Nutrihealth Study: Seasonal Variation in Vitamin D Status Among the Slovenian Adult and Elderly Population
Abstract
1. Introduction
2. Experimental Section
2.1. Study Design and Data Collection
2.2. Study Population
2.3. Serum 25(OH)D Concentration
2.4. Statistical Analysis
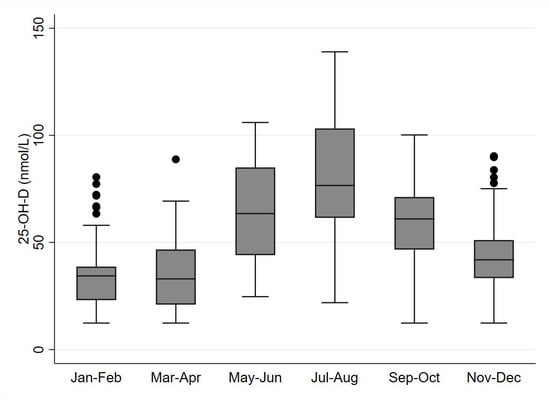
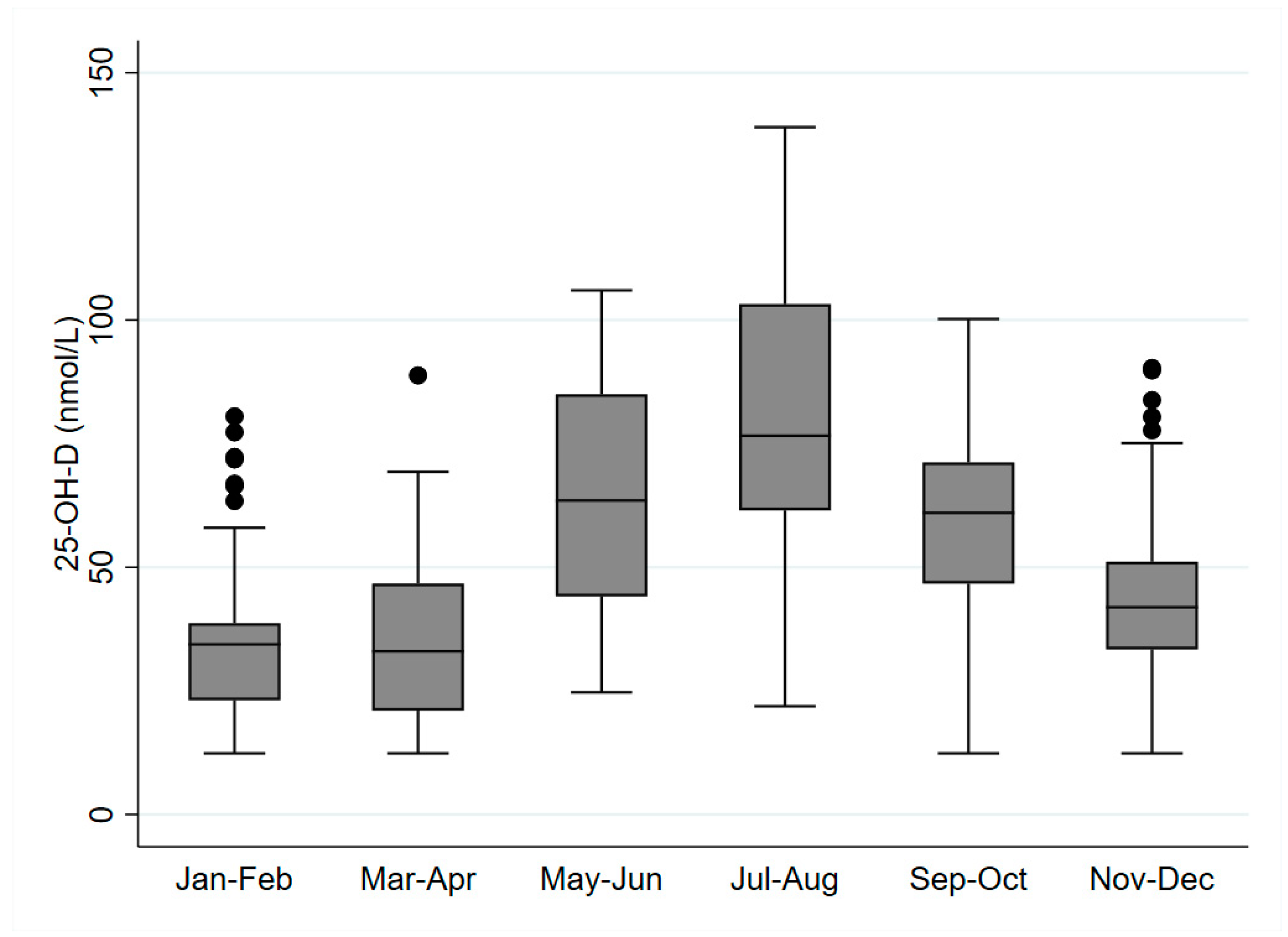
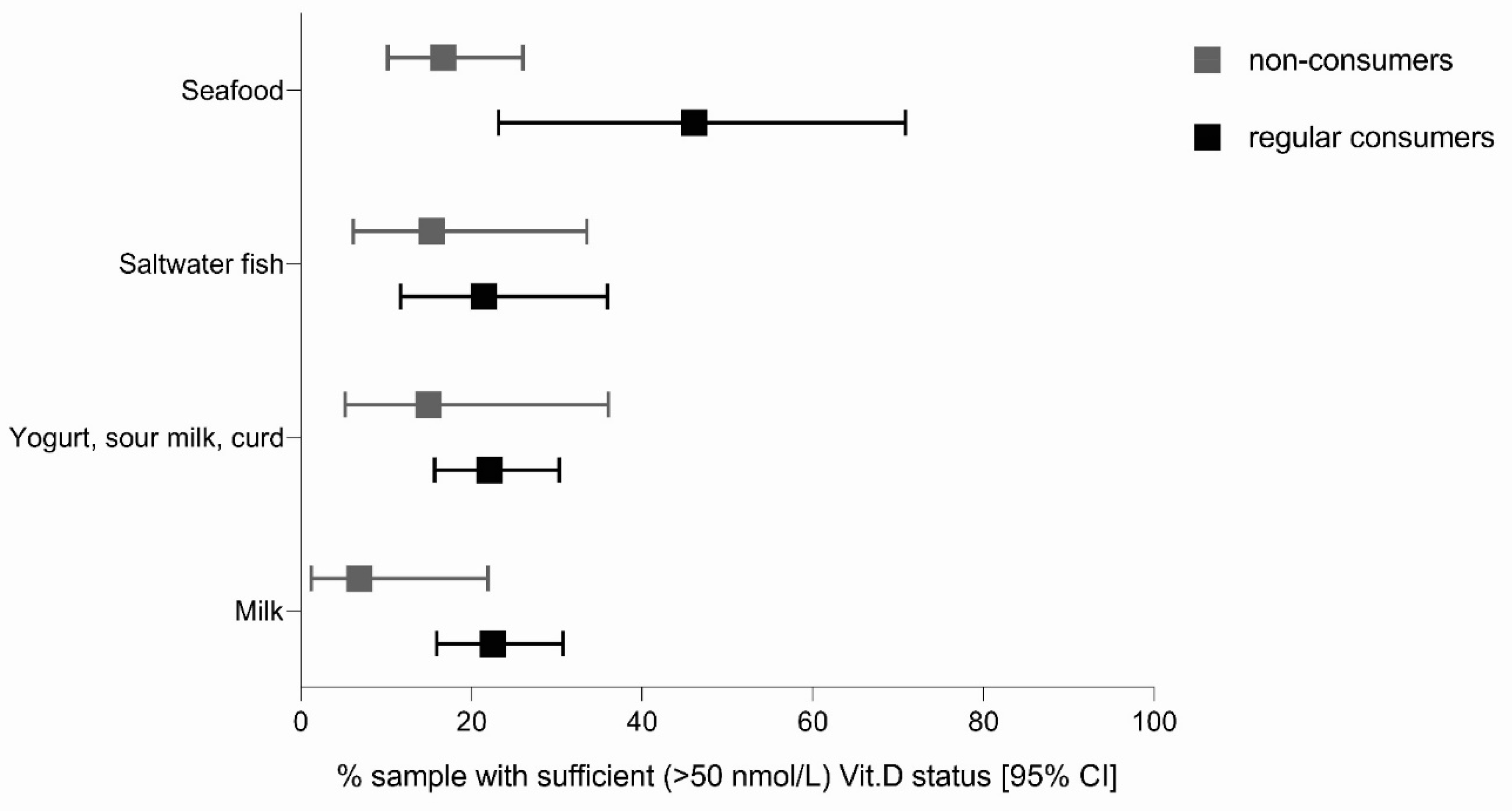
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Spiro, A.; Buttriss, J.L. Vitamin D: An overview of vitamin D status and intake in Europe. Nutr. Bull. 2014, 39, 322–350. [Google Scholar] [CrossRef] [PubMed]
- Cashman, K.D.; Dowling, K.G.; Skrabakova, Z.; Gonzalez-Gross, M.; Valtuena, J.; De Henauw, S.; Moreno, L.; Damsgaard, C.T.; Michaelsen, K.F.; Molgaard, C.; et al. Vitamin D deficiency in Europe: Pandemic? Am. J. Clin. Nutr. 2016, 103, 1033–1044. [Google Scholar] [CrossRef] [PubMed]
- Palacios, C.; Gonzalez, L. Is vitamin D deficiency a major global public health problem? J. Steroid Biochem. Mol. Biol. 2014, 144 (Pt A), 138–145. [Google Scholar] [CrossRef]
- Holick, M.F. The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Rev. Endocr. Metab. Disord. 2017, 18, 153–165. [Google Scholar] [CrossRef]
- Kiely, M.; Cashman, K.D. Summary Outcomes of the ODIN Project on Food Fortification for Vitamin D Deficiency Prevention. Int. J. Environ. Res. Public Health 2018, 15, 2342. [Google Scholar] [CrossRef] [PubMed]
- Lips, P. Vitamin D status and nutrition in Europe and Asia. J. Steroid Biochem. Mol. Biol. 2007, 103, 620–625. [Google Scholar] [CrossRef]
- Pludowski, P.; Grant, W.B.; Bhattoa, H.P.; Bayer, M.; Povoroznyuk, V.; Rudenka, E.; Ramanau, H.; Varbiro, S.; Rudenka, A.; Karczmarewicz, E.; et al. Vitamin d status in central europe. Int. J. Endocrinol. 2014, 2014, 589587. [Google Scholar] [CrossRef]
- Manios, Y.; Moschonis, G.; Lambrinou, C.P.; Tsoutsoulopoulou, K.; Binou, P.; Karachaliou, A.; Breidenassel, C.; Gonzalez-Gross, M.; Kiely, M.; Cashman, K.D. A systematic review of vitamin D status in southern European countries. Eur. J. Nutr. 2018, 57, 2001–2036. [Google Scholar] [CrossRef]
- Holick, M.F. The vitamin D deficiency pandemic and consequences for nonskeletal health: Mechanisms of action. Mol. Aspects Med. 2008, 29, 361–368. [Google Scholar] [CrossRef]
- Molina, P.; Carrero, J.J.; Bover, J.; Chauveau, P.; Mazzaferro, S.; Torres, P.U.; European Renal, N.; Chronic Kidney, D.-M.; Bone Disorder Working Groups of the European Renal Association-European Dialysis Transplant Association. Vitamin D, a modulator of musculoskeletal health in chronic kidney disease. J. Cachexia Sarcopenia Muscle 2017, 8, 686–701. [Google Scholar] [CrossRef]
