Intra-Individual Double Burden of Malnutrition among Adults in China: Evidence from the China Health and Nutrition Survey 2015
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Assessments of Dietary Micronutrient Intakes
2.3. Anthropometric Measurements
2.4. Assessment of Covariates
2.5. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Double Burden of Undernutrition and Overnutrition
3.3. Disparity in Micronutrient Intake across BMI Levels
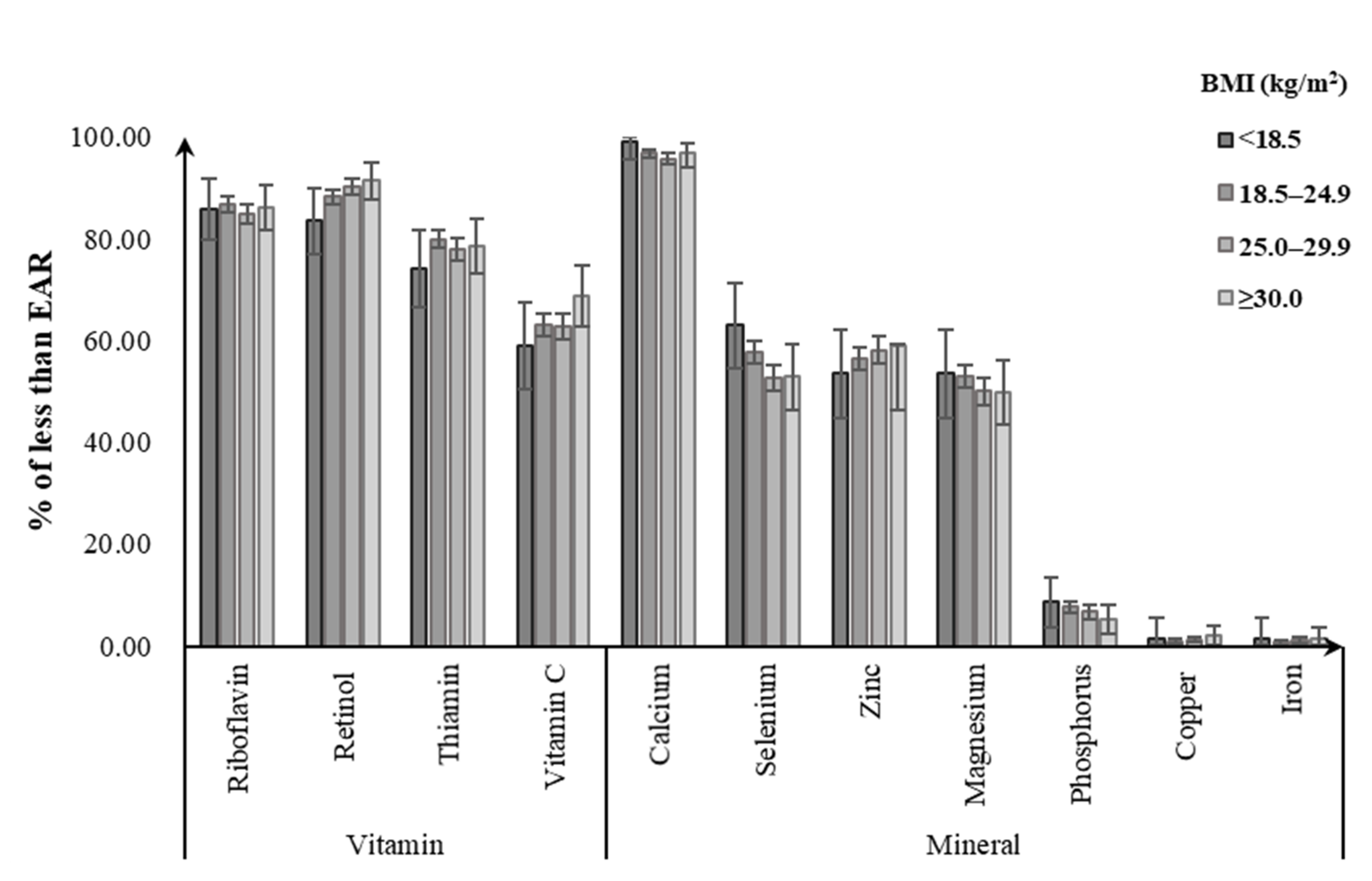
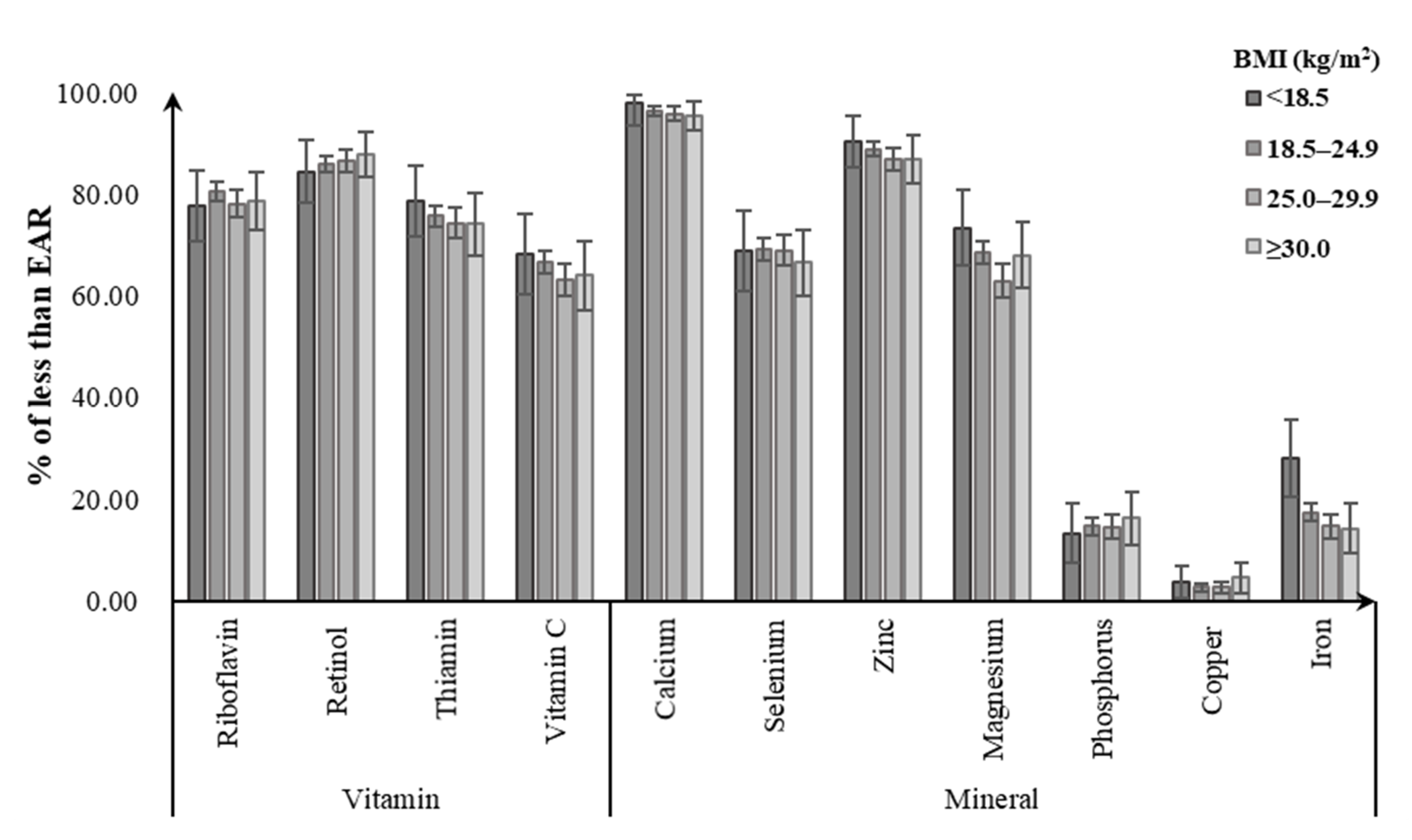
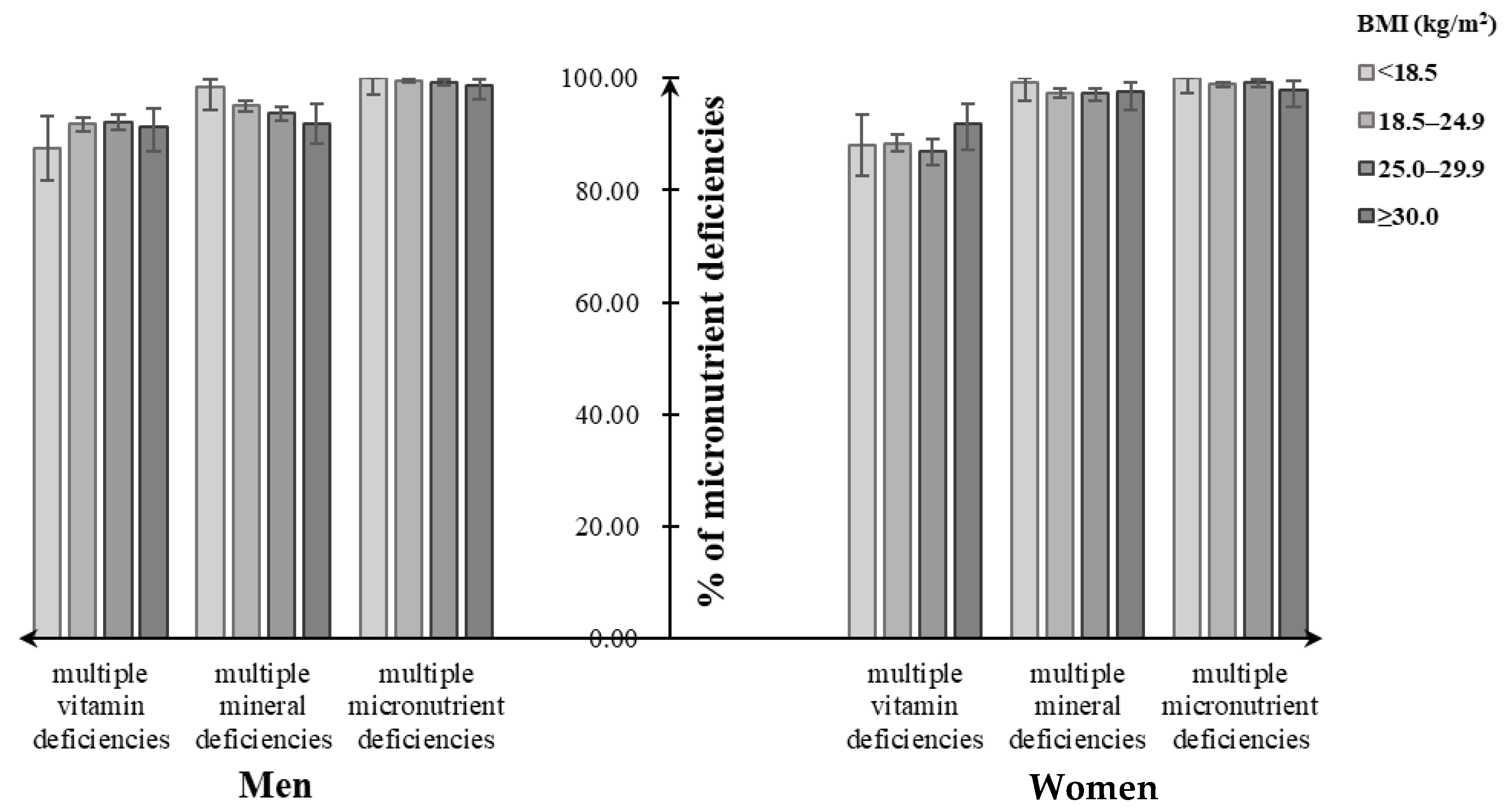
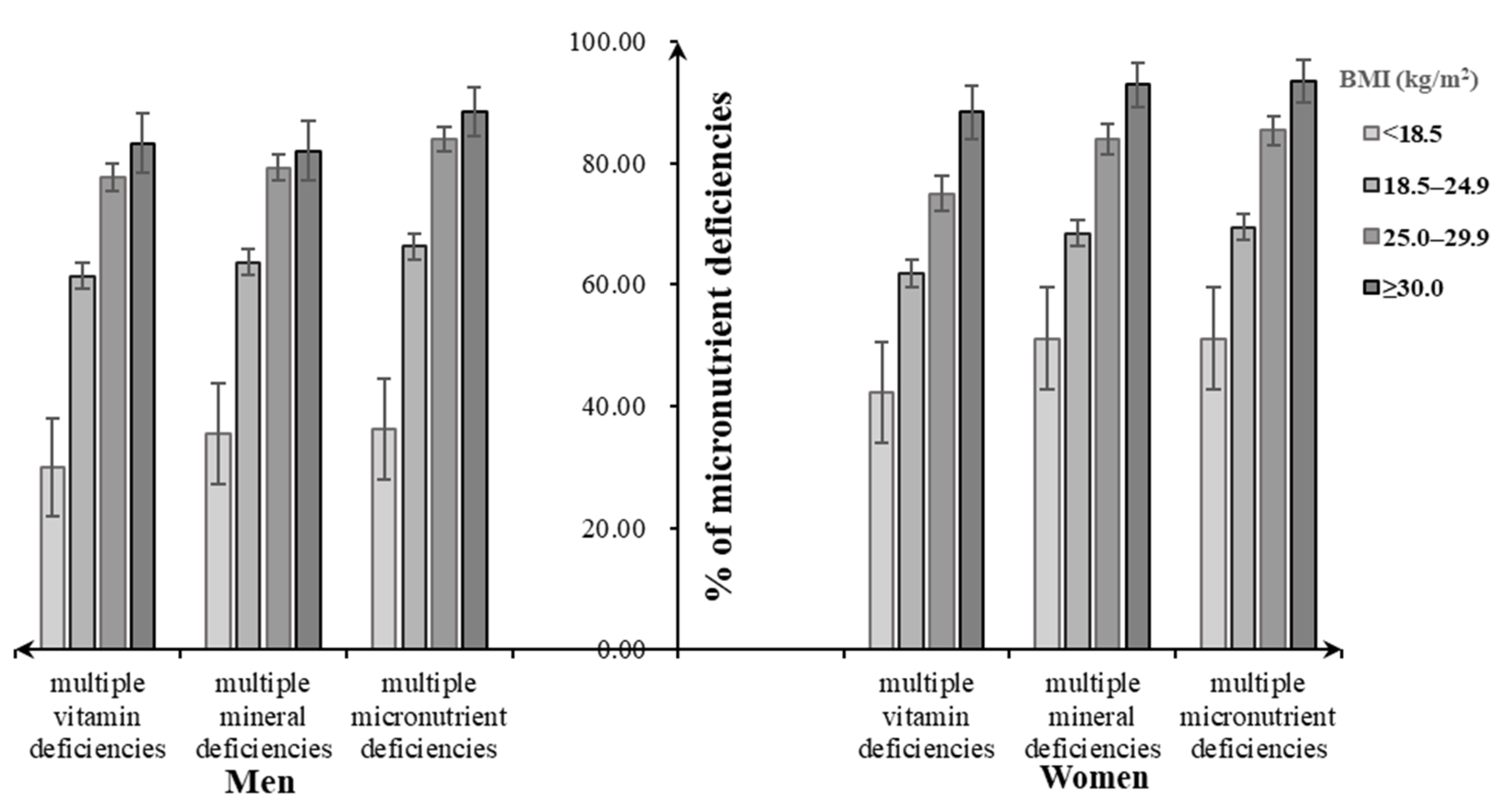
3.4. Disparity in Micronutrient Deficiency Status across BMI Levels
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Popkin, B.M.; Corvalan, C.; Grummer-Strawn, L.M. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 2020, 395, 65–74. [Google Scholar] [CrossRef]
- Shay, C.M.; Van Horn, L.; Stamler, J.; Dyer, A.R.; Brown, I.J.; Chan, Q.; Miura, K.; Zhao, L.; Okuda, N.; Daviglus, M.L.; et al. Food and nutrient intakes and their associations