Is Drinking Alcohol Really Linked to Cardiovascular Health? Evidence from the Kardiovize 2030 Project
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Alcohol Consumption Assessment
2.3. Assessment of Cardiovascular Health
2.4. Statistical Analyses
3. Results
3.1. Relations of Total Alcohol Intake with Cardiovascular Risk Factors
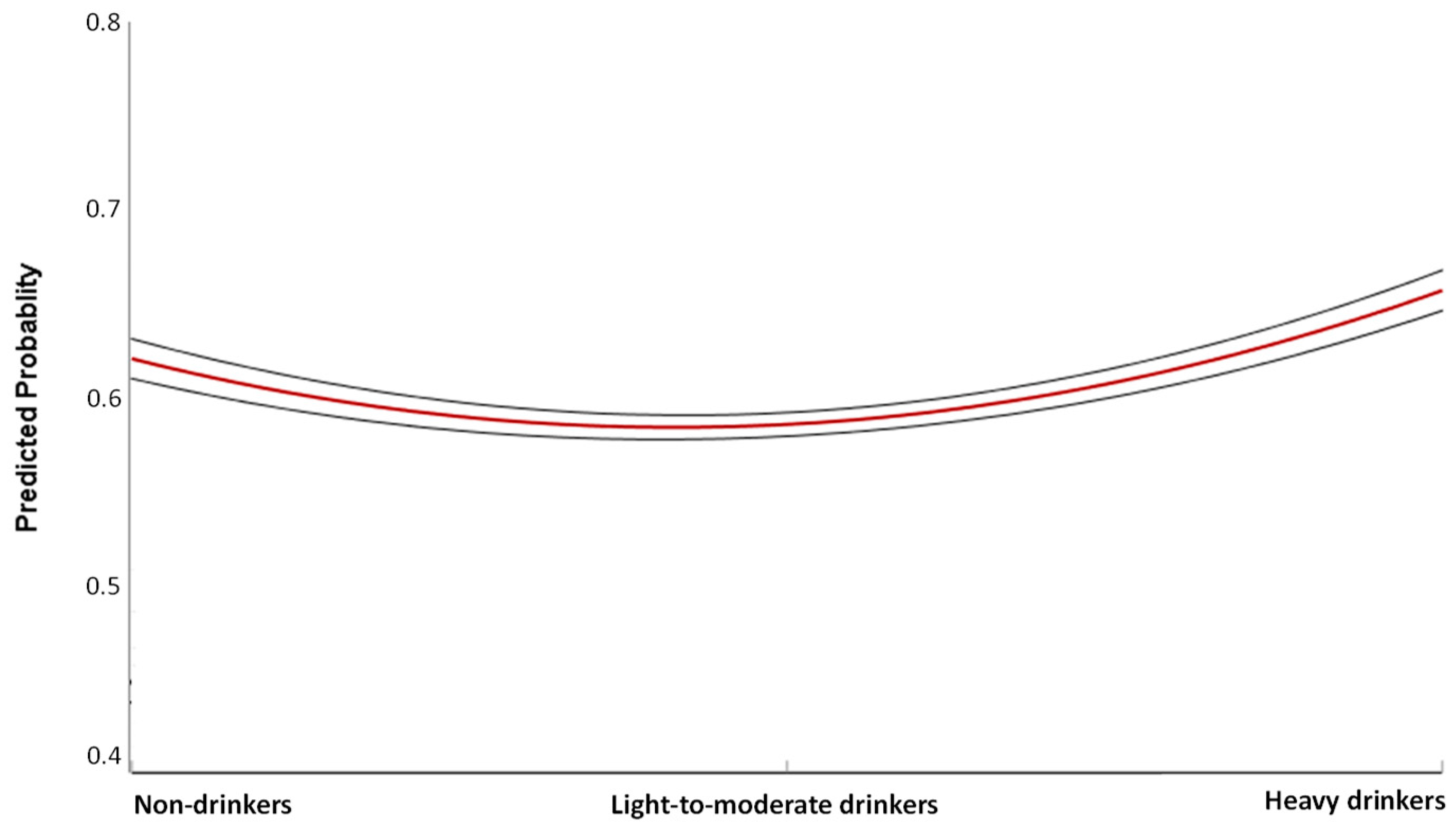
3.2. Total Alcohol Intake and Cardiovascular Health
3.3. Total Alcohol Intake and Cardiovascular Health
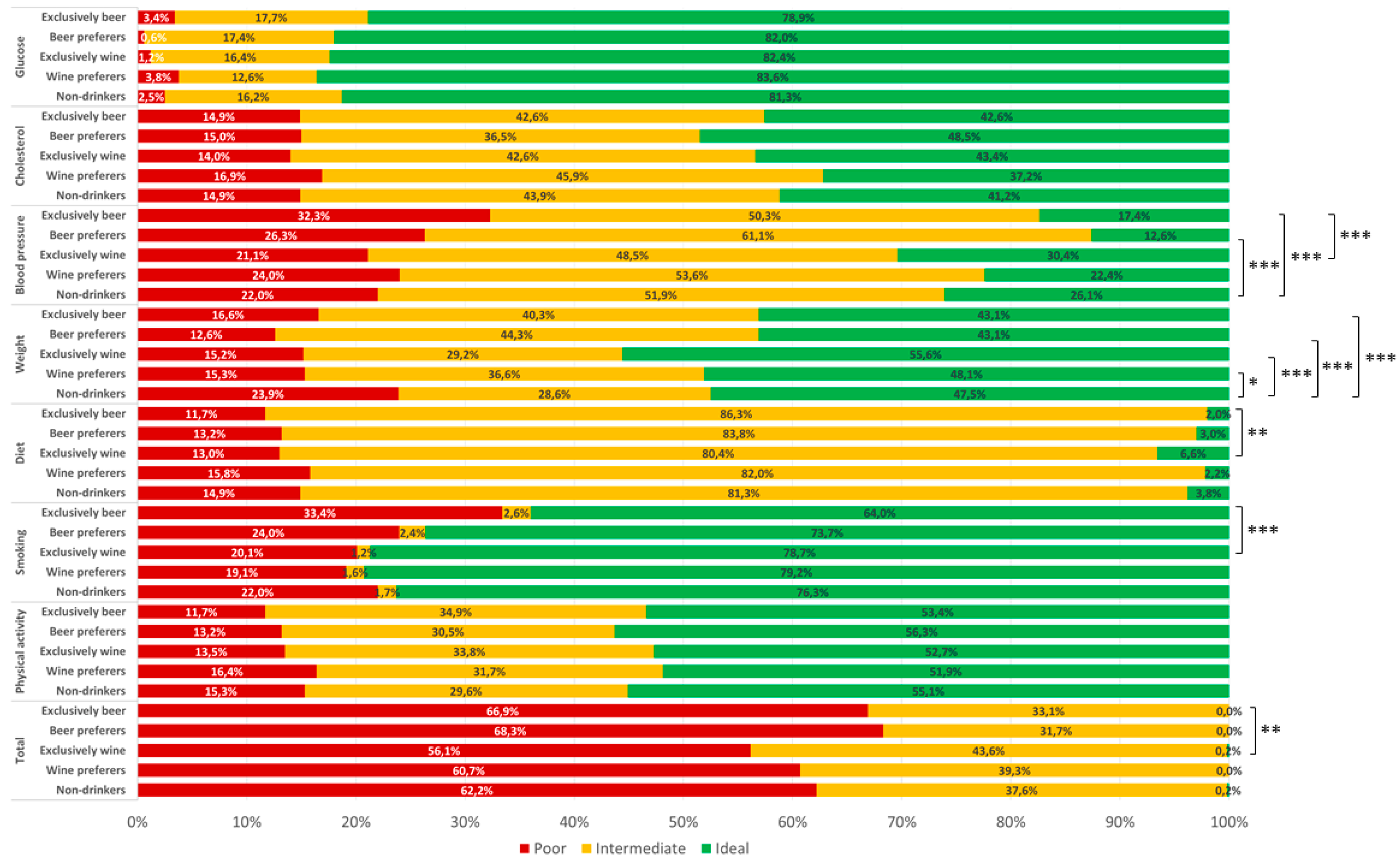
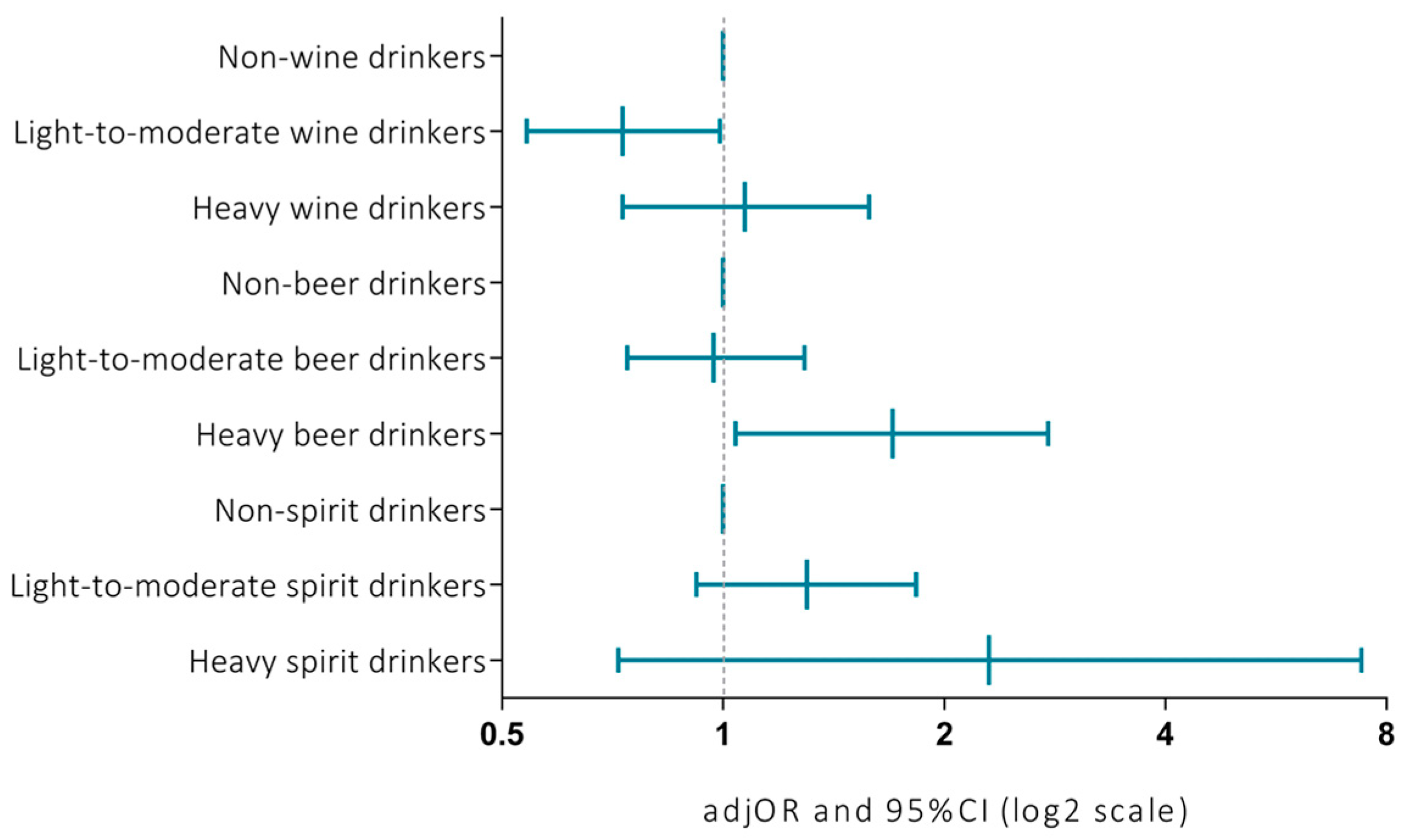
3.4. Relations of Alcohol Consumption with CVH According to Types of Beverages
3.5. Covariate Relations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Global Status Report on Alcohol and Health; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- O’Keefe, J.H.; Bybee, K.A.; Lavie, C.J. Alcohol and cardiovascular health: The razor-sharp double-edged sword. J. Am. Coll. Cardiol. 2007, 50, 1009–1014. [Google Scholar] [CrossRef] [PubMed]
- O’Keefe, J.H.; Bhatti, S.K.; Bajwa, A.; DiNicolantonio, J.J.; Lavie, C.J. Alcohol and cardiovascular health: The dose makes the poison or the remedy. Mayo Clin. Proc. 2014, 89, 382–393. [Google Scholar] [CrossRef] [PubMed]
- Marfella, R.; Cacciapuoti, F.; Siniscalchi, M.; Sasso, F.C.; Marchese, F.; Cinone, F.; Musacchio, E.; Marfella, M.A.; Ruggiero, L.; Chiorazzo, G.; et al. Effect of moderate red wine intake on cardiac prognosis after recent acute myocardial infarction of subjects with Type 2 diabetes mellitus. Diabet. Med. 2006, 23, 974–981. [Google Scholar] [CrossRef] [PubMed]
- Chiva-Blanch, G.; Urpi-Sarda, M.; Ros, E.; Arranz, S.; Valderas-Martínez, P.; Casas, R.; Sacanella, E.; Llorach, R.; Lamuela-Raventos, R.M.; Andres-Lacueva, C.; et al. Dealcoholized red wine decreases systolic and diastolic blood pressure and increases plasma nitric oxide: Short communication. Circ. Res. 2012, 111, 1065–1068. [Google Scholar] [CrossRef]