- Autier, P.; Mullie, P.; Macacu, A.; Dragomir, M.; Boniol, M.; Coppens, K.; Pizot, C.; Boniol, M. Effect of vitamin D supplementation on non-skeletal disorders: A systematic review of meta-analyses and randomised trials. Lancet Diabetes Endocrinol. 2017, 5, 986–1004. [Google Scholar] [CrossRef]
- EFSA Scientific Panel NDA. Scientific Opinion on the substantiation of a health claim related to vitamin D and contribution to the normal function of the immune system pursuant to Article 14 of Regulation (EC) No. 1924/2006. EFSA J. 2015, 13, 7. [Google Scholar]
- Lips, P. Vitamin D Deficiency and Secondary Hyperparathyroidism in the Elderly: Consequences for Bone Loss and Fractures and Therapeutic Implications. Endocr. Rev. 2001, 22, 477–501. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Vitamin D and Health: Evolution, Biologic Functions, and Recommended Dietary Intakes for Vitamin D; Clinic. Rev. Bone. Miner. Metab. 2009, 7, 2–19. [Google Scholar] [CrossRef]
- O’Connor, A.; Benelam, B. An update on UK Vitamin D intakes and status, and issues for food fortification and supplementation. Nutr. Bull. 2011, 36, 390–396. [Google Scholar] [CrossRef]
- Bleizgys, A.; Kurovskij, J. Vitamin D Levels of Out-Patients in Lithuania: Deficiency and Hypervitaminosis. Medicina 2018, 54, 25. [Google Scholar] [CrossRef]
- Holick, M.F. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am. J. Clin. Nutr. 2004, 80, 1678S–1688S. [Google Scholar] [CrossRef]
- Kimlin, M.G. Geographic location and vitamin D synthesis. Mol. Aspects Med. 2008, 29, 453–461. [Google Scholar] [CrossRef]
- O’Neill, C.M.; Kazantzidis, A.; Ryan, M.J.; Barber, N.; Sempos, C.T.; Durazo-Arvizu, R.A.; Jorde, R.; Grimnes, G.; Eiriksdottir, G.; Gudnason, V.; et al. Seasonal Changes in Vitamin D-Effective UVB Availability in Europe and Associations with Population Serum 25-Hydroxyvitamin D. Nutrients 2016, 8, 533. [Google Scholar] [CrossRef]
- Roseland, J.M.; Phillips, K.M.; Patterson, K.Y.; Pehrsson, P.R.; Taylor, C.L. Chapter 60–Vitamin D in Foods: An Evolution of Knowledge. In Vitamin D, 4th ed.; Feldman, D., Ed.; Academic Press: Cambridge, MA, USA, 2018; pp. 41–77. [Google Scholar]
- Bouillon, R. Comparative analysis of nutritional guidelines for vitamin D. Nat. Rev. Endocrinol. 2017, 13, 466–479. [Google Scholar] [CrossRef]
- World Health Organization; Food and Agriculture Organization of the United Nations. Vitamin and Mineral Requirements in Human Nutrition: Report of a Joint FAO/WHO Expert Consultation, Bangkok, Thailand, 21–30 September 1998, 2nd ed.; World Health Organization: Geneva, Switzerland; FAO: Rome, Italy, 2004; p. xix. 341p. [Google Scholar]
- German Nutrition Society. New reference values for vitamin D. Ann. Nutr. Metab. 2012, 60, 241–246. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Dietetic Products, N.a.A.N. Dietary reference values for vitamin D. EFSA J. 2016, 14, e04547. [Google Scholar] [CrossRef]