with lower BMI in middle-aged US adults: The International Study of Macro-/Micronutrients and Blood Pressure (INTERMAP). Am. J. Clin. Nutr. 2012, 96, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Farhat, G.; Lees, E.; Macdonald-Clarke, C.; Amirabdollahian, F. Inadequacies of micronutrient intake in normal weight and overweight young adults aged 18-25 years: A cross-sectional study. Public Health 2019, 167, 70–77. [Google Scholar] [CrossRef]
- Chinese Nutrition Society. Chinese DRIs Handbook; Standards Press of China: Beijing, China, 2014. [Google Scholar]
- Huang, Q.; Wang, L.; Zhang, B.; Wang, H.; Wang, Z. Secular trends in dietary micronutrient intakes and demographic characteristics of adults in nine provinces (autonomous regions) of China from 1991 to 2015. J. Environ. Occup. Med. 2019, 36, 410–417. [Google Scholar]
- Du, W.; Wang, H.; Zhang, J.; Zhang, J.; Su, C.; Jia, X.; Zhang, J.; Jiang, H.; Huang, F.; Ouyang, Y.; et al. Dietary vitamin a intake among Chinese adults: Findings from CNTCS2015. Nutr. J. 2018, 17, 60. [Google Scholar] [CrossRef]
- Huang, F.; Wang, Z.; Zhang, J.; Du, W.; Su, C.; Jiang, H.; Jia, X.; Ouyang, Y.; Wang, Y.; Li, L.; et al. Dietary calcium intake and food sources among Chinese adults in CNTCS. PLoS ONE 2018, 13, e0205045. [Google Scholar] [CrossRef]
- Popkin, B.M.; Du, S.; Zhai, F.; Zhang, B. Cohort Profile: The China Health and Nutrition Survey--monitoring and understanding socio-economic and health change in China, 1989–2011. Int. J. Epidemiol. 2010, 39, 1435–1440. [Google Scholar] [CrossRef]
- Wang, H.J.; Wang, Z.H.; Du, W.W.; Su, C.; Zhai, F.Y.; Zhang, B.; Zhang, J.G.; Zhang, J. Trends in dietary fiber intake in Chinese aged 45 years and above, 1991–2011. Eur. J. Clin. Nutr. 2014, 68, 619–622. [Google Scholar] [CrossRef]
- Bell, A.C.; Ge, K.; Popkin, B.M. Weight gain and its predictors in Chinese adults. Int. J. Obes. 2001, 25, 1079–1086. [Google Scholar] [CrossRef]
- Bell, A.C.; Ge, K.; Popkin, B.M. The Road to Obesity or the Path to Prevention: Motorized Transportation and Obesity in China. Obes. Res. 2002, 10, 277–283. [Google Scholar] [CrossRef]
- Monda, K.L.; Adair, L.S.; Zhai, F.; Popkin, B.M. Longitudinal relationships between occupational and domestic physical activity patterns and body weight in China. Eur. J. Clin. Nutr. 2007, 62, 1318–1325. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R., Jr.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000, 32 (Suppl. 9), S498–S504. [Google Scholar] [CrossRef]
- Jones-Smith, J.C.; Popkin, B.M. Understanding community context and adult health changes in China: Development of an urbanicity scale. Soc. Sci. Med. 2010, 71, 1436–1446. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements; National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- National Health Commission of People’s Republic of China. Chinese Dietary Reference Intakes—Part 3: Trace Element; National Health Commission of People’s Republic of China: Beijing, China, 2017.
- National Health Commission of People’s Republic of China. Chinese Dietary Reference Intakes—Part 4: Lipid-Soluble Vitamin; National Health Commission of People’s Republic of China: Beijing, China, 2018.
