Priority Actions to Advance Population Sodium Reduction
Abstract
1. Introduction
1.1. Action to Date on Sodium Reduction
1.2. Evidence for Sodium Reduction Interventions
2. Framework Development
2.1. Existing Sodium Reduction Strategies
2.2. Developing a Framework for Prioritizing High-Impact Sodium Reduction Strategies
- 1.
- Scalable and Sustainable
- 2.
- Evidence of effectiveness or innovation
- (a)
- Rigorously evaluated with demonstrated success in sodium reduction
- (b)
- Suggestive evidence of effectiveness in reducing sodium consumption from lower quality evaluations or modeling studies
- (c)
- Rigorously evaluated strategies that do not specifically target sodium reduction but could be adapted to address sodium and then evaluated to assess impact on sodium intake
- (d)
- Innovation: If a specific source of sodium in a population cannot be sufficiently addressed by a strategy meeting one of the 3 sub-criteria above, a strategy taking an innovative and promising approach may be included with a planned evaluation
- 3.
- Large benefit
3. Applying the Framework
3.1. Evaluate Existing Interventions against the Proposed Framework
3.2. Summaries of High-Impact Recommended Strategies
3.2.1. Sodium Reduction Strategies for Packaged Food
Front-of-Pack Labeling Regulations
Food Reformulation Targets for Packaged Food (Voluntary or Mandatory)
Regulation of Marketing of Foods and Nonalcoholic Beverages to Children
Fiscal Policies: Taxation on High Sodium Foods
3.2.2. Strategies to Reduce Sodium Consumed from Food Prepared Outside the Home
Standards for Sodium as Part of Food Procurement Policies in Public Institutions
3.2.3. Strategies to Reduce Sodium Consumed at Home
Mass Media Campaigns
Increase Uptake of Low-Sodium Salt (Promotion, Distribution, Subsidies)
4. Discussion
Areas for Future Research
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller, E.R.; Morton, D.G.S.; et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N. Engl. J. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef]
- He, F.J.; Li, J.; Macgregor, G.A. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 2013, 346, f1325. [Google Scholar] [CrossRef]
- INTERSALT. Intersalt: An international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ 1988, 297, 319–328. [Google Scholar] [CrossRef]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Fahimi, S.; Singh, G.M.; Micha, R.; Khatibzadeh, S.; Engell, R.E.; Lim, S.; Danaei, G.; Ezzati, M.; Powles, J.; et al. Global sodium consumption and death from cardiovascular causes. N. Engl. J. Med. 2014, 371, 624–634. [Google Scholar] [CrossRef]
- World Health Organization. Global Strategy on Diet, Physical Activity and Health; WHO: Geneva, Switzerland, 2004. [Google Scholar]
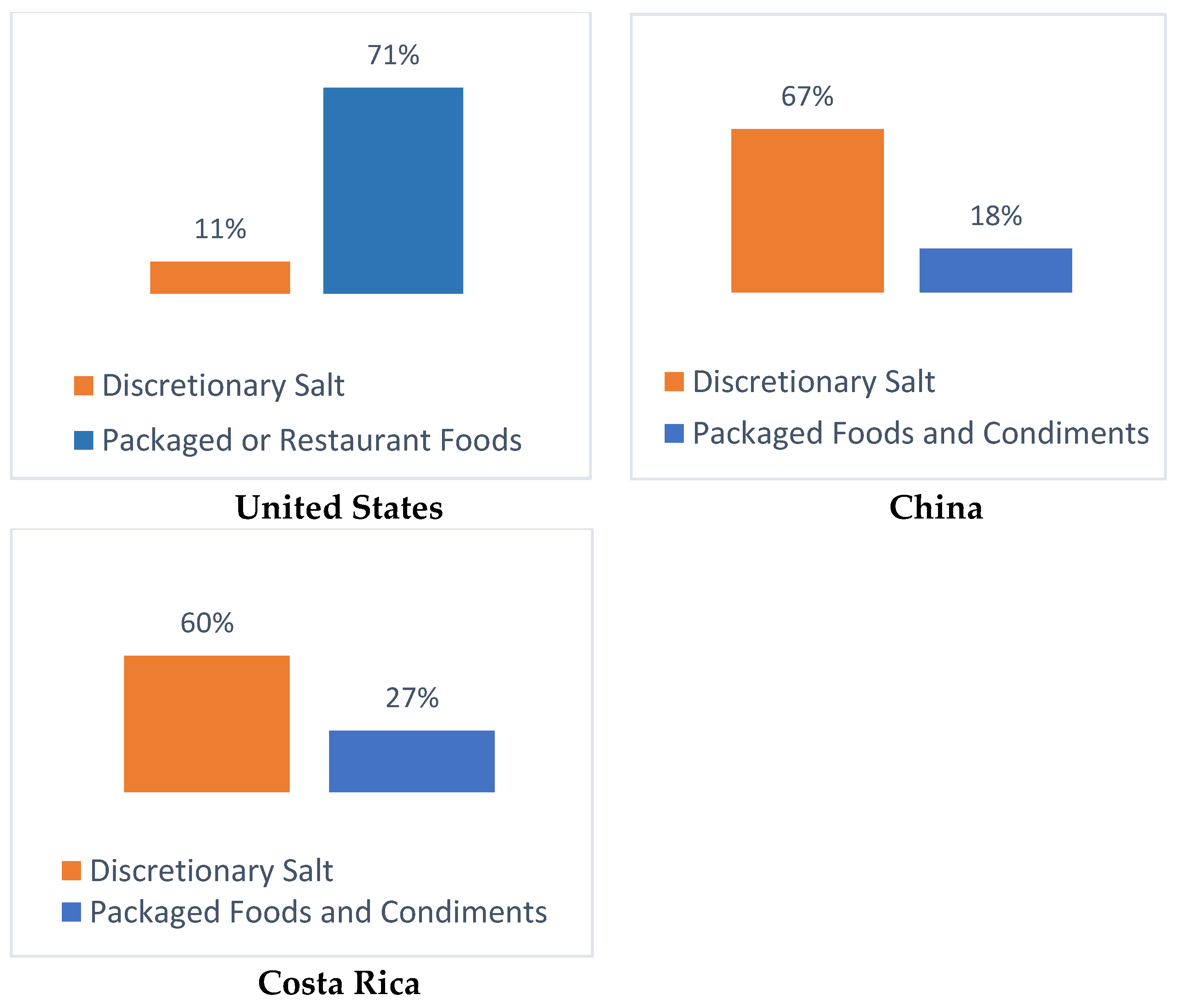
- Bhat, S.; Marklund, M.; Henry, M.E.; Appel, L.J.; Croft, K.D.; Neal, B.; Wu, J.H.Y. A systematic review of the sources of dietary salt around the world. Adv. Nutr. 2020, 11, 677–686. [Google Scholar] [CrossRef]
- Harnack, L.J.; Cogswell, M.E.; Shikany, J.M.; Gardner, C.D.; Gillespie, C.; Loria, C.M.; Zhou, X.; Yuan, K.; Steffen, L.M. Sources of sodium in US adults from 3 geographic regions. Circulation 2017, 135, 1775–1783. [Google Scholar] [CrossRef] [PubMed]