- Krnic, M.; Modun, D.; Budimir, D.; Gunjaca, G.; Jajic, I.; Vukovic, J.; Salamunic, I.; Sutlovic, D.; Kozina, B.; Boban, M. Comparison of acute effects of red wine, beer and vodka against hyperoxia-induced oxidative stress and increase in arterial stiffness in healthy humans. Atherosclerosis 2011, 218, 530–535. [Google Scholar] [CrossRef]
- Chiva-Blanch, G.; Urpi-Sarda, M.; Ros, E.; Valderas-Martinez, P.; Casas, R.; Arranz, S.; Guillén, M.; Lamuela-Raventós, R.M.; Llorach, R.; Andres-Lacueva, C.; et al. Effects of red wine polyphenols and alcohol on glucose metabolism and the lipid profile: A randomized clinical trial. Clin. Nutr. 2013, 32, 200–206. [Google Scholar] [CrossRef]
- Corder, R.; Mullen, W.; Khan, N.Q.; Marks, S.C.; Wood, E.G.; Carrier, M.J.; Crozier, A. Oenology: Red wine procyanidins and vascular health. Nature 2006, 444, 566. [Google Scholar] [CrossRef]
- Ellison, R.C. Importance of pattern of alcohol consumption. Circulation 2005, 112, 3818–3819. [Google Scholar] [CrossRef]
- Mukamal, K.J.; Jensen, M.K.; Grønbaek, M.; Stampfer, M.J.; Manson, J.E.; Pischon, T.; Rimm, E.B. Drinking frequency, mediating biomarkers, and risk of myocardial infarction in women and men. Circulation 2005, 112, 1406–1413. [Google Scholar] [CrossRef]
- Mukamal, K.J.; Conigrave, K.M.; Mittleman, M.A.; Camargo, C.A.; Stampfer, M.J.; Willett, W.C.; Rimm, E.B. Roles of drinking pattern and type of alcohol consumed in coronary heart disease in men. N. Engl. J. Med. 2003, 348, 109–118. [Google Scholar] [CrossRef]
- Huffman, M.D.; Capewell, S.; Ning, H.; Shay, C.M.; Ford, E.S.; Lloyd-Jones, D.M. Cardiovascular health behavior and health factor changes (1988-2008) and projections to 2020: Results from the National Health and Nutrition Examination Surveys. Circulation 2012, 125, 2595–2602. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef] [PubMed]
- Agodi, A.; Maugeri, A.; Kunzova, S.; Sochor, O.; Bauerova, H.; Kiacova, N.; Barchitta, M.; Vinciguerra, M. Association of Dietary Patterns with Metabolic Syndrome: Results from the Kardiovize Brno 2030 Study. Nutrients 2018, 10, 898. [Google Scholar] [CrossRef] [PubMed]
