Extrauterine Growth Restriction: Definitions and Predictability of Outcomes in a Cohort of Very Low Birth Weight Infants or Preterm Neonates
Abstract
1. Introduction
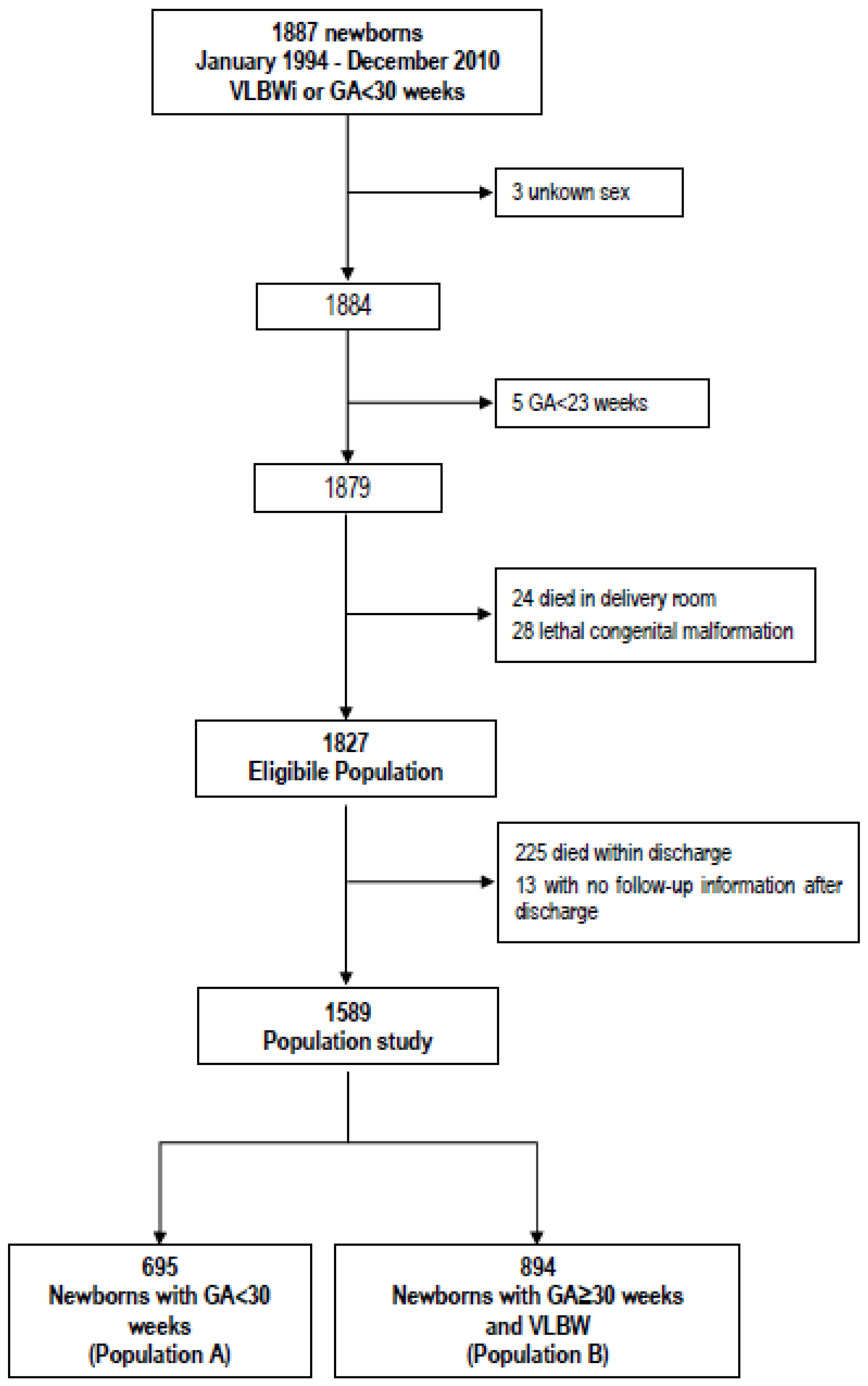
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Clark, R.H.; Thomas, P.; Peabody, J. Extrauterine Growth Restriction Remains a Serious Problem in Prematurely Born Neonates. Pediatrics 2003, 111, 986–990. [Google Scholar] [CrossRef]
- Ofek Shlomai, N.; Reichman, B.; Lerner-Geva, L.; Boyko, V.; Bar-Oz, B. Population-based study shows improved postnatal growth in preterm very-low-birthweight infants between 1995 and 2010. Acta Paediatr. 2014, 103, 498–503. [Google Scholar] [CrossRef] [PubMed]
- Griffin, I.J.; Tancredi, D.J.; Bertino, E.; Lee, H.C.; Profit, J. Postnatal growth failure in very low birthweight infants born between 2005 and 2012. Arch. Dis. Child.-Fetal Neonatal Ed. 2016, 101, F50–F55. [Google Scholar] [CrossRef] [PubMed]
- Shan, H.M.; Cai, W.; Cao, Y.; Fang, B.H.; Feng, Y. Extrauterine growth retardation in premature infants in Shanghai: A multicenter retrospective review. Eur. J. Pediatr. 2009, 168, 1055–1059. [Google Scholar] [CrossRef] [PubMed]
- Ruth, V.A. Extrauterine growth restriction: A review of the literature. Neonatal Netw. 2008, 27, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Jiménez, M.D.; Gómez-García, F.J.; Gil-Campos, M.; Pérez-Navero, J.L. Comorbidities in childhood associated with extrauterine growth restriction in preterm infants: A scoping review. Eur. J. Pediatr. 2020. [Google Scholar] [CrossRef]
- Leppänen, M.; Lapinleimu, H.; Lind, A.; Matomäki, J.; Lehtonen, L.; Haataja, L.; Rautava, P.; PIPARI Study Group. Antenatal and postnatal growth and 5-year cognitive outcome in very preterm infants. Pediatrics 2014, 133, 63–70. [Google Scholar] [CrossRef]
- Pampanini, V.; Boiani, A.; De Marchis, C.; Giacomozzi, C.; Navas, R.; Agostino, R.; Dini, F.; Ghirri, P.; Cianfarani, S. Preterm infants with severe extrauterine growth retardation (EUGR) are at high risk of growth impairment during childhood. Eur. J. Pediatr. 2015, 174, 33–41. [Google Scholar] [CrossRef]
- Chien, H.C.; Chen, C.H.; Wang, T.M.; Hsu, Y.C.; Lin, M.C. Neurodevelopmental outcomes of infants with very low birth weights are associated with the severity of their extra-uterine growth retardation. Pediatr. Neonatol. 2018, 59, 168–175. [Google Scholar] [CrossRef]