- Du, S.; Wang, H.; Zhang, B.; Popkin, B. Dietary potassium intake remains low and sodium intake remains high, and most sodium is derived from home food preparation for Chinese adults, 1991–2015 trends. J. Nutr. 2020, 150, 1230–1239. [Google Scholar] [CrossRef] [PubMed]
- Metzler, A.B.; Claro, R.M.; Blonval, K.H.; Rodríguez, I.C.; Campos, M.L.A.; Legetic, B.; L’Abbe, M.R. Baseline and estimated trends of sodium availability and food sources in the costa rican population during 2004–2005 and 2012–2013. Nutrients 2017, 9, 1020. [Google Scholar] [CrossRef] [PubMed]
- Trieu, K.; Neal, B.; Hawkes, C.; Dunford, E.; Campbell, N.; Fernandez, R.R.; Legetic, B.; McLaren, L.; Barberio, A.; Webster, J. Salt reduction initiatives around the world-a systematic review of progress towards the global target. PLoS ONE 2015, 10, e0130247. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Nutrition Policy Review 2016–2017: Country Progress in Creating Enabling Policy Environments for Promoting Healthy Diets and Nutrition; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Campbell, N.R.; Dary, O.; Cappuccio, F.P.; Neufeld, L.M.; Harding, K.B.; Zimmermann, M.B. Need for coordinated programs to improve global health by optimizing salt and iodine intake. Rev. Panam. Salud Publica 2012, 32, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Charlton, K.; Ware, L.J.; Baumgartner, J.; Cockeran, M.; Schutte, A.E.; Naidoo, N.; Kowal, P. How will South Africa’s mandatory salt reduction policy affect its salt iodisation programme? A cross-sectional analysis from the WHO-SAGE Wave 2 Salt & Tobacco study. BMJ Open 2018, 8, e020404. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Saving Lives, Spending Less: A Strategic Response to Noncommunicable Diseases; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Hyseni, L.; Green, A.E.; Williams, F.L.; Kypridemos, C.; O’Flaherty, M.; McGill, R.; Orton, L.; Bromley, H.; Cappuccio, F.P.; Capewell, S. Systematic review of dietary salt reduction policies: Evidence for an effectiveness hierarchy? PLoS ONE 2017, 12, e0177535. [Google Scholar] [CrossRef] [PubMed]
- McLaren, L.; Sumar, N.; Barberio, A.M.; Trieu, K.; Lorenzetti, D.L.; Tarasuk, V.; Webster, J.; Campbell, N.R. Population-level interventions in government jurisdictions for dietary sodium reduction. Cochrane Database Syst. Rev. 2016, 9, CD010166. [Google Scholar] [CrossRef]
- McLaren, L.; McIntyre, L.; Kirkpatrick, S. Rose’s population strategy of prevention need not increase social inequalities in health. Int. J. Epidemiol 2010, 39, 372–377. [Google Scholar] [CrossRef]
- He, F.J.; Rodrigues, S.P.; Macgregor, G.A. Salt reduction in England from 2003 to 2011: Its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open 2014, 4, e004549. [Google Scholar] [CrossRef]
- Park, H.-K.; Lee, Y.; Kang, B.-W.; Kwon, K.-I.; Kim, J.-W.; Kwon, O.-S.; Cobb, L.K.; Campbell, N.R.C.; Blakeman, D.E.; Kim, C.-I. Progress on sodium reduction in South Korea. BMJ Glob. Health 2020. [Google Scholar] [CrossRef]
- He, F.J.; Brinsden, H.C.; MacGregor, G.A. Salt reduction in the United Kingdom: A successful experiment in public health. J. Hum. Hypertens. 2014, 28, 345–352. [Google Scholar] [CrossRef]
- World Cancer Research Fund. Nourishing Database. Available online: https://www.wcrf.org/int/policy/nourishing-database (accessed on 1 May 2020).
