Associations of Coarse Grain Intake with Undiagnosed Hypertension among Chinese Adults: Results from the China Kadoorie Biobank
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection
2.3. Dietary Assessment
2.4. Definition of Outcomes
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Olsen, M.H.; Angell, S.Y.; Asma, S.; Boutouyrie, P.; Burger, D.; Chirinos, J.A.; Damasceno, A.; Delles, C.; Gimenez-Roqueplo, A.P.; Hering, D.; et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: The Lancet Commission on hypertension. Lancet 2016, 388, 2665–2712. [Google Scholar] [CrossRef]
- Lacey, B.; Lewington, S.; Clarke, R.; Kong, X.L.; Chen, Y.P.; Guo, Y.; Yang, L.; Bennett, D.; Bragg, F.; Bian, Z.; et al. Age-specific association between blood pressure and vascular and non-vascular chronic diseases in 0.5 million adults in China: A prospective cohort study. Lancet Glob. Health 2018, 6, E641–E649. [Google Scholar] [CrossRef]
- Wang, Z.W.; Chen, Z.; Zhang, L.F.; Wang, X.; Hao, G.; Zhang, Z.G.; Shao, L.; Tian, Y.; Dong, Y.; Zheng, C.Y.; et al. Status of Hypertension in China Results From the China Hypertension Survey, 2012–2015. Circulation 2018, 137, 2344–2356. [Google Scholar] [CrossRef] [PubMed]
- Saneei, P.; Salehi-Abargouei, A.; Esmaillzadeh, A.; Azadbakht, L. Influence of Dietary Approaches to Stop Hypertension (DASH) diet on blood pressure: A systematic review and meta-analysis on randomized controlled trials. Nutr. Metab. Cardiovasc. Dis. NMCD 2014, 24, 1253–1261. [Google Scholar] [CrossRef] [PubMed]
- Nissensohn, M.; Roman-Vinas, B.; Sanchez-Villegas, A.; Piscopo, S.; Serra-Majem, L. The Effect of the Mediterranean Diet on Hypertension: A Systematic Review and Meta-Analysis. J. Nutr. Educ. Behav. 2016, 48, 42–53.e41. [Google Scholar] [CrossRef]
- Shono, C.; Suzuki, N.; Kaiser, H.M. Will China’s diet follow western diets? Agribus. Int. J. 2000, 16, 271–279. [Google Scholar] [CrossRef]
- Lelong, H.; Blacher, J.; Baudry, J.; Adriouch, S.; Galan, P.; Fezeu, L.; Hercberg, S.; Kesse-Guyot, E. Individual and Combined Effects of Dietary Factors on Risk of Incident Hypertension: Prospective Analysis from the NutriNet-Sante Cohort. Hypertension 2017, 70, 712–720. [Google Scholar] [CrossRef]
- Vernay, M.; Aidara, M.; Salanave, B.; Deschamps, V.; Malon, A.; Oleko, A.; Mallion, J.M.; Hercberg, S.; Castetbon, K. Diet and blood pressure in 18–74-year-old adults: The French Nutrition and Health Survey (ENNS, 2006–2007). J. Hypertens. 2012, 30, 1920–1927. [Google Scholar] [CrossRef]
