Impact of a Three-Year Obesity Prevention Study on Healthy Behaviors and BMI among Lebanese Schoolchildren: Findings from Ajyal Salima Program
Abstract
1. Introduction
2. Materials and Methods
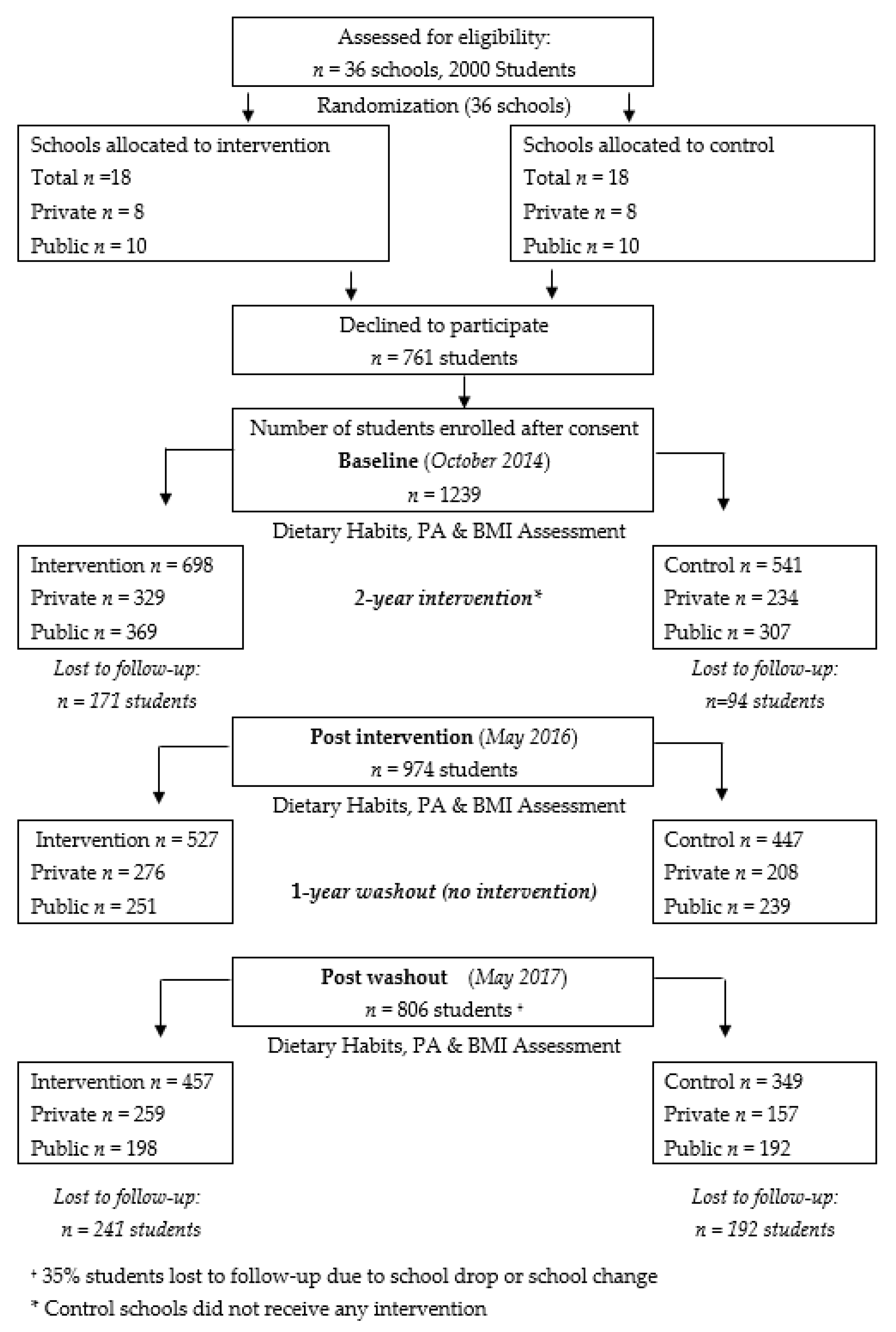
2.1. Participants, Recruitment and Procedures
2.2. Ethics Approval and Consent to Participate
2.3. Data Collection
2.4. Process Evaluation
2.5. Intervention Design
2.6. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Impact of Intervention on Body Mass Index (BMI) and Obesity
3.3. Impact of Intervention on Dietary Habits
3.4. Impact of Intervention on Physical Activity
3.5. Impact of Intervention on Knowledge and Self-Efficacy
3.6. Process Evaluation Outcomes
- Classroom activities: during the first year, the program was delivered as designed in both public and private schools. The 12 educational lessons and activities were all implemented in the intervention schools along with meetings with parents and the food service management. In the second year, the commitment of teachers in private schools decreased, thus reducing both the reach and dose received by the students; while it remained constant in public schools given the adoption of the program by the Ministry of Education.