- Ministry of Health. Law No. 20,606 on Nutritional Composition of Food and its Advertising; Diario Oficial de Chile: Santiago, Republic of Chile, 2012. [Google Scholar]
- World Health Organization Regional Office for Europe. Assessment of the Impact of a Public Health Product Tax; WHO Regional Office for Europe: Copenhagen, Denmark, 2015. [Google Scholar]
- Durkin, S.; Brennan, E.; Wakefield, M. Mass media campaigns to promote smoking cessation among adults: An integrative review. Tob. Control 2012, 21, 127–138. [Google Scholar] [CrossRef]
- Neal, B.; Tian, M.; Li, N.; Elliott, P.; Yan, L.L.; Labarthe, D.R.; Huang, L.; Yin, X.; Hao, Z.; Stepien, S.; et al. Rationale, design, and baseline characteristics of the salt substitute and stroke study (SSaSS)—A large-scale cluster randomized controlled trial. Am. Heart J. 2017, 188, 109–117. [Google Scholar] [CrossRef]
- Dehmer, S.; Cogswell, M.; Ritchey, M.; Hong, Y.; Maciosek, M.; LaFrance, A.; Roy, K. Health and budgetary impact of achieving 10-year U.S. sodium reduction targets. Am. J. Prev. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Liberato, S.; Bailie, R.; Brimblecombe, J. Nutrition Interventions at point-of-sale to encourage healthier food purchasing: A systematic review. BMC Public Health 2014, 14. [Google Scholar] [CrossRef] [PubMed]
- Boyce, J.H.; Bianchi, F.; Piernas, C.; Payne, R.S.; Frie, K.; Nourse, R.; Jebb, S. Grocery store interventions to change food purchasing behaviors: A systematic review of randomized controlled trials. Am. J. Clin. Nutr. 2018, 107. [Google Scholar] [CrossRef]
- Kanter, R.; Vanderlee, L.; Vandevijvere, S. Front-of-package nutrition labelling policy: Global progress and future directions. Public Health Nutr. 2018, 21, 1399–1408. [Google Scholar] [CrossRef]
- Campos, S.; Doxey, J.; Hammond, D. Nutrition labels on pre-packaged foods: A systematic review. Public Health Nutr. 2011, 14, 1496–1506. [Google Scholar] [CrossRef]
- Khandpur, N.; Sato, P.d.M.; Mais, L.A.; Martins, A.P.B.; Spinillo, C.G.; Garcia, M.T.; Rojas, C.F.U.; Jaime, P.C. Are front-of-package warning labels more effective at communicating nutrition information than traffic-light labels? A randomized controlled experiment in a Brazilian sample. Nutrients 2018, 10, 688. [Google Scholar] [CrossRef]
- Arrua, A.; Machin, L.; Curutchet, M.R.; Martinez, J.; Antunez, L.; Alcaire, F.; Gimenez, A.; Ares, G. Warnings as a directive front-of-pack nutrition labelling scheme: Comparison with the guideline daily amount and traffic-light systems. Public Health Nutr. 2017, 20, 2308–2317. [Google Scholar] [CrossRef]
- Taillie, L.S.; Hall, M.G.; Popkin, B.M.; Ng, S.W.; Murukutla, N. Experimental studies of front-of-package nutrient warning labels on sugar-sweetened beverages and ultra-processed foods: A scoping review. Nutrients 2020, 12, 569. [Google Scholar] [CrossRef]
- Cecchini, M.; Warin, L. Impact of food labelling systems on food choices and eating behaviours: A systematic review and meta-analysis of randomized studies. Obes. Rev. 2016, 17, 201–210. [Google Scholar] [CrossRef]
- Ministerio de Salud. Informe de Evaluacion de la Implementacion de la Ley Sobre Composicion Nutricional de Los Alimentos y su Publicidad; Ministerio de Salud: Santiago, Republic de Chile, 2018.
- Díaz, A.A.; Veliz, P.M.; Mariño, G.R.; Mafla, C.V.; Altamirano, L.M.M.; Jones, C.V. Etiquetado de alimentos en Ecuador: Implementación, resultados y acciones pendientes. Rev. Panam. Salud Pública 2017, 41. [Google Scholar] [CrossRef]
- Pan American Health Organization. Salt-Smart Americas: A Guide for Country-Level Action; Pan American Health Organization: Washington, DC, USA, 2013. [Google Scholar]
- Laverty, A.; Kypridemos, C.; Seferidi, P.; Vamos, E.; Stuttard, J.P.; Collins, B.; Capewell, S.; Mwatsama, M.; Cairney, P.; Fleming, K.; et al. Quantifying the impact of the public health responsibility deal on salt intake, cardiovascular disease and gastric cancer burdens: Interrupted time series and microsimulation study. J. Epidemiol. Community Health 2019, 73. [Google Scholar] [CrossRef] [PubMed]
- Promoción de la Reducción del Consumo de Sodio en la Población; Boletin Oficial de la Republica Argentina: Buenos Aires, Argentina, 2013; Ley 26.905.