- Frondas-Chauty, A.; Simon, L.; Branger, B.; Gascoin, G.; Flamant, C.; Ancel, P.Y.; Darmaun, D.; Rozé, J.C. Early growth and neurodevelopmental outcome in very preterm infants: Impact of gender. Arch. Dis. Child.-Fetal Neonatal Ed. 2014, 99, F366–F372. [Google Scholar] [CrossRef]
- Ramel, S.E.; Demerath, E.W.; Gray, H.L.; Younge, N.; Boys, C.; Georgieff, M.K. The relationship of poor linear growth velocity with neonatal illness and two-year neurodevelopment in preterm infants. Neonatology 2012, 102, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Ehrenkranz, R.A.; Dusick, A.M.; Vohr, B.R.; Wright, L.L.; Wrage, L.A.; Poole, W.K. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics 2006, 117, 1253–1261. [Google Scholar] [CrossRef]
- Latal-Hajnal, B.; von Siebenthal, K.; Kovari, H.; Bucher, H.U.; Largo, R.H. Postnatal growth in VLBW infants: Significant association with neurodevelopmental outcome. J. Pediatr. 2003, 143, 163–170. [Google Scholar] [CrossRef]
- Casey, P.H.; Whiteside-Mansell, L.; Barrett, K.; Bradley, R.H.; Gargus, R. Impact of prenatal and/or postnatal growth problems in low birth weight preterm infants on school-age outcomes: An 8-year longitudinal evaluation. Pediatrics 2006, 118, 1078–1086. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.T.; Chen, C.H.; Lin, M.C.; Wang, T.M.; Hsu, Y.C. Post-discharge body weight and neurodevelopmental outcomes among very low birth weight infants in Taiwan: A nationwide cohort study. PLoS ONE 2018, 13, e0192574. [Google Scholar] [CrossRef]
- Li, Y.; Shah, M.; Miller, M.R.; Lee, D.S.C.; Sharan, S. Impact of Early Postnatal Weight Gain on Retinopathy of Prematurity in Very Preterm Infants in Southwestern Ontario. J. Pediatr. Ophthalmol. Strabismus 2019, 56, 168–172. [Google Scholar] [CrossRef]
- Finken, M.J.; Dekker, F.W.; de Zegher, F.; Wit, J.M. Dutch Project on Preterm and Small-for-Gestational-Age-19 Collaborative Study Group. Long-term height gain of prematurely born children with neonatal growth restraint: Parallellism with the growth pattern of short children born small for gestational age. Pediatrics 2006, 118, 640–643. [Google Scholar] [CrossRef]
- Bertino, E.; Di Nicola, P.; Occhi, L.; Prandi, G.; Gilli, G. Causes of postnatal growth failure in preterm infants. In Perinatal Growth and Nutrition; Griffin, I.J., Ed.; CRC Press: New York, NY, USA, 2014; pp. 41–60. [Google Scholar]
- Vermont Oxford Network. Manual of Operations: Part 2. Available online: https://vtoxford.zendesk.com/hc/en-us/articles/360013115393-2019-Manual-of-Operations-Part-2-Release-23-2-PDF- (accessed on 26 April 2020).
