Association between Bone Turnover Markers, Leptin, and Nutritional Status in Girls with Adolescent Idiopathic Scoliosis (AIS)
Abstract
1. Introduction
2. Materials and Methods
2.1. Studied Population
2.2. The Evaluation of the Scoliotic Curve Magnitude
2.3. Anthropometric Parameters
2.4. Body Composition Analysis
2.5. Biochemical Analysis
2.6. Ethical Considerations
2.7. Statistical Analysis
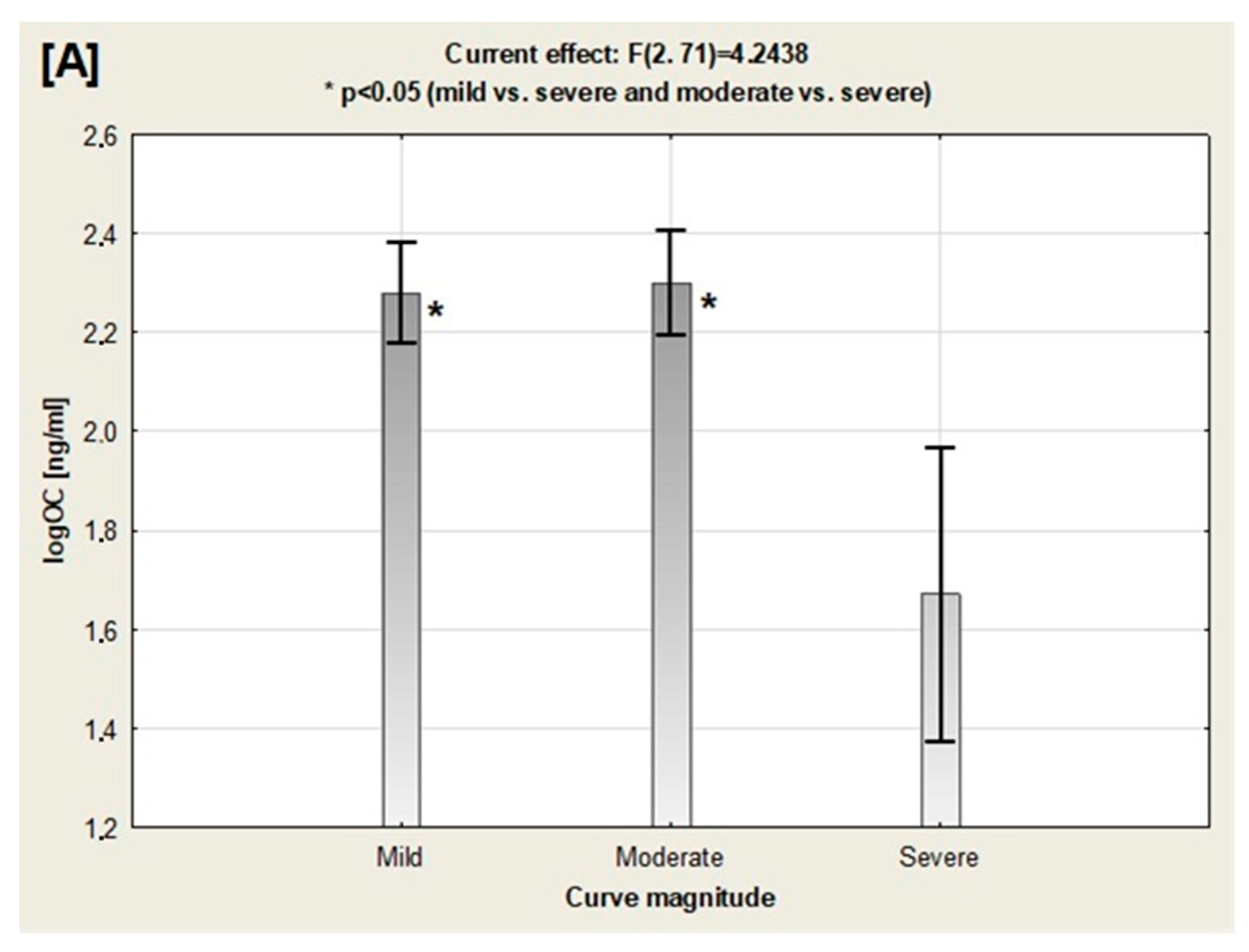
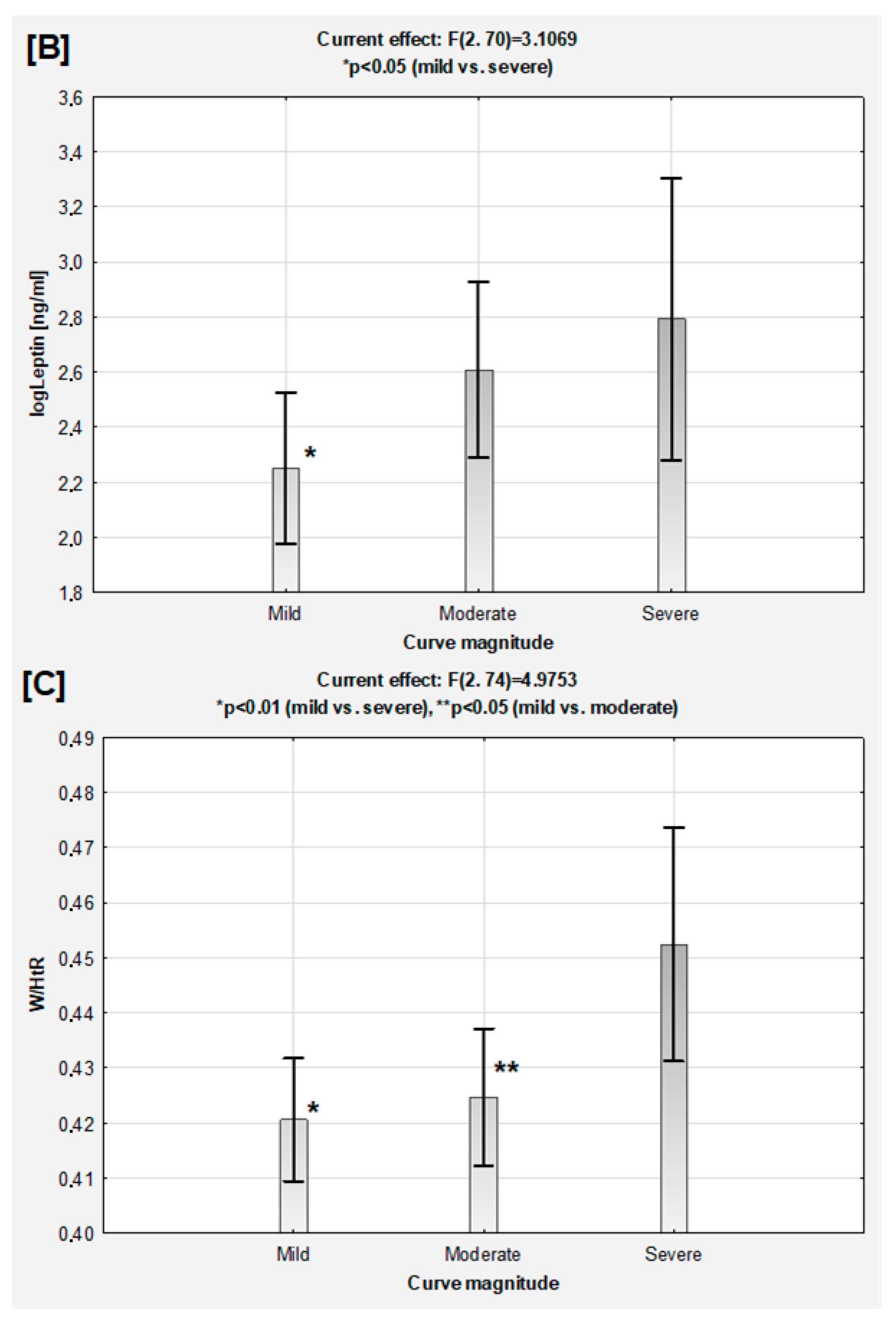
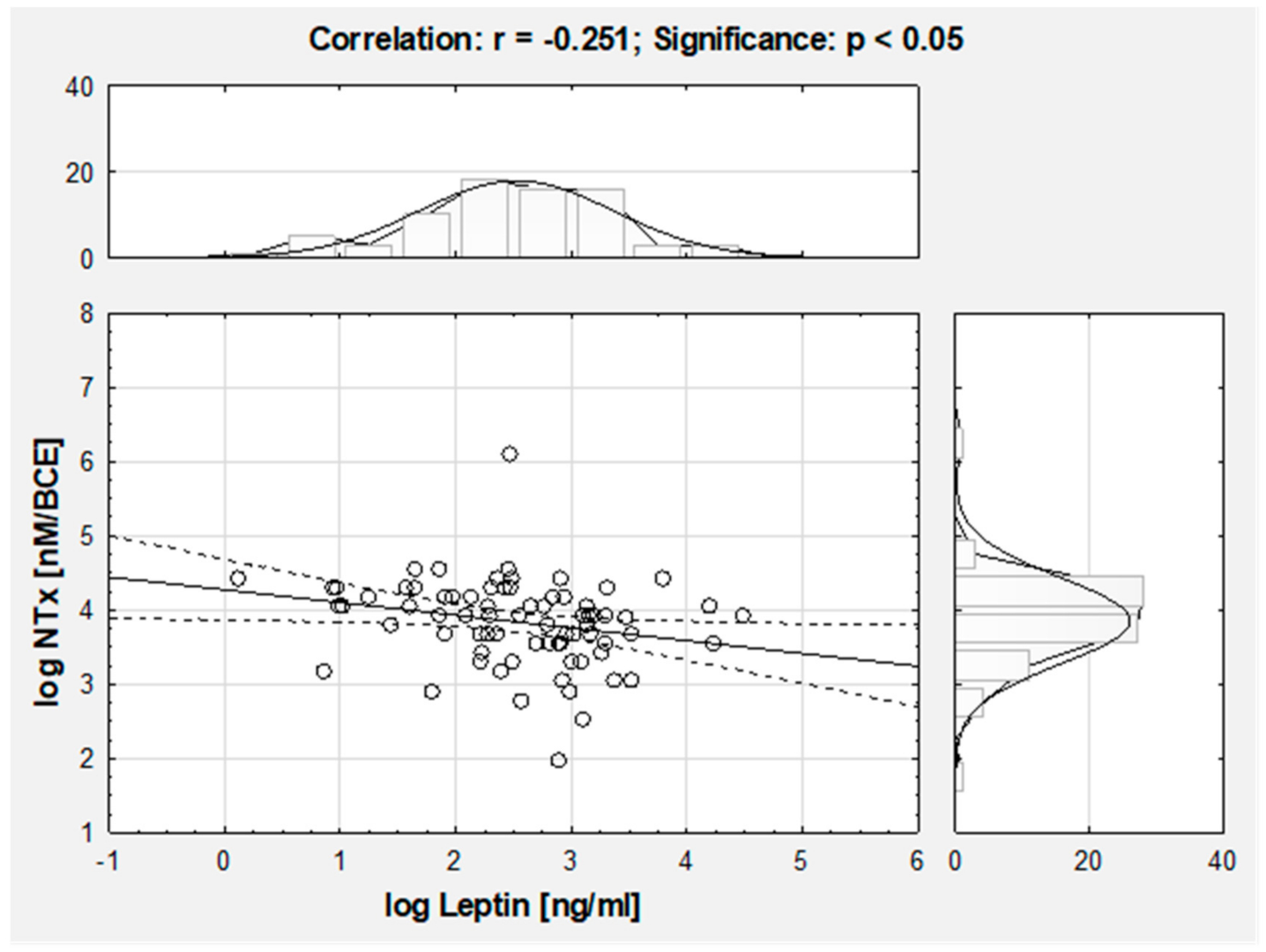
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Burwell, G.R.; Aujla, R.K.; Grevitt, M.; Dangerfield, P.H.; Moulton, A.; Randell, T.; Anderson, S. Pathogenesis of adolescent idiopathic scoliosis in girls—A double neuro-osseous theory-involving disharmony between two nervous systems, somatic and autonomic expressed in the spine and hormones with implications for medical therapy. Scoliosis 2009, 4, 29. [Google Scholar] [CrossRef]
- Mao, S.-H.; Jiang, J.; Sun, X.; Zhao, Q.; Qian, B.-P.; Liu, Z.; Shu, H.; Qiu, Y. Timing of menarche in Chinese girls with and without adolescent idiopathic scoliosis: Current results and review of the literature. Eur. Spine J. 2011, 20, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Y.; Sun, X.; Qiu, X.; Li, W.; Zhu, Z.; Zhu, F.; Wang, B.; Yü, Y.; Qian, B. Decreased circulating leptin level and its association with body and bone mass in girls with adolescent idiopathic scoliosis. Spine 2007, 32, 2703–2710. [Google Scholar] [CrossRef] [PubMed]
- Burwell, R.G.; Aujla, R.K.; Kirby, A.S.; Dangerfield, P.H.; Moulton, A.; Cole, A.; Polak, F.J.; Pratt, R.K.; Webb, J.K. Body mass index of girls in health influences menarche and skeletal maturation: A leptin-sympathetic nervous system focuses on the trunk with hypothalamic asymmetric dysfunction in the pathogenesis of adolescent idiopathic scoliosis? Stud. Health Technol. Inform. 2008, 140, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Nicolopoulos, K.S.; Burwell, R.G.; Webb, J.K. Stature and its components in adolescent idiopathic scoliosis. Cephalo-caudal disproportion in the trunk in girls. J. Bone Joint Surg. Br. 1985, 67, 594–601. [Google Scholar] [CrossRef]