- Roman Vinas, B.; Ribas Barba, L.; Ngo, J.; Gurinovic, M.; Novakovic, R.; Cavelaars, A.; de Groot, L.C.; van’t Veer, P.; Matthys, C.; Serra Majem, L. Projected prevalence of inadequate nutrient intakes in Europe. Ann. Nutr. Metab. 2011, 59, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Lichthammer, A.; Nagy, B.; Orbán, C.; Tóth, T.; Csajbók, R.; Molnár, S.; Tátrai-Nèmeth, K.; Bálint, M.V. A comparative study of eating habits, calcium and vitamin D intakes in the population of Central-Eastern European countries. New Med. 2015, 2, 66–70. [Google Scholar]
- Seamans, K.M.; Cashman, K.D. Existing and potentially novel functional markers of vitamin D status: A systematic review. Am. J. Clin. Nutr. 2009, 89, 1997S–2008S. [Google Scholar] [CrossRef]
- Institute of Medicine Committee to Review Dietary Reference Intakes for Vitamin D and Calcium. The National Academies Collection: Reports funded by National Institutes of Health. In Dietary Reference Intakes for Calcium and Vitamin D; Ross, A.C., Taylor, C.L., Yaktine, A.L., Del Valle, H.B., Eds.; National Academies Press (US), National Academy of Sciences: Washington, DC, USA, 2011. [Google Scholar]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M.; Endocrine, S. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef]
- Lips, P.; Cashman, K.D.; Lamberg-Allardt, C.; Bischoff-Ferrari, H.A.; Obermayer-Pietsch, B.; Bianchi, M.L.; Stepan, J.; El-Hajj Fuleihan, G.; Bouillon, R. Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: A position statement of the European Calcified Tissue Society. Eur. J. Endocrinol. 2019, 180, P23–P54. [Google Scholar] [CrossRef]
- Cesareo, R.; Attanasio, R.; Caputo, M.; Castello, R.; Chiodini, I.; Falchetti, A.; Guglielmi, R.; Papini, E.; Santonati, A.; Scillitani, A.; et al. Italian Association of Clinical Endocrinologists (AME) and Italian Chapter of the American Association of Clinical Endocrinologists (AACE) Position Statement: Clinical Management of Vitamin D Deficiency in Adults. Nutrients 2018, 10, 546. [Google Scholar] [CrossRef]
- Dovnik, A.; Mujezinović, F.; Treiber, M.; Pečovnik Balon, B.; Gorenjak, M.; Maver, U.; Takač, I. Seasonal variations of vitamin D concentrations in pregnant women and neonates in Slovenia. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 181, 6–9. [Google Scholar] [CrossRef]
- Soltirovska Salamon, A.; Benedik, E.; Bratanic, B.; Velkavrh, M.; Rogelj, I.; Fidler Mis, N.; Bogovic Matijasic, B.; Paro-Panjan, D. Vitamin D Status and Its Determinants in Healthy Slovenian Pregnant Women. Ann. Nutr. Metab. 2015, 67, 96–103. [Google Scholar] [CrossRef]
- Kudlacek, S.; Schneider, B.; Peterlik, M.; Leb, G.; Klaushofer, K.; Weber, K.; Woloszczuk, W.; Willvonseder, R. Assessment of vitamin D and calcium status in healthy adult Austrians. Eur. J. Clin. Investig. 2003, 33, 323–331. [Google Scholar] [CrossRef] [PubMed]