- Bertino, E.; Spada, E.; Occhi, L.; Coscia, A.; Giuliani, F.; Gagliardi, L.; Gilli, G.; Bona, G.; Fabris, C.; De Curtis, M.; et al. Neonatal anthropometric charts: The Italian neonatal study compared with other European studies. J. Pediatr. Gastroenterol. Nutr. 2010, 51, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Kuczmarski, R.J.; Ogden, C.L.; Guo, S.S.; Grummer-Strawn, L.M.; Flegal, K.M.; Mei, Z.; Wei, R.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. 2000 CDC growth charts for the United States: Methods and development. National Center for Health Statistics. Vital Health Stat. 2002, 11, 1–190. [Google Scholar]
- Radmacher, P.G.; Looney, S.W.; Rafail, S.T.; Adamkin, D.H. Prediction of extrauterine growth retardation (EUGR) in VLBW infants. J. Perinatol. 2003, 23, 392–395. [Google Scholar] [CrossRef] [PubMed]
- Karagol, B.S.; Zenciroglu, A.; Okumus, N.; Polin, R.A. Randomized Controlled Trial of Slow vs Rapid Enteral Feeding Advancements on the Clinical Outcomes of Preterm Infants With Birth Weight 750–1250 g. J. Parenter. Enteral Nutr. 2013, 37, 223–228. [Google Scholar] [CrossRef]
- Lemons, J.A.; Bauer, C.R.; Oh, W.; Korones, S.B.; Papile, L.A.; Stoll, B.J.; Verter, J.; Temprosa, M.; Wright, L.L.; Ehrenkranz, R.A.; et al. Very low birth weight outcomes of the National Institute of Child health and human development neonatal research network, January 1995 through December 1996. NICHD Neonatal Research Network. Pediatrics 2001, 107, e1–e2. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.R.; Brown, Y.F.; Ehrenkranz, R.A.; O’Shea, T.M.; Allred, E.N.; Belfort, M.B.; McCormick, M.C.; Leviton, A. Extremely Low Gestational Age Newborns Study Investigators. Nutritional practices and growth velocity in the first month of life in extremely premature infants. Pediatrics 2009, 124, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Franz, A.R.; Pohlandt, F.; Bode, H.; Mihatsch, W.A.; Sander, S.; Kron, M.; Steinmacher, J. Intrauterine, early neonatal, and postdischarge growth and neurodevelopmental outcome at 5.4 years in extremely preterm infants after intensive neonatal nutritional support. Pediatrics 2009, 123, e101–e109. [Google Scholar] [CrossRef] [PubMed]
- Marks, K.A.; Reichman, B.; Lusky, A.; Zmora, E. Israel Neonatal Network. Fetal growth and postnatal growth failure in very-low-birthweight infants. Acta Paediatr. 2006, 95, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Roggero, P.; Gianni, M.L.; Orsi, A.; Amato, O.; Piemontese, P.; Liotto, N.; Morlacchi, L.; Taroni, F.; Garavaglia, E.; Bracco, B.; et al. Implementation of nutritional strategies decreases postnatal growth restriction in preterm infants. PLoS ONE 2012, 7, e51166. [Google Scholar] [CrossRef] [PubMed]