- Burwell, R.G.; Dangerfield, P.H.; Moulton, A.; Anderson, S.I. Etiologic theories of idiopathic scoliosis: Autonomic nervous system and the leptin-sympathetic nervous system concept for the pathogenesis of adolescent idiopathic scoliosis. Stud. Health Technol. Inform. 2008, 140, 197–207. [Google Scholar] [CrossRef]
- Burwell, R.G.; Dangerfield, P.H.; Moulton, A.; Grivas, T.B.; Cheng, J.C.Y. Whither the etiopathogenesis (and scoliogeny) of adolescent idiopathic scoliosis? Incorporating presentations on scoliogeny at the 2012 IRSSD and SRS meetings. Scoliosis 2013, 8. [Google Scholar] [CrossRef]
- Schlosser, T.P.C.; van der Heijden, G.J.M.G.; Versteeg, A.L.; Castelein, R.M. How ‘idiopathic’ is adolescent idiopathic scoliosis? A systematic review on associated abnormalities. PLoS ONE 2014, 9, e97461. [Google Scholar] [CrossRef]
- Cheung, C.S.K.; Lee, W.T.K.; Tse, Y.K.; Tang, S.P.; Lee, K.M.; Guo, X.; Qin, L.; Cheng, J. Abnormal peri-pubertal anthropometric measurements and growth pattern in adolescent idiopathic scoliosis: A study of 598 patients. Spine 2003, 28, 2152–2157. [Google Scholar] [CrossRef]
- Li, X.F.; Li, H.; Liu, Z.D.; Dai, L.Y. Low bone mineral status in adolescent idiopathic scoliosis. Eur. Spine J. 2008, 17, 1431–1440. [Google Scholar] [CrossRef]
- Cheung, C.S.K.; Lee, W.T.K.; Tse, Y.K.; Lee, K.M.; Guo, X.; Qin, L.; Cheng, J. Generalized osteopenia in adolescent idiopathic scoliosis-association with abnormal pubertal growth, bone turnover, and calcium intake? Spine 2006, 31, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.T.; Cheung, C.S.; Tse, Y.K.; Guo, X.; Qin, L.; Ho, S.C.; Lau, J.; Cheng, J.C. Generalized low bone mass of girls with adolescent idiopathic scoliosis is related to inadequate calcium intake and weight bearing physical activity in peripubertal period. Osteoporos. Int. 2005, 16, 1024–1035. