Inflaming Public Interest: A Qualitative Study of Adult Learners’ Perceptions on Nutrition and Inflammation
Abstract
1. Introduction
2. Materials and Methods
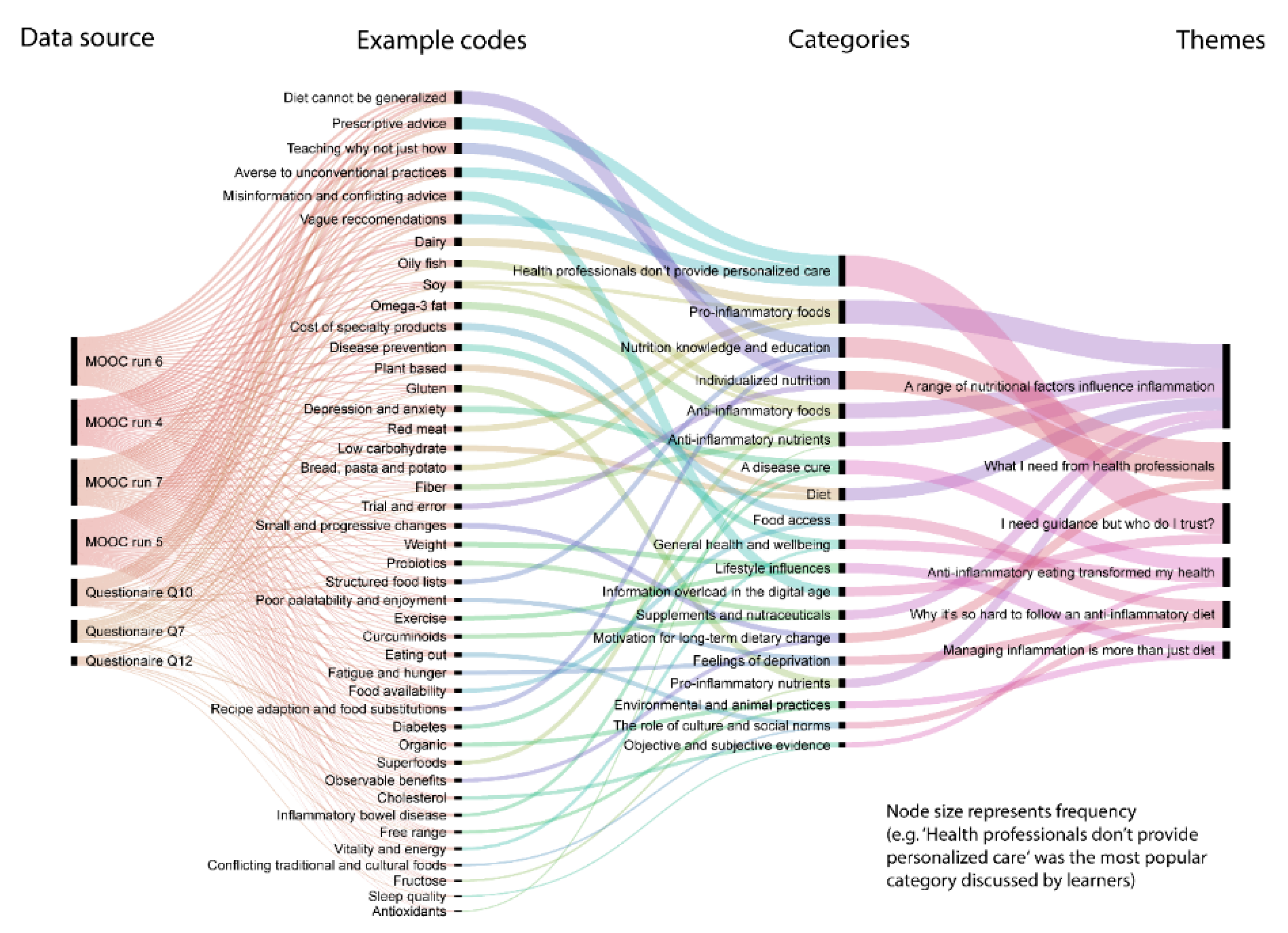
2.1. Familiarization and Coding
2.2. Developing A Working Analytical Framework
2.3. Applying the Analytical Framework
2.4. Charting Data into the Framework Matrix
2.5. Interpreting the Data
2.6. The Research Team
3. Results
3.1. Learners’ Backgrounds
3.2. Learners’ Perceptions and Experiences
3.2.1. A range of Nutritional Factors Influence Inflammation
3.2.2. Managing Inflammation is More than Just Diet
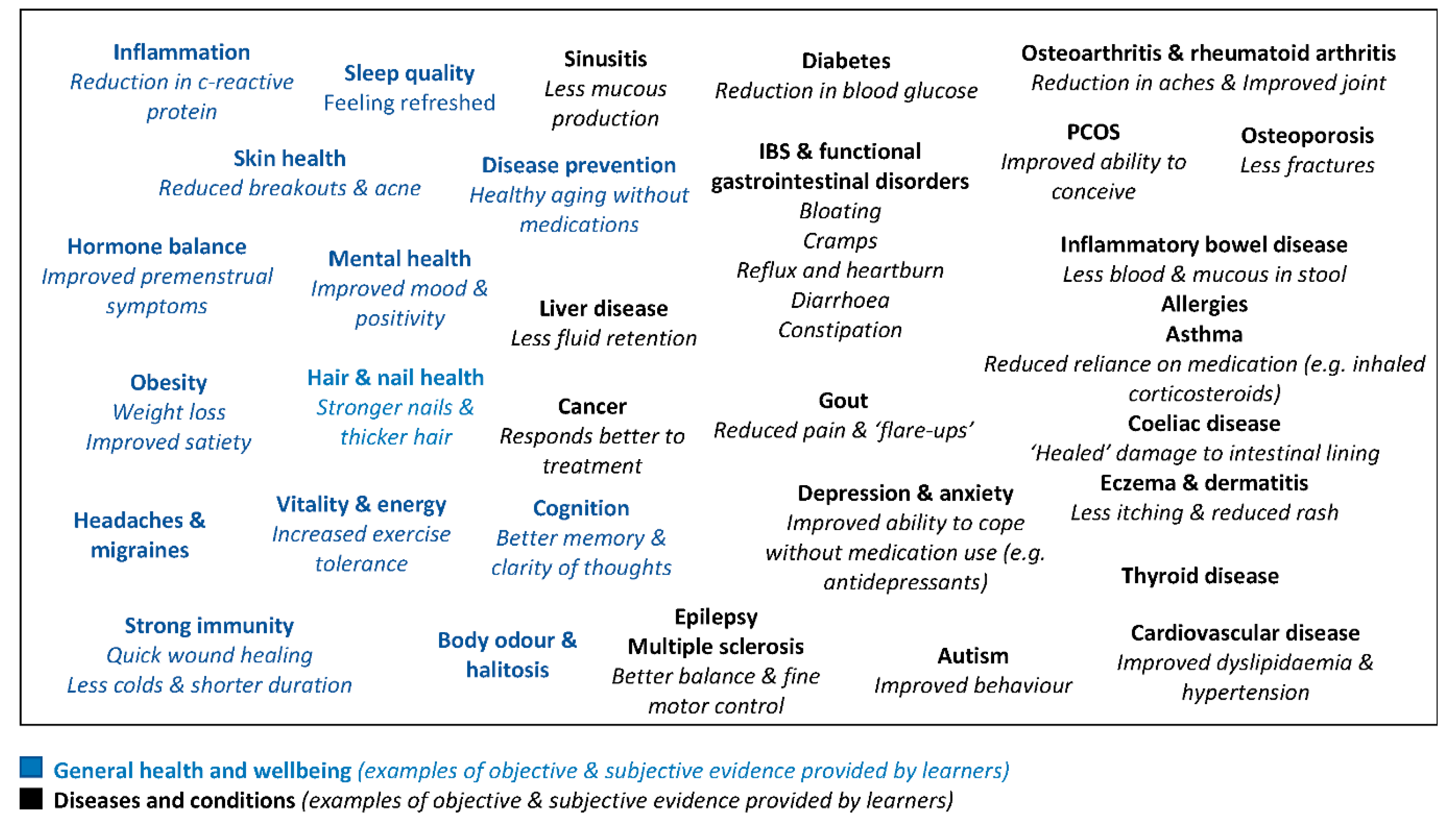
3.2.3. Anti-Inflammatory Eating Transformed My Health
3.2.4. I Need Guidance but Who Do I Trust
3.2.5. Why it’s so Hard to Follow an Anti-Inflammatory Diet
3.2.6. What I need from Health Professionals
4. Discussion
5. Conclusions
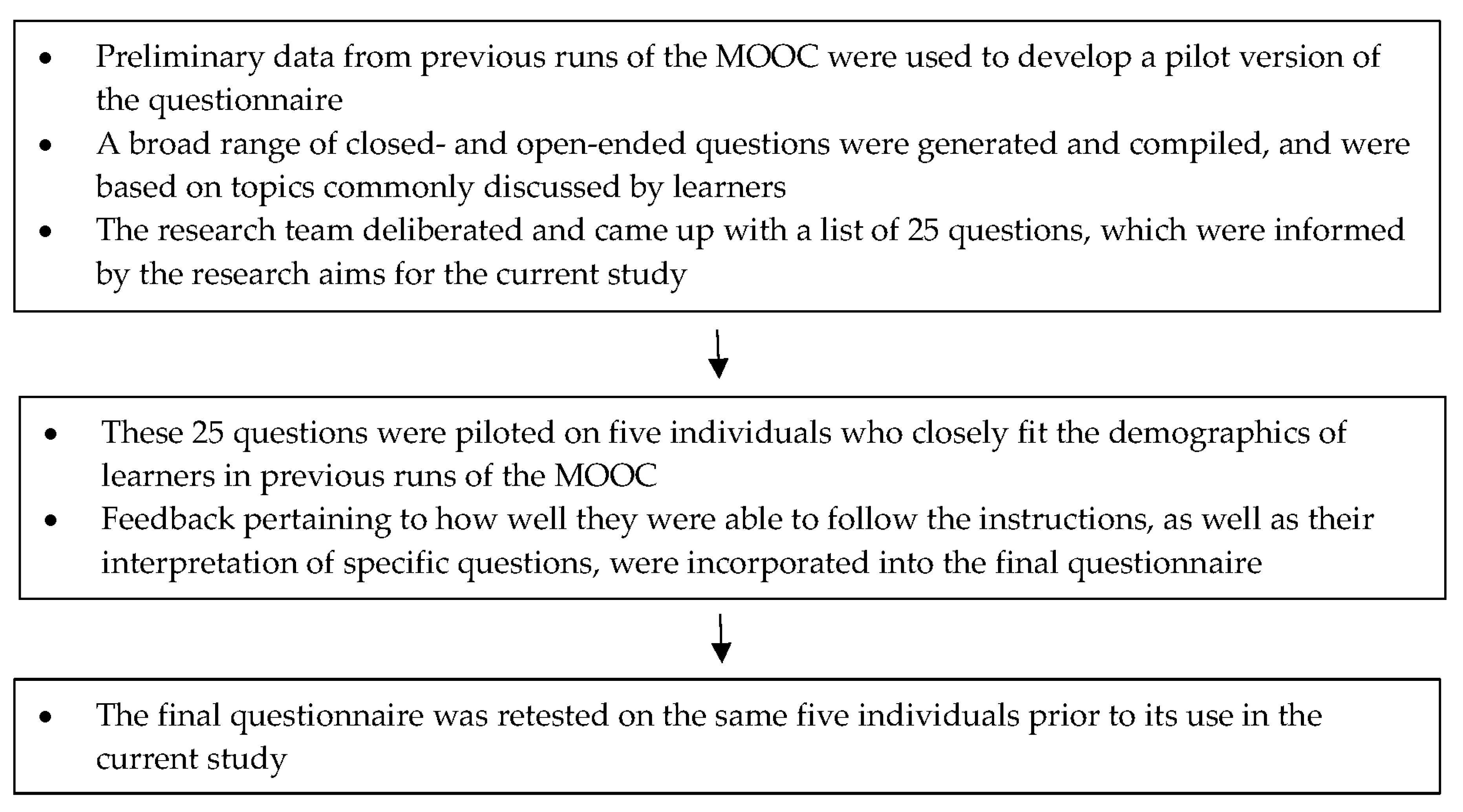
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Appendix A
Appendix B
| Question | Data Source |
|---|---|
| What are the major foods in this diet and are there any foods that are avoided? Are there any particular patterns you must follow? | Questionnaire |
| You answered ‘somewhat difficult’ or ‘extremely difficult’, please explain why (e.g. cost, practicality, taste). This relates to the previous question "Do you find this diet easy to follow?" | Questionnaire |
| You answered ’very useful’ or ’extremely useful’, please explain why (e.g. less joint stiffness in the morning, lowered blood glucose levels, weight loss). This relates to the previous question "Do you find this diet helpful in managing your condition?" | Questionnaire |
| Within the comments, consider sharing your thoughts on the role you think diet plays in inflammation. | Discussion forum |
| Have you followed an anti-inflammatory diet to help manage any conditions and did you find the diet difficult to follow? Within the Comments, consider sharing with other learners your experience with this type of diet. | Discussion forum |
Appendix C
| Participant Comments | Description (in-vivo Codes) | Preliminary Thoughts (What is This about) | How Would It Inform the Research Questions? |
|---|---|---|---|
