Assessment of Sodium Knowledge and Urinary Sodium Excretion among Regions of the United Arab Emirates: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
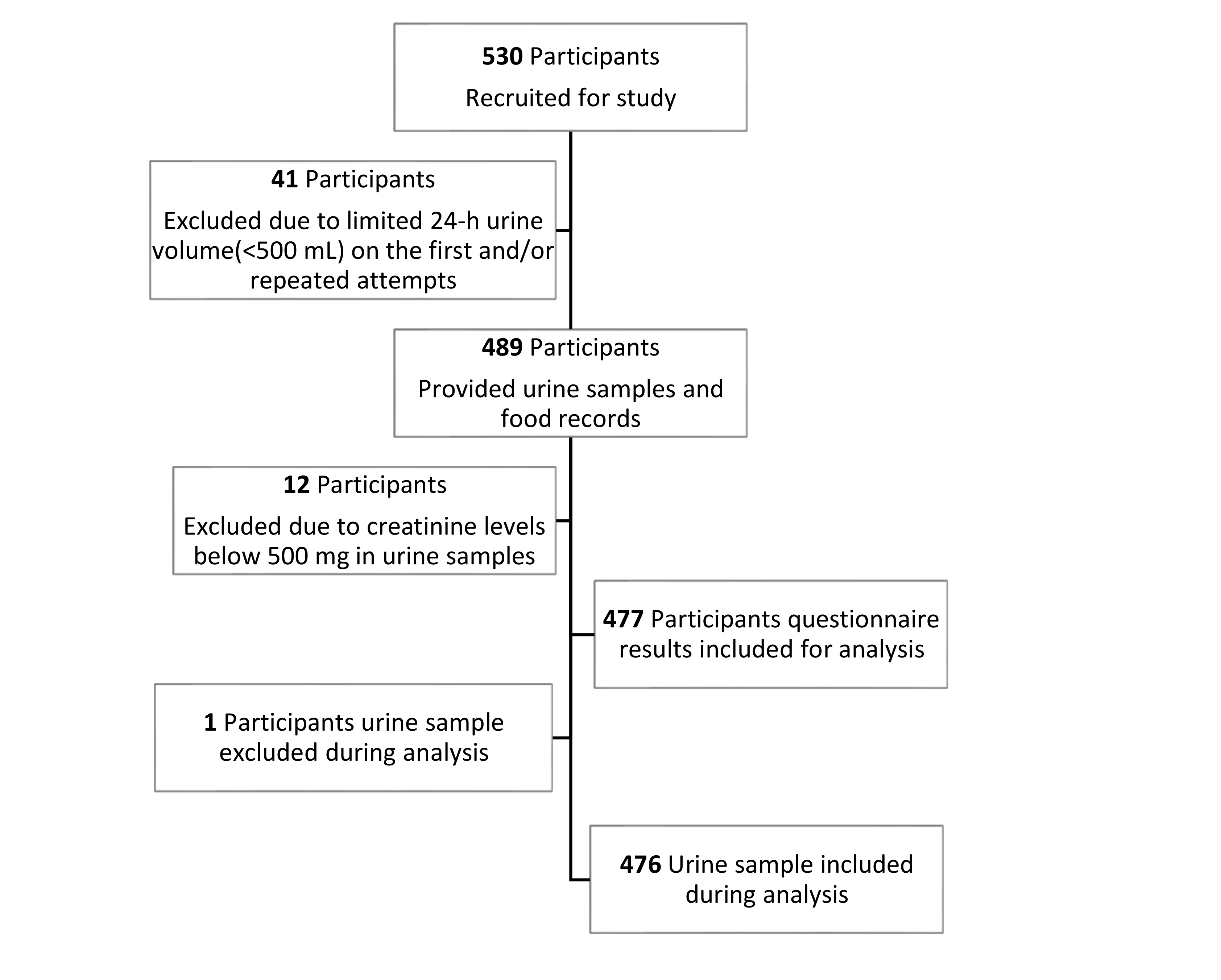
2.1. Study Design and Participants
2.2. Anthropometric Measurements
2.3. Knowledge, Attitude and Practice (KAP) Questionnaire
2.4. 24-h Urine Collections and Analysis
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
3.2. Major Findings of the Knowledge, Attitude and Practice (KAP) Questionnaire
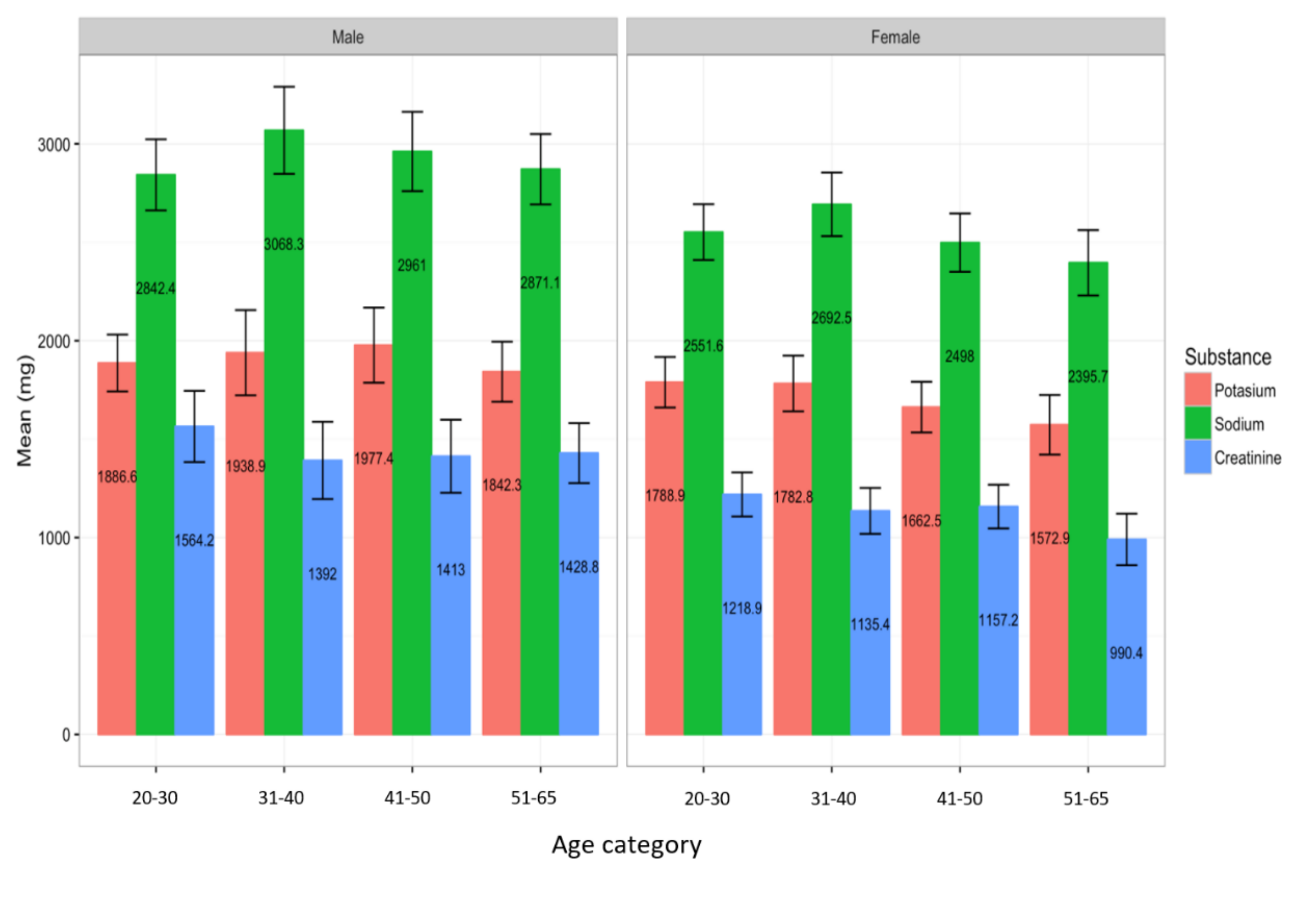
3.3. High Levels of Sodium Secretion in the UAE Population within 24-h Urine Collection
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Plan of Action for the Prevention and Control of Noncommunicable Diseases in the Eastern Mediterranean Region; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Stamler, J.; Rose, G.; Stamler, R.; Elliott, P.; Dyer, A.; Marmot, M. Intersalt study findings. Public health and medical care implications. Hypertension 1989, 14, 570–577. [Google Scholar] [CrossRef] [PubMed]
- He, F.J.; MacGregor, G.A. Effect of modest salt reduction on blood pressure: A meta-analysis of randomized trials. Implications for public health. J. Hum. Hypertens. 2002, 16, 761–770. [Google Scholar] [CrossRef] [PubMed]
- Morrison, A.C.; Ness, R.B. Sodium intake and cardiovascular disease. Ann. Rev. Public Health 2011, 32, 71–90. [Google Scholar] [CrossRef]
- World Health Organization. Noncommunicable Diseases Country Profiles 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Loney, T.; Aw, T.-C.; Handysides, D.G.; Ali, R.; Blair, I.; Grivna, M.; Shah, S.M.; Sheek-Hussein, M.; El-Sadig, M.; Sharif, A.A. An analysis of the health status of the United Arab Emirates: The ‘Big 4’public health issues. Glob. Health Action 2013, 6, 20100. [Google Scholar] [CrossRef] [PubMed]
- He, F.J.; Burnier, M.; MacGregor, G.A. Nutrition in cardiovascular disease: Salt in hypertension and heart failure. Eur. Heart J. 2011, 32, 3073–3080. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Noncommunicable Diseases 2010, Geneva. 2011. Available online: http://www.who.int/nmh/publications/ncd_report_full_en.pdf (accessed on 28 August 2020).