- Kirwan, J.P.; Malin, S.K.; Scelsi, A.R.; Kullman, E.L.; Navaneethan, S.D.; Pagadala, M.R.; Haus, J.M.; Filion, J.; Godin, J.P.; Kochhar, S.; et al. A Whole-Grain Diet Reduces Cardiovascular Risk Factors in Overweight and Obese Adults: A Randomized Controlled Trial. J. Nutr. 2016, 146, 2244–2251. [Google Scholar] [CrossRef]
- Ampatzoglou, A.; Atwal, K.K.; Maidens, C.M.; Williams, C.L.; Ross, A.B.; Thielecke, F.; Jonnalagadda, S.S.; Kennedy, O.B.; Yaqoob, P. Increased whole grain consumption does not affect blood biochemistry, body composition, or gut microbiology in healthy, low-habitual whole grain consumers. J. Nutr. 2015, 145, 215–221. [Google Scholar] [CrossRef]
- Aune, D.; Keum, N.; Giovannucci, E.; Fadnes, L.T.; Boffetta, P.; Greenwood, D.C.; Tonstad, S.; Vatten, L.J.; Riboli, E.; Norat, T. Whole grain consumption and risk of cardiovascular disease, cancer, and all cause and cause specific mortality: Systematic review and dose-response meta-analysis of prospective studies. BMJ 2016, 353, i2716. [Google Scholar] [CrossRef] [PubMed]
- Villegas, R.; Liu, S.; Gao, Y.T.; Yang, G.; Li, H.; Zheng, W.; Shu, X.O. Prospective study of dietary carbohydrates, glycemic index, glycemic load, and incidence of type 2 diabetes mellitus in middle-aged Chinese women. Arch. Intern. Med. 2007, 167, 2310–2316. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Pan, A.; Zong, G.; Yu, Z.; Wu, H.; Chen, X.; Tang, L.; Feng, Y.; Zhou, H.; Chen, X.; et al. Substituting white rice with brown rice for 16 weeks does not substantially affect metabolic risk factors in middle-aged Chinese men and women with diabetes or a high risk for diabetes. J. Nutr. 2011, 141, 1685–1690. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Zhao, L.; Yu, D.; Xia, J.; Yang, X.; Yang, Y. The coarse food intake and its impact on dietary nutrients in Chinese adults. Acta Nutr. Sin. 2016, 38, 326–331. [Google Scholar]
- He, Y.; Zhao, L.; Yu, D.; Hu, J.; Yang, Y.; Yang, X. The status of coarse food intake among Chinese adults. Acta Nutr. Sin. 2016, 38, 115–118. [Google Scholar]
- Liu, X.; Liao, X.; Gan, W.; Ding, X.; Gao, B.; Wang, H.; Zhao, X.; Liu, Y.; Feng, L.; Abdulkadil, W.; et al. Inverse Relationship between Coarse Food Grain Intake and Blood Pressure among Young Chinese Adults. Am. J. Hypertens. 2019, 32, 402–408. [Google Scholar] [CrossRef]