- South African Department of Health Foodstuffs. Regulations relating to the reduction of sodium in certain foodstuffs and related matters. In Cosmetics and Disinfectants Act; Government Gazette: Pretoria, South Africa, 2013; Volume 36274, Act No. 54 of 1972. [Google Scholar]
- Allemandi, L.; Tiscornia, M.V.; Guarnieri, L.; Castronuovo, L.; Martins, E. Monitoring sodium content in processed foods in argentina 2017–2018: Compliance with national legislation and regional targets. Nutrients 2019, 11, 1474. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.A.E.; Dunford, E.; Ware, L.J.; Harris, T.; Walker, A.; Wicks, M.; Zyl, T.V.; Swanepoel, B.; Charlton, K.E.; Woodward, M.; et al. The sodium content of processed foods in south africa during the introduction of mandatory sodium limits. Nutrients 2017, 9, 404. [Google Scholar] [CrossRef] [PubMed]
- Boyland, E.J.; Nolan, S.; Kelly, B.; Smith, C.T.; Jones, A.; Halford, J.C.; Robinson, E. Advertising as a cue to consume: A systematic review and meta-analysis of the effects of acute exposure to unhealthy food and nonalcoholic beverage advertising on intake in children and adults. Am. J. Clin. Nutr. 2016, 103, 519–533. [Google Scholar] [CrossRef] [PubMed]
- Kelly, B.; King, M.L.; Chapman Mnd, K.; Boyland, E.; Bauman, A.E.; Baur, L.A. A hierarchy of unhealthy food promotion effects: Identifying methodological approaches and knowledge gaps. Am. J. Public Health 2015, 105, e86–e95. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Marketing of Foods and Non-Alcoholic Beverages to Children; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- UNICEF. A Child Rights-Based Approach to Food Marketing: A Guide for Policy Makers; UNICEF: Geneva, Switzerland, 2018.
- Bobowski, N. Shifting human salty taste preference: Potential opportunities and challenges in reducing dietary salt intake of Americans. Chemosens Percept 2015, 8, 112–116. [Google Scholar] [CrossRef]
- Ronit, K.; Jensen, J.D. Obesity and industry self-regulation of food and beverage marketing: A literature review. Eur. J. Clin. Nutr. 2014, 68, 753–759. [Google Scholar] [CrossRef]
- Chambers, S.A.; Freeman, R.; Anderson, A.S.; MacGillivray, S. Reducing the volume, exposure and negative impacts of advertising for foods high in fat, sugar and salt to children: A systematic review of the evidence from statutory and self-regulatory actions and educational measures. Prev. Med. 2015, 75, 32–43. [Google Scholar] [CrossRef]
- King, L.; Hebden, L.; Grunseit, A.; Kelly, B.; Chapman, K. Building the case for independent monitoring of food advertising on Australian television. Public Health Nutr. 2013, 16, 2249–2254. [Google Scholar] [CrossRef][Green Version]
- Kent, M.P.; Pauze, E. The effectiveness of self-regulation in limiting the advertising of unhealthy foods and beverages on children’s preferred websites in Canada. Public Health Nutr. 2018, 21, 1608–1617. [Google Scholar] [CrossRef]
- Vandevijvere, S.; Soupen, A.; Swinburn, B. Unhealthy food advertising directed to children on New Zealand television: Extent, nature, impact and policy implications. Public Health Nutr. 2017, 20, 3029–3040. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Harris, J.L.; Kalnova, S.S. Food and beverage TV advertising to young children: Measuring exposure and potential impact. Appetite 2018, 123, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Garde, A.; Jeffery, B.; Rigby, N. Implementing the WHO recommendations whilst avoiding real, perceived or potential conflicts of interest. Eur. J. Risk Regul. 2017, 8, 237–250. [Google Scholar] [CrossRef]
- Stoltze, F.M.; Reyes, M.; Smith, T.L.; Correa, T.; Corvalan, C.; Carpentier, F.R.D. Prevalence of child-directed marketing on breakfast cereal packages before and after chile’s food marketing law: A pre-and post-quantitative content analysis. Int. J. Environ. Res. Public Health 2019, 16, 4501. [Google Scholar] [CrossRef] [PubMed]
- Carpentier, F.R.D.; Correa, T.; Reyes, M.; Taillie, L.S. Evaluating the impact of Chile’s marketing regulation of unhealthy foods and beverages: Preschool and adolescent children’s changes in exposure to food advertising on television. Public Health Nutr. 2020, 23, 747–755. [Google Scholar] [CrossRef]
- Correa, T.; Reyes, M.; Taillie, L.; Corvalán, C.; Carpentier, F.R.D. Food advertising on television before and after a national unhealthy food marketing regulation in chile, 2016–2017. Am. J. Public Health 2020, 110, 1054–1059. [Google Scholar] [CrossRef]