- Shah, S.M.; Loney, T.; Sheek-Hussein, M.; El Sadig, M.; Al Dhaheri, S.; El Barazi, I.; Al Marzouqi, L.; Aw, T.-C.; Ali, R. Hypertension prevalence, awareness, treatment, and control, in male South Asian immigrants in the United Arab Emirates: A cross-sectional study. BMC Cardiovasc. Disord. 2015, 15, 30. [Google Scholar] [CrossRef]
- Abdulle, A.M.; Nagelkerke, N.J.; Abouchacra, S.; Pathan, J.Y.; Adem, A.; Obineche, E.N. Under-treatment and under diagnosis of hypertension: A serious problem in the United Arab Emirates. BMC Cardiovasc. Disorders 2006, 6, 24. [Google Scholar] [CrossRef][Green Version]
- Aburto, N.J.; Ziolkovska, A.; Hooper, L.; Elliott, P.; Cappuccio, F.P.; Meerpohl, J.J. Effect of lower sodium intake on health: Systematic review and meta-analyses. BMJ 2013, 346, f1326. [Google Scholar] [CrossRef]
- Brown, I.J.; Tzoulaki, I.; Candeias, V.; Elliott, P. Salt intakes around the world: Implications for public health. Int. J. Epidemiol. 2009, 38, 791–813. [Google Scholar] [CrossRef]
- World Health Organization. Diet, Nutrition, and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation; World Health Organization: Geneva, Switzerland, 2003; Volume 916, p. 5. [Google Scholar]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L., Jr.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T., Jr. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA 2003, 289, 2560–2571. [Google Scholar] [CrossRef]
- Wyness, L.A.; Butriss, J.L.; Stanner, S.A. Reducing the population’s sodium intake: The UK Food Standards Agency’s salt reduction programme. Public Health Nutr. 2012, 15, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Newberry, S.J.; Chung, M.; Anderson, C.A.; Chen, C.; Fu, Z.; Tang, A.; Zhao, N.; Booth, M.; Marks, J.; Hollands, S.; et al. Sodium and Potassium Intake: Effects on Chronic Disease Outcomes and Risks; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2018. [Google Scholar]
- Kokkinos, P.; Panagiotakos, D.B.; Polychronopoulos, E. Dietary influences on blood pressure: The effect of the Mediterranean diet on the prevalence of hypertension. J. Clin. Hypertens. 2005, 7, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Wielgosz, A.; Robinson, C.; Mao, Y.; Jiang, Y.; Campbell, N.R.; Muthuri, S.; Morrison, H. The impact of using different methods to assess completeness of 24-hour urine collection on estimating dietary sodium. J. Clin. Hypertens. 2016, 18, 581–584. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R.J.; Feehally, J.; Floege, J. Comprehensive Clinical Nephrology E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Lee, R.; Nieman, D. Nutritional Assessment; McGraw-Hill Education: New York, NY, USA, 2012. [Google Scholar]