- School shop: amendments at the school shops level were more successful in public schools, since the MEHE has issued a ministerial order regulating the type of snacks and drinks to be sold. The sale of energy dense snacks (e.g., chips, donuts, croissant, hot dogs, sweet and soft drinks) was banned while the sale of healthy food choices (e.g., fruits and vegetables, popcorn, 100% juice, nuts, dried fruits, sandwiches) were mandated. The implementation was less successful in private schools where the ministerial order was not mandatory and the school shop owners were primarily revenue-oriented.
- Parental involvement: parents’ attendance at meetings was impacted by various factors, namely when both parents worked, and when younger children were still at home. Parents’ presence was enhanced when they were given a direct motivation such as an invitation to a breakfast meal.
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Tenfold increase in childhood and adolescent obesity in four decades: New study by Imperial College London and WHO. Saudi Med. J. 2017, 38, 1162–1163. [Google Scholar]
- WHO. Consideration of the Evidence on Childhood Obesity for the Commission on Ending Childhood Obesity: Report of the Ad Hoc Working Group on Science and Evidence for Ending Childhood Obesity; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Nasreddine, L.; Naja, F.; Chamieh, M.C.; Adra, N.; Sibai, A.-M.; Hwalla, N. Trends in overweight and obesity in Lebanon: Evidence from two national cross-sectional surveys (1997 and 2009). BMC Public Health 2012, 12, 798. [Google Scholar] [CrossRef] [PubMed]
- Kac, G.; Pérez-Escamilla, R. Nutrition transition and obesity prevention through the life-course. Int. J. Obes. Suppl. 2013, 3, S6–S8. [Google Scholar] [CrossRef] [PubMed]
- FAO. The State of Food and Agriculture: Paying Farmers for Environmental Services; FAO: Rome, Italy, 2007. [Google Scholar]
- Naja, F.; Hwalla, N.; Itani, L.; Karam, S.; Sibai, A.M.; Nasreddine, L. A Western dietary pattern is associated with overweight and obesity in a national sample of Lebanese adolescents (13–19 years): A cross-sectional study. Br. J. Nutr. 2015, 114, 1909–1919. [Google Scholar] [CrossRef] [PubMed]
- Fazah, A.; Jacob, C.; Moussa, E.; El-Hage, R.; Youssef, H.; Delamarche, P. Activity, inactivity and quality of life among Lebanese adolescents. Pediatr. Int. 2010, 52, 573–578. [Google Scholar] [CrossRef] [PubMed]
- Ickes, M.J.; McMullen, J.; Haider, T.; Sharma, M. Global school-based childhood obesity interventions: A review. Int. J. Environ. Res. Public Health 2014, 11, 8940–8961. [Google Scholar] [CrossRef]
- Liu, Z.; Xu, H.M.; Wen, L.M.; Peng, Y.Z.; Lin, L.Z.; Zhou, S.; Li, W.H.; Wang, H.J. A systematic review and meta-analysis of the overall effects of school-based obesity prevention interventions and effect differences by intervention components. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 95. [Google Scholar] [CrossRef]
- Brown, T.; Moore, T.H.M.; Hooper, L.; Gao, Y.; Zayegh, A.; Ijaz, S.; Elwenspoek, M.; Foxen, S.C.; Magee, L.; O’Malley, C.; et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2019. [Google Scholar] [CrossRef]