| By drinking around 5l of fluid per day. Eating lots of fruit and veg with whole grains. Large amounts of low fat animal protein (150 grams per day) I can exercise very intensely with minimal inflammation also take 1tsp of tumeric, black pepper and ginger mixed with water. Plus 1 table spoon of cod liver oil. | Drinking fluid Lots of fruits and vegetables Wholegrains Low fat Improved exercise tolerance Herbs and spices | Fruits, vegetables, wholegrains and herbs and spices are anti-inflammatory Good Hydration is also important for reducing inflammation Improved quality of life is a beneficial effect of following anti-inflammatory diets | Provides insights into dietary components perceived as important in reducing inflammation Highlights alleged benefits of following anti-inflammatory diets as providing incentives |
| How we react to certain food is so specific to each person that it’s such a difficult task to make generalizations find out which foods are healing for what person. | Difficult to make generalizations Specific to each person | Providing an individualized approach to nutrition advice is important | Helps in understanding why people gravitate towards elimination diets |
| Perhaps a list of foods with anti-inflammatory properties would be useful here as an example. | Lists of foods | Detailed dietary advice including lists of specific foods is helpful | Informs healthcare professionals of enablers to following anti-inflammatory diet advice |
| Researcher 1 Code(s) | Description | Researcher 2 code(s) | Description | Merged Code | Inclusion Criteria | Notes | Emerging Categories |
|---|---|---|---|---|---|---|---|
| Mental health | When participants discuss poor mental health as having detrimental effects on inflammation. | Emotional health | Emotional health affects inflammation depending on how one is feeling (i.e. stressed or happy) can affect inflammation in the body by either worsening it or lowering it. | Mental health | When participants discuss lifestyle factors, other than diet, specifically relating to mental and emotional wellbeing, that they believe has an effect on inflammation in the body. | Inclusion criteria can be broadly applied to other lifestyle factors that have been identified, including but not limited to exercise and weight management. | Lifestyle factors |