- National Health Commission of People’s Republic of China. Chinese Dietary Reference Intakes—Part 5: Water-Soluble Vitamin; National Health Commission of People’s Republic of China: Beijing, China, 2018.
- National Health Commission of People’s Republic of China. Chinese Dietary Reference Intakes—Part 2: Macroelement; National Health Commission of People’s Republic of China: Beijing, China, 2018.
- Wells, J.C.; Sawaya, A.L.; Wibaek, R.; Mwangome, M.; Poullas, M.S.; Yajnik, C.S.; DeMaio, A. The double burden of malnutrition: Aetiological pathways and consequences for health. Lancet 2020, 395, 75–88. [Google Scholar] [CrossRef]
- Hawkes, C.; Ruel, M.T.; Salm, L.; Sinclair, B.; Branca, F. Double-duty actions: Seizing programme and policy opportunities to address malnutrition in all its forms. Lancet 2020, 395, 142–155. [Google Scholar] [CrossRef]
- Nugent, R.; Levin, C.; Hale, J.; Hutchinson, B. Economic effects of the double burden of malnutrition. Lancet 2020, 395, 156–164. [Google Scholar] [CrossRef]
- Fongar, A.; Gödecke, T.; Qaim, M. Various forms of double burden of malnutrition problems exist in rural Kenya. BMC Public Health 2019, 19, 1543. [Google Scholar] [CrossRef]
- Dutta, M.; Selvamani, Y.; Singh, P.; Prashad, L. The double burden of malnutrition among adults in India: Evidence from the National Family Health Survey-4 (2015–16). Epidemiol. Health 2019, 41, e2019050. [Google Scholar] [CrossRef]
- Laillou, A.; Yakes, E.; Le, T.H.; Wieringa, F.T.; Le, B.M.; Moench-Pfanner, R.; Berger, J. Intra-Individual Double Burden of Overweight and Micronutrient Deficiencies among Vietnamese Women. PLoS ONE 2014, 9, e110499. [Google Scholar] [CrossRef]
- Heydenreich, J.; Melzer, K.; Flury, C.; Kayser, B. Low Energy Turnover of Physically Inactive Participants as a Determinant of Insufficient Mineral and Vitamin Intake in NHANES. Nutrients 2017, 9, 754. [Google Scholar] [CrossRef]
- Hosseini, B.; Saedisomeolia, A.; Allman-Farinelli, M. Association between Antioxidant Intake/Status and Obesity: A Systematic Review of Observational Studies. Biol. Trace Element Res. 2016, 175, 287–297. [Google Scholar] [CrossRef]
- Ferreira, T.D.S.; Torres, M.R.S.G.; Sanjuliani, A.F. Dietary calcium intake is associated with adiposity, metabolic profile, inflammatory state and blood pressure, but not with erythrocyte intracellular calcium and endothelial function in healthy pre-menopausal women. Br. J. Nutr. 2013, 110, 1079–1088. [Google Scholar] [CrossRef]
- Quann, E.E.; Fulgoni, V.L., 3rd; Auestad, N. Consuming the daily recommended amounts of dairy products would reduce the prevalence of inadequate micronutrient intakes in the United States: Diet modeling study based on NHANES 2007–2010. Nutr. J. 2015, 14, 90. [Google Scholar] [CrossRef]
- Polcz, M.E.; Barbul, A. The Role of Vitamin A in Wound Healing. Nutr. Clin. Pract. 2019, 34, 695–700. [Google Scholar] [CrossRef]
- Brown, K.H.; Rivera, J.A.; Bhutta, Z.; Gibson, R.S.; King, J.C.; Lönnerdal, B.; Ruel, M.T.; Sandtröm, B.; Wasantwisut, E.; Hotz, C. International Zinc Nutrition Consultative Group (IZiNCG) technical document #1. Assessment of the risk of zinc deficiency in populations and options for its control. Food Nutr. Bull. 2004, 25 (Suppl. 2), S99–S203. [Google Scholar] [PubMed]
- UNICEF. Report on Risk Evaluation of Vitamin and Mineral Deficiency in China; UNICEF: New York, NY, USA, 2004.