- Bertino, E.; Coscia, A.; Mombro, M.; Boni, L.; Rossetti, G.; Fabris, C.; Spada, E.; Milani, S. Postnatal weight increase and growth velocity of very low birthweight infants. Arch. Dis. Child.-Fetal Neonatal Ed. 2006, 91, F349–F356. [Google Scholar] [CrossRef] [PubMed]
- Bertino, E.; Coscia, A.; Boni, L.; Rossi, C.; Martano, C.; Giuliani, F.; Fabris, C.; Spada, E.; Zolin, A.; Milani, S. Weight growth velocity of very low birth weight infants: Role of gender, gestational age and major morbidities. Early Hum. Dev. 2009, 85, 339–347. [Google Scholar] [CrossRef]
- Cole, T.J.; Statnikov, Y.; Santhakumaran, S.; Pan, H.; Modi, N.; On behalf of the Neonatal Data Analysis Unit and the Preterm Growth Investigator Group. Birth weight and longitudinal growth in infants born below 32 weeks’ gestation: A UK population study. Arch. Dis. Child.-Fetal Neonatal Ed. 2014, 99, F34–F40. [Google Scholar] [CrossRef]
- Bonnar, K.; Fraser, D. Extrauterine Growth Restriction in Low Birth Weight Infants. Neonatal Netw. 2019, 38, 27–33. [Google Scholar] [CrossRef]
| Population A (N = 695) | Population B (N = 894) | |
|---|---|---|
| Females, n (%) | 342 (49.2) | 492 (55.0) |
| Singleton, n (%) | 527 (75.8) | 588 (65.8) |
| Gestational Age (week), median (IQR) | 28 (27–29) | 31 (30–33) |
| Birth weight (g), mean (SD) | 991 (255) | 1251 (193) |
| Birth length (mm), mean (SD) | 356 (30) | 387 (22) |
| Head circumference (mm), mean (SD) | 252 (19) | 277 (14) |
| Birth weight (SDS), mean (SD) | −0.02 (0.946) | −1.29 (0.845) |
| Birth length (SDS), mean (SD) | −0.10 (0.928) | −1.09 (0.976) |
| Head circumference (SDS), mean (SD) | −0.06 (1.046) | −1.24 (1.013) |
| SGA, n (%) | 76 (10.9) | 459 (51.3) |
| LGA, n (%) | 51 (7.3) | 0 (0.0) |
| Antenatal steroids, n (%) * | 534 (86.1) | 647 (87.6) |
| Population A (N = 695) | Population B (N = 894) | |
|---|---|---|
| Major morbidities, n (%) | 621(89.4) | 349(39.0) |
| Late sepsis, n (%) | 120(17.3) | 34 (1.9) |
| NEC, n (%) | 18(2.6) | 17(3.8) |
| ROP, n (%) | 44(6.3) | 2(0.2) |
| BPD, n (%) | 24(3.5) | 5(0.6) |
| RDS, n (%) | 598(86.0) | 299(33.5) |
| MV, n (%) * | 568(83.5) | 231(28.9) |
| HFOV, n (%) ** | 67(10.9) | 10(1.3) |
| IVH, n (%) | 43(7.4) | 6(1.0) |
| PVL, n (%) | 32(5.7) | 19(3.2) |
| PDA, n (%) | 292(42.0) | 73(8.2) |
| Age at discharge in days | ||
| median (min-max) | 65 (24–137) | 39 (17–90) |