| Food availability Food affordability | It can be difficult to source fresh and healthy foods (e.g. fresh fish when you don’t live near the ocean), and when they are available often they are too expensive. | Food access | When people show sympathy/empathy for others who cannot access healthy food. | Cost Food availability | Where participants acknowledge that not everyone has access to healthy foods, and this may not only be related to cost constraints, but also to location, availability of cooking equipment, and poor food knowledge. | Part of a broader inclusion criteria that encompassing all identified barriers to successful implementation of anti-inflammatory diets. | Barriers |
| Free-range animals Fresh and local produce | Participants refer to local and free range animal products as having superior nutritional quality or being better for health. | Pasture fed animals Seasonality | Animal products that are pasture fed have a better ratio of omega-3 to omega-6 in their diet, hence, provide nutritional benefits. When participants believe that eating seasonal foods (e.g. seasonal winter fruits) assists with lowering inflammation in the body and helps to regulate other body functions. | Free-range animals Local and seasonal produce | When free range animal products are referred to as having superior nutritional quality and health benefits when compared to animals that have been caged or grain fed. When the freshest produce is referred to as have superior nutritional quality and health benefits. Participants may discuss local food or seasonal food as "… being the best choice". | NA | Environmental and animal practices |
| Overarching Theme Code | Sub-Theme Code | Subtheme | Definition | Illustrative Quote |
|---|---|---|---|---|
| 02.01 Lifestyle influences | 02.01.01 | Exercise Yoga | When participants discuss lifestyle factors, other than diet, that they believe have an effect on inflammation in the body that are just as important as diet. | “I think that the diet have a big influence on the inflamation proces and the sedentary life has a very strong influence as well.” (MOOC 4 1.24; ID 479) “AND introduced REGULAR excersise – that made a big difference with the inflammation.” (question 7; ID 6) “I was practicing yoga everyday at the time and the inflammation in my joints was improving.” (MOOC 41.24; ID 481) |
| 02.01.02 | Gut health | “Someone recently said that "if your get your gut-health right, then your overall health should be good. In other words bad gut health is bad for inflammation" (MOOC 5 1.24; ID 304) | ||