- Bleich, S.N.; Vercammen, K.A.; Zatz, L.Y.; Frelier, J.M.; Ebbeling, C.B.; Peeters, A. Interventions to prevent global childhood overweight and obesity: A systematic review. Lancet Diabetes Endocrinol. 2018, 6, 332–346. [Google Scholar] [CrossRef]
- Cauchi, D.; Glonti, K.; Petticrew, M.; Knai, C. Environmental components of childhood obesity prevention interventions: An overview of systematic reviews. Obes. Rev. 2016, 17, 1116–1130. [Google Scholar] [CrossRef]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national Preval. of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Habib-Mourad, C.; Ghandour, L.A.; Moore, H.J.; Nabhani-Zeidan, M.; Adetayo, K.; Hwalla, N.; Summerbell, C. Promoting healthy eating and physical activity among school children: Findings from Health-E-PALS, the first pilot intervention from Lebanon. BMC Public Health 2014, 14, 940. [Google Scholar] [CrossRef] [PubMed]
- Sobol-Goldberg, S.; Rabinowitz, J.; Gross, R. School-based obesity prevention programs: A meta-analysis of randomized controlled trials. Obesity 2013, 21, 2422–2428. [Google Scholar] [CrossRef] [PubMed]
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr. Suppl. 2006, 450, 76. [Google Scholar]
- Sibai, A.M.; Hwalla, N.; Adra, N.; Rahal, B. Prevalence and covariates of obesity in Lebanon: Findings from the first epidemiological study. Obes. Res. 2003, 11, 1353–1361. [Google Scholar] [CrossRef]
- MyPlate | ChooseMyPlate. Available online: https://www.choosemyplate.gov/ (accessed on 15 January 2020).
- Bandura, A. Health promotion by social cognitive means. Health Educ. Behav. 2004, 31, 143–164. [Google Scholar] [CrossRef]
- Herrin, J. CLTEST: Stata modules for performing cluster-adjusted chi-square and t-tests. EconPapers 2012. [Google Scholar]
- Waters, E.; Gibbs, L.; Tadic, M.; Ukoumunne, O.C.; Magarey, A.; Okely, A.D.; de Silva, A.; Armit, C.; Green, J.; O’Connor, T.; et al. Cluster randomised trial of a school-community child health promotion and obesity prevention intervention: Findings from the evaluation of fun ‘n healthy in Moreland! BMC Public Health 2017, 18, 92. [Google Scholar] [CrossRef]
- Cao, Z.J.; Wang, S.M.; Chen, Y. A randomized trial of multiple interventions for childhood obesity in China. Am. J. Prev Med. 2015, 48, 552–560. [Google Scholar] [CrossRef]
- Verjans-Janssen, S.R.B.; van de Kolk, I.; Van Kann, D.H.H.; Kremers, S.P.J.; Gerards, S. Effectiveness of school-based physical activity and nutrition interventions with direct parental involvement on children’s BMI and energy balance-related behaviors—A systematic review. PLoS ONE 2018, 13, e0204560. [Google Scholar] [CrossRef]
- Andrade, S.; Lachat, C.; Ochoa-Aviles, A.; Verstraeten, R.; Huybregts, L.; Roberfroid, D.; Andrade, D.; Camp, J.V.; Rojas, R.; Donoso, S.; et al. A school-based intervention improves physical fitness in Ecuadorian adolescents: A cluster-randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 153. [Google Scholar] [CrossRef] [PubMed]