- Maugeri, A.; Kunzova, S.; Medina-Inojosa, J.R.; Agodi, A.; Barchitta, M.; Homolka, M.; Kiacova, N.; Bauerova, H.; Sochor, O.; Lopez-Jimenez, F.; et al. Association between eating time interval and frequency with ideal cardiovascular health: Results from a random sample Czech urban population. Nutr. Metab. Cardiovasc. Dis. 2018. [Google Scholar] [CrossRef] [PubMed]
- Hruskova, J.; Maugeri, A.; Podrouzkova, H.; Stipalova, T.; Jakubik, J.; Barchitta, M.; Medina-Inojosa, J.R.; Homolka, M.; Agodi, A.; Kunzova, S.; et al. Association of Cardiovascular Health with Epicardial Adipose Tissue and Intima Media Thickness: The Kardiovize Study. J. Clin. Med. 2018, 7, 113. [Google Scholar] [CrossRef]
- Movsisyan, N.K.; Vinciguerra, M.; Lopez-Jimenez, F.; Kunzová, Š.; Homolka, M.; Jaresova, J.; Cífková, R.; Sochor, O. Kardiovize Brno 2030, a prospective cardiovascular health study in Central Europe: Methods, baseline findings and future directions. Eur. J. Prev. Cardiol. 2017, 25. [Google Scholar] [CrossRef]
- Maugeri, A.; Medina-Inojosa, J.R.; Kunzova, S.; Agodi, A.; Barchitta, M.; Sochor, O.; Lopez-Jimenez, F.; Geda, Y.E.; Vinciguerra, M. Sleep Duration and Excessive Daytime Sleepiness Are Associated with Obesity Independent of Diet and Physical Activity. Nutrients 2018, 10, 1219. [Google Scholar] [CrossRef]
- Buzova, D.; Maugeri, A.; Liguori, A.; Napodano, C.; Lo Re, O.; Oben, J.; Alisi, A.; Gasbarrini, A.; Grieco, A.; Cerveny, J.; et al. Circulating histone signature of human lean metabolic-associated fatty liver disease (MAFLD). Clin. Epigenet. 2020, 12, 126. [Google Scholar] [CrossRef]
- Maugeri, A.; Barchitta, M.; Kunzova, S.; Bauerova, H.; Agodi, A.; Vinciguerra, M. The association of social and behavioral factors with dietary risks in adults: Evidence from the Kardiovize Brno 2030 study. Nutr. Metab. Cardiovasc. Dis. 2020, 896–906. [Google Scholar] [CrossRef]
- Maugeri, A.; Hruskova, J.; Jakubik, J.; Hlinomaz, O.; Medina-Inojosa, J.R.; Barchitta, M.; Agodi, A.; Vinciguerra, M. How dietary patterns affect left ventricular structure, function and remodelling: Evidence from the Kardiovize Brno 2030 study. Sci. Rep. 2019, 9, 19154. [Google Scholar] [CrossRef]