| 02.01.03 | Mental health Mindfulness & meditation | “You forgot to mention that chronic high levels of stress mean that inflammation is not resolved withing the body.” (MOOC 4 1.22; ID 112) | ||
| 02.01.04 | Weight | “And having excessive weight causes problems for several conditions especially when it comes to inflammation.” (MOOC 4 1.24; ID 496) | ||
| 02.02 Environmental & animal practices | 02.02.01 | Free range animals | When free range animal products are referred to as having superior nutritional quality and health benefits when compared to animals that have been caged or grain fed. | “Because fish recently are being considered as healthy option, there’s more and more farmed fishes and due to contaminated fish food/water are just sick/genetically mutated. Therefore, I’ve got some doubts regarding how healthy fishes available today are.” (MOOC 4 1.24; ID 563) “Am glad that someone else picked up on the importance of what the animals are fed influences their omega profile.” (MOOC 4 1.22; ID 43) |
| 02.02.02 | Fresh, local & seasonal produce | When the freshest produce is referred to as have superior nutritional quality and health benefits. Participants may discuss local food or seasonal food as "… being the best choice". | “I eat foods in season as much as possible Much healthier for me and the environment.” (question 7; ID 800) “I don’t trust industrial foods and try to buy organic and from farmers directly. Skipping the pesticicdes!” (question 7; ID 2516) | |
| 02.02.03 | Organic | When organic foods are referred to as have superior nutritional quality and health benefits when compared to non-organic foods. | “And I always prefer to buy organic or farmers fresh (non processed) products.” (question 7; ID 2271) |
References
- Health and Medical Research Council. Australian Dietary Guidelines Providing the Scientific Evidence for Healthier Australian Diets. Available online: https://www.nhmrc.gov.au/about-us/publications/australian-dietary-guidelines#block-views-block-file-attachments-content-block-1 (accessed on 6 September 2019).
- U.S. Department of Health and Human Services; U.S. Department of Agriculture. Dietary guidelines for Americans 2015–2020, 8th ed. Available online: https://health.gov/dietaryguidelines/2015/guidelines/ (accessed on 16 July 2019).