- Kim, S.; Lee, Y.; Yoon, J.; Chung, S.J.; Lee, S.K.; Kim, H. Restriction of television food advertising in South Korea: Impact on advertising of food companies. Health Promot. Int. 2013, 28, 17–25. [Google Scholar] [CrossRef]
- Wright, A.; Smith, K.E.; Hellowell, M. Policy lessons from health taxes: A systematic review of empirical studies. BMC Public Health 2017, 17, 583. [Google Scholar] [CrossRef]
- World Health Organization. International agency for research on cancer. In Effectiveness of Tax and Price Policies for Tobacco Control; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Wagenaar, A.C.; Salois, M.J.; Komro, K.A. Effects of beverage alcohol price and tax levels on drinking: A meta-analysis of 1003 estimates from 112 studies. Addiction 2009, 104, 179–190. [Google Scholar] [CrossRef]
- Niebylski, M.L.; Redburn, K.A.; Duhaney, T.; Campbell, N.R. Healthy food subsidies and unhealthy food taxation: A systematic review of the evidence. Nutrition 2015, 31, 787–795. [Google Scholar] [CrossRef]
- Teng, A.; Jones, A.C.; Mizdrak, A.; Signal, L.; Genç, M.; Wilson, N. Impact of sugar-sweetened beverage taxes on purchases and dietary intake: Systematic review and meta-analysis. Obes. Rev. J. Int. Assoc. Study Obes. 2019, 20, 1187–1204. [Google Scholar] [CrossRef] [PubMed]
- Colchero, M.A.; Dommarco, J.R.; Popkin, B.M.; Ng, S.W. In Mexico, evidence of sustained consumer response two years after implementing a sugar-sweetened beverage tax. Health Aff. 2017, 36, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Batis, C.; Rivera, J.A.; Popkin, B.M.; Taillie, L.S. First-year evaluation of mexico’s tax on nonessential energy-dense foods: An observational study. PLoS Med. 2016, 13, e1002057. [Google Scholar] [CrossRef] [PubMed]
- Osornprasop, S.; Zheng, R.; Hufanga, S.V.; Latu, C.F.; Lounkaew, K.; Krahn, J. Using Taxation to Address Noncommunicable Diseases: Lessons from Tonga; The World Bank: Washington, DC, USA, 2019. [Google Scholar]
- Cobiac, L.J.; Tam, K.; Veerman, L.; Blakely, T. Taxes and subsidies for improving diet and population health in Australia: A cost-effectiveness modelling study. PLoS Med. 2017, 14, e1002232. [Google Scholar] [CrossRef] [PubMed]
- Harding, M.; Lovenheim, M. The effect of prices on nutrition: Comparing the impact of product-and nutrient-specific taxes. J. Health Econ. 2017, 53, 53–71. [Google Scholar] [CrossRef] [PubMed]
- Schorling, E.; Niebuhr, D.; Kroke, A. Cost-effectiveness of salt reduction to prevent hypertension and CVD: A systematic review. Public Health Nutr. 2017, 20, 1993–2003. [Google Scholar] [CrossRef]
- Caro, J.C.; Taillie, L.S.; Ng, S.W.; Popkin, B. Designing a food tax to impact food-related non-communicable diseases: The case of Chile. Food Policy 2017, 71, 86–100. [Google Scholar] [CrossRef]
- Donaldson, E. Advocating for sugar-sweetened beverage taxation: A case study of Mexico. NCD Alliance 2015, 1, 3–27. [Google Scholar]
- Briggs, A.D.M.; Mytton, O.T.; Kehlbacher, A.; Tiffin, R.; Elhussein, A.; Rayner, M.; Jebb, S.A.; Blakely, T.; Scarborough, P. Health impact assessment of the UK soft drinks industry levy: A comparative risk assessment modelling study. Lancet Public Health 2017, 2, e15–e22. [Google Scholar] [CrossRef]
- Roache, S.A.; Gostin, L.O. The untapped power of soda taxes: Incentivizing consumers, generating revenue, and altering corporate behavior. Int. J. Health Policy Manag. 2017, 6, 489–493. [Google Scholar] [CrossRef]
- Andreyeva, T.; Chaloupka, F.J.; Brownell, K.D. Estimating the potential of taxes on sugar-sweetened beverages to reduce consumption and generate revenue. Prev. Med. 2011, 52, 413–416. [Google Scholar] [CrossRef] [PubMed]
- Thow, A.; Downs, S.; Jan, S. A systematic review of the effectiveness of food taxes and subsidies to improve diets: Understanding the recent evidence. Nutr. Rev. 2014, 72. [Google Scholar] [CrossRef] [PubMed]
- Dodd, R.; Santos, J.A.; Tan, M.; Campbell, N.R.C.; Mhurchu, C.N.; Cobb, L.; Jacobson, M.F.; He, F.J.; Trieu, K.; Osornprasop, S.; et al. Effectiveness and feasibility of taxing salt and foods high in sodium: A systematic review of the evidence. Adv. Nutr. 2020. [Google Scholar] [CrossRef] [PubMed]
- Government of India. About the Mid Day Meal Scheme. Available online: Mdm.nic.in (accessed on 1 May 2020).
- NYC Health; New York City Food Standards: New York, NY, USA, 2015.