- Parise, I. The built environment and obesity: You are where you live. Built Environ. 2020, 49, 226–230. [Google Scholar] [CrossRef] [PubMed]
- Chacar, H.R.; Salameh, P. Public schools adolescents’ obesity and growth curves in Lebanon. J. Med. Liban 2011, 59, 80–88. [Google Scholar]
- Youssef, H.; Zind, M.; Garnier, S.; Fazah, A.; Jacob, C.; Moussa, E.; Gratas-Delamarche, A.; Groussard, C. Overweight and Obesity Related Factors among Lebanese Adolescents: An Explanation for Gender and Socioeconomic Differences. Epidemiology 2017, 7, 300. [Google Scholar] [CrossRef]
- Scherr, R.E.; Linnell, J.D.; Dharmar, M.; Beccarelli, L.M.; Bergman, J.J.; Briggs, M.; Brian, K.M.; Feenstra, G.; Hillhouse, J.C.; Keen, C.L.; et al. A Multicomponent, School-Based Intervention, the Shaping Healthy Choices Program, Improves Nutrition-Related Outcomes. J. Nutr. Educ. Behav. 2017, 49, 368–379. [Google Scholar] [CrossRef] [PubMed]
- Fung, C.; Kuhle, S.; Lu, C.; Purcell, M.; Schwartz, M.; Storey, K.; Veugelers, P.J. From “best practice” to “next practice”: The effectiveness of school-based health promotion in improving healthy eating and physical activity and preventing childhood obesity. Int. J. Behav Nutr Phys. Act. 2012, 9, 27. [Google Scholar] [CrossRef]
- Veugelers, P.J.; Fitzgerald, A.L. Effectiveness of school programs in preventing childhood obesity: A multilevel comparison. Am. J. Public Health 2005, 95, 432–435. [Google Scholar] [CrossRef]
- Stelmach-Mardas, M.; Rodacki, T.; Dobrowolska-Iwanek, J.; Brzozowska, A.; Walkowiak, J.; Wojtanowska-Krosniak, A.; Zagrodzki, P.; Bechthold, A.; Mardas, M.; Boeing, H. Link between Food Energy Density and Body Weight Changes in Obese Adults. Nutrients 2016, 8, 229. [Google Scholar] [CrossRef]
- Driessen, C.E.; Cameron, A.J.; Thornton, L.E.; Lai, S.K.; Barnett, L.M. Effect of changes to the school food environment on eating behaviours and/or body weight in children: A systematic review. Obes. Rev. 2014, 15, 968–982. [Google Scholar] [CrossRef]
- Story, M.; Nanney, M.S.; Schwartz, M.B. Schools and obesity prevention: Creating school environments and policies to promote healthy eating and physical activity. Milbank Q. 2009, 87, 71–100. [Google Scholar] [CrossRef]
- Jansen, W.; Borsboom, G.; Meima, A.; Zwanenburg, E.J.; Mackenbach, J.P.; Raat, H.; Brug, J. Effectiveness of a primary school-based intervention to reduce overweight. Int. J. Pediatr. Obes. 2011, 6, e70–e77. [Google Scholar] [CrossRef] [PubMed]
- Sigmund, E.; El Ansari, W.; Sigmundová, D. Does school-based physical activity decrease overweight and obesity in children aged 6–9 years? A two-year non-randomized longitudinal intervention study in the Czech Republic. BMC Public Health 2012, 12, 570. [Google Scholar] [CrossRef] [PubMed]
- Van Kann, D.H.H.; Kremers, S.P.J.; de Vries, N.K.; de Vries, S.I.; Jansen, M.W.J. The effect of a school-centered multicomponent intervention on daily physical activity and sedentary behavior in primary school children: The Active Living study. Prev. Med. 2016, 89, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Althouse, A.D. Adjust for Multiple Comparisons? It’s Not That Simple. Ann. Thorac. Surg. 2016, 101, 1644–1645. [Google Scholar] [CrossRef]