- Chen, Z.; Lee, L.; Chen, J.; Collins, R.; Wu, F.; Guo, Y.; Linksted, P.; Peto, R. Cohort profile: The Kadoorie Study of Chronic Disease in China (KSCDC). Int. J. Epidemiol. 2005, 34, 1243–1249. [Google Scholar] [CrossRef]
- Chen, Z.; Chen, J.; Collins, R.; Guo, Y.; Peto, R.; Wu, F.; Li, L.; China Kadoorie Biobank Collaborative Group. China Kadoorie Biobank of 0.5 million people: Survey methods, baseline characteristics and long-term follow-up. Int. J. Epidemiol. 2011, 40, 1652–1666. [Google Scholar] [CrossRef]
- Yu, H.-T.; Fu, X.-Y.; Xu, B.; Zuo, L.-l.; Ma, H.-B.; Wang, S.-R. Untargeted metabolomics approach (UPLC-Q-TOF-MS) explores the biomarkers of serum and urine in overweight/obese young men. Asia Pac. J. Clin. Nutr. 2018, 27, 1067–1076. [Google Scholar] [CrossRef]
- Lewington, S.; Li, L.; Sherliker, P.; Guo, Y.; Millwood, I.; Bian, Z.; Whitlock, G.; Yang, L.; Collins, R.; Chen, J.; et al. Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: The China Kadoorie Biobank. J. Hypertens. 2012, 30, 1383–1391. [Google Scholar] [CrossRef]
- Li, L.M.; Lv, J.; Guo, Y.; Collins, R.; Chen, J.S.; Peto, R.; Wu, F.; Chen, Z.M.; China Kadoorie Biobank Collaborative Group. The China Kadoorie Biobank: Related methodology and baseline characteristics of the participants. Zhonghua Liu Xing Bing Xue Za Zhi 2012, 33, 249–255. [Google Scholar] [PubMed]
- Du, H.; Li, L.; Bennett, D.; Guo, Y.; Key, T.J.; Bian, Z.; Sherliker, P.; Gao, H.; Chen, Y.; Yang, L.; et al. Fresh Fruit Consumption and Major Cardiovascular Disease in China. N. Engl. J. Med. 2016, 374, 1332–1343. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Qi, L.; Yu, C.; Yang, L.; Guo, Y.; Chen, Y.; Bian, Z.; Sun, D.; Du, J.; Ge, P.; et al. Consumption of spicy foods and total and cause specific mortality: Population based cohort study. BMJ 2015, 351, h3942. [Google Scholar] [CrossRef] [PubMed]
- Lewington, S.; Lacey, B.; Clarke, R.; Guo, Y.; Kong, X.L.; Yang, L.; Chen, Y.; Bian, Z.; Chen, J.; Meng, J.; et al. The Burden of Hypertension and Associated Risk for Cardiovascular Mortality in China. JAMA Intern. Med. 2016, 176, 524–532. [Google Scholar] [CrossRef] [PubMed]
- Sundstrom, J.; Neovius, M.; Tynelius, P.; Rasmussen, F. Association of blood pressure in late adolescence with subsequent mortality: Cohort study of Swedish male conscripts. BMJ 2011, 342, d643. [Google Scholar] [CrossRef]
- Wall, H.K.; Hannan, J.A.; Wright, J.S. Patients with undiagnosed hypertension: Hiding in plain sight. JAMA 2014, 312, 1973–1974. [Google Scholar] [CrossRef]