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.S.; Chan, K.Y.; Yu, F.W.; Yeung, H.Y.; Ng, B.K.; Lee, K.M.; Lam, T.P.; Cheng, J.C. Abnormal bone quality versus low bone mineral density in adolescent idiopathic scoliosis: A case-control study with in vivo high-resolution peripheral quantitative computed tomography. Spine J. 2013, 13, 1493–1499. [Google Scholar] [CrossRef] [PubMed]
- Cheuk, K.Y.; Zhu, T.Y.; Yu, F.W.P.; Hung, V.W.Y.; Lee, K.M.; Qin, L.; Cheng, J.; Lam, T. Abnormal bone mechanical and structural properties in adolescent idiopathic scoliosis: A study with finite element analysis and structural model index. Calcif. Tissue Int. 2015, 97, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Greenblatt, M.B.; Tsai, N.J.; Wein, M.N. Bone turnover markers in the diagnosis and monitoring of metabolic bone disease. Clin. Chem. 2017, 63, 464–474. [Google Scholar] [CrossRef] [PubMed]
- Matusik, P.; Olszanecka-Glinianowicz, M.; Chudek, J.; Małecka-Tendera, E. Bone turnover markers in the obese children—Relation to gender, body composition and leptin level. Pediatr. Endocrinol. Diabetes Metab. 2015, 21, 154–161. [Google Scholar] [CrossRef]
- Mantzoros, S.C.; Magkos, F.; Brinkoetter, M.; Sienkiewicz, E.; Dardeno, T.A.; Kim, S.Y.; Hamnvik, O.P.R.; Koniaris, A. Leptin in human physiology and pathophysiology. Am. J. Physiol. Endocrinol. Metab. 2011, 301, 567–584. [Google Scholar] [CrossRef]
- Reid, I.R. Fat and bone. Arch. Biochem. Biophys. 2010, 503, 20–27. [Google Scholar] [CrossRef]
- Confavreux, C.B.; Levine, R.L.; Karsenty, G. A paradigm of integrative physiology, the crosstalk between bone and energy metabolism. Mol. Cell. Endocrinol. 2009, 310, 21–29. [Google Scholar] [CrossRef]