| Total Sample | Intervention | Control | p-Value * | |
|---|---|---|---|---|
| No. of students | 1239 | 698 | 541 | |
| Mean Age (yrs.) | 9.95 ± 1.13 | 9.81 ± 0.68 | 10.13 ± 0.68 | <0.01 |
| n (%) | ||||
| Gender: | 0.165 | |||
| Male | 574 (46.3) | 311 (54.2) | 263 (45.8) | |
| Female | 666 (53.7) | 387 (58.1) | 279 (41.9) | |
| Type of school: | 0.185 | |||
| Private schools † | 564 (45.5) | 329 (47.1) | 235 (43.4) | |
| Public schools † | 676 (54.5) | 369 (52.9) | 307 (56.6) | |
| Body mass index (BMI): | 0.235 | |||
| Normal | 737 (59.5) | 400 (57.3) | 337 (62.3) | |
| At risk | 281 (22.7) | 161 (23.1) | 120 (22.2) | |
| Overweight | 181 (14.6) | 112 (16) | 69 (12.8) | |
| Obese | 40 (3.2) | 25 (3.6) | 15 (2.8) | |
| Dietary and physical activity (PA) habits: | ||||
| Fruits consumption § | 883 (71.9) | 485 (54.9) | 398 (45.1) | 0.129 |
| Raw vegetables consumption § | 809 (65.6) | 467 (57.7) | 342 (42.3) | 0.137 |
| Having chips § | 695 (56.4) | 425 (61.2) | 270 (38.8) | <0.001 |
| Drinking soft drinks § | 744 (60.4) | 425 (57.1) | 319 (42.9) | 0.404 |
| Drinking sweet drinks § | 559 (45.4) | 317 (56.7) | 242 (43.3) | 0.808 |
| Exercise after school §§ | 483 (39.2) | 274 (56.7) | 209 (43.3) | 0.697 |
| Post Intervention N = 974 Mean ± SE | After 1 Year Washout N = 806 Mean ± SE | |||||
|---|---|---|---|---|---|---|
| Intervention N = 527 | Control N = 447 | p-Value * | Intervention N = 457 | Control N = 349 | p-Value * | |
| Total sample | 0.07 ± 0.047 | 0.145 ± 0.048 | 0.272 | 0.134 ± 0.048 | 0.237 ± 0.054 | 0.1623 |
| Private schools† | 0.112 ± 0.072 | 0.136 ± 0.073 | 0.8136 | 0.111 ± 0.072 | 0.141 ± 0.083 | 0.795 |
| Public schools† | 0.024 ± 0.063 | 0.152 ± 0.065 | 0.1713 | 0.164 ± 0.065 | 0.316 ± 0.066 | 0.1165 |
| OR (95% CI) Post Intervention n = 974 | p-Value * | OR (95% CI) after 1-Year Washout n = 806 | p-Value * | |
|---|---|---|---|---|
| Total | 1.35 (0.77; 2.36) | 0.284 | 0.79 (0.47; 1.32) | 0.373 |
| Private schools† | 1.39 (0.71; 2.70) | 0.333 | 1.17 (0.75; 1.83) | 0.49 |
| Public schools† | 1.28 (0.53; 3.10) | 0.58 | 0.48 (0.26; 0.88) | 0.018 |
| OR (95% CI) Post Intervention n = 974 | p-Value * | OR (95% CI) after 1-Year Washout n = 806 | p-Value * | |
|---|---|---|---|---|
| Fruits consumption § | ||||
| Total sample | 1.56 (1.18; 2.08) | 0.002 | 1.28 (0.99; 1.65) | 0.054 |
| Private schools † | 1.84 (1.30; 2.60) | 0.001 | 1.04 (0.76; 1.43) | 0.770 |
| Public schools † | 1.44 (0.89; 2.32) | 0.135 | 1.66 (1.14; 2.42) | 0.008 |
| Raw Veggies consumption § | ||||
| Total sample | 1.79 (1.32; 2.43) | 0.000 | 1.66 (1.25; 2.19) | 0.000 |
| Private schools † | 2.32 (1.42; 3.80) | 0.001 | 1.33 (0.90; 1.95) | 0.141 |
| Public schools † | 1.47 (0.95; 2.28) | 0.082 | 2.19 (1.59; 3.01) | 0.000 |
| Having chips § | ||||
| Total sample | 0.52 (0.32; 0.84) | 0.008 | 0.86 (0.58; 1.26) | 0.493 |
| Private schools † | 0.59 (0.32; 1.11) | 0.103 | 1.08 (0.62; 1.92) | 0.776 |
| Public schools † | 0.44 (0.24; 0.8) | 0.007 | 0.70 (0.49; 1.02) | 0.060 |