- Ismail, L.C.; Hashim, M.; Jarrar, A.H.; Mohamad, M.N.; Saleh, S.T.; Jawish, N.; Bekdache, M.; Albaghli, H.; Kdsi, D.; Aldarweesh, D. Knowledge, Attitude, and Practice on Salt and Assessment of Dietary Salt and Fat Intake among University of Sharjah Students. Nutrients 2019, 11, 941. [Google Scholar] [CrossRef] [PubMed]
- Bowers, L.D.; Wong, E.T. Kinetic serum creatinine assays. II. A critical evaluation and review. Clin. Chem. 1980, 26, 555–561. [Google Scholar] [CrossRef]
- World Health Organization. Guideline: Sodium Intake for Adults and Children; 9241504838; World Health Organization (WHO): Geneva, Switzerland, 2012. [Google Scholar]
- World Health Organization. Guideline: Potassium Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Wesson, L.G. Electrolyte excretion in relation to diurnal cycles of renal function: Plasma electrolyte concentrations and aldosterone secretion before and during salt and water balance changes in normotensive subjects. Medicine 1964, 43, 547–592. [Google Scholar] [CrossRef]
- Alkhunaizi, A.; Al Jishi, H.; Al Sadah, Z. Salt intake in Eastern Saudi Arabia. East Mediterr. Health J. 2013, 19, 915–918. [Google Scholar] [CrossRef]
- Alawwa, I.; Dagash, R.; Saleh, A.; Ahmad, A. Dietary salt consumption and the knowledge, attitudes and behavior of healthy adults: A cross-sectional study from Jordan. Libyan J. Med. 2018, 13, 1479602. [Google Scholar] [CrossRef]
- Al-Ghannami, S.; Library of Ministry of Health; Ministry of Health; Sultanate of Oman. National Nutrition Survey. 2004. Available online: https://www.moh.gov.om/en/web/statistics/ (accessed on 1 August 2020).
- Zaghloul, S.; Al-Hooti, S.N.; Al-Hamad, N.; Al-Zenki, S.; Alomirah, H.; Alayan, I.; Al-Attar, H.; Al-Othman, A.; Al-Shami, E.; Al-Somaie, M. Evidence for nutrition transition in Kuwait: Over-consumption of macronutrients and obesity. Public Health Nutr. 2013, 16, 596–607. [Google Scholar] [CrossRef]
- Alomirah, H.; Al-Zenki, S.; Husain, A. Assessment of Acrylamide Levels in Heat-Processed Foodstuffs Consumed by Kuwaitis; KISR No. 9316; Library of the Kuwait Institute of Scientific Research: Safat, Kuwait, 2008. [Google Scholar]