- Mozaffarian, D.; Angell, S.Y.; Lang, T.; Rivera, J.A. Role of government policy in nutrition-barriers to and opportunities for healthier eating. BMJ 2018, 361, k2426. [Google Scholar] [CrossRef] [PubMed]
- Sustainable procurement: The Official Government Buying Standards (GBS) for Food and Catering Services; UK Department for Environment: London, UK, 2015.
- WOG Healthier Catering Policy; Singapore Health Promotion Board: Singapore, 2017.
- Philadelphia Nutrition Standards; Philadelphia Department of Public Health: Philadelphia, PA, USA, 2018.
- Healthy Food and Drink Choices Policy; ACT Government: Canberra City ACT, Australia, 2016. Available online: https://www.health.act.gov.au/about-our-health-system/population-health/health-promotion-programs/healthy-food-and-drink-choices (accessed on 21 August 2020).
- ACT Public Sector Healthy Food and Drink Choices Policy; ACT Government: Canberra City ACT, Australia, 2016. Available online: http://www.cmd.act.gov.au/__data/assets/pdf_file/0003/905772/WHS-01-2016-Healthy-Food-and-Drink-Choices-Policy.pdf (accessed on 21 August 2020).
- ACT Public School Food and Drink Policy; ACT Government: Canberra City ACT, Australia, 2016. Available online: https://www.education.act.gov.au/publications_and_policies/School-and-Corporate-Policies/school-administration-and-management/food-and-drink/act-public-school-food-and-drink-policy/act-public-school-food-and-drink-policy (accessed on 21 August 2020).
- Niebylski, M.L.; Lu, T.; Campbell, N.R.; Arcand, J.; Schermel, A.; Hua, D.; Yeates, K.E.; Tobe, S.W.; Twohig, P.A.; L’Abbe, M.R.; et al. Healthy food procurement policies and their impact. Int. J. Environ. Res. Public Health 2014, 11, 2608–2627. [Google Scholar] [CrossRef]
- Driessen, C.E.; Cameron, A.J.; Thornton, L.E.; Lai, S.K.; Barnett, L.M. Effect of changes to the school food environment on eating behaviours and/or body weight in children: A systematic review. Obes. Rev. 2014, 15, 968–982. [Google Scholar] [CrossRef]
- Micha, R.; Karageorgou, D.; Bakogianni, I.; Trichia, E.; Whitsel, L.P.; Story, M.; Penalvo, J.L.; Mozaffarian, D. Effectiveness of school food environment policies on children’s dietary behaviors: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0194555. [Google Scholar] [CrossRef]
- Wakefield, M.; Loken, B.; Hornik, R. Use of mass media campaigns to change health behaviour. Lancet 2010, 376. [Google Scholar] [CrossRef]
- Bethesda, M.D. The Role of the Media in Promoting and Reducing Tobacco Use; U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute: Bethesda, MD, USA, 2008.
- Durkin, S.J.; Biener, L.; Wakefield, M.A. Effects of different types of antismoking ads on reducing disparities in smoking cessation among socioeconomic subgroups. Am. J. Public Health 2009, 99. [Google Scholar] [CrossRef]
- Pomerleau, J.; Lock, K.; Knai, C.; McKee, M. Interventions designed to increase adult fruit and vegetable intake can be effective: A systematic review of the literature. J. Nutr. 2005, 135. [Google Scholar] [CrossRef]
- Marcus, B.; Williams, D.; Dubbert, P.; Sallis, J.; King, A.; Yancey, A.; Franklin, B.; Buchner, D.; Daniels, S.; Claytor, R. Physical activity intervention studies: What we know and what we need to know: A scientific statement from the american heart association council on nutrition, physical activity, and metabolism (subcommittee on physical activity); council on cardiovascular disease in the young; and the interdisciplinary working group on quality of care and outcomes research. Circulation 2006, 114. [Google Scholar] [CrossRef]
- Abioye, A.; Hajifathalian, K.; Danaei, G. Do mass media campaigns improve physical activity? A systematic review and meta-analysis. Arch. Public Health 2013, 71. [Google Scholar] [CrossRef] [PubMed]
- Afshin, A.A.; Ajala, O.N.; Nguyen, A.B.; See, K.C.; Mozaffarian, D. Abstract P087: Effectiveness of mass media campaigns for improving dietary behaviors: A systematic review and meta-analysis. Circulation 2013, 127. [Google Scholar] [CrossRef]
- Viljoen, E.W.; Steyn, K.; Lombard, C.; Villiers, A.D.; Charlton, K.; Frielinghaus, S.; Crickmore, C.; Singh, V.M. Evaluation of a mass-media campaign to increase the awareness of the need to reduce discretionary salt use in the South African population. Nutrients 2017, 9, 1238. [Google Scholar] [CrossRef]