- Dimitri, P.; Jacques, R.; Paggiosi, M.; King, D.; Walsh, J.S.; Taylor, Z.A.; Frangi, A.F.; Bishop, N.; Eastell, R. Leptin may play a role in bone microstructural alterations in obese children. J. Clin. Endocrinol. Metab. 2015, 100, 594–602. [Google Scholar] [CrossRef]
- Nikolova, S.T.; Yablanski, V.; Vlaev, E.; Getova, G.; Atanasov, V.; Stokov, L.; Savov, A.S.; Kremensky, I.M. In search of biomarkers for idiopathic scoliosis: Leptin and BMP4 functional polymorphisms. J. Biomark. 2015, 2015, 425310. [Google Scholar] [CrossRef]
- Schwetz, V.; Pieber, T.; Obermayer-Pietsch, B. The endocrine role of the skeleton: Background and clinical evidence. Eur. J. Endocrinol. 2012, 166, 959–967. [Google Scholar] [CrossRef]
- Man, G.C.; Tam, E.M.; Wong, Y.S.; Hung, V.W.; Hu, Z.; Lam, T.P.; Liu, Z.; Cheung, W.H.; Ng, T.B.; Zhu, Z.; et al. Abnormal osteoblastic response to leptin in patients with adolescent idiopathic scoliosis. Sci. Rep. 2019, 20, 17128. [Google Scholar] [CrossRef] [PubMed]
- Tam, E.M.; Liu, Z.; Lam, T.P.; Ting, T.; Cheung, G.; Ng, BK.; Lee, SK.; Qiu, Y.; Cheng, J.C. Lower muscle mass and body fat in adolescent idiopathic scoliosis are associated with abnormal leptin bioavailability. Spine 2016, 41, 940–946. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Tam, E.M.S.; Sun, G.-Q.; Lam, T.; Zhu, Z.-Z.; Sun, X.; Lee, K.-M.; Ng, T.B.; Qiu, Y.; Cheng, J.; et al. Abnormal leptin bioavailability in adolescent idiopathic scoliosis. Spine 2012, 37, 599–604. [Google Scholar] [CrossRef] [PubMed]
- Hamrick, M.W.; Pennington, C.; Newton, D.; Xie, D.; Isales, C. Leptin deficiency produces contrasting phenotypes in bones of the limb and spine. Bone 2004, 34, 376–383. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.T.K.; Cheung, C.S.K.; Tse, Y.K.; Guo, X.; Qin, L.; Lam, T.; Ng, B.K.W.; Cheng, J. Association of osteopenia with curve severity in adolescent idiopathic scoliosis: A study of 919 girls. Osteoporos Int. 2005, 16, 1924–1932. [Google Scholar] [CrossRef] [PubMed]