- Hart, K.; Herriot, A.; Bishop, J.; Truby, H. Promoting healthy diet and exercise patterns amongst primary school children: A qualitative investigation of parental perspectives. J. Hum. Nutr. Diet 2003, 16, 89–96. [Google Scholar] [CrossRef]
- Adam Smith Institute. Britons say no to nanny! Modern attitudes to paternalism and state provision. Available online: https://www.adamsmith.org/research/britons-say-no-to-nanny (accessed on 15 July 2019).
- Patterson, R.E.; Satia, J.A.; Kristal, A.R.; Neuhouser, M.L.; Drewnowski, A. Is there a consumer backlash against the diet and health message? J. Am. Diet Assoc. 2001, 101, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Department for Business, Innovation and Skills. Public attitudes to science 2014. Available online: https://www.gov.uk/government/publications/public-attitudes-to-science-2014 (accessed on 20 June 2019).
- World Health Organization. Global strategy on diet, physical activity and health. Available online: https://www.who.int/dietphysicalactivity/strategy/eb11344/strategy_english_web.pdf (accessed on 20 June 2019).
- Wynne, B. Public engagement as a means of restoring public trust in science–hitting the notes, but missing the music? Community Genet 2006, 9, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Watson, R.; Wyness, L. ‘Don’t tell me what to eat!’–ways to engage the population in positive behaviour change. Nutr. Bull 2013, 38, 23–29. [Google Scholar] [CrossRef]
- Penders, B. Why public dismissal of nutrition science makes sense: Post-truth, public accountability and dietary credibility. Br. Food J. 2018, 120, 1953–1964. [Google Scholar] [CrossRef]
- Esser, N.; Legrand-Poels, S.; Piette, J.; Scheen, A.J.; Paquot, N. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res. Clin. Pract. 2014, 105, 141–150. [Google Scholar] [CrossRef]
- Park, H.E.; Cho, G.-Y.; Chun, E.-J.; Choi, S.-I.; Lee, S.-P.; Kim, H.-K.; Youn, T.-J.; Kim, Y.-J.; Choi, D.-J.; Sohn, D.-W. Can c-reactive protein predict cardiovascular events in asymptomatic patients? Analysis based on plaque characterization. Atheroscler. 2012, 224, 201–207. [Google Scholar] [CrossRef]
- Pearson, T.A.; Blair, S.N.; Daniels, S.R.; Eckel, R.H.; Fair, J.M.; Fortmann, S.P.; Franklin, B.A.; Goldstein, L.B.; Greenland, P.; Grundy, S.M. AHA guidelines for primary prevention of cardiovascular disease and stroke: 2002 update. Circ. 2002, 106, 388–391. [Google Scholar] [CrossRef]
- Calder, P.C.; Ahluwalia, N.; Albers, R.; Bosco, N.; Bourdet-Sicard, R.; Haller, D.; Holgate, S.T.; Jönsson, L.S.; Latulippe, M.E.; Marcos, A. A consideration of biomarkers to be used for evaluation of inflammation in human nutritional studies. Br. J. Nutr. 2013, 109, S1–S34. [Google Scholar] [CrossRef]
- Guebre-Egziabher, F.; Rabasa-Lhoret, R.; Bonnet, F.; Bastard, J.; Desage, M.; Skilton, M.; Vidal, H.; Laville, M. Nutritional intervention to reduce the n− 6/n− 3 fatty acid ratio increases adiponectin concentration and fatty acid oxidation in healthy subjects. Eur. J. Clin. Nutr. 2008, 62, 1287–1293. [Google Scholar] [CrossRef]
- Kondo, K.; Morino, K.; Nishio, Y.; Kondo, M.; Fuke, T.; Ugi, S.; Iwakawa, H.; Kashiwagi, A.; Maegawa, H. Effects of a fish-based diet on the serum adiponectin concentration in young, non-obese, healthy japanese subjects. J. Atheroscler Thromb 2010, 17, 628–637. [Google Scholar] [CrossRef]
- Emerson, S.R.; Kurti, S.P.; Harms, C.A.; Haub, M.D.; Melgarejo, T.; Logan, C.; Rosenkranz, S.K. Magnitude and timing of the postprandial inflammatory response to a high-fat meal in healthy adults: A systematic review. Adv. Nutr. 2017, 8, 213–225. [Google Scholar] [CrossRef]
- King, D.E.; Mainous, A.G.; Egan, B.M.; Woolson, R.F.; Geesey, M.E. Effect of psyllium fiber supplementation on c-reactive protein: The trial to reduce inflammatory markers (TRIM). Ann. Fam. Med. 2008, 6, 100–106. [Google Scholar] [CrossRef]