- Brown, I.J.; Dyer, A.R.; Chan, Q.; Cogswell, M.E.; Ueshima, H.; Stamler, J.; Elliott, P.; Group ICOR. Estimating 24-hour urinary sodium excretion from casual urinary sodium concentrations in Western populations: The INTERSALT study. Am. J. Epidemiol. 2013, 177, 1180–1192. [Google Scholar] [CrossRef]
- Lichtenstein, A.H.; Appel, L.J.; Brands, M.; Carnethon, M.; Daniels, S.; Franch, H.A.; Franklin, B.; Kris-Etherton, P.; Harris, W.S.; Howard, B. Diet and lifestyle recommendations revision 2006: A scientific statement from the American Heart Association Nutrition Committee. Circulation 2006, 114, 82–96. [Google Scholar] [CrossRef] [PubMed]
- Micha, R.; Khatibzadeh, S.; Shi, P.; Fahimi, S.; Lim, S.; Andrews, K.G.; Engell, R.E.; Powles, J.; Ezzati, M.; Mozaffarian, D. Global, regional, and national consumption levels of dietary fats and oils in 1990 and 2010: A systematic analysis including 266 country-specific nutrition surveys. BMJ 2014, 348, g2272. [Google Scholar] [CrossRef] [PubMed]
- Anderson, C.A.; Appel, L.J.; Okuda, N.; Brown, I.J.; Chan, Q.; Zhao, L.; Ueshima, H.; Kesteloot, H.; Miura, K.; Curb, J.D. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: The INTERMAP study. J. Am. Diet. Assoc. 2010, 110, 736–745. [Google Scholar] [CrossRef]
- Ashford, R.; Jones, K.; Collins, D.; Earl, K.; Moore, S.; Koulman, A.; Yarde, J.; Polly, B.; Swan, G. Assessment of Salt Intake from Urinary Sodium in Adults (Aged 19 to 64 Years) in England, 2018 to 2019. National Diet and Nutrition Survey; Public Health England: London, UK, 2020. [Google Scholar]
- Geleijnse, J.M.; Witteman, J.C.; Stijnen, T.; Kloos, M.W.; Hofman, A.; Grobbee, D.E. Sodium and potassium intake and risk of cardiovascular events and all-cause mortality: The Rotterdam Study. Eur. J. Epidemiol. 2007, 22, 763–770. [Google Scholar] [CrossRef] [PubMed]
- Taylor, E.N.; Stampfer, M.J.; Mount, D.B.; Curhan, G.C. DASH-style diet and 24-hour urine composition. Clin. J. Am. Soc. Nephrol. 2010, 5, 2315–2322. [Google Scholar] [CrossRef]
- Nilson, E.A. The strides to reduce salt intake in Brazil: Have we done enough? Cardiovasc. Diagn. Ther. 2015, 5, 243. [Google Scholar]
