Physical and Psychological Effects Related to Food Habits and Lifestyle Changes Derived from COVID-19 Home Confinement in the Spanish Population
Abstract
1. Introduction
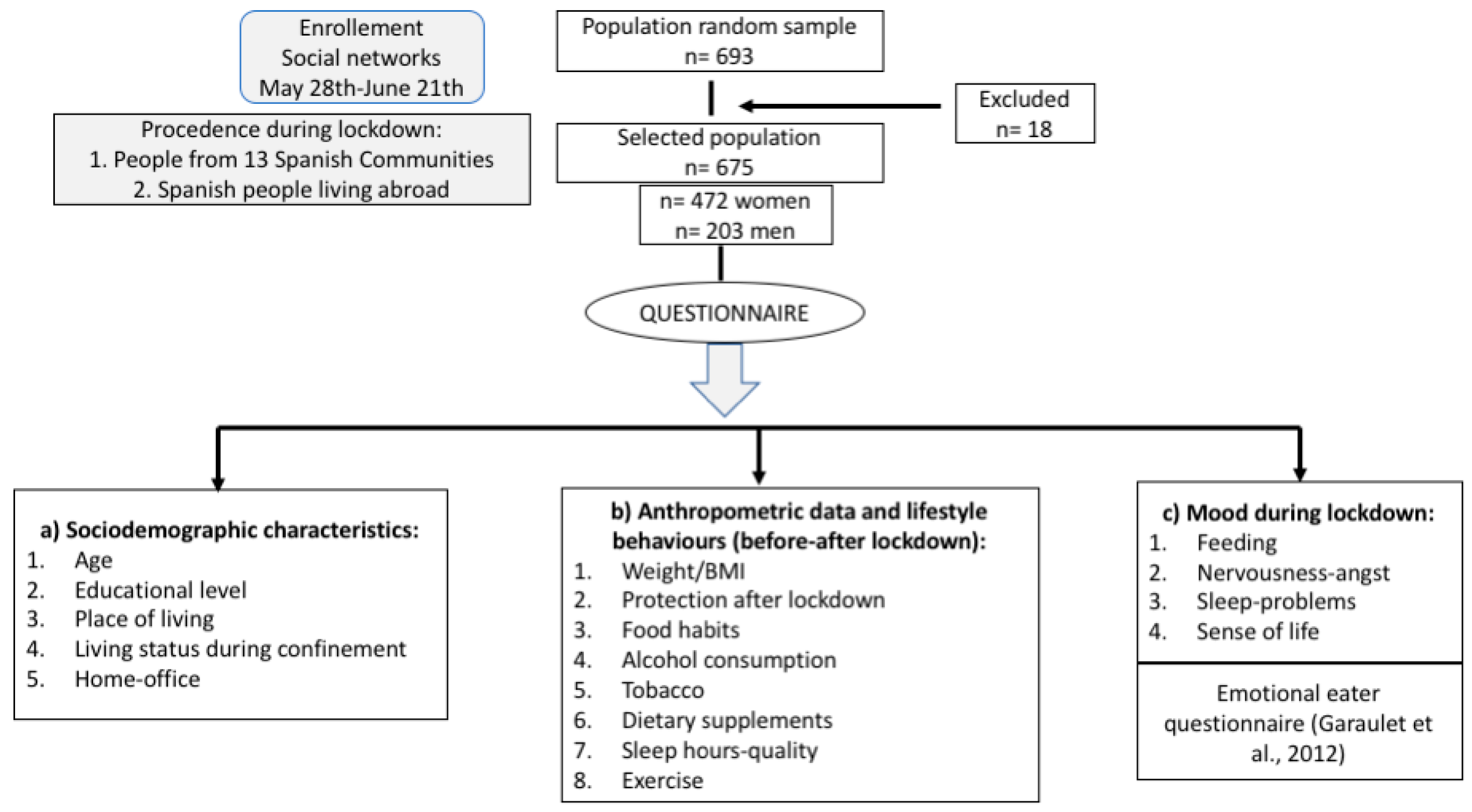
2. Materials and Methods
2.1. Participants and Study Design
2.2. Data Collection
- Socio-demographic characteristics: age, gender, educational level, place of living during confinement, living status during confinement (alone, 1 person, 2 people, 3 people, >4 or more people) and home office (yes or no).