- Hou, D.; Chen, J.; Ren, X.; Wang, C.; Diao, X.; Hu, X.; Zhang, Y.; Shen, Q. A whole foxtail millet diet reduces blood pressure in subjects with mild hypertension. J. Cereal Sci. 2018, 84, 13–19. [Google Scholar] [CrossRef]
- Ascherio, A.; Rimm, E.B.; Giovannucci, E.L.; Colditz, G.A.; Rosner, B.; Willett, W.C.; Sacks, F.; Stampfer, M.J. A prospective study of nutritional factors and hypertension among US men. Circulation 1992, 86, 1475–1484. [Google Scholar] [CrossRef]
- Witteman, J.C.; Willett, W.C.; Stampfer, M.J.; Colditz, G.A.; Sacks, F.M.; Speizer, F.E.; Rosner, B.; Hennekens, C.H. A prospective study of nutritional factors and hypertension among US women. Circulation 1989, 80, 1320–1327. [Google Scholar] [CrossRef]
- Komukai, K.; Mochizuki, S.; Yoshimura, M. Gender and the renin-angiotensin-aldosterone system. Fundam. Clin. Pharmacol. 2010, 24, 687–698. [Google Scholar] [CrossRef]
- Marques, F.Z.; Nelson, E.; Chu, P.Y.; Horlock, D.; Fiedler, A.; Ziemann, M.; Tan, J.K.; Kuruppu, S.; Rajapakse, N.W.; El-Osta, A.; et al. High-Fiber Diet and Acetate Supplementation Change the Gut Microbiota and Prevent the Development of Hypertension and Heart Failure in Hypertensive Mice. Circulation 2017, 135, 964–977. [Google Scholar] [CrossRef] [PubMed]
- Keenan, J.M.; Pins, J.J.; Frazel, C.; Moran, A.; Turnquist, L. Oat ingestion reduces systolic and diastolic blood pressure in patients with mild or borderline hypertension: A pilot trial. J. Fam. Pract. 2002, 51, 369. [Google Scholar] [PubMed]
- Aleixandre, A.; Miguel, M. Dietary fiber and blood pressure control. Food Funct. 2016, 7, 1864–1871. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Shi, L.; Dai, X.; Chen, H.; Zhang, C.; Wang, P.; Wu, Q.; Zeng, L.; Yan, H. Plasma metabolites mediate the association of coarse grain intake with blood pressure in hypertension-free adults. Nutr. Metab. Cardiovasc. Dis. NMCD 2020, 30, 1512–1519. [Google Scholar] [CrossRef] [PubMed]
- Walker, M.; Xanthakis, V.; Ma, J.; Quatromoni, P.A.; Moore, L.; Ramachandran, V.; Jacques, P. A Mediterranean Style Diet Is Favorably Associated with Concentrations of Circulating Ceramides and Ceramide Ratios in the Framingham Offspring Cohort (P18-048-19). Curr. Dev. Nutr. 2019, 3. [Google Scholar] [CrossRef]
- Sasset, L.; Zhang, Y.; Dunn, T.M.; Di Lorenzo, A. Sphingolipid De Novo Biosynthesis: A Rheostat of Cardiovascular Homeostasis. Trends Endocrinol. Metab. TEM 2016, 27, 807–819. [Google Scholar] [CrossRef]