- Branca, F.; DeMaio, A.; Udomkesmalee, E.; Baker, P.; Aguayo, V.M.; Barquera, S.; Dain, K.; Keir, L.; Lartey, A.; Mugambi, G.; et al. A new nutrition manifesto for a new nutrition reality. Lancet 2020, 395, 8–10. [Google Scholar] [CrossRef]
- Ding, G.Q. Promoting balanced dietary structure and preventing micronutrient deficiencies. J. Environ. Occup. Med. 2019, 36, 407–409. [Google Scholar]
- Leão, A.L.M.; Dos Santos, L.C. Micronutrient consumption and overweight: Is there a relationship? Rev. Bras. Epidemiol. 2012, 15, 85–95. [Google Scholar] [CrossRef]
- Paeratakul, S.; Popkin, B.M.; Kohlmeier, L.; Hertz-Picciotto, I.; Guo, X.; Edwards, L.J. Measurement error in dietary data: Implications for the epidemiologic study of the diet-disease relationship. Eur. J. Clin. Nutr. 1998, 52, 722–727. [Google Scholar] [CrossRef]
- He, W.; Li, Q.; Yang, M.; Jiao, J.; Ma, X.; Zhou, Y.; Song, A.; Heymsfield, S.B.; Zhang, S.; Zhu, S. Lower BMI cutoffs to define overweight and obesity in China. Obesity 2015, 23, 684–691. [Google Scholar] [CrossRef]
| Characteristics | Participants | Underweight | Overweight | Obesity | Vitamin Deficiency | Mineral Deficiency | Underweight and Micronutrient Deficiency | Overweight/Obesity and Micronutrient Deficiency | Malnutrition 2 |
|---|---|---|---|---|---|---|---|---|---|
| Number of subjects | 6602(100.00) | 262(3.97) | 2183(33.07) | 430(6.51) | 6391(96.80) | 6600(99.97) | 262(3.97) | 2613(39.58) | 2875(43.55) |
| Sex | |||||||||
| Men | 3699(56.03) | 127(3.43) 3 | 1345(36.36) 3 | 233(6.30) | 3610(97.59) 3 | 3697(99.95) | 127(3.43) | 1578(42.66) 3 | 1705(46.09) 3 |
| Women | 2903(43.97) | 135(4.65) | 838(28.87) | 197(6.79) | 2781(95.80) | 2903(100.00) | 135(4.65) | 1035(35.65) | 1170(40.30) |
| Age | |||||||||
| 18–44 years | 3016(45.68) | 185(6.13) 3 | 887(29.41) 3 | 188(6.23) | 2928(97.08) | 3016(100.00) | 185(6.13) 3 | 1075(35.64) 3 | 1260(41.78) 3 |
| 45–59 years | 3586(54.32) | 77(2.15) | 1296(36.14) | 242(6.75) | 3463(96.57) | 3584(99.94) | 77(2.15) | 1538(42.89) | 1615(45.04) |
| Education | |||||||||
| Illiterate | 952(14.42) | 40(4.20) | 329(34.56) | 66(6.93) | 929(97.58) | 952(100.00) | 40(4.20) | 395(41.49) 3 | 435(45.69) |
| Primary school | 2572(38.96) | 88(3.42) | 878(34.14) | 179(6.96) | 2498(97.12) | 2571(99.96) | 88(3.42) | 1057(41.10) | 1145(44.52) |
| ≥High school | 3078(46.62) | 134(4.35) | 976(31.71) | 185(6.01) | 2964(96.30) | 3077(99.97) | 134(4.35) | 1161(37.72) | 1295(42.07) |
| Urbanicity index | |||||||||
| Low | 2208(33.44) | 93(4.21) | 712(32.25) | 139(6.30) 3 | 2155(97.60) 3 | 2207(99.95) | 93(4.21) | 851(38.54) | 944(42.75) |
| Medium | 2197(33.28) | 92(4.19) | 710(32.32) | 166(7.56) | 2124(96.68) | 2197(100.00) | 92(4.19) | 876(39.87) | 968(44.06) |
| High | 2197(33.28) | 77(3.50) | 761(34.64) | 125(5.69) | 2112(96.13) | 2196(99.95) | 77(3.50) | 886(40.33) | 963(43.83) |
| Yearly Income | |||||||||
| Low | 2199(33.31) | 105(4.77) | 685(31.15) 3 | 142(6.46) | 2141(97.36) | 2197(99.91) | 105(4.77) | 827(37.61) 3 | 932(42.38) 3 |
| Medium | 2202(33.35) | 80(3.63) | 774(35.15) | 157(7.13) | 2129(96.68) | 2202(100.00) | 80(3.63) | 931(42.28) | 1011(45.91) |