- Angell, S.Y.; Yi, S.; Eisenhower, D.; Kerker, B.D.; Curtis, C.J.; Bartley, K.; Silver, L.D.; Farley, T.A. Sodium intake in a cross-sectional, representative sample of New York City adults. Am. J. Public Health 2014, 104, 2409–2416. [Google Scholar] [CrossRef]
- Nasreddine, L.; Akl, C.; Al-Shaar, L.; Almedawar, M.M.; Isma’eel, H. Consumer knowledge, attitudes and salt-related behavior in the Middle-East: The case of Lebanon. Nutrients 2014, 6, 5079–5102. [Google Scholar] [CrossRef]
- Claro, R.M.; Linders, H.; Ricardo, C.Z.; Legetic, B.; Campbell, N.R. Consumer attitudes, knowledge, and behavior related to salt consumption in sentinel countries of the Americas. Rev. Panam. Salud. Publica 2012, 32, 265–273. [Google Scholar] [CrossRef]
- World Health Organization. Mapping Salt Reduction Initiatives in the WHO European Region; WHO Regional Office for Europe: Copenhagen, Denmark, 2013. [Google Scholar]
- Berry, E.M.; Arnoni, Y.; Aviram, M. The Middle Eastern and biblical origins of the Mediterranean diet. Public Health Nutr. 2011, 14, 2288–2295. [Google Scholar] [CrossRef]
- La Verde, M.; Mulè, S.; Zappalà, G.; Privitera, G.; Maugeri, G.; Pecora, F.; Marranzano, M. Higher adherence to the Mediterranean diet is inversely associated with having hypertension: Is low salt intake a mediating factor? Int. J. Food Sci. Nutr. 2018, 69, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Magriplis, E.; Farajian, P.; Pounis, G.D.; Risvas, G.; Panagiotakos, D.B.; Zampelas, A. High sodium intake of children through ‘hidden’ food sources and its association with the Mediterranean diet: The GRECO study. J. Hypertens. 2011, 29, 1069–1076. [Google Scholar] [CrossRef] [PubMed]
| Inclusion | Exclusion |
|---|---|
| Age 20–65 | Renal or urinary pathology |
| Non-pregnant | Chronic disease |
| Non-lactating | Current menstrual period |
| No chronic kidney disease | 24-h urine volume <500 mL |
| No medical conditions | Urine creatinine <500 mg or >2000 mg |
| Not currently taking prescribed medications known to affect urine |
| Variable | Mean ± SD |
|---|---|
| Age (years) | 37.31 ± 12.5 |
| Weight (kg) | 73.37 ± 15.4 |
| Height (cm) | 165.8 ± 8.95 |
| Body Mass Index (BMI) | 26.7 ± 5.15 |
| N (%) | |
| Emirates 1 | |
| Abu Dhabi (West) | 137 (28.72) |
| Al-Ain (East) | 150 (31.45) |
| Northern Emirates 2 | 190 (39.83) |
| Age Category (years) | |
| 20–30 | 156 (32.70) |
| 31–40 | 113 (23.69) |
| 41–50 | 123 (25.78) |