- Lo Re, O.; Maugeri, A.; Hruskova, J.; Jakubik, J.; Kucera, J.; Bienertova-Vasku, J.; Oben, J.A.; Kubala, L.; Dvorakova, A.; Ciz, M.; et al. Obesity-induced nucleosome release predicts poor cardio-metabolic health. Clin. Epigenet. 2019, 12, 2. [Google Scholar] [CrossRef] [PubMed]
- Medina-Inojosa, J.R.; Vinciguerra, M.; Maugeri, A.; Kunzova, S.; Sochor, O.; Movsisyan, N.; Geda, Y.E.; Stokin, G.B.; Lopez-Jimenez, F. Prevalence of ideal cardiovascular health in a Central European community: Results from the Kardiovize Brno 2030 Project. Eur. J. Prev. Cardiol. 2019, 27. [Google Scholar] [CrossRef] [PubMed]
- Fiala, J.; Sochor, O.; Klimusová, H.; Homolka, M. Alcohol Consumption in Population Aged 25-65 Years Living in the Metropolis of South Moravia, Czech Republic. Cent. Eur. J. Public Health 2017, 25, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Maugeri, A.; Hruskova, J.; Jakubik, J.; Kunzova, S.; Sochor, O.; Barchitta, M.; Agodi, A.; Bauerova, H.; Medina-Inojosa, J.R.; Vinciguerra, M. Dietary antioxidant intake decreases carotid intima media thickness in women but not in men: A cross-sectional assessment in the Kardiovize study. Free Radic. Biol. Med. 2019, 131, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Dufour, M.C. What is moderate drinking? Defining “drinks” and drinking levels. Alcohol Res. Health 1999, 23, 5–14. [Google Scholar]
- Folsom, A.R.; Yatsuya, H.; Nettleton, J.A.; Lutsey, P.L.; Cushman, M.; Rosamond, W.D.; Investigators, A.S. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J. Am. Coll. Cardiol. 2011, 57, 1690–1696. [Google Scholar] [CrossRef]
- Di Castelnuovo, A.; Costanzo, S.; Bagnardi, V.; Donati, M.B.; Iacoviello, L.; de Gaetano, G. Alcohol dosing and total mortality in men and women: An updated meta-analysis of 34 prospective studies. Arch. Intern. Med. 2006, 166, 2437–2445. [Google Scholar] [CrossRef]
- Djoussé, L.; Gaziano, J.M. Alcohol consumption and risk of heart failure in the Physicians’ Health Study, I. Circulation 2007, 115, 34–39. [Google Scholar] [CrossRef]