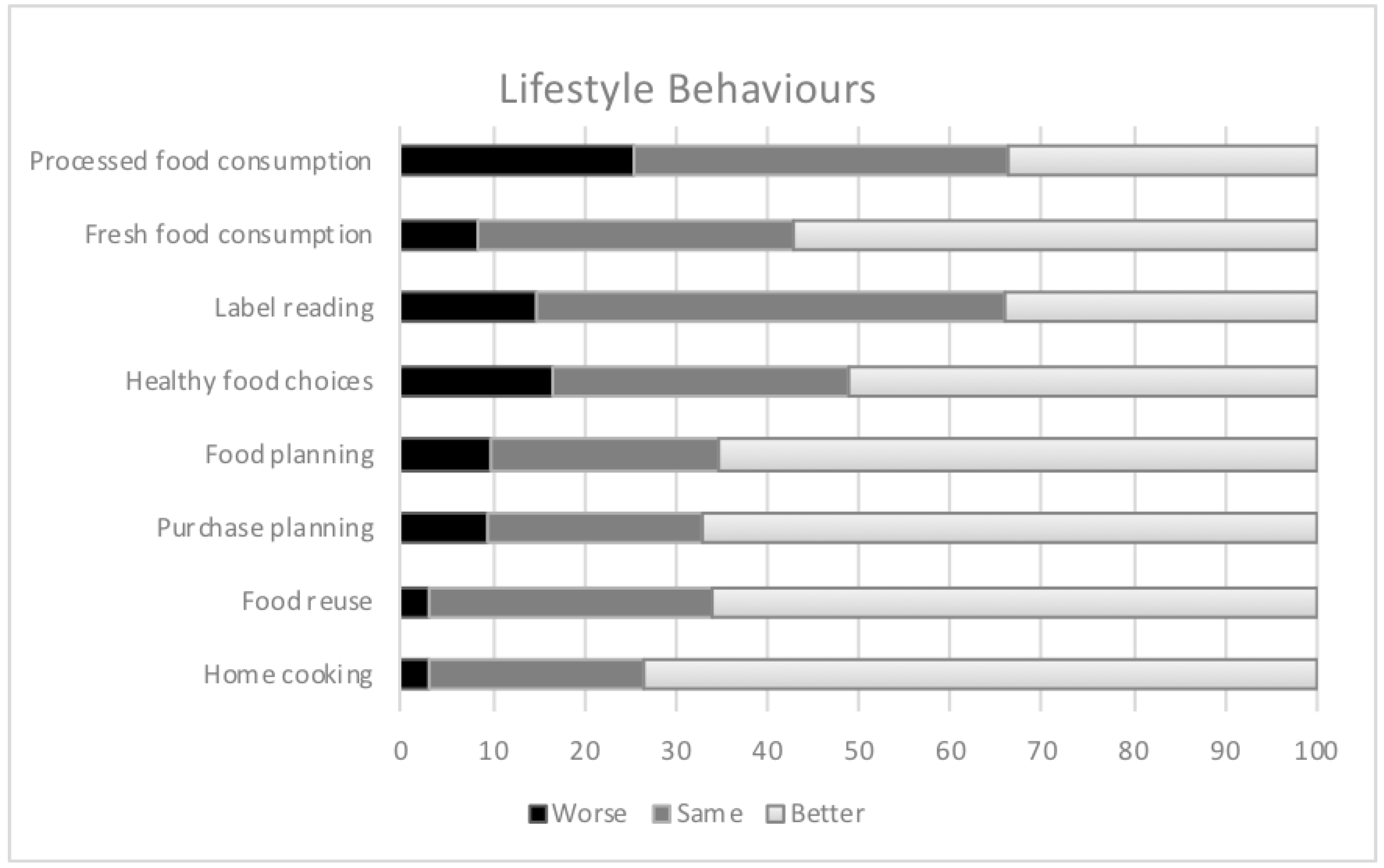
- Lifestyle behaviors adopted during lockdown with respect to pre-epidemic conditions:
- Anthropometric data. Body Mass Index (BMI) calculated as body weight in kg divided by height in meters squared; height and weight before and during confinement. According to the criteria of the World Health Organization, the BMI was categorized as: underweight (below 18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2) and obese (above 30.0 kg/m2) [18].