| Drinking soft drinks § | ||||
| Total sample | 0.64 (0.42; 0.95) | 0.027 | 0.68 (0.48; 0.97) | 0.031 |
| Private schools † | 0.66 (0.36; 1.23) | 0.190 | 0.69 (0.39; 1.23) | 0.213 |
| Public schools † | 0.59 (0.34; 1.02) | 0.057 | 0.68 (0.44; 1.05) | 0.081 |
| Drinking sweet drinks § | ||||
| Total sample | 0.62 (0.40; 0.96) | 0.032 | 0.71 (0.47; 1.07) | 0.104 |
| Private schools † | 0.58 (0.28; 1.19) | 0.136 | 0.90 (0.48; 1.69) | 0.752 |
| Public schools † | 0.63 (0.37; 1.07) | 0.087 | 0.62 (0.39; 1.00) | 0.048 |
| Exercise after school §§ | ||||
| Total sample | 1.25 (0.87; 1.80) | 0.225 | 1.39 (1.00; 1.92) | 0.044 |
| Private schools † | 1.07 (0.64; 1.78) | 0.782 | 1.47 (0.94; 2.30) | 0.087 |
| Public schools † | 1.44 (0.87; 2.41) | 0.154 | 1.27 (0.77; 2.09) | 0.330 |
| Post Intervention | p Value * | After 1-Year Washout | p Value * | |||
|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | |||
| n = 528 | n = 448 | n = 457 | n = 349 | |||
| Mean Difference (95% CI) | Mean Difference (95% CI) | |||||
| Knowledge score | ||||||
| Total sample | 3.13 (2.80; 3.46) | 1.37 (1.02; 1.71) | <0.001 | 2.84 (2.47; 3.20) | 1.57 (1.16; 1.98) | <0.001 |
| Private schools † | 2.87 (2.29; 3.45) | 1.16 (0.57; 1.75) | <0.001 | 2.44 (1.83; 3.04) | 1.31 (0.56; 2.05) | 0.014 |
| Public schools † | 3.41 (3.01; 3.81) | 1.54 (1.13; 1.95) | <0.001 | 3.35 (2.91; 3.79) | 1.78 (1.33; 2.23) | <0.001 |
| Self-efficacy score | ||||||
| Total sample | 1.16 (0.76; 1.56) | 0.29 (−0.13; 0.70) | 0.003 | 0.68 (0.17; 1.20) | −0.12 (0.69; 0.43) | 0.031 |
| Private schools † | 1.15 (0.68; 1.62) | 0.51 (−0.01; 1.03) | 0.050 | 0.44 (−0.13; 1.01) | 0.33 (−0.39; 1.05) | 0.779 |
| Public schools † | 1.17 (0.45; 1.89) | 0.09 (−0.65; 0.83) | 0.030 | 1.00 (0.12; 1.88) | −0.50 (−1.43; 0.42) | 0.016 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Habib-Mourad, C.; Ghandour, L.A.; Maliha, C.; Dagher, M.; Kharroubi, S.; Hwalla, N. Impact of a Three-Year Obesity Prevention Study on Healthy Behaviors and BMI among Lebanese Schoolchildren: Findings from Ajyal Salima Program. Nutrients 2020, 12, 2687. https://doi.org/10.3390/nu12092687
Habib-Mourad C, Ghandour LA, Maliha C, Dagher M, Kharroubi S, Hwalla N. Impact of a Three-Year Obesity Prevention Study on Healthy Behaviors and BMI among Lebanese Schoolchildren: Findings from Ajyal Salima Program. Nutrients. 2020; 12(9):2687. https://doi.org/10.3390/nu12092687
Chicago/Turabian StyleHabib-Mourad, Carla, Lilian A. Ghandour, Carla Maliha, Michèle Dagher, Samer Kharroubi, and Nahla Hwalla. 2020. "Impact of a Three-Year Obesity Prevention Study on Healthy Behaviors and BMI among Lebanese Schoolchildren: Findings from Ajyal Salima Program" Nutrients 12, no. 9: 2687. https://doi.org/10.3390/nu12092687
APA StyleHabib-Mourad, C., Ghandour, L. A., Maliha, C., Dagher, M., Kharroubi, S., & Hwalla, N. (2020). Impact of a Three-Year Obesity Prevention Study on Healthy Behaviors and BMI among Lebanese Schoolchildren: Findings from Ajyal Salima Program. Nutrients, 12(9), 2687. https://doi.org/10.3390/nu12092687