- Wolever, T.M.; Gibbs, A.L.; Mehling, C.; Chiasson, J.-L.; Connelly, P.W.; Josse, R.G.; Leiter, L.A.; Maheux, P.; Rabasa-Lhoret, R.; Rodger, N.W. The canadian trial of carbohydrates in diabetes (CCD), a 1-y controlled trial of low-glycemic-index dietary carbohydrate in type 2 diabetes: No effect on glycated hemoglobin but reduction in c-reactive protein. Am. J. Clin. Nutr. 2008, 87, 114–125. [Google Scholar] [CrossRef]
- Watzl, B.; Kulling, S.E.; Möseneder, J.; Barth, S.W.; Bub, A. A 4-wk intervention with high intake of carotenoid-rich vegetables and fruit reduces plasma c-reactive protein in healthy, nonsmoking men. Am. J. Clin. Nutr. 2005, 82, 1052–1058. [Google Scholar] [CrossRef] [PubMed]
- Barbaresko, J.; Koch, M.; Schulze, M.B.; Nöthlings, U. Dietary pattern analysis and biomarkers of low-grade inflammation: A systematic literature review. Nutr. Rev. 2013, 71, 511–527. [Google Scholar] [CrossRef]
- Neale, E.; Batterham, M.; Tapsell, L.C. Consumption of a healthy dietary pattern results in significant reductions in c-reactive protein levels in adults: A meta-analysis. Nutr. Res. 2016, 36, 391–401. [Google Scholar] [CrossRef]
- Ko, B.-J.; Park, K.H.; Shin, S.; Zaichenko, L.; Davis, C.R.; Crowell, J.A.; Joung, H.; Mantzoros, C.S. Diet quality and diet patterns in relation to circulating cardiometabolic biomarkers. Clin. Nutr. 2016, 35, 484–490. [Google Scholar] [CrossRef]
- Shivappa, N.; Steck, S.E.; Hurley, T.G.; Hussey, J.R.; Hébert, J.R. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014, 17, 1689–1696. [Google Scholar] [CrossRef]
- Cowan, S.F.; Leeming, E.R.; Sinclair, A.; Dordevic, A.L.; Truby, H.; Gibson, S.J. Effect of whole foods and dietary patterns on markers of subclinical inflammation in weight-stable overweight and obese adults: A systematic review. Nutr. Rev. 2019, nuz030:1–nuz030:20. [Google Scholar] [CrossRef]
- Goldberg, J.P.; Sliwa, S.A. Communicating actionable nutrition messages: Challenges and opportunities. Proc. Nutr. Soc. 2011, 70, 26–37. [Google Scholar] [CrossRef] [PubMed]
- Nagler, R.H. Adverse outcomes associated with media exposure to contradictory nutrition messages. J. Health Commun. 2014, 19, 24–40. [Google Scholar] [CrossRef] [PubMed]
- Bestwick, C.; Douglas, F.; Allan, J.; Macdiarmid, J.; Ludbrook, A.; Carlisle, S. A perspective on the strategic approach to the complexity and challenges of behaviour change in relation to dietary health. Nutr. Bull. 2013, 38, 50–56. [Google Scholar] [CrossRef]
- Miller, G.D.; Cohen, N.L.; Fulgoni, V.L.; Heymsfield, S.B.; Wellman, N.S. From nutrition scientist to nutrition communicator: Why you should take the leap. Am. J. Clin. Nutr. 2006, 83, 1272–1275. [Google Scholar] [CrossRef] [PubMed]
- Brennan, R.; Dahl, S.; Eagle, L. Persuading young consumers to make healthy nutritional decisions. J. Mark. Manag. 2010, 26, 635–655. [Google Scholar] [CrossRef]
- Calder, P.C.; Ahluwalia, N.; Brouns, F.; Buetler, T.; Clement, K.; Cunningham, K.; Esposito, K.; Jönsson, L.S.; Kolb, H.; Lansink, M. Dietary factors and low-grade inflammation in relation to overweight and obesity. Br. J. Nutr. 2011, 106, S1–S78. [Google Scholar] [CrossRef] [PubMed]
- Gibson, S.; Adamski, M.; Blumfield, M. Promoting evidence based nutrition education across the world in a competitive space: Delivering a Massive Open Online Course. Nutrients 2020, 12. (in press). [CrossRef]
- McDonald, L.; Malcolm, B.; Ramagopalan, S.; Syrad, H. Real-world data and the patient perspective: The promise of social media? BMC Med. 2019, 17, 11:1–11:5. [Google Scholar] [CrossRef]
- Excel [computer program]. Version 2013 (Windows); Microsoft Office®: Redmond, WA, USA, 2013.
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol 2013, 13, 117:1–117:8. [Google Scholar] [CrossRef]
- Nvivo [computer program]. Version 12; QSR International Pty Ltd.: Melbourne, VIC, Australia, 2018.
- Australian Institute of Health and Welfare. Australia’s health 2018. Available online: https://www.aihw.gov.au/getmedia/95830c0a-ee53-4f95-a6a4-860f90e4bd66/aihw-aus-221-chapter-2-4.pdf.aspx (accessed on 24 July 2019).