- Sutherland, J.; Edwards, P.; Shankar, B.; Dangour, A. Fewer adults add salt at the table after initiation of a national salt campaign in the UK: A repeated cross-sectional analysis. Br. J. Nutr. 2013, 110. [Google Scholar] [CrossRef]
- Greer, R.C.; Marklund, M.; Anderson, C.A.M.; Cobb, L.K.; Dalcin, A.T.; Henry, M.; Appel, L.J. Potassium-enriched salt substitutes as a means to lower blood pressure: Benefits and risks. Hypertension 2020, 75, 266–274. [Google Scholar] [CrossRef]
- Newberry, S.J.; Chung, M.; Anderson, C.A.M.; Chen, C.; Fu, Z.; Tang, A.; Zhao, N.; Booth, M.; Marks, J.; Hollands, S.; et al. Sodium and potassium intake: Effects on chronic disease outcomes and risks. Agency Healthc. Res. Qual. 2018. [Google Scholar]
- Mu, L.; Li, C.; Liu, T.; Xie, W.; Li, G.; Wang, M.; Wang, R.; Rao, H.; He, Q.; Wang, W.; et al. A pilot study on efficacy and safety of a new salt substitute with very low sodium among hypertension patients on regular treatment. Medicine 2020, 99. [Google Scholar] [CrossRef]
- Huang, L.; Tian, M.; Yu, J.; Li, Q.; Liu, Y.; Yin, X.; Wu, J.; Marklund, M.; Wu, Y.; Li, N.; et al. Interim effects of salt substitution on urinary electrolytes and blood pressure in the China salt substitute and stroke study (SSaSS). Am. Heart J. 2020, 221. [Google Scholar] [CrossRef]
- Marklund, M.; Singh, G.; Greer, R.; Cudhea, F.; Matsushita, K.; Micha, R.; Brady, T.; Zhao, D.; Huang, L.; Tian, M.; et al. Estimated population wide benefits and risks in china of lowering sodium through potassium enriched salt substitution: Modelling study. BMJ 2020, 369. [Google Scholar] [CrossRef]
- Li, N.; Yan, L.L.; Niu, W.; Yao, C.; Feng, X.; Zhang, J.; Shi, J.; Zhang, Y.; Zhang, R.; Hao, Z.; et al. The effects of a community-based sodium reduction program in rural China—A cluster-randomized trial. PLoS ONE 2016, 11, e0166620. [Google Scholar] [CrossRef]
- Ortiz, A.B.; Sal, Y.; Rosas, V.; Lucero, V.P.; Cárdenas, M.; Larco, R.C.; Canseco, F.D.; Pesantes, M.; Sacksteder, K.; Gilman, R.; et al. Effect of salt substitution on community-wide blood pressure and hypertension incidence. Nat. Med. 2020, 26. [Google Scholar] [CrossRef]
- Garcia, L.S.; Ortiz, A.B.; Gilman, R.; Canseco, F.D.; Cárdenas, M.; Sacksteder, K.; Miranda, J. Applying the triangle taste test to assess differences between low sodium salts and common salt: Evidence from Peru. PLoS ONE 2015, 10, e0134700. [Google Scholar] [CrossRef]
- SACN-COT Statements on Potassium-Based Sodium Replacers: Assessment of the Health Benefits and Risks of Using Potassium-Based Sodium Replacers in Foods in the UK; Scientific Advisory Committee on Nutrition and the Committee on Toxicity: London, UK, 2017.
- Hawkes, C. Promoting Healthy Diets through Nutrition Education and Changes in the Food Environment: An International Review of Actions and their Effectiveness; Nutrition Education and Consumer Awareness Group, Food and Agriculture Organization of the United Nations: Rome, Italy, 2013. [Google Scholar]
- Contento, I. Nutrition education: Linking research, theory, and practice. Asia Pac. J. Clin. Nutr. 2008, 17, 176–179. [Google Scholar] [PubMed]
- Cook, N.R.; Cutler, J.A.; Obarzanek, E.; Buring, J.E.; Rexrode, K.M.; Kumanyika, S.K.; Appel, L.J.; Whelton, P.K. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: Observational follow-up of the trials of hypertension prevention (TOHP). BMJ 2007, 334, 885–888. [Google Scholar] [CrossRef] [PubMed]
- He, F.J.; Wu, Y.; Feng, X.X.; Ma, J.; Ma, Y.; Wang, H.; Zhang, J.; Yuan, J.; Lin, C.P.; Nowson, C.; et al. School based education programme to reduce salt intake in children and their families (School-EduSalt): Cluster randomised controlled trial. BMJ 2015, 350. [Google Scholar] [CrossRef] [PubMed]
- Trieu, K.; McMahon, E.; Santos, J.A.; Bauman, A.; Jolly, K.A.; Bolam, B.; Webster, J. Review of behaviour change interventions to reduce population salt intake. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 17. [Google Scholar] [CrossRef] [PubMed]
- Approval of a New Food Act in Chile: Process Summary; Food and Agriculture Organization of the United Nations; World Health Organization: Santiago, Chile, 2016.
- Guiding Principles and Framework Manual for Front-of-Pack Labelling for Promoting Healthy Diet; World Health Organization: Geneva, Switzerland, 2019.