- European Food Safety Authority. Guidance on the EU Menu methodology. EFSA J. 2014, 15, 3944. [Google Scholar]
- Gregorič, M.; Blaznik, U.; Delfar, N.; Zaletel, M.; Lavtar, D.; Koroušić Seljak, B.; Golja, P.; Zdešar Kotnik, K.; Pravst, I.; Fidler Mis, N.; et al. Slovenian national food consumption survey in adolescents, adults and elderly. EFSA Supporting Publ. 2019, EN-1729, 28. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Ross, A.C.; Manson, J.E.; Abrams, S.A.; Aloia, J.F.; Brannon, P.M.; Clinton, S.K.; Durazo-Arvizu, R.A.; Gallagher, J.C.; Gallo, R.L.; Jones, G.; et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: What clinicians need to know. J. Clin. Endocrinol. Metab. 2011, 96, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Souberbielle, J.-C.; Massart, C.; Brailly-Tabard, S.; Cavalier, E.; Chanson, P. Prevalence and determinants of vitamin D deficiency in healthy French adults: The VARIETE study. Endocrine 2016, 53, 543–550. [Google Scholar] [CrossRef] [PubMed]
- Povoroznyuk, V.V.; Balatska, N.I.; Muts, V.Y.; Klymovytsky, F.V.; Synenky, O.V. Vitamin D deficiency in Ukraine: A demographic and seasonal analysis. Gerontologija 2012, 13, 191–198. [Google Scholar]
- Forrest, K.Y.; Stuhldreher, W.L. Prevalence and correlates of vitamin D deficiency in US adults. Nutr. Res. 2011, 31, 48–54. [Google Scholar] [CrossRef]
- Yu, S.; Fang, H.; Han, J.; Cheng, X.; Xia, L.; Li, S.; Liu, M.; Tao, Z.; Wang, L.; Hou, L.; et al. The high prevalence of hypovitaminosis D in China: A multicenter vitamin D status survey. Medicine 2015, 94, e585. [Google Scholar] [CrossRef]
- Chen, J.; Yun, C.; He, Y.; Piao, J.; Yang, L.; Yang, X. Vitamin D status among the elderly Chinese population: A cross-sectional analysis of the 2010-2013 China national nutrition and health survey (CNNHS). Nutr. J. 2017, 16, 3. [Google Scholar] [CrossRef]
- Gill, T.K.; Hill, C.L.; Shanahan, E.M.; Taylor, A.W.; Appleton, S.L.; Grant, J.F.; Shi, Z.; Dal Grande, E.; Price, K.; Adams, R.J. Vitamin D levels in an Australian population. BMC Public Health 2014, 14, 1001. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Worldwide Prevalence of Anaemia 1993–2005: WHO Global Database on Anaemia; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Antonucci, R.; Locci, C.; Clemente, M.G.; Chicconi, E.; Antonucci, L. Vitamin D deficiency in childhood: Old lessons and current challenges. J. Pediatr. Endocrinol. Metab. 2018, 31, 247–260. [Google Scholar] [CrossRef] [PubMed]
- Duarte, C.; Carvalheiro, H.; Rodrigues, A.M.; Dias, S.S.; Marques, A.; Santiago, T.; Canhao, H.; Branco, J.C.; da Silva, J.A.P. Prevalence of vitamin D deficiency and its predictors in the Portuguese population: A nationwide population-based study. Arch. Osteoporos. 2020, 15, 36. [Google Scholar] [CrossRef]