- Bjure, J.; Nachemson, A. Non-treated scoliosis. Clin. Orthop. Relat. Res. 1973, 93, 44–52. [Google Scholar] [CrossRef]
- de Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- Matusik, E.; Durmala, J.; Matusik, P.; Piotrowski, J. Evaluation of nutritional status of children and adolescents with idiopathic scoliosis—A pilot study. Ortop. Traumatol. Rehabil. 2012, 14, 351–362. [Google Scholar] [CrossRef]
- Wei-Jun, W.; Xu, S.; Zhi-Wei, W.; Xu-Sheng, Q.; Zhen, L.; Yong, Q. Abnormal anthropometric measurements and growth pattern in male adolescent idiopathic scoliosis. Eur. Spine J. 2012, 21, 77–83. [Google Scholar] [CrossRef]
- Davey, R.C.; Cochrane, T.; Dangerfield, P.H.; Chockalingam, N.; Dorgan, J.C. Anthropometry and body composition in females with adolescent idiopathic scoliosis. In International Research Society of Spinal Deformities Symposium; Sawatzky, B.J., Ed.; University of British Columbia: Vancouver, Canada, 2004; pp. 323–326. [Google Scholar]
- Dangerfield, P.H.; Davey, R.C.; Chockalingam, N.; Cochrane, T.; Dorgan, J.C. Body composition in females with adolescent idiopathic scoliosis (AIS) [Abstract]. J. Bone Joint Surg. Br. 2005, 88 (Suppl. 2), 230. [Google Scholar]
- Demerath, E.W.; Schubert, C.M.; Maynard, L.M.; Sun, S.; Chumlea, W.C.; Pickoff, A.; Czerwinski, S.A.; Towne, B.; Siervogel, R.M. Do changes in body mass index percentile reflect changes in body composition in children? Data from the Fels longitudinal study. Pediatrics 2006, 117, 487–495. [Google Scholar]
- de Lorenzo, A.; Sorge, S.P.; Iacopino, L.; Andreoli, A.; de Luca, P.P.; Stasso, G.F. Fat-free mass by bioelectrical impedance vs. dual-energy X-ray absorptiometry (DXA). Appl. Radiat. Isot. 1998, 49, 739–741. [Google Scholar] [PubMed]