- Sacco, R.L.; Elkind, M.; Boden-Albala, B.; Lin, I.F.; Kargman, D.E.; Hauser, W.A.; Shea, S.; Paik, M.C. The protective effect of moderate alcohol consumption on ischemic stroke. JAMA 1999, 281, 53–60. [Google Scholar] [CrossRef]
- Mukamal, K.J.; Chung, H.; Jenny, N.S.; Kuller, L.H.; Longstreth, W.T.; Mittleman, M.A.; Burke, G.L.; Cushman, M.; Beauchamp, N.J.; Siscovick, D.S. Alcohol use and risk of ischemic stroke among older adults: The cardiovascular health study. Stroke 2005, 36, 1830–1834. [Google Scholar] [CrossRef] [PubMed]
- Femia, R.; Natali, A.; L’Abbate, A.; Ferrannini, E. Coronary atherosclerosis and alcohol consumption: Angiographic and mortality data. Arter. Thromb. Vasc. Biol. 2006, 26, 1607–1612. [Google Scholar] [CrossRef] [PubMed]
- Vliegenthart, R.; Oei, H.H.; van den Elzen, A.P.; van Rooij, F.J.; Hofman, A.; Oudkerk, M.; Witteman, J.C. Alcohol consumption and coronary calcification in a general population. Arch. Intern. Med. 2004, 164, 2355–2360. [Google Scholar] [CrossRef] [PubMed]
- Schminke, U.; Luedemann, J.; Berger, K.; Alte, D.; Mitusch, R.; Wood, W.G.; Jaschinski, A.; Barnow, S.; John, U.; Kessler, C. Association between alcohol consumption and subclinical carotid atherosclerosis: The Study of Health in Pomerania. Stroke 2005, 36, 1746–1752. [Google Scholar] [CrossRef] [PubMed]
- Lucas, D.L.; Brown, R.A.; Wassef, M.; Giles, T.D. Alcohol and the cardiovascular system: Research challenges and opportunities. J. Am. Coll. Cardiol. 2005, 45, 1916–1924. [Google Scholar] [CrossRef]
- Klatsky, A.L. Alcohol and stroke: An epidemiological labyrinth. Stroke 2005, 36, 1835–1836. [Google Scholar] [CrossRef]
- Yusuf, S.; Hawken, S.; Ounpuu, S.; Dans, T.; Avezum, A.; Lanas, F.; McQueen, M.; Budaj, A.; Pais, P.; Varigos, J.; et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet 2004, 364, 937–952. [Google Scholar] [CrossRef]
- Mukamal, K.J.; Chiuve, S.E.; Rimm, E.B. Alcohol consumption and risk for coronary heart disease in men with healthy lifestyles. Arch. Intern. Med. 2006, 166, 2145–2150. [Google Scholar] [CrossRef]