- Fenger, M.; Linneberg, A.; Jorgensen, T.; Madsbad, S.; Sobye, K.; Eugen-Olsen, J.; Jeppesen, J. Genetics of the ceramide/sphingosine-1-phosphate rheostat in blood pressure regulation and hypertension. BMC Genet. 2011, 12, 44. [Google Scholar] [CrossRef]

| Characteristic | Never or Rarely | Monthly | 1–3 Days/Week | 4–6 Days/Week | Daily | All Participants |
|---|---|---|---|---|---|---|
| n | 127,277 | 194,325 | 54,693 | 3615 | 55,997 | 435,907 |
| Age (years) | 49.6 (12.2) | 50.4 (12.6) | 51.5 (11.3) | 53.8 (10.4) | 56.2 (30.6) | 50.8 (10.4) |
| Female (%) | 55.4 | 60.5 | 62.4 | 65.8 | 56.2 | 58.7 |
| Urban residence (%) | 37.8 | 46.9 | 75.9 | 83.1 | 7.0 | 43.0 |
| Education level (%) | ||||||
| No formal education | 20.9 | 18.7 | 11.4 | 10.3 | 11.6 | 17.4 |
| Primary school | 36.5 | 32.5 | 17.9 | 15.2 | 33.2 | 31.8 |
| Middle or high school | 39.2 | 43.2 | 55.1 | 55.6 | 52.9 | 44.9 |
| College or university | 3.4 | 5.6 | 15.6 | 18.8 | 2.3 | 5.9 |
| Household Income (%) | ||||||
| <10,000 yuan/year | 29.9 | 27.4 | 21.2 | 17.9 | 39.1 | 28.8 |
| 10,000–19,999 yuan/year | 25.7 | 27.5 | 28.3 | 30.2 | 43.4 | 29.1 |
| 20,000–34,999 yuan/year | 25.1 | 26.1 | 29.2 | 29.5 | 13.1 | 24.5 |
| ≥35,000 yuan/year | 19.3 | 19.1 | 21.4 | 22.4 | 4.4 | 17.6 |
| Smoking status (%) | ||||||
| Never | 56.3 | 63.5 | 67.3 | 69.6 | 60.2 | 61.5 |
| Occasional | 5.5 | 5.5 | 5.1 | 4.8 | 8.1 | 5.8 |
| Ex-regular | 5.6 | 4.8 | 5.9 | 6.4 | 5.7 | 5.3 |
| Regular | 32.7 | 26.2 | 21.6 | 19.2 | 26.1 | 27.4 |
| Alcohol drinking (%) | ||||||
| Never | 47.9 | 50.6 | 41.4 | 40.0 | 18.6 | 44.4 |
| Occasional | 24.7 | 29.9 | 36.8 | 38.6 | 59.4 | 33.1 |
| Ex-regular | 2.0 | 1.5 | 1.0 | 0.8 | 0.4 | 1.4 |
| Regular | 25.5 | 18.0 | 20.9 | 20.7 | 21.6 | 21.1 |
| Physical activity (MET-hr/day) | 19.4 (17.3) | 19.2 (19.0) | 19.3 (14.6) | 19.3 (12.2) | 19.7 (36.3) | 21.9 (13.9) |
| BMI (kg/m2) | 23.1 (4.5) | 23.2 (4.9) | 23.2 (3.8) | 23.3 (3.2) | 23.1 (9.5) | 23.4 (3.3) |
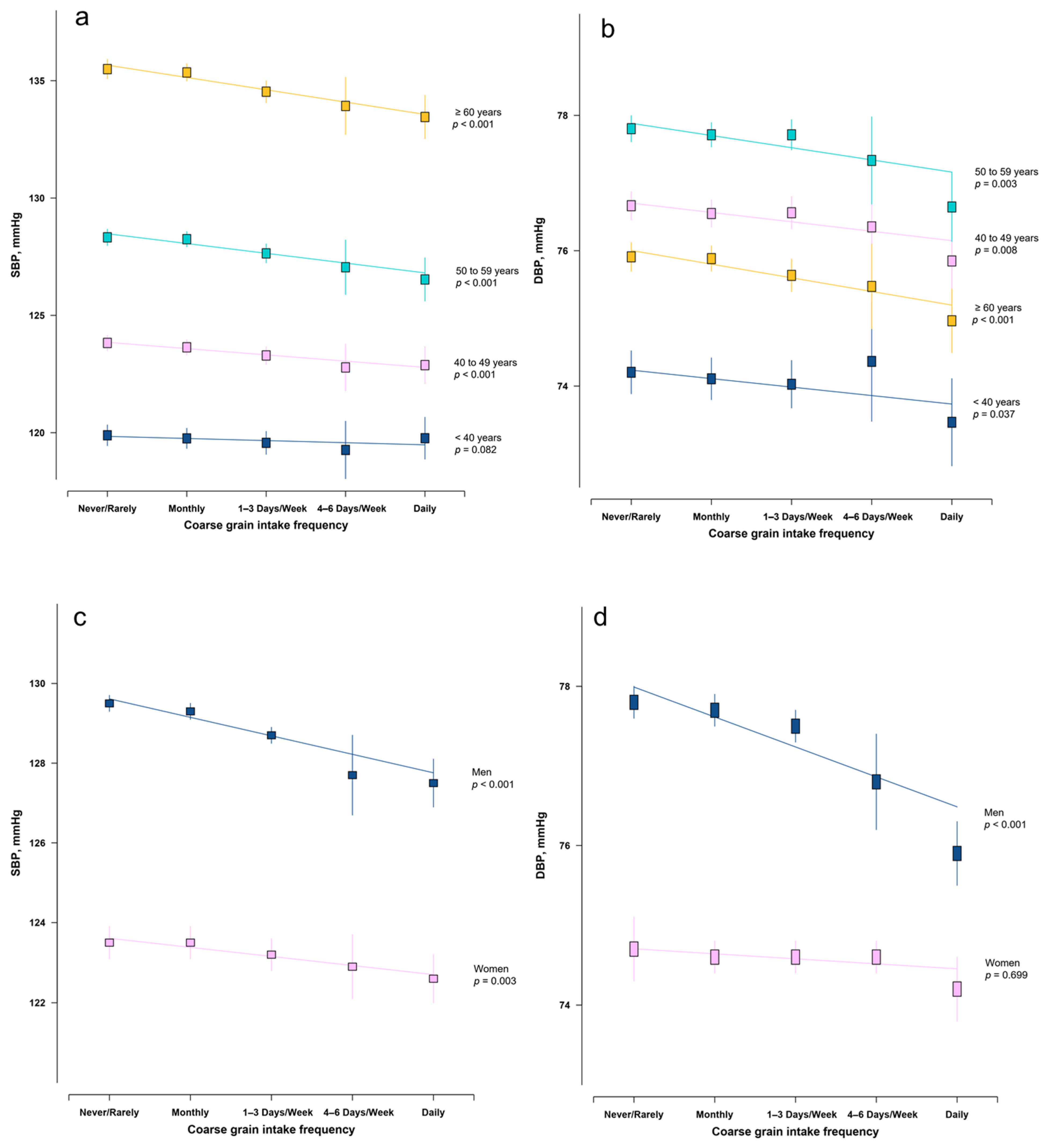
| SBP (mmHg) | 130.0 (25.4) | 129.9 (27.8) | 129.3 (21.4) | 128.8 (17.9) | 128.2 (53.2) | 127.5 (18.9) |
| DBP (mmHg) | 76.1 (14.6) | 76.0 (16.0) | 76.0 (12.3) | 75.8 (10.3) | 74.9 (30.6) | 76.4 (10.4) |
| Odds Ratio (95% CI) | p for Trend | |||||
|---|---|---|---|---|---|---|
| Never or Rarely | Monthly | 1–3 Days/Week | 4–6 Days/Week | Daily | ||
| All participants | ||||||
| Model 1 | 1.00 | 0.97 (0.96–0.99) | 0.92 (0.89–0.94) | 0.86 (0.79–0.93) | 0.77 (0.72–0.82) | <0.001 |
| Model 2 | 1.00 | 0.97 (0.95–0.99) | 0.91 (0.88–0.94) | 0.84 (0.77–0.91) | 0.78 (0.73–0.84) | <0.001 |