- Curtis, C.J.; Clapp, J.; Niederman, S.A.; Ng, S.W.; Angell, S.Y. US Food industry progress during the national salt reduction initiative: 2009–2014. Am. J. Public Health 2016, 106, 1815–1819. [Google Scholar] [CrossRef]
- Anekwe, A.; Lent, M.; Farley, S.; Kessler, K.; Kennelly, M.; Angell, S. New York city’s sodium warning regulation: From conception to enforcement. Am. J. Public Health 2019, 109. [Google Scholar] [CrossRef]
- Iwahori, T.; Ueshima, H.; Ohgami, N.; Yamashita, H.; Miyagawa, N.; Kondo, K.; Torii, S.; Yoshita, K.; Shiga, T.; Ohkubo, T.; et al. Effectiveness of a self-monitoring device for urinary sodium-to-potassium ratio on dietary improvement in free-living adults: A randomized controlled trial. J. Epidemiol. 2018, 28. [Google Scholar] [CrossRef]
- He, F.J.; Zhang, P.; Luo, R.; Li, Y.; Chen, F.; Zhao, Y.; Zhao, W.; Li, D.; Chen, H.; Wu, T.; et al. An application-based programme to reinforce and maintain lower salt intake (AppSalt) in schoolchildren and their families in China. BMJ Open 2019, 9. [Google Scholar] [CrossRef] [PubMed]
| United Kingdom | South Korea |
|---|---|
| Start date: 2003/2004 | Start date: 2012 |
| Target: Reduce the population average salt intake to 6 g/day | Target: Reduce population sodium consumption by 20%, to 3900 mg/day, by 2020 |
| Package components: | Package components: |
|
|
|
|
|
|
|
|
|
|
| Results: | Results: |
|
|
|
|
| Sodium from packaged foods |
| Labeling: front-of-pack labeling regulations |
| Labeling: mandatory nutrient declaration on labels |
| Labeling: regulating nutrition/health claims on food packaging |
| Food reformulation targets for packaged food (voluntary or mandatory) |
| Regulation of marketing of foods and nonalcoholic beverages to children |
| Fiscal policies: taxation on high sodium foods |
| Supermarket interventions using product, placement, price, or promotion strategies (4Ps) |
| Sodium from food prepared outside the home |
| Standards for sodium as part of food procurement policies for public institutions |
| Restaurants: menu labeling of high or low sodium items (primarily chain restaurants) |
| Restaurants: removal of salt shakers and high sodium condiments from tables |
| Restaurants: chef training on reducing sodium in food |
| Restaurants: requiring the provision of low sodium or no-sodium added items on menus |
| Restaurants: food reformulation targets for restaurants (voluntary or mandatory; primarily chain restaurants) |
| Sodium added in the home |
| Mass media campaigns |
| Community education (e.g., through schools, community groups, workplaces, etc.) |
| Individual education and counselling (usually through primary health care) |
| Increase uptake of low sodium salt (promotion, distribution, subsidies) |
| Scalable and Sustainable | Evidence of Effectiveness or Innovation | Large Benefit | ||
|---|---|---|---|---|
| Sodium consumed from packaged foods | ||||
| Front-of-pack labeling regulations | ✓ | Suggestive evidence of effectiveness | Modeling studies available | |
| Theoretically large benefit | ||||
| Food reformulation targets for packaged food (voluntary or mandatory) | ✓ | Rigorously evaluated | Impact evaluations conducted on sodium and health outcomes | |
| Regulation of marketing of foods and nonalcoholic beverages to children | ✓ | Suggestive evidence of effectiveness | Theoretically large benefit | |
| Fiscal policies: taxation on high sodium foods | ✓ | Suggestive evidence for sodium, rigorously evaluated for other topic areas (e.g., sugar sweetened beverages) | Modeling studies available | |
| Theoretically large benefit | ||||
| Sodium consumed from food prepared outside the home | ||||
| Standards for sodium as part of food procurement policies for public institutions | ✓ | Suggestive evidence of effectiveness | Modeling studies available | |
| Theoretically large benefit | ||||
| Sodium consumed at home | ||||
| Mass media campaigns | ✓ 1 | Some suggestive evidence of effectiveness, rigorously evaluated for other topic areas (e.g., tobacco) | Theoretically large benefit | |
| Increase uptake of low-sodium salt (promotion, distribution, subsidies) | ✓ | Innovative approach for sodium added at home | Modeling studies available | |
| Theoretically large benefit |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ide, N.; Ajenikoko, A.; Steele, L.; Cohn, J.; J. Curtis, C.; Frieden, T.R.; Cobb, L.K. Priority Actions to Advance Population Sodium Reduction. Nutrients 2020, 12, 2543. https://doi.org/10.3390/nu12092543
Ide N, Ajenikoko A, Steele L, Cohn J, J. Curtis C, Frieden TR, Cobb LK. Priority Actions to Advance Population Sodium Reduction. Nutrients. 2020; 12(9):2543. https://doi.org/10.3390/nu12092543
Chicago/Turabian StyleIde, Nicole, Adefunke Ajenikoko, Lindsay Steele, Jennifer Cohn, Christine J. Curtis, Thomas R. Frieden, and Laura K. Cobb. 2020. "Priority Actions to Advance Population Sodium Reduction" Nutrients 12, no. 9: 2543. https://doi.org/10.3390/nu12092543
APA StyleIde, N., Ajenikoko, A., Steele, L., Cohn, J., J. Curtis, C., Frieden, T. R., & Cobb, L. K. (2020). Priority Actions to Advance Population Sodium Reduction. Nutrients, 12(9), 2543. https://doi.org/10.3390/nu12092543