- Renaud, S.; de Lorgeril, M. Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet 1992, 339, 1523–1526. [Google Scholar] [CrossRef]
- Grønbaek, M.; Deis, A.; Sørensen, T.I.; Becker, U.; Schnohr, P.; Jensen, G. Mortality associated with moderate intakes of wine, beer, or spirits. BMJ 1995, 310, 1165–1169. [Google Scholar] [CrossRef]
- Grønbaek, M.; Becker, U.; Johansen, D.; Gottschau, A.; Schnohr, P.; Hein, H.O.; Jensen, G.; Sørensen, T.I. Type of alcohol consumed and mortality from all causes, coronary heart disease, and cancer. Ann. Intern. Med. 2000, 133, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Ferrières, J. The French paradox: Lessons for other countries. Heart 2004, 90, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Stockley, C.; Teissedre, P.L.; Boban, M.; Di Lorenzo, C.; Restani, P. Bioavailability of wine-derived phenolic compounds in humans: A review. Food Funct. 2012, 3, 995–1007. [Google Scholar] [CrossRef] [PubMed]
- Hertog, M.G.; Feskens, E.J.; Hollman, P.C.; Katan, M.B.; Kromhout, D. Dietary antioxidant flavonoids and risk of coronary heart disease: The Zutphen Elderly Study. Lancet 1993, 342, 1007–1011. [Google Scholar] [CrossRef]
- Nigdikar, S.V.; Williams, N.R.; Griffin, B.A.; Howard, A.N. Consumption of red wine polyphenols reduces the susceptibility of low-density lipoproteins to oxidation in vivo. Am. J. Clin. Nutr. 1998, 68, 258–265. [Google Scholar] [CrossRef]
- Perez-Vizcaino, F.; Duarte, J.; Andriantsitohaina, R. Endothelial function and cardiovascular disease: Effects of quercetin and wine polyphenols. Free Radic. Res. 2006, 40, 1054–1065. [Google Scholar] [CrossRef]
- Mukamal, K.J.; Chung, H.; Jenny, N.S.; Kuller, L.H.; Longstreth, W.T.; Mittleman, M.A.; Burke, G.L.; Cushman, M.; Psaty, B.M.; Siscovick, D.S. Alcohol consumption and risk of coronary heart disease in older adults: The Cardiovascular Health Study. J. Am. Geriatr. Soc. 2006, 54, 30–37. [Google Scholar] [CrossRef]