- Webb, A.R.; Kline, L.; Holick, M.F. Influence of season and latitude on the cutaneous synthesis of vitamin D3: Exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. J. Clin. Endocrinol. Metab. 1988, 67, 373–378. [Google Scholar] [CrossRef]
- Daly, R.M.; Gagnon, C.; Lu, Z.X.; Magliano, D.J.; Dunstan, D.W.; Sikaris, K.A.; Zimmet, P.Z.; Ebeling, P.R.; Shaw, J.E. Prevalence of vitamin D deficiency and its determinants in Australian adults aged 25 years and older: A national, population-based study. Clin. Endocrinol. 2012, 77, 26–35. [Google Scholar] [CrossRef]
- Bolland, M.J.; Chiu, W.W.; Davidson, J.S.; Grey, A.; Bacon, C.; Gamble, G.D.; Reid, I.R. The effects of seasonal variation of 25-hydroxyvitamin D and fat mass on diagnosis of vitamin D insufficiency. N. Z. Med. J. 2008, 121, 63–74. [Google Scholar]
- Chang, S.W.; Lee, H.C. Vitamin D and health—The missing vitamin in humans. Pediatr. Neonatol. 2019, 60, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Osredkar, J.; Marc, J. Vitamin D and metabolites: Physiology, pathophisiology and reference values. Med. Razgl. 1996, 35, 543–565. [Google Scholar]
- McKenna, M.J. Differences in vitamin D status between countries in young adults and the elderly. Am. J. Med. 1992, 93, 69–77. [Google Scholar] [CrossRef]
- Brouwer-Brolsma, E.M.; Vaes, A.M.M.; van der Zwaluw, N.L.; van Wijngaarden, J.P.; Swart, K.M.A.; Ham, A.C.; van Dijk, S.C.; Enneman, A.W.; Sohl, E.; van Schoor, N.M.; et al. Relative importance of summer sun exposure, vitamin D intake, and genes to vitamin D status in Dutch older adults: The B-PROOF study. J. Steroid Biochem. Mol. Biol. 2016, 164, 168–176. [Google Scholar] [CrossRef]
- MacLaughlin, J.; Holick, M.F. Aging decreases the capacity of human skin to produce vitamin D3. J. Clin. Investig. 1985, 76, 1536–1538. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.; Amaral, T.F.; Guerra, R.S.; Sousa, A.S.; Alvares, L.; Moreira, P.; Padrao, P.; Afonso, C.; Borges, N. Vitamin D status and associated factors among Portuguese older adults: Results from the Nutrition UP 65 cross-sectional study. BMJ Open 2017, 7, e016123. [Google Scholar] [CrossRef]
- Ter Borg, S.; Verlaan, S.; Hemsworth, J.; Mijnarends, D.M.; Schols, J.M.; Luiking, Y.C.; de Groot, L.C. Micronutrient intakes and potential inadequacies of community-dwelling older adults: A systematic review. Br. J. Nutr. 2015, 113, 1195–1206. [Google Scholar] [CrossRef]
- Laktasic-Zerjavic, N.; Korsic, M.; Crncevic-Orlic, Z.; Kovac, Z.; Polasek, O.; Soldo-Juresa, D. Vitamin D status, dependence on age, and seasonal variations in the concentration of vitamin D in Croatian postmenopausal women initially screened for osteoporosis. Clin. Rheumatol. 2010, 29, 861–867. [Google Scholar] [CrossRef] [PubMed]