| <50.1 years (Median) | ||||||
| Model 1 | 1.00 | 0.95 (0.93–0.98) | 0.91 (0.87–0.95) | 0.82 (0.70–0.96) | 0.85 (0.75–0.95) | <0.001 |
| Model 2 | 1.00 | 0.96 (0.93–0.99) | 0.93 (0.89–0.97) | 0.83 (0.70–0.98) | 0.95 (0.84–1.07) | 0.001 |
| ≥50.1 years (Median) | ||||||
| Model 1 | 1.00 | 0.99 (0.97–1.02) | 0.94 (0.91–0.97) | 0.90 (0.82–1.00) | 0.77 (0.71–0.84) | <0.001 |
| Model 2 | 1.00 | 0.98 (0.96–1.01) | 0.92 (0.89–0.96) | 0.88 (0.79–0.97) | 0.76 (0.70–0.83) | <0.001 |
| Men | ||||||
| Model 1 | 1.00 | 0.97 (0.95–1.00) | 0.92 (0.88–0.96) | 0.81 (0.71–0.92) | 0.71 (0.64–0.78) | <0.001 |
| Model 2 | 1.00 | 0.97 (0.94–0.99) | 0.90 (0.86–0.94) | 0.79 (0.69–0.91) | 0.74 (0.66–0.81) | <0.001 |
| Women | ||||||
| Model 1 | 1.00 | 1.00 (0.98–1.03) | 0.99 (0.95–1.03) | 1.00 (0.90–1.11) | 0.92 (0.84–1.01) | 0.267 |
| Model 2 | 1.00 | 0.99 (0.97–1.02) | 0.97 (0.93–1.00) | 0.95 (0.85–1.07) | 0.90 (0.81–0.99) | 0.020 |
| Rural | ||||||
| Model 1 | 1.00 | 1.01 (0.99–1.04) | 1.03 (0.98–1.08) | 1.03 (0.85–1.24) | 0.84 (0.74–0.95) | 0.911 |
| Model 2 | 1.00 | 0.98 (0.96–1.01) | 0.95 (0.91–1.00) | 0.95 (0.77–1.16) | 0.86 (0.75–0.98) | 0.008 |
| Urban | ||||||
| Model 1 | 1.00 | 0.95 (0.92–0.98) | 0.88 (0.85–0.91) | 0.83 (0.76–0.92) | 0.75 (0.69–0.82) | <0.001 |
| Model 2 | 1.00 | 0.97 (0.94–1.00) | 0.91 (0.88–0.95) | 0.86 (0.78–0.95) | 0.79 (0.73–0.86) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, X.; Lai, H.; Mi, B.; Qi, X.; Gan, W.; Du, H. Associations of Coarse Grain Intake with Undiagnosed Hypertension among Chinese Adults: Results from the China Kadoorie Biobank. Nutrients 2020, 12, 3814. https://doi.org/10.3390/nu12123814
Liu X, Lai H, Mi B, Qi X, Gan W, Du H. Associations of Coarse Grain Intake with Undiagnosed Hypertension among Chinese Adults: Results from the China Kadoorie Biobank. Nutrients. 2020; 12(12):3814. https://doi.org/10.3390/nu12123814
Chicago/Turabian StyleLiu, Xin, Hao Lai, Baibing Mi, Xin Qi, Wei Gan, and Huaidong Du. 2020. "Associations of Coarse Grain Intake with Undiagnosed Hypertension among Chinese Adults: Results from the China Kadoorie Biobank" Nutrients 12, no. 12: 3814. https://doi.org/10.3390/nu12123814
APA StyleLiu, X., Lai, H., Mi, B., Qi, X., Gan, W., & Du, H. (2020). Associations of Coarse Grain Intake with Undiagnosed Hypertension among Chinese Adults: Results from the China Kadoorie Biobank. Nutrients, 12(12), 3814. https://doi.org/10.3390/nu12123814