- Fuchs, C.S.; Stampfer, M.J.; Colditz, G.A.; Giovannucci, E.L.; Manson, J.E.; Kawachi, I.; Hunter, D.J.; Hankinson, S.E.; Hennekens, C.H.; Rosner, B. Alcohol consumption and mortality among women. N. Engl. J. Med. 1995, 332, 1245–1250. [Google Scholar] [CrossRef]
- Moore, A.A.; Giuli, L.; Gould, R.; Hu, P.; Zhou, K.; Reuben, D.; Greendale, G.; Karlamangla, A. Alcohol use, comorbidity, and mortality. J. Am. Geriatr. Soc. 2006, 54, 757–762. [Google Scholar] [CrossRef]

| Characteristics | Non-Drinkers (n = 500) | Drinkers | |||||
|---|---|---|---|---|---|---|---|
| Light to Moderate (n = 808) | Heavy (n = 465) | Overall (n = 1273) | |||||
| Median (IQR) or % | Median (IQR) or % | p-Value | Median (IQR) or % | p-Value | Median (IQR) or % | p-Value | |
| Age, years | 49.0 (19.0) | 47.0 (19.0) | 0.310 | 45.0 (19.0) | 0.001 | 46.0 (19.0) | 0.028 |
| Sex (% male) | 27.3% | 50.4% | <0.001 | 51.6% | <0.001 | 50.9% | <0.001 |
| Educational level (% low) * | 25.4% | 16.7% | <0.001 | 15.5% | <0.001 | 16.3% | <0.001 |
| Marital status (% living alone) | 39.5% | 35.5% | 0.147 | 41.5% | 0.538 | 37.7% | 0.477 |
| Employment (% unemployed) | 25.1% | 16.8% | 0.001 | 13.6% | <0.001 | 15.6% | <0.001 |
| Smoking (% current smokers) | 24.9% | 23.8% | 0.757 | 34.1% | <0.001 | 27.6% | 0.077 |
| BMI, kg/m2 | 25.6 (7.8) | 25.1 (5.9) | 0.277 | 25.4 (5.6) | 0.548 | 25.2 (7.8) | 0.312 |
| Waist circumference, cm | 88.0 (22.0) | 88.0 (20.0) | 0.430 | 89.0 (19.0) | 0.270 | 88.0 (20.0) | 0.302 |
| Systolic Blood Pressure, mmHg | 117.0 (21.5) | 118.0 (18.5) | 0.590 | 119.0 (19.0) | 0.083 | 118.5 (18.5) | 0.254 |
| Diastolic Blood Pressure, mmHg | 78.0 (12.5) | 78.5 (12.5) | 0.072 | 80.5 (13.0) | <0.001 | 79.5 (12.5) | 0.002 |
| Diagnosis of Hypertension | 30.9% | 31.1% | 0.921 | 29.3% | 0.610 | 30.5% | 0.874 |
| Fasting Glucose, mmol/L | 4.9 (0.7) | 4.9 (0.7) | 0.387 | 5.0 (0.7) | 0.021 | 4.9 (0.7) | 0.103 |
| Diagnosis of Diabetes | 10.4% | 9.0% | 0.415 | 6.8% | 0.057 | 8.2% | 0.147 |
| Triglycerides, mmol/L | 1.03 (0.90) | 1.03 (0.80) | 0.609 | 1.08 (0.80) | 0.022 | 1.05 (0.80) | 0.167 |