- Touvier, M.; Deschasaux, M.; Montourcy, M.; Sutton, A.; Charnaux, N.; Kesse-Guyot, E.; Assmann, K.E.; Fezeu, L.; Latino-Martel, P.; Druesne-Pecollo, N.; et al. Determinants of vitamin D status in Caucasian adults: Influence of sun exposure, dietary intake, sociodemographic, lifestyle, anthropometric, and genetic factors. J. Investig. Dermatol. 2015, 135, 378–388. [Google Scholar] [CrossRef]
- Sanghera, D.K.; Sapkota, B.R.; Aston, C.E.; Blackett, P.R. Vitamin D Status, Gender Differences, and Cardiometabolic Health Disparities. Ann. Nutr. Metab. 2017, 70, 79–87. [Google Scholar] [CrossRef] [PubMed]
- AlQuaiz, A.M.; Kazi, A.; Fouda, M.; Alyousefi, N. Age and gender differences in the prevalence and correlates of vitamin D deficiency. Arch. Osteoporos. 2018, 13, 49. [Google Scholar] [CrossRef]
- Wortsman, J.; Matsuoka, L.Y.; Chen, T.C.; Lu, Z.; Holick, M.F. Decreased bioavailability of vitamin D in obesity. Am. J. Clin. Nutr. 2000, 72, 690–693. [Google Scholar] [CrossRef]
- Zmitek, K.; Hribar, M.; Hristov, H.; Pravst, I. Efficiency of Vitamin D Supplementation in Healthy Adults is Associated with Body Mass Index and Baseline Serum 25-Hydroxyvitamin D Level. Nutrients 2020, 12, 1268. [Google Scholar] [CrossRef]
- Scragg, R.; Camargo, C.A., Jr. Frequency of leisure-time physical activity and serum 25-hydroxyvitamin D levels in the US population: Results from the Third National Health and Nutrition Examination Survey. Am. J. Epidemiol. 2008, 168, 577–586. [Google Scholar] [CrossRef]
| Variable | Adults | Elderly | |
|---|---|---|---|
| (18–64 Years Old) | (65–74 Years Old) | ||
| N = 125 | N = 155 | ||
| Age (mean ± SD) | 46.5 (13.2) | 68.6 (2.8) | |
| Residential area (%) | village | 50.4 | 54.2 |
| town | 15.2 | 15.5 | |
| city | 34.4 | 30.3 | |
| Sex (%) | male | 41.6 | 49 |
| female | 58.4 | 51 | |
| Education (%) | primary school | 8.8 | 19.4 |
| high school | 60 | 55.5 | |
| higher education | 31.2 | 25.1 | |
| Monthly net income (%) | ≤900 € | 20.3 | 32.2 |
| 900–1800 € | 47.8 | 55 | |
| >1800 € | 31.9 | 12.8 | |
| Season (%) | November–April | 58.4 | 58.7 |
| May–October | 41.6 | 41.3 | |
| BMI (mean ± SD) | 27.6 (5.5) | 27.9 (4.7) | |
| BMI (%) | <25 | 39.2 | 29.7 |
| ≥25 | 60.8 | 70.3 | |
| Smoking status (%) | current smoker | 17.6 | 11.6 |
| ex-/non-smoker | 82.4 | 88.4 | |
| Physical activity * (%) | low level | 31.2 | 33.1 |
| moderate level | 32 | 31.8 | |
| high level | 36.8 | 35.1 | |
| Vitamin D supplement use (%) | users | 8.8 | 8.4 |
| non-users | 91.2 | 91.6 | |
| N (%) * | Serum 25(OH)D Level (nmol/L) | Prevalence (%) | |||||
|---|---|---|---|---|---|---|---|
| Mean | S.E. | Median | <30 nmol/L | <50 nmol/L | <75 nmol/L | ||