- Thomson, R.; Brinkworth, G.D.; Buckley, J.D.; Noakes, M.; Clifton, P.M. Good agreement between bioelectrical impedance and dual-energy X-ray absorptiometry for estimating changes in body composition during weight loss in overweight young women. Clin. Nutr. 2007, 26, 771–777. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, H.D.; Cole, T.J.; Fry, T.; Jebb, S.A.; Prentice, A.M. Body fat reference curves for children. Int. J. Obes. 2006, 30, 598–602. [Google Scholar] [CrossRef]
- Ramirez, M.; Martínez-Llorens, J.; Sanchez, J.F.; Bago, J.; Molina, A.; Gea, J.; Cáceres, E. Body composition in adolescent idiopathic scoliosis. Eur. Spine J. 2012, 22, 324–329. [Google Scholar] [CrossRef]
- Chen, H.; Zhang, J.; Wang, Y.; Cheuk, K.Y.; Hung, A.L.H.; Lam, T.P.; Qiu, Y.; Feng, Y.Q.; Lee, W.Y.W.; Cheng, J.C.Y. Abnormal lacuno-canalicular network and negative correlation between serum osteocalcin and Cobb angle indicate abnormal osteocyte function in adolescent idiopathic scoliosis. FASEB J. 2019, 33, 13882–13892. [Google Scholar] [CrossRef]
- Berglund, J.A.; Tella, S.H.; Tuthill, K.F.; Kim, L.; Guthrie, L.C.; Paul, S.M.; Stanton, R.; Collins, M.T.; Boyce, A.M. Scoliosis in fibrous Dysplasia/McCune-Albright syndrome: Factors associated with curve progression and effects of bisphosphonates. J. Bone Miner. Res. 2018, 33, 1641–1648. [Google Scholar] [CrossRef]
- Dubnov-Raz, G.; Ish-Shalom, S.; Chodick, G.; Rozen, G.S.; Giladi, A.; Constantini, N.W. Osteocalcin is independently associated with body mass index in adolescent girls. Pediatr. Obes. 2012, 7, 313–318. [Google Scholar] [CrossRef]
- Jürimäe, J.; Lätt, E.; Mäestu, E.; Saar, M.; Purge, P.; Maasalu, K.; Jürimäe, T. Osteocalcin is inversely associated with adiposity and leptin in adolescent boys. J. Ped. Endocrinol. Metab. 2015, 28, 571–577. [Google Scholar] [CrossRef] [PubMed]
- Neve, A.; Corrado, A.; Cantatore, F.P. Osteocalcin: Skeletal and extra-skeletal effects. J. Cell. Physiol. 2013, 228, 1149–1153. [Google Scholar] [CrossRef] [PubMed]