- Protection used during lockdown (no use of protection, handwashing, gloves, mask, protective screen).
- Food habits: Current diet; whether quarantine resulted in change in dietary habits, increased food consumption, specific food consumed, snacking, and specific type of cooking during lockdown; daily number of consumed meals and frequency of meals before and during lockdown; sources of food during isolation: methods for purchasing or obtaining food; three foods most often consumed; soft drinks and type consumed.
- Frequency and type of alcohol consumption.
- Smoking frequency during confinement.
- Dietary supplements consumption during confinement
- Sleep hours before and during lockdown and sleep quality during confinement.
- Exercise before and during the lockdown with respect to the time and intensity dedicated.
- Mood changes during lockdown with respect to feeding, nervousness, sleep-problems, overall feeling about life.
2.3. Data Analysis
3. Results
3.1. Socio-Demographic Characteristics
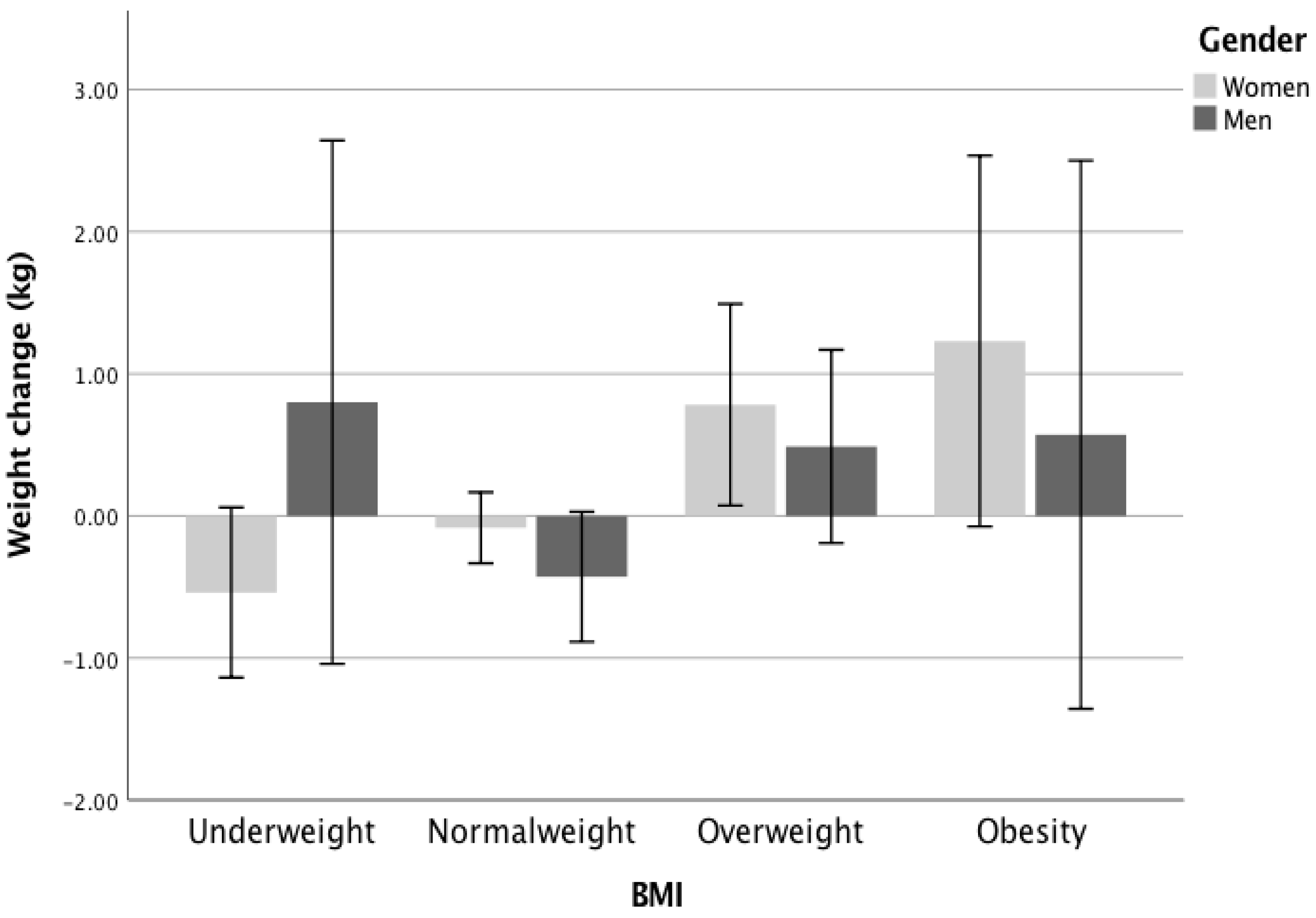
3.2. Anthropometric Data
3.3. Intake of Dietary Supplements
3.4. Changes in Alcohol and Tobacco Consumption
3.5. Physical Exercise and Sleep
3.6. Influences on Emotional Status
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
References
- Fauci, A.S.; Morens, D.M. The Perpetual Challenge of Infectious Diseases. New Engl. J. Med. 2012, 366, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Jribi, S.; Ben Ismail, H.; Doggui, D.; Debbabi, H. COVID-19 virus outbreak lockdown: What impacts on household food wastage? Environ. Dev. Sustain. 2020, 22, 3939–3955. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Novel Coronavirus (2019-nCoV) Situation Report-209; WHO: Geneva, Switzerland, 2020.
