 21 January 2021).
- Pedersen, T.L. patchwork: The Composer of Plots; R Package Version 1.1.1. Available online: https://CRAN.R-project.org/package=patchwork (accessed on 21 January 2021).
- Terranova, C.O.; Protani, M.M.; Reeves, M.M. Overall Dietary Intake and Prognosis after Breast Cancer: A Systematic Review. Nutr Cancer 2018, 70, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Ergas, I.J.; Cespedes Feliciano, E.M.; Bradshaw, P.T.; Roh, J.M.; Kwan, M.L.; Cadenhead, J.; Santiago-Torres, M.; Troeschel, A.N.; Laraia, B.; Madsen, K.; et al. Diet Quality and Breast Cancer Recurrence and Survival: The Pathways Study. JNCI Cancer Spectr. 2021, 5, pkab019. [Google Scholar] [CrossRef] [PubMed]
- Kwan, M.L.; Weltzien, E.; Kushi, L.H.; Castillo, A.; Slattery, M.L.; Caan, B.J. Dietary patterns and breast cancer recurrence and survival among women with early-stage breast cancer. J. Clin. Oncol. 2009, 27, 919–926. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Izano, M.A.; Fung, T.T.; Chiuve, S.S.; Hu, F.B.; Holmes, M.D. Are diet quality scores after breast cancer diagnosis associated with improved breast cancer survival? Nutr. Cancer 2013, 65, 820–826. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vrieling, A.; Buck, K.; Seibold, P.; Heinz, J.; Obi, N.; Flesch-Janys, D.; Chang-Claude, J. Dietary patterns and survival in German postmenopausal breast cancer survivors. Br. J. Cancer 2013, 108, 188–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.; Caulfield, L.E.; Rebholz, C.M. Healthy Plant-Based Diets Are Associated with Lower Risk of All-Cause Mortality in US Adults. J. Nutr. 2018, 148, 624–631. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bradshaw, P.T.; Stevens, J.; Khankari, N.; Teitelbaum, S.L.; Neugut, A.I.; Gammon, M.D. Cardiovascular Disease Mortality Among Breast Cancer Survivors. Epidemiology 2016, 27, 6–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pan, H.; Gray, R.; Braybrooke, J.; Davies, C.; Taylor, C.; McGale, P.; Peto, R.; Pritchard, K.I.; Bergh, J.; Dowsett, M.; et al. 20-Year Risks of Breast-Cancer Recurrence after Stopping Endocrine Therapy at 5 Years. N. Engl. J. Med. 2017, 377, 1836–1846. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Overall | Quintiles of PDI Score | |||||
|---|---|---|---|---|---|---|
| Characteristic | n = 3646 1 | Q1, n = 784 1 | Q2, n = 749 1 | Q3, n = 815 1 | Q4, n = 682 1 | Q5, n = 616 1 |
| Scores: 32–48 | Scores: 49–52 | Scores: 53–56 | Scores: 57–60 | Scores: 61–79 | ||
| Age at diagnosis | 60 (12) | 60 (12) | 60 (12) | 60 (12) | 59 (12) | 58 (12) |
| BMI (kg/m2) | 28 (7) | 29 (7) | 28 (7) | 28 (7) | 28 (7) | 28 (7) |
| Physical Activity (MET h/week) | 54 (36) | 46 (34) | 50 (34) | 54 (35) | 58 (36) | 63 (39) |
| Energy intake (kcal/day) | 1465 (568) | 1112 (432) | 1296 (461) | 1481 (505) | 1679 (551) | 1864 (580) |
| Race/Ethnicity | ||||||
| White | 2481 (68%) | 552 (70%) | 501 (67%) | 563 (69%) | 446 (65%) | 419 (68%) |
| Black | 237 (6.5%) | 51 (6.5%) | 53 (7.1%) | 51 (6.3%) | 45 (6.6%) | 37 (6.0%) |
| Asian/Pacific Islander | 474 (13%) | 96 (12%) | 96 (13%) | 111 (14%) | 93 (14%) | 78 (13%) |