| High | 2201(33.34) | 77(3.50) | 724(32.89) | 131(5.95) | 2121(96.37) | 2201(100.00) | 77(3.50) | 855(38.84) | 932(42.34) |
| Physical activity | |||||||||
| Low | 2200(33.32) | 96(4.36) | 721(32.77) | 158(7.18) | 2123(96.50) | 2199(99.95) | 96(4.36) | 879(39.95) | 975(44.31) |
| Medium | 2201(33.34) | 84(3.82) | 707(32.12) | 138(6.27) | 2125(96.55) | 2201(100.00) | 84(3.82) | 845(38.39) | 929(42.21) |
| High | 2201(33.34) | 82(3.73) | 755(34.30) | 134(6.09) | 2143(97.36) | 2200(99.95) | 82(3.73) | 889(40.39) | 971(44.12) |
| Current smoking | |||||||||
| No | 4516(68.40) | 185(4.10) | 1454(32.20) 3 | 305(6.75) | 4360(96.55) | 4515(99.98) | 185(4.10) | 1759(38.95) | 1944(43.05) |
| Yes | 2086(31.60) | 77(3.69) | 729(34.95) | 125(5.99) | 2031(97.36) | 2085(99.95) | 77(3.69) | 854(40.94) | 931(44.63) |
| Current drinking | |||||||||
| No | 4306(65.22) | 197(4.58) 3 | 1340(31.12) 3 | 285(6.62) | 4150(96.38) 3 | 4306(100.00) 3 | 197(4.58) 3 | 1625(37.73) 3 | 1822(42.31) 3 |
| Yes | 2296(34.78) | 65(2.83) | 843(36.72) | 145(6.32) | 2241(97.60) | 2294(99.91) | 65(2.83) | 988(43.03) | 1053(45.86) |
| History of diet-related chronic diseases | |||||||||
| No | 1692(25.63) | 147(8.69) 3 | 327(19.33) | 34(2.01) | 1649(97.46) | 1691(99.94) | 147(8.69) 3 | 361(21.33) 3 | 508(30.02) 3 |
| Yes | 4910(74.37) | 115(2.34) | 1856(37.80) | 396(8.07) | 4742(96.58) | 4909(99.98) | 115(2.34) | 2252(45.87) | 2367(48.21) |
| Micronutrient | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| BMI < 18.5 kg/m2 | BMI 18.5–24.9kg/m2 | BMI 25.0–29.9 kg/m2 | BMI ≥ 30.0 kg/m2 | BMI <18.5 kg/m2 | BMI 18.5–24.9 kg/m2 | BMI 25.0–29.9 kg/m2 | BMI ≥ 30.0 kg/m2 | |
| Retinol (μg RAE) | 337.53 ± 71.48 | 373.40 ± 17.97 | 358.47 ± 21.90 | 346.98 ± 52.58 | 376.94 ± 53.60 | 332.48 ± 14.68 | 354.89 ± 21.27 | 294.52 ± 43.55 |
| Thiamin (mg) 2 | 0.96 ± 0.04 | 0.93 ± 0.01 | 0.96 ± 0.01 | 0.94 ± 0.03 | 0.82 ± 0.03 4 | 0.82 ± 0.01 4 | 0.83 ± 0.01 4 | 0.82 ± 0.03 4 |
| Riboflavin (mg) 2 | 0.87 ± 0.03 | 0.84 ± 0.01 | 0.88 ± 0.01 | 0.86 ± 0.02 | 0.77 ± 0.03 4 | 0.77 ± 0.01 4 | 0.79 ± 0.01 4 | 0.78 ± 0.03 4 |
| Vitamin C (mg) | 81.76 ± 9.84 | 81.13 ± 2.47 | 88.23 ± 3.02 | 73.24 ± 7.24 | 79.77 ± 14.79 | 87.54 ± 4.05 | 91.13 ± 5.87 | 93.52 ± 12.02 |
| Calcium (mg) | 382.74 ± 18.88 | 384.44 ± 4.75 | 400.13 ± 5.78 | 383.28 ± 13.89 | 354.73 ± 18.86 | 368.30 ± 5.16 4 | 369.05 ± 7.48 4 | 373.34 ± 15.32 |
| Phosphorus (mg) 3 | 987.79 ± 30.08 | 1012.60 ± 7.56 | 1054.06 ± 9.22 | 1054.13 ± 22.13 | 880.56 ± 29.92 4 | 895.98 ± 8.19 4 | 913.99 ± 11.87 4 | 889.60 ± 24.31 4 |
| Magnesium (mg) 3 | 285.88 ± 10.12 | 286.94 ± 2.54 | 301.59 ± 3.10 | 304.43 ± 7.45 | 251.43 ± 11.24 4 | 261.81 ± 3.08 4 | 272.53 ± 4.46 4 | 264.51 ± 9.13 4 |
| Iron (mg) 3 | 23.64 ± 1.02 | 23.86 ± 0.26 | 24.79 ± 0.31 | 24.52 ± 0.75 | 20.30 ± 1.03 4 | 21.19 ± 0.28 4 | 21.49 ± 0.41 4 | 22.05 ± 0.84 |
| Zinc (mg) | 11.45 ± 0.37 | 11.54 ± 0.09 | 11.89 ± 0.11 | 11.78 ± 0.27 | 9.94 ± 0.36 4 | 10.04 ± 0.10 4 | 10.01 ± 0.14 4 | 9.82 ± 0.29 4 |
| Copper (mg) 3 | 1.71 ± 0.08 | 1.81 ± 0.02 | 1.89 ± 0.03 | 1.84 ± 0.06 | 1.62 ± 0.08 | 1.66 ± 0.02 4 | 1.68 ± 0.03 4 | 1.58 ± 0.06 4 |