| Total Cholesterol, mmol/L | 5.13 (1.40) | 5.11 (1.30) | 0.784 | 5.12 (1.20) | 0.398 | 5.11 (1.30) | 0.571 |
| HDL Cholesterol, mmol/L | 1.47 (0.50) | 1.47 (0.50) | 0.624 | 1.56 (0.50) | 0.001 | 1.50 (0.50) | 0.061 |
| LDL Cholesterol, mmol/L | 3.14 (1.30) | 2.97 (1.20) | 0.641 | 3.03 (1.2) | 0.035 | 3.00 (1.20) | 0.206 |
| Cholesterol/HDL-Cholesterol ratio | 3.46 (1.50) | 3.27 (1.40) | 0.549 | 3.46 (1.50) | 0.005 | 3.38 (1.40) | 0.094 |
| Diagnosis of hypercholesterolemia | 28.7% | 29.3% | 0.817 | 25.7% | 0.299 | 28.0% | 0.766 |
| Cardiovascular Health Score † | 9.0 (3.0) | 9.0 (3.0) | 0.488 | 9.0 (3.0) | 0.476 | 9.0 (3.0) | 0.880 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maugeri, A.; Hlinomaz, O.; Agodi, A.; Barchitta, M.; Kunzova, S.; Bauerova, H.; Sochor, O.; Medina-Inojosa, J.R.; Lopez-Jimenez, F.; Vinciguerra, M.; et al. Is Drinking Alcohol Really Linked to Cardiovascular Health? Evidence from the Kardiovize 2030 Project. Nutrients 2020, 12, 2848. https://doi.org/10.3390/nu12092848
Maugeri A, Hlinomaz O, Agodi A, Barchitta M, Kunzova S, Bauerova H, Sochor O, Medina-Inojosa JR, Lopez-Jimenez F, Vinciguerra M, et al. Is Drinking Alcohol Really Linked to Cardiovascular Health? Evidence from the Kardiovize 2030 Project. Nutrients. 2020; 12(9):2848. https://doi.org/10.3390/nu12092848
Chicago/Turabian StyleMaugeri, Andrea, Ota Hlinomaz, Antonella Agodi, Martina Barchitta, Sarka Kunzova, Hana Bauerova, Ondrej Sochor, Jose R. Medina-Inojosa, Francisco Lopez-Jimenez, Manlio Vinciguerra, and et al. 2020. "Is Drinking Alcohol Really Linked to Cardiovascular Health? Evidence from the Kardiovize 2030 Project" Nutrients 12, no. 9: 2848. https://doi.org/10.3390/nu12092848
APA StyleMaugeri, A., Hlinomaz, O., Agodi, A., Barchitta, M., Kunzova, S., Bauerova, H., Sochor, O., Medina-Inojosa, J. R., Lopez-Jimenez, F., Vinciguerra, M., Stokin, G. B., & González-Rivas, J. P. (2020). Is Drinking Alcohol Really Linked to Cardiovascular Health? Evidence from the Kardiovize 2030 Project. Nutrients, 12(9), 2848. https://doi.org/10.3390/nu12092848