| Adults | 125 (100) | 50.7 (45.4–56.0) | 2.7 | 45.3 | 24.9 (17.5–34.1) | 58.2 (48.5–67.3) | 83.3(74.9–89.2) |
| -Male | 52 (41.6) | 55.3 (46.4–64.1) | 4.5 | 50.7 | 22.8 (12.6–37.8) | 50.0 (35.4–64.6) | 79.6 (65.7–88.8) |
| -Female | 73 (58.4) | 46.2 (40.4–51.9) | 2.9 | 43.8 | 27.0 (17.6–39.0) | 66.4 (54.3–76.7) | 86.9 (76.1–93.2) |
| Elderly | 155 (100) | 47.7 (43.9–51.5) | 1.9 | 42.4 | 23.5 (17.4–30.9) | 62.9 (54.9–70.2) | 84.4 (77.8–89.4) |
| -Male | 76 (49.0) | 48.2 (43.0–53.3) | 2.6 | 42.1 | 19.1 (11.8–29.5) | 60.3 (48.7–70.7) | 84.9 (74.7–91.5) |
| -Female | 79 (51.0) | 47.3 (41.8–52.8) | 2.8 | 43.1 | 27.5 (18.6–38.5) | 65.2 (54.1–74.9) | 84.0 (74.2–90.5) |
| Extended Summer: May–October | Extended Winter: November–April | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N (%) * | Serum 25(OH)D Level (nmol/L) | Prevalence (%) | N (%) * | Serum 25(OH)D Level (nmol/L) | Prevalence (%) | |||||||||
| Mean | S.E. | Med. | <30 nmol/L | <50 nmol/L | <75 nmol/L | Mean | S.E. | Med. | <30 nmol/L | <50 nmol/L | <75 nmol/L | |||
| Adults | 52 (100) | 70.4 (62.2–78.5) | 4.1 | 64.0 | 2.6 (0.6–10.2) | 25.3 (14.8–39.9) | 62.6 (47.4–75.6) | 73 (100) | 36.7 (32.5–40.9) | 2.1 | 34.4 | 40.8 (29.0–53.7) | 81.6 (69.4–89.7) | 98.0 (92.2–99.5) |
| - Male | 22 (42.3) | 76.2 (62.4–90.1) | 6.9 | 71.2 | 2.8 (0.3–18.3) | 16.1 (4.9–41.5) | 56.6 (34.1–76.6) | 30 (41.1) | 40.3 (33.3–47.3) | 3.5 | 37.6 | 37.1 (20.4–57.6) | 74.2 (53.3–87.8) | 96.0 (84.9–99.0) |
| - Female | 30 (57.7) | 64.5 (56.5–72.5) | 4.0 | 63.0 | 2.4 (0.3–15.8) | 34.6 (19.5–53.6) | 68.5 (48.8–83.3) | 43 (58.9) | 33.1 (28.8–37.4) | 2.2 | 32.8 | 44.5 (29.7–60.3) | 89.1 (76.9–95.3) | 100 |
| Elderly | 64 (100) | 60.1 (54.0–66.2) | 3.1 | 57.0 | 7.8 (3.2–17.5) | 40.2 (28.8–52.7) | 73.4 (61.1–82.9) | 91 (100) | 39.0 (35.0–43.0) | 2.0 | 37.4 | 34.6 (25.4–45.1) | 78.8 (69.0–86.1) | 92.2 (84.4–96.3) |
| - Male | 29 (45.3) | 62.6 (54.4–70.8) | 4.1 | 58.5 | 6.9 (1.7–24.1) | 27.6 (14.3–46.5) | 72.4 (53.5–85.7) | 47 (51.7) | 38.2 (33.3–43.0) | 2.4 | 38.1 | 27.7 (16.7–42.2) | 83.0 (69.3–91.3) | 93.6 (81.8–98.0) |
| - Female | 35 (54.7) | 57.9 (49.0–66.9) | 4.5 | 47.9 | 8.6 (2.7–23.8) | 51.4 (35.1–67.5) | 74.3 (57.2–86.2) | 44 (48.3) | 39.8 (33.6–46.0) | 3.1 | 36.5 | 40.9 (27.4–56.0) | 75.0 (60.1–85.7) | 90.9 (78.0–96.6) |
| Variable | Adults | Elderly | |||||
|---|---|---|---|---|---|---|---|
| N | Prevalence N (%) | Odds Ratio | N | Prevalence N (%) | Odds Ratio | ||
| Overall | 125 | 73 (58.4) | 155 | 98 (63.2) | |||
| Place of living | village | 63 | 35 (55.6) | 1.80 (0.57–5.64) | 84 | 52 (61.9) | 0.49 (0.18–1.35) |
| town | 19 | 14 (73.7) | 3.77 (0.58–24.51) | 24 | 15 (62.5) | 0.87 (0.24–3.15) | |
| city | 43 | 24 (55.8) | 1 | 47 | 31 (66.0) | 1 | |
| Sex | male | 52 | 25 (48.1) | 1 | 76 | 47 (61.8) | 1 |