| Selenium (μg) 3 | 46.76 ± 2.58 | 51.88 ± 0.65 | 54.35 ± 0.79 | 53.79 ± 1.90 | 44.63 ± 2.19 | 45.22 ± 0.60 4 | 44.67 ± 0.87 4 | 44.66 ± 1.78 4 |
| Micronutrient | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| BMI < 18.5 kg/m2 | BMI 18.5–24.9kg/m2 | BMI 25.0–29.9 kg/m2 | BMI ≥ 30.0 kg/m2 | BMI < 18.5 kg/m2 | BMI 18.5–24.9 kg/m2 | BMI 25.0–29.9 kg/m2 | BMI ≥ 30.0 kg/m2 | |
| Retinol (μg RAE/1000 kcal) | 152.64 ± 31.63 | 179.15 ± 7.95 | 163.23 ± 9.69 | 152.12 ± 23.27 | 199.02 ± 27.22 | 183.17 ± 7.45 | 184.88 ± 10.80 | 168.97 ± 22.11 |
| Thiamin (mg/1000 kcal) | 0.43 ± 0.01 | 0.43 ± 0.00 | 0.43 ± 0.00 | 0.41 ± 0.01 | 0.43 ± 0.01 | 0.43 ± 0.01 | 0.43 ± 0.01 | 0.44 ± 0.01 2 |
| Riboflavin (mg/1000 kcal) | 0.40 ± 0.01 | 0.40 ± 0.00 | 0.40 ± 0.00 | 0.38 ± 0.01 | 0.41 ± 0.01 | 0.42 ± 0.01 2 | 0.42 ± 0.01 2 | 0.42 ± 0.01 2 |
| Vitamin C (mg/1000 kcal) | 38.32 ± 4.12 | 39.37 ± 1.04 | 40.14 ± 1.26 | 33.93 ± 3.03 | 42.28 ± 7.17 | 47.49 ± 1.96 2 | 48.55 ± 2.84 2 | 53.76 ± 5.82 2 |
| Calcium (mg/1000 kcal) | 183.26 ± 8.10 | 184.18 ± 2.04 | 183.24 ± 2.48 | 175.35 ± 5.96 | 194.49 ± 9.32 | 201.15 ± 2.55 2 | 197.58 ± 3.70 2 | 207.27 ± 7.57 2 |
| Phosphorus (mg/1000 kcal) | 454.70 ± 9.05 | 476.52 ± 2.27 | 477.47 ± 2.77 | 471.39 ± 6.65 | 468.42 ± 9.56 | 481.41 ± 2.62 | 479.55 ± 3.79 | 483.24 ± 7.77 |
| Magnesium (mg/1000 kcal) | 131.19 ± 3.37 | 135.05 ± 0.85 | 136.24 ± 1.03 | 135.97 ± 2.48 | 132.43 ± 3.60 | 139.35 ± 0.992 | 141.61 ± 1.43 2 | 143.15 ± 2.93 |
| Iron (mg/1000 kcal) | 10.95 ± 0.40 | 11.22 ± 0.10 | 11.20 ± 0.12 | 10.92 ± 0.29 | 10.71 ± 0.39 | 11.27 ± 0.11 | 11.11 ± 0.16 | 11.82 ± 0.32 2 |
| Zinc (mg/1000 kcal) | 5.25 ± 0.12 | 5.42 ± 0.03 | 5.37 ± 0.04 | 5.23 ± 0.09 | 5.24 ± 0.12 | 5.35 ± 0.03 | 5.24 ± 0.05 2 | 5.35 ± 0.10 |
| Copper (mg/1000 kcal) | 0.78 ± 0.03 | 0.85 ± 0.01 | 0.84 ± 0.01 | 0.82 ± 0.02 | 0.86 ± 0.03 2 | 0.88 ± 0.01 2 | 0.87 ± 0.01 | 0.85 ± 0.02 |
| Selenium (μg/1000 kcal) | 21.34 ± 1.21 | 24.59 ± 0.30 | 24.69 ± 0.37 | 23.78 ± 0.89 | 23.90 ± 1.01 | 24.21 ± 0.28 | 23.37 ± 0.40 2 | 24.20 ± 0.82 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Q.; Wang, L.; Jiang, H.; Wang, H.; Zhang, B.; Zhang, J.; Jia, X.; Wang, Z. Intra-Individual Double Burden of Malnutrition among Adults in China: Evidence from the China Health and Nutrition Survey 2015. Nutrients 2020, 12, 2811. https://doi.org/10.3390/nu12092811
Huang Q, Wang L, Jiang H, Wang H, Zhang B, Zhang J, Jia X, Wang Z. Intra-Individual Double Burden of Malnutrition among Adults in China: Evidence from the China Health and Nutrition Survey 2015. Nutrients. 2020; 12(9):2811. https://doi.org/10.3390/nu12092811
Chicago/Turabian StyleHuang, Qiumin, Liusen Wang, Hongru Jiang, Huijun Wang, Bing Zhang, Jiguo Zhang, Xiaofang Jia, and Zhihong Wang. 2020. "Intra-Individual Double Burden of Malnutrition among Adults in China: Evidence from the China Health and Nutrition Survey 2015" Nutrients 12, no. 9: 2811. https://doi.org/10.3390/nu12092811
APA StyleHuang, Q., Wang, L., Jiang, H., Wang, H., Zhang, B., Zhang, J., Jia, X., & Wang, Z. (2020). Intra-Individual Double Burden of Malnutrition among Adults in China: Evidence from the China Health and Nutrition Survey 2015. Nutrients, 12(9), 2811. https://doi.org/10.3390/nu12092811