- Pollard, C.M.; Pulker, C.E.; Meng, X.; Kerr, D.A.; Scott, J.A. Who uses the internet as a source of nutrition and dietary information? An Australian population perspective. J. Med. Internet Res. 2015, 17, e209. [Google Scholar] [CrossRef]
- Thieme, K.; Mathys, M.; Turk, D.C. Evidenced-based guidelines on the treatment of fibromyalgia patients: Are they consistent and if not, why not? Have effective psychological treatments been overlooked? J. Pain 2017, 18, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.; Bagnall, A.-M.; Sowden, A.J.; Cornell, J.E.; Mulrow, C.D.; Ramírez, G. Interventions for the treatment and management of chronic fatigue syndrome: A systematic review. JAMA 2001, 286, 1360–1368. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.T. Information seeking over the course of illness: The experience of people with fibromyalgia. Musculoskeletal Care 2012, 10, 212–220. [Google Scholar] [CrossRef]
- Schlaeger, J.M.; Roach, K.; Golas, M.; Takayama, M.; Wilkie, D.J. Treatment-seeking behaviors of persons with rheumatoid arthritis. J. Holist. Nurs. 2018, 36, 179–191. [Google Scholar] [CrossRef] [PubMed]
- American Dietetic Association. Position of the American dietetic association: Food and nutrition misinformation. J. Am. Diet Assoc. 2002, 102, 260–266. [Google Scholar] [CrossRef]
- Rowe, R.; Calnan, M. Trust relations in health care—the new agenda. Eur. J. Public Health 2006, 16, 4–6. [Google Scholar] [CrossRef]
- Rathert, C.; Wyrwich, M.D.; Boren, S.A. Patient-centered care and outcomes: A systematic review of the literature. Med. Care Res. Rev. 2013, 70, 351–379. [Google Scholar] [CrossRef]
- Bruner, J.S. The culture of education; Harvard University Press: Cambridge, MA, USA, 1996; ISBN 9780674179530. [Google Scholar]
- Damgaard, B.; Lewis, J.M. Accountability and citizen participation. In The Oxf. handbook of public Account; Oxford University Press: Oxford, UK, 2014; ISBN 9780199641253. [Google Scholar]
- Australian Bureau of Statistics. National Health Survey: Health Literacy, 2018. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Latestproducts/4364.0.55.014Main%20Features12018?opendocument&tabname=Summary&prodno=4364.0.55.014&issue=2018&num=&view= (accessed on 24 July 2019).
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC public health 2012, 12, 80:1–80:13. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Australian Social Trends, June 2009. Available online: https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4102.0Main+Features20June+2009 (accessed on 14 June 2019).
- Lobo, R.A.; Davis, S.R.; De Villiers, T.J.; Gompel, A.; Henderson, V.W.; Hodis, H.N.; Lumsden, M.A.; Mack, W.J.; Shapiro, S.; Baber, R.J. Prevention of diseases after menopause. Climacteric 2014, 17, 540–556. [Google Scholar] [CrossRef]
- Briggs, L.; Hyde, A.; Mile, S.M. The health information needs of older women in the UK. Available online: https://www.rcog.org.uk/globalassets/documents/patients/womens-network/health-information-needs-of-older-women-final-report.pdf (accessed on 1 January 2020).
- Tuohy, D.; Cooney, A. Older Women’s Experiences of Aging and Health: An Interpretive Phenomenological Study. Gerontol Geriatr Med. 2019, 5, 10. [Google Scholar] [CrossRef]
- Thompson, A.E.; Anisimowicz, Y.; Miedema, B.; Hogg, W.; Wodchis, W.P.; Aubrey-Bassler, K. The influence of gender and other patient characteristics on health care-seeking behaviour: A QUALICOPC study. BMC Fam. Prac. 2016, 17, 38. [Google Scholar] [CrossRef] [PubMed]

| Sources of Nutrition Information | Number (percentage) of Questionnaire Respondents 2 |
|---|---|
| Internet (includes search engines such as Google and social media sites) | 1308 (38) |
| Doctors | 445 (13) |
| Alternative health providers (includes naturopath, homeopath, chiropractor, acupuncturist, yoga instructor, personal trainer) | 445 (13) |
| Books | 411 (12) |
| Friends and family | 343 (10) |
| Nutritionists | 308 (9) |
| Dietitians | 206 (6) |
| Inflammatory Condition | Number (percentage) of Questionnaire Respondents 2 |
|---|---|
| Irritable bowel syndrome or food intolerance | 994 (29) |
| Eczema or psoriasis | 514 (15) |
| Depression | 478 (14) |
| Asthma | 478 (14) |
| Hypertension | 411 (12) |
| Obesity | 411 (12) |
| Rheumatoid arthritis | 377 (11) |
| Food allergy (medically diagnosed) | 308 (9) |
| Osteoporosis | 274 (8) |
| Hypercholesterolemia | 274 (8) |
| Chronic fatigue syndrome | 240 (7) |
| Fibromyalgia | 206 (6) |
| Inflammatory bowel disease | 172 (5) |
| Cancer | 137 (4) |
| Type two diabetes mellitus | 133 (4) |
| Cardiovascular disease | 133 (4) |
| Coeliac disease | 130 (4) |
| Metabolic Syndrome | 69 (2) |
| Lupus | 35 (1) |
| Other (n = 66), including but not limited to endometriosis, poly-cystic ovarian syndrome, thyroid disease such as Grave’s disease, multiple sclerosis, Parkinson’s disease, chronic back pain and chronic kidney disease | 1268 (37) |