| female | 73 | 48 (65.8) | 3.36 (1.05–10.74) | 79 | 51 (64.56) | 1.94 (0.80–4.69) | |
| Education | elementary school | 11 | 7 (63.6) | 3.23 (0.47–22.19) | 30 | 23 (76.7) | 1.16 (0.33–4.00) |
| high school | 75 | 42 (56) | 1 | 86 | 53 (61.6) | 1 | |
| higher education | 39 | 24 (61.5) | 2.19 (0.58–8.23) | 39 | 22 (56.4) | 0.56 (0.21–1.54) | |
| Family net income * | ≤900 € | 23 | 14 (60.9) | 1.57 (0.34–7.34) | 48 | 34 (70.8) | 1.75 (0.65–4.76) |
| 900–1800 € | 54 | 31 (57.4) | 1 | 82 | 49 (59.8) | 1 | |
| >1800 € | 36 | 21 (58.3) | 1.78 (0.51–6.25) | 19 | 13 (68.4) | 1.47 (0.38–5.65) | |
| Season | November–April | 73 | 59 (80.8) | 34.94 (9.22–132.50) | 91 | 72 (79.1) | 10.34 (4.10–26.07) |
| May–October | 52 | 14 (26.9) | 1 | 64 | 26 (40.6) | 1 | |
| BMI | <25 | 49 | 31 (63.3) | 1.68 (0.52–5.35) | 46 | 24 (52.2) | 0.31 (0.12–0.78) |
| ≥25 | 76 | 22 (51.2) | 1 | 109 | 34 (56.7) | 1 | |
| Smoking status | current smoker | 22 | 15 (56.3) | 1 | 18 | 11 (63.5) | 1 |
| ex-/non-smoker | 103 | 58 (68.2) | 5.01 (0.90–27.78) | 137 | 87 (61.1) | 1.40 (0.36–5.43) | |
| Physical activity | low level | 39 | 28 (71.8) | 5.59 (1.38–22.69) | 51 | 33 (64.7) | 1.78 (0.66–4.81) |
| moderate level | 40 | 20 (50.0) | 1 | 49 | 28 (57.1) | 1 | |
| high level | 46 | 25 (54.4) | 1.76 (0.44–7.05) | 54 | 36 (66.7) | 1.57 (0.59–4.22) | |
| Vitamin D supplement use | users | 11 | 5 (45.5) | 1 | 13 | 7 (53.9) | 1 |
| non-users | 114 | 68 (59.7) | 1.20 (0.17–8.25) | 142 | 91 (64.1) | 3.61 (0.82–15.92) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hribar, M.; Hristov, H.; Gregorič, M.; Blaznik, U.; Zaletel, K.; Oblak, A.; Osredkar, J.; Kušar, A.; Žmitek, K.; Rogelj, I.; et al. Nutrihealth Study: Seasonal Variation in Vitamin D Status Among the Slovenian Adult and Elderly Population. Nutrients 2020, 12, 1838. https://doi.org/10.3390/nu12061838
Hribar M, Hristov H, Gregorič M, Blaznik U, Zaletel K, Oblak A, Osredkar J, Kušar A, Žmitek K, Rogelj I, et al. Nutrihealth Study: Seasonal Variation in Vitamin D Status Among the Slovenian Adult and Elderly Population. Nutrients. 2020; 12(6):1838. https://doi.org/10.3390/nu12061838
Chicago/Turabian StyleHribar, Maša, Hristo Hristov, Matej Gregorič, Urška Blaznik, Katja Zaletel, Adrijana Oblak, Joško Osredkar, Anita Kušar, Katja Žmitek, Irena Rogelj, and et al. 2020. "Nutrihealth Study: Seasonal Variation in Vitamin D Status Among the Slovenian Adult and Elderly Population" Nutrients 12, no. 6: 1838. https://doi.org/10.3390/nu12061838
APA StyleHribar, M., Hristov, H., Gregorič, M., Blaznik, U., Zaletel, K., Oblak, A., Osredkar, J., Kušar, A., Žmitek, K., Rogelj, I., & Pravst, I. (2020). Nutrihealth Study: Seasonal Variation in Vitamin D Status Among the Slovenian Adult and Elderly Population. Nutrients, 12(6), 1838. https://doi.org/10.3390/nu12061838