- Mokha, J.; Srinivasan, S.R.; DasMahapatra, P.; Fernandez, C.; Chen, W.; Xu, J.; Berenson, G.S. Utility of waist-to-height ratio in assessing the status of central obesity and related cardiometabolic risk profile among normal weight and overweight/obese children: The Bogalusa Heart Study. BMC Pediatrics 2010, 10, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Browning, L.M.; Hsieh, S.D.; Ashwell, M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0–5 could be a suitable global boundary value. Nutr. Res. Rev. 2010, 23, 247–269. [Google Scholar] [CrossRef] [PubMed]
- Yan, W.; Bingxian, H.; Hua, Y.; Jianghong, D.; Jun, C.; Dongliang, G.; Yujian, Z.; Ling, L.; Yanying, G.; Kaiti, X.; et al. Waist-to-height ratio is an accurate and easier index for evaluating obesity in children and adolescents. Obesity 2007, 15, 748–752. [Google Scholar] [CrossRef] [PubMed]
| N | 77 |
|---|---|
| Age (years) | 14.7 ± 2.17 |
| Corrected height (cm) | 166.55 ± 9.48 |
| Corrected height Z score (SD) | 0.93 ± 0.99 |
| Weight (kg) | 51.28 ± 9.62 |
| BMI (kg/m2) | 18.38 ± 2.56 |
| BMI Z score (SD) | −0.70 ± 1.03 |
| W/HtR | 0.43 ± 0.04 |
| FAT (%) | 21.47 ± 5.56 |
| FFM (%) | 77.69 ± 9.03 |
| PMM (%) | 74.55 ± 5.73 |
| TBW (%) | 56.91 ± 6.34 |
| Cobb’s angle (°) | 25.21 ± 15.32 |
| Variable | Coefficient β | Cobb’s Angle | Adjusted R2 |
|---|---|---|---|
| Log Leptin (ng/mL) | 0.243 | p < 0.05 | 0.062 |
| Log OC (ng/mL) | −0.260 | p < 0.05 | 0.082 |
| Log NTx (nM/BCE) | −0.381 | p < 0.01 | 0.109 |
| W/HtR | 0.314 | p < 0.01 | 0.075 |
| FAT (%) | 0.268 | p < 0.05 | 0.083 |
| Mild (n = 36) Mean ± SD | Moderate (n = 30) Mean ± SD | Severe (n = 11) Mean ± SD | Significance (ANOVA) | |
|---|---|---|---|---|
| BMI (kg/m2) | 18.13 ± 1.74 | 18.30 ± 2.82 | 19.08 ± 2.30 | NS |
| BMI z-score (SD) | −0.74 ± 0.77 | −0.81 ± 1.12 | −0.44 ± 1.54 | NS |
| FAT (%) | 20.76 ± 4.82 | 21.47 ± 5.39 | 24.78 ± 7.54 | NS |