| 51–65 | 85 (17.82) |
| BMI Classifications (WHO definition) | |
| Underweight (<18.5 kg/m2) | 15 (3.14) |
| Normal-weight (18.5–24.9 kg/m2) | 177 (37.11) |
| Overweight (25.0–29.9 kg/m2) | 172 (36.06) |
| Obese (30.0–34.9 kg/m2) | 113 (23.69) |
| Gender Distribution, N (%) | |
| Males | 214 (44.86) |
| Females | 263 (55.14) |
| Gender | Chi-Square (p-Value) | Age Category (Year) | Chi-Square (p-Value) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Do you Add Salt during Cooking (Missing Answers = 0) | Male N = 214 (%) | Female N = 263 (%) | Total N = 477 (%) | 20–30 N = 156 (%) | 31–40 N = 113 (%) | 41–50 N = 123 (%) | 51–65 N = 85 (%) | ||
| Never | 46 (21.6) | 38 (14.1) | 84 (17.5) | 5.60 (0.061) | 28 (18.0) | 26 (23.0) | 13 (10.6) | 17 (19.0) | 20.01 (0.01) |
| Sometimes | 80 (37.6) | 96 (36.6) | 176 (37.1) | 65 (41.7) | 42 (37.2) | 46 (37.4) | 23 (27.4) | ||
| Always | 88 (40.8) | 129 (49.2) | 217 (45.5) | 63 (40.4) | 45 (39.8) | 64 (52.0) | 45 (54.2) | ||
| Do you Add Salt to Food at the Table (Missing Answers = 1) | Male N (%) | Female N (%) | Total N = 476 N (%) | Chi-Square (p-Value) | 20–30 N (%) | 31–40 N (%) | 41–50 N (%) | 51–65 N (%) | Chi-Square (p-Value) |
| Never | 71 (33.3) | 90 (34.4) | 161 (33.8) | 2.12 (0.548) | 54 (34.6) | 31 (27.4) | 40 (32.8) | 36 (42.8) | 12.71 (0.391) |
| Sometimes | 93 (43.7) | 122 (46.60 | 215 (45.2) | 75 (48.1) | 53 (46.9) | 51 (41.8) | 36 (42.8) | ||
| Always | 49 (23.0) | 51 (19.0) | 100 (21.0) | 27 (17.3) | 29 (25.7) | 31 (25.4) | 13 (14.3) | ||
| Do you Use Stock Cubes during Cooking (Missing Answers = 0) | Male N (%) | Female N (%) | Total N = 477 N (%) | Chi-Square (p-Value) | 20–30 N (%) | 31–40 N (%) | 41–50 N (%) | 51–65 N (%) | Chi-Square (p-Value) |
| Never | 55 (25.8) | 76 (28.6) | 131 (27.4) | 0.50 (0.779) | 39 (25.0) | 30 (26.6) | 33 (26.8) | 29 (34.1) | 4.65 (0.794) |
| Sometimes | 61 (28.6) | 74 (28.2) | 135 (28.4) | 42 (26.9) | 35 (31.0) | 36 (29.2) | 22 (25.9) | ||
| Always | 98 (45.5) | 113 (43.1) | 211 (44.2) | 75 (48.1) | 48 (42.5) | 54 (44.0) | 34 (40.0) | ||
| How Much Salt do you Think you Consume (Missing Answers = 0) | Male N (%) | Female N (%) | Total N = 477 N (%) | Chi-Square (p-Value) | 20–30 N (%) | 31–40 N (%) | 41–50 N (%) | 51–65 N (%) | Chi-Square (p-Value) |