| Hispanic | 378 (10%) | 74 (9.4%) | 85 (11%) | 73 (9.0%) | 77 (11%) | 69 (11%) |
| American Indian/Alaska Native | 76 (2.1%) | 11 (1.4%) | 14 (1.9%) | 17 (2.1%) | 21 (3.1%) | 13 (2.1%) |
| Education | ||||||
| High school or less | 544 (15%) | 138 (18%) | 129 (17%) | 118 (14%) | 85 (12%) | 74 (12%) |
| Some college | 1241 (34%) | 305 (39%) | 239 (32%) | 269 (33%) | 241 (35%) | 187 (30%) |
| College graduate | 1022 (28%) | 194 (25%) | 223 (30%) | 226 (28%) | 199 (29%) | 180 (29%) |
| Postgraduate | 839 (23%) | 147 (19%) | 158 (21%) | 202 (25%) | 157 (23%) | 175 (28%) |
| Menopausal Status | ||||||
| Premenopausal | 1057 (29%) | 207 (26%) | 205 (27%) | 236 (29%) | 207 (30%) | 202 (33%) |
| Postmenopausal | 2589 (71%) | 577 (74%) | 544 (73%) | 579 (71%) | 475 (70%) | 414 (67%) |
| Smoking status | ||||||
| Never | 2091 (57%) | 422 (54%) | 410 (55%) | 469 (58%) | 418 (61%) | 372 (60%) |
| Former | 1403 (38%) | 325 (41%) | 305 (41%) | 317 (39%) | 233 (34%) | 223 (36%) |
| Current | 152 (4.2%) | 37 (4.7%) | 34 (4.5%) | 29 (3.6%) | 31 (4.5%) | 21 (3.4%) |
| AJCC Cancer Stage | ||||||
| 1 | 1998 (55%) | 424 (54%) | 411 (55%) | 463 (57%) | 369 (54%) | 331 (54%) |
| 2 | 1247 (34%) | 279 (36%) | 267 (36%) | 268 (33%) | 226 (33%) | 207 (34%) |
| 3 | 346 (9.5%) | 72 (9.2%) | 60 (8.0%) | 69 (8.5%) | 77 (11%) | 68 (11%) |
| 4 | 55 (1.5%) | 9 (1.1%) | 11 (1.5%) | 15 (1.8%) | 10 (1.5%) | 10 (1.6%) |
| ER Status | ||||||
| Positive | 3063 (84%) | 651 (83%) | 631 (84%) | 680 (83%) | 573 (84%) | 528 (86%) |
| Negative | 583 (16%) | 133 (17%) | 118 (16%) | 135 (17%) | 109 (16%) | 88 (14%) |
| HER2 Status | ||||||
| Positive | 469 (13%) | 103 (13%) | 92 (12%) | 109 (13%) | 86 (13%) | 79 (13%) |
| Negative | 3037 (83%) | 654 (83%) | 628 (84%) | 673 (83%) | 567 (83%) | 515 (84%) |
| Missing | 140 (3.8%) | 27 (3.4%) | 29 (3.9%) | 33 (4.0%) | 29 (4.3%) | 22 (3.6%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anyene, I.C.; Ergas, I.J.; Kwan, M.L.; Roh, J.M.; Ambrosone, C.B.; Kushi, L.H.; Cespedes Feliciano, E.M. Plant-Based Dietary Patterns and Breast Cancer Recurrence and Survival in the Pathways Study. Nutrients 2021, 13, 3374. https://doi.org/10.3390/nu13103374
Anyene IC, Ergas IJ, Kwan ML, Roh JM, Ambrosone CB, Kushi LH, Cespedes Feliciano EM. Plant-Based Dietary Patterns and Breast Cancer Recurrence and Survival in the Pathways Study. Nutrients. 2021; 13(10):3374. https://doi.org/10.3390/nu13103374
Chicago/Turabian StyleAnyene, Ijeamaka C., Isaac J. Ergas, Marilyn L. Kwan, Janise M. Roh, Christine B. Ambrosone, Lawrence H. Kushi, and Elizabeth M. Cespedes Feliciano. 2021. "Plant-Based Dietary Patterns and Breast Cancer Recurrence and Survival in the Pathways Study" Nutrients 13, no. 10: 3374. https://doi.org/10.3390/nu13103374
APA StyleAnyene, I. C., Ergas, I. J., Kwan, M. L., Roh, J. M., Ambrosone, C. B., Kushi, L. H., & Cespedes Feliciano, E. M. (2021). Plant-Based Dietary Patterns and Breast Cancer Recurrence and Survival in the Pathways Study. Nutrients, 13(10), 3374. https://doi.org/10.3390/nu13103374