| FFM (%) | 79.24 ± 4.90 | 76.33 ± 12.71 | 75.24 ± 7.57 | NS |
| TBW (%) | 58.01 ± 3.58 | 55.99 ± 8.81 | 55.09 ± 5.54 | NS |
| PMM (%) | 74.96 ± 5.62 | 74.87 ± 5.37 | 71.43 ± 6.99 | NS |
| Log Leptin [ng/mL] | ||||
|---|---|---|---|---|
| Pearson’s Correlation | ||||
| Mild (n = 36) | Moderate (n = 30) | Severe (n = 11) | Total (n = 77) | |
| BMI z-score (SD) | 0.374 * | 0.445 * | 0.421 (p = 0.197) | 0.372 *** |
| W/HtR | 0.417 * | 0.570 ** | 0.551 (p = 0.079) | 0.487 ^ |
| FAT (%) | 0.694 *** | 0.540 ** | 0.558 (p = 0.075) | 0.583 ^ |
| FFM (%) | −0.691 *** | −0.537 ** | −0.551 (p = 0.073) | −0.581 ^^ |
| TBW (%) | −0.694 *** | −0.532 ** | −0.564 (p = 0.071) | −0.581 ^^ |
| PMM(%) | −0.641 *** | −0.551 ** | −0.556 (p = 0.076) | −0.570 ^^ |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matusik, E.; Durmala, J.; Olszanecka-Glinianowicz, M.; Chudek, J.; Matusik, P. Association between Bone Turnover Markers, Leptin, and Nutritional Status in Girls with Adolescent Idiopathic Scoliosis (AIS). Nutrients 2020, 12, 2657. https://doi.org/10.3390/nu12092657
Matusik E, Durmala J, Olszanecka-Glinianowicz M, Chudek J, Matusik P. Association between Bone Turnover Markers, Leptin, and Nutritional Status in Girls with Adolescent Idiopathic Scoliosis (AIS). Nutrients. 2020; 12(9):2657. https://doi.org/10.3390/nu12092657
Chicago/Turabian StyleMatusik, Edyta, Jacek Durmala, Magdalena Olszanecka-Glinianowicz, Jerzy Chudek, and Pawel Matusik. 2020. "Association between Bone Turnover Markers, Leptin, and Nutritional Status in Girls with Adolescent Idiopathic Scoliosis (AIS)" Nutrients 12, no. 9: 2657. https://doi.org/10.3390/nu12092657
APA StyleMatusik, E., Durmala, J., Olszanecka-Glinianowicz, M., Chudek, J., & Matusik, P. (2020). Association between Bone Turnover Markers, Leptin, and Nutritional Status in Girls with Adolescent Idiopathic Scoliosis (AIS). Nutrients, 12(9), 2657. https://doi.org/10.3390/nu12092657