| Too much | 49 (23.0) | 47 (17.6) | 96 (20.0) | 2.85 (0.240) | 32 (20.5) | 26 (23.0) | 22 (18.0) | 16 (19.1) | 3.101 (0.928) |
| Just the right amount | 125 (58.2) | 171 (65.3) | 296 (62.1) | 96 (61.5) | 70 (62.0) | 80 (65.0) | 50 (59.5) | ||
| Far too little | 40 (18.8) | 45 (17.2) | 85 (17.9) | 28 (17.9) | 17 (15.0) | 21 (17.0) | 19 (21.4) | ||
| Do you Think that High Salt Diet could Cause Serious Health Problems? (Missing Answers = 0) | Male N (%) | Female N (%) | Total N = 477 N (%) | Chi-Square (p-Value) | 20–30 N (%) | 31–40 N (%) | 41–50 N (%) | 51–65 N (%) | Chi-Square (p-Value) |
| Yes | 149 (69.6) | 181 (68.8) | 330 (69.1) | 3.682 (0.158) | 113 (72.4) | 73 (64.6) | 84 (68.4) | 60 (70.0) | 4.782 (0.780) |
| No | 45 (21.0) | 68 (25.8) | 113 (23.7) | 32 (20.6) | 32 (28.3) | 31 (25.2) | 18 (23.7) | ||
| Don’t know | 20 (9.3) | 14 (5.4) | 34 (7.2) | 11 (7.1) | 8 (7.1) | 8 (6.56) | 7 (8.4) | ||
| What are the Health Problems Associated with High Salt Intake * | Male N (%) | Female N (%) | Total N = 477N (%) | Chi-Square (p-Value) | 20–30 N (%) | 31–40 N (%) | 41–50 N (%) | 51–65 N (%) | Chi-Square (p-Value) |
| High blood pressure | 90 (42.1) | 126 (47.9) | 216 (45.2) | 3.43 (0.414) | 73 (46.8) | 47 (41.6) | 59 (48.0) | 37 (43.5) | 4.23 (0.624) |
| Kidney stones | 43 (20.1) | 46 (17.5) | 89 (18.7) | 31 (19.9) | 22 (19.5) | 21 (17.1) | 15 (17.6) | ||
| Obesity | 38 (17.8) | 47 (17.9) | 85 (17.8) | 25 (16.0) | 23 (20.3) | 18 (14.6) | 19 (22.3) | ||
| Diabetes | 18 (8.4) | 13 (4.9) | 31 (6.5) | 8 (5.1) | 9 (8.0) | 8 (6.5) | 6 (7.1) | ||
| Heart disease | 25 (11.7) | 31 (11.8) | 56 (11.7) | 19 (12.2) | 12 (10.6) | 17 (13.8) | 8 (9.4) | ||
| Do you Think Processed Foods are High in Sodium? (Missing Answers = 0) | Male N (%) | Female N (%) | Total N = 477 (%) | Chi-Square (p-Value) | 20–30 N (%) | 31–40 N (%) | 41–50 N (%) | 51–65 N (%) | Chi-Square (p-Value) |
| Yes | 159 (74.2) | 207 (78.6) | 366 (76.7) | 1.620 (0.444) | 123 (78.9) | 88 (77.9) | 88 (71.5) | 68 (80.0) | 6.578 (0.574) |
| No | 55 (25.8) | 56 (21.4) | 111 (23.3) | 33 (21.1) | 25 (22.1) | 35 (28.5) | 17 (20.0) | ||
| Do you do Anything on a Regular Basis to Control your Salt or Sodium Intake? (Missing Answers = 0) | Male N (%) | Female N (%) | Total N = 477 (%) | Chi-Square (p-Value) | 20–30 N (%) | 31–40 N (%) | 41–50 N (%) | 51–65 N (%) | Chi-Square (p-Value) |