| Theme | Categories | Illustrative Quote(s) |
|---|---|---|
| 1.0 A range of nutritional factors influence inflammation | 1.01 Diets 1.02 Foods 1.03 Nutrients 1.04 Supplements and nutraceuticals | “I went Paleo after being diagnosed with an inflammatory condition. It has truly helped.” (learner ID 58.96.80.106) “I believe a plant based diet prevents inflammatory diseases/conditions.” (learner ID 92.25.35.22) “Choosing foods with anti-inflammatory properties and foods which are more alkalising than acidic will definitely play a large role in promoting healing.” “Pro-inflammatory foods are sugar and alcohol.” (learner ID 187.201.48.75) |
| 2.0 Managing inflammation is more than just diet | 2.01 Lifestyle influences 2.02 Environmental and animal practices | “chronic high levels of stress mean that inflammation is not resolved withing the body.” (learner ID 103.85.106.87) “I don’t trust industrial foods and try to buy organic and from farmers directly.” (learner ID 202.133.214.88) |
| 3.0 Anti-inflammatory eating transformed my health | 3.01 A disease cure 3.02 Objective and subjective evidence 3.03 General health and wellbeing | “I was not expected to survive the cancer which was stage 3 when it was found but after surgery, chemo and radiotherapy and a very clean diet for a year I am still here 12 years later. The medics were very surprised.” (learner ID 31.18.251.69) “cholesterol numbers, without medication as I reacted to all tried, dropped from 9.5 to 6.5.” (learner ID 1.143.153.148) “Cannot pin point physical benefits except more energy, general feeling of wellbeing” (learner ID 5.52.109.5) |
| 4.0 I need guidance but who do I trust? | 4.01 Information overload in the digital age 4.02 Health professionals don’t provide personalized care | “There’s so much misinformation it’s hard to decipher.” (learner ID 89.120.155.144) “I have researched many books on RA and diet, most of which were difficult to follow” (learner ID 24.30.74.17) “I have not had advice on this from my GP or the dietitian I went to see, and find conflicting views online.” (learner ID 210.1.90.94) “Look for another GP. Get someone who listens to you, respects you and is willing to offer advice, not necessarily pills.” (learner ID 51.39.225.80) |
| 5.0 Why it’s so hard to follow an anti-inflammatory diet | 5.01 Food access 5.02 The role of culture and social norms 5.03 Feelings of deprivation | “It was lonely eating differently from my family and I had little energy to cook.” (learner ID 125.236.138.13) “The cost of the organic foods that I have switched to is much higher than the cheap processed foods I used to buy.” (learner ID 24.108.0.208) “Because it takes time to buy fresh food and to cook it would be easier to eat fast food” (learner ID 2.218.59.59) “The challenge however is being able to have these foods on a constant and affordable basis… because in my country we have a very small choice of special products.” (learner ID 121.214.109.127 – questionnaire) |
| 6.0 What I need from health professionals | 6.01 Nutrition knowledge and education 6.02 Motivation for long-term dietary change 6.03 Individualized nutrition | “It means different foods react in different ways with different people. Each person has to discover his/her own” through “trial and error” (learner ID 14.201.127.194 – discussion forum) “Individual advice is key” (learner ID 27.252.219.51) “Time of day for foods was very useful, so to was advice on how to pair foods to create balance, the more detail the better for me.” (learner ID 141.168.83.49) “CAN YOU GIVE ME A LIST OF ANTI-INFLAMMATORY FOODS? THANK YOU” (learner ID 51.6.145.23) “Found this helpful in knowing in such detail, why I should avoid all those tempting food ’baddies’. Thank you. Learning the science is fun!” (learner ID 74.222.74.127) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cowan, S.; Sood, S.; Truby, H.; Dordevic, A.; Adamski, M.; Gibson, S. Inflaming Public Interest: A Qualitative Study of Adult Learners’ Perceptions on Nutrition and Inflammation. Nutrients 2020, 12, 345. https://doi.org/10.3390/nu12020345
Cowan S, Sood S, Truby H, Dordevic A, Adamski M, Gibson S. Inflaming Public Interest: A Qualitative Study of Adult Learners’ Perceptions on Nutrition and Inflammation. Nutrients. 2020; 12(2):345. https://doi.org/10.3390/nu12020345
Chicago/Turabian StyleCowan, Stephanie, Surbhi Sood, Helen Truby, Aimee Dordevic, Melissa Adamski, and Simone Gibson. 2020. "Inflaming Public Interest: A Qualitative Study of Adult Learners’ Perceptions on Nutrition and Inflammation" Nutrients 12, no. 2: 345. https://doi.org/10.3390/nu12020345
APA StyleCowan, S., Sood, S., Truby, H., Dordevic, A., Adamski, M., & Gibson, S. (2020). Inflaming Public Interest: A Qualitative Study of Adult Learners’ Perceptions on Nutrition and Inflammation. Nutrients, 12(2), 345. https://doi.org/10.3390/nu12020345