| EUGR Definition | Cross-sectional | Longitudinal | ||||||
|---|---|---|---|---|---|---|---|---|
| 36 Weeks | 40 Weeks | 28 Days | Discharge | 36 Weeks | 40 Weeks | 28 Days | Discharge | |
| Study population | ||||||||
| non-SGA, n (%) | 489/561 (87.2) | 163/262 (62.2) | 335/572 (58.6) | 565/732 (77.2) | 487/561 (86.8) | 179/262 (68.3) | 390/572 (68.2) | 626/732 (85.5) |
| SGA, n (%) | 340/340 (100.0) | 159/167 (95.2) | 250/250 (100.0) | 331/332 (99.7) | 109/340 (32.1) | 90/167 (53.9) | 62/250 (24.8) | 145/332 (43.7) |
| Population A | ||||||||
| non-SGA, n (%) | 268/331 (81.0) | 107/170 (62.9) | 168/358 (46.9) | 318/447 (71.1) | 312/331 (94.3) | 135/170 (79.4) | 260/358 (72.6) | 414/447 (92.6) |
| SGA, n (%) | 47/47 (100.0) | 43/43 (100.0) | 46/46 (100.0) | 49/49 (100.0) | 36/47 (76.6) | 42/43 (97.7) | 11/46 (23.9) | 43/49 (87.8) |
| Population B | ||||||||
| non-SGA, n (%) | 221/230 (96.1) | 56/92 (60.9) | 167/214 (78.0) | 247/285 (86.7) | 175/230 (76.1) | 44/92 (47.8) | 130/214 (60.8) | 212/285 (74.4) |
| SGA, n (%) | 293/293 (100.0) | 116/124 (93.6) | 204/204 (100.0) | 282/283 (99.7) | 73/293 (24.9) | 48/124 (38.7) | 51/204 (25.0) | 102/283 (36.0) |
| Study Population | Population A | Population B | |
|---|---|---|---|
| Weight (g), mean (SD) | 11,146 (1578) | 11,261 (1724) | 11,029 (1406) |
| Length (mm), mean (SD) | 853 (39) | 853 (39) | 853 (40) |
| Head circumference (mm), mean (SD) | 477 (18) | 477 (19) | 477 (17) |
| Weight (SDS), mean (SD) | −1.43 (1.373) | −1.39 (1.492) | −1.47 (1.240) |
| Length (SDS), mean (SD) | −0.94 (1.060) | −1.01 (1.057) | −0.86 (1.059) |
| Head circumference (SDS), mean (SD) | −0.41 (1.163) | −0.43 (1.231) | −0.39 (1.088) |
| TRAIT | EVALUATION | t | EUGR | |||
|---|---|---|---|---|---|---|
| No | Yes | No vs. Yes | p | |||
| WEIGHT | Cross- Sectional | 36 weeks of GA | −0.32 ± 0.192 | −0.67 ± 0.056 | +0.36 ± 0.201 | 0.077 |
| 40 weeks of GA | −0.57 ± 0.153 | −0.86 ± 0.086 | +0.29 ± 0.180 | 0.110 | ||
| 28 days | −0.95 ± 0.113 | −0.71 ± 0.065 | −0.24 ± 0.136 | 0.076 | ||
| discharge | −0.92 ± 0.121 | −0.65 ± 0.051 | −0.27 ± 0.133 | 0.043 | ||
| Longitudinal | 36 weeks of GA | −0.23 ± 0.112 | −0.82 ± 0.067 | +0.59 ± 0.141 | <0.001 | |
| 40 weeks of GA | −0.47 ± 0.130 | −0.95 ± 0.093 | +0.48 ± 0.166 | 0.004 | ||
| 28 days | −0.58 ± 0.087 | −0.93 ± 0.074 | +0.36 ± 0.120 | 0.003 | ||
| discharge | −0.38 ± 0.099 | −0.80 ± 0.055 | +0.42 ± 0.118 | <0.001 | ||
| LENGTH | Cross- Sectional | 36 weeks of GA | −0.09 ± 0.181 | −0.14 ± 0.050 | 0.05 ± 0.189 | 0.772 |