| Yes | 131 (61.2) | 158 (60.1) | 289 (60.6) | 0.935 (0.626) | 88 (56.4) | 69 (61.1) | 76 (61.8) | 56 (65.9) | 4.823 (0.764) |
| No | 83 (38.8) | 105 (39.9) | 188 (39.4) | 68 (43.6) | 44 (38.9) | 47 (38.2) | 29 (34.1) | ||
| Nutrients | Mean ± SD | Recommendation | p-Value |
|---|---|---|---|
| Mean 24-h sodium excretion in urine (mg) | 2713.40 ± 713 | <2300 mg | <0.001 |
| Mean 24-h potassium excretion in urine (mg) | 1803.30 ± 618.03 | >3510 mg | <0.001 |
| Mean 24-h creatinine excretion in urine (mg) | 1284.81 ± 607.0 | ||
| Mean 24-h creatinine (mg/kg body mass) | 16.83 ± 4.84 | ||
| Mean 24-h creatinine (mg/kg body mass)—female | 13.42 ± 1.95 | ||
| Mean 24-h creatinine (mg/kg body mass)—male | 21.81 ± 3.80 | ||
| Mean 24-h urinary Na/K ratio | 1.64 ± 0.55 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jarrar, A.H.; Stojanovska, L.; Apostolopoulos, V.; Cheikh Ismail, L.; Feehan, J.; Ohuma, E.O.; Ahmad, A.Z.; Alnoaimi, A.A.; Al Khaili, L.S.; Allowch, N.H.; et al. Assessment of Sodium Knowledge and Urinary Sodium Excretion among Regions of the United Arab Emirates: A Cross-Sectional Study. Nutrients 2020, 12, 2747. https://doi.org/10.3390/nu12092747
Jarrar AH, Stojanovska L, Apostolopoulos V, Cheikh Ismail L, Feehan J, Ohuma EO, Ahmad AZ, Alnoaimi AA, Al Khaili LS, Allowch NH, et al. Assessment of Sodium Knowledge and Urinary Sodium Excretion among Regions of the United Arab Emirates: A Cross-Sectional Study. Nutrients. 2020; 12(9):2747. https://doi.org/10.3390/nu12092747
Chicago/Turabian StyleJarrar, Amjad H., Lily Stojanovska, Vasso Apostolopoulos, Leila Cheikh Ismail, Jack Feehan, Eric O. Ohuma, Ala Z. Ahmad, Asma A. Alnoaimi, Latifa S. Al Khaili, Najah H. Allowch, and et al. 2020. "Assessment of Sodium Knowledge and Urinary Sodium Excretion among Regions of the United Arab Emirates: A Cross-Sectional Study" Nutrients 12, no. 9: 2747. https://doi.org/10.3390/nu12092747
APA StyleJarrar, A. H., Stojanovska, L., Apostolopoulos, V., Cheikh Ismail, L., Feehan, J., Ohuma, E. O., Ahmad, A. Z., Alnoaimi, A. A., Al Khaili, L. S., Allowch, N. H., Meqbaali, F. T. A., Souka, U., & Al Dhaheri, A. S. (2020). Assessment of Sodium Knowledge and Urinary Sodium Excretion among Regions of the United Arab Emirates: A Cross-Sectional Study. Nutrients, 12(9), 2747. https://doi.org/10.3390/nu12092747