| 40 weeks of GA | −0.30 ± 0.129 | −0.27 ± 0.073 | −0.02 ± 0.152 | 0.872 | ||
| 28 days | −0.46 ± 0.103 | −0.19 ± 0.060 | −0.27 ± 0.125 | 0.030 | ||
| discharge | −0.61 ± 0.108 | −0.16 ± 0.046 | −0.45 ± 0.120 | <0.001 | ||
| Longitudinal | 36 weeks of GA | +0.02 ± 0.100 | −0.21 ± 0.061 | +0.23 ± 0.126 | 0.072 | |
| 40 weeks of GA | −0.11 ± 0.107 | −0.38 ± 0.079 | +0.27 ± 0.137 | 0.053 | ||
| 28 days | −0.18 ± 0.078 | −0.33 ± 0.069 | +0.15 ± 0.109 | 0.180 | ||
| discharge | −0.11 ± 0.089 | −0.29 ± 0.051 | +0.18 ± 0.107 | 0.094 | ||
| HEAD CIRCUMFERENCE | Cross- Sectional | 36 weeks of GA | +0.31 ± 0.159 | +0.33 ± 0.046 | −0.02 ± 0.167 | 0.924 |
| 40 weeks of GA | +0.20 ± 0.126 | +0.22 ± 0.071 | −0.01 ± 0.148 | 0.939 | ||
| 28 days | −0.01 ± 0.094 | +0.22 ± 0.053 | −0.23 ± 0.113 | 0.045 | ||
| discharge | +0.07 ± 0.104 | +0.32 ± 0.043 | −0.25 ± 0.114 | 0.029 | ||
| Longitudinal | 36 weeks of GA | +0.64 ± 0.092 | +0.20 ± 0.055 | +0.44 ± 0.115 | <0.001 | |
| 40 weeks of GA | +0.34 ± 0.108 | +0.15 ± 0.077 | +0.20 ± 0.138 | 0.156 | ||
| 28 days | +0.33 ± 0.072 | +0.03 ± 0.061 | +0.30 ± 0.100 | 0.003 | ||
| nidischarge | +0.52 ± 0.084 | +0.20 ± 0.047 | +0.32 ± 0.100 | 0.001 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peila, C.; Spada, E.; Giuliani, F.; Maiocco, G.; Raia, M.; Cresi, F.; Bertino, E.; Coscia, A. Extrauterine Growth Restriction: Definitions and Predictability of Outcomes in a Cohort of Very Low Birth Weight Infants or Preterm Neonates. Nutrients 2020, 12, 1224. https://doi.org/10.3390/nu12051224
Peila C, Spada E, Giuliani F, Maiocco G, Raia M, Cresi F, Bertino E, Coscia A. Extrauterine Growth Restriction: Definitions and Predictability of Outcomes in a Cohort of Very Low Birth Weight Infants or Preterm Neonates. Nutrients. 2020; 12(5):1224. https://doi.org/10.3390/nu12051224
Chicago/Turabian StylePeila, Chiara, Elena Spada, Francesca Giuliani, Giulia Maiocco, Melissa Raia, Francesco Cresi, Enrico Bertino, and Alessandra Coscia. 2020. "Extrauterine Growth Restriction: Definitions and Predictability of Outcomes in a Cohort of Very Low Birth Weight Infants or Preterm Neonates" Nutrients 12, no. 5: 1224. https://doi.org/10.3390/nu12051224
APA StylePeila, C., Spada, E., Giuliani, F., Maiocco, G., Raia, M., Cresi, F., Bertino, E., & Coscia, A. (2020). Extrauterine Growth Restriction: Definitions and Predictability of Outcomes in a Cohort of Very Low Birth Weight Infants or Preterm Neonates. Nutrients, 12(5), 1224. https://doi.org/10.3390/nu12051224