- Gorbalenya, A.E.; Baker, S.C.; Baric, R.S.; de Groot, R.J.; Drosten, C.; Gulyaeva, A.A.; Haagmans, B.L.; Lauber, C.; Leontovich, A.M.; Neuman, B.W.; et al. The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 2020, 5, 536–544. [Google Scholar]
- Burki, T. Outbreak of coronavirus disease 2019. Lancet Infect. Dis. 2020, 20, 292–293. [Google Scholar] [CrossRef]
- Yu, J.; Chai, P.; Ge, S.; Fan, X. Recent Understandings Toward Coronavirus Disease 2019 (COVID-19): From Bench to Bedside. Front. Cell Dev. Biol. 2020, 8, 476. [Google Scholar] [CrossRef]
- Anderson, A.S.; Good, D.J. Increased body weight affects academic performance in university students. Prev. Med. Rep. 2016, 5, 220–223. [Google Scholar] [CrossRef]
- Rodríguez-Pérez, C.; Molina-Montes, E.; Verardo, V.; Artacho, R.; García-Villanova, B.; Guerra-Hernández, E.J.; Ruíz-López, M.D. Changes in Dietary Behaviours during the COVID-19 Outbreak Confinement in the Spanish COVIDiet Study. Nutrients 2020, 12, 1730. [Google Scholar] [CrossRef]
- Moynihan, A.B.; Van Tilburg, W.A.P.; Igou, E.R.; Ewisman, A.; Donnelly, A.E.; Mulcaire, J.B. Eaten up by boredom: Consuming food to escape awareness of the bored self. Front. Psychol. 2015, 6, 369. [Google Scholar] [CrossRef]
- IASC. Joint System-Wide Operational Guidance on Data Responsibility and Challenges during the COVID-19 Response; IASC: Geneva, Switzerland, 2020. [Google Scholar]
- Frühbeck, G.; Baker, J.L.; Busetto, L.; Dicker, D.; Goossens, G.H.; Halford, J.C.; Handjieva-Darlenska, T.; Hassapidou, M.; Holm, J.-C.; Lehtinen-Jacks, S.; et al. European Association for the Study of Obesity Position Statement on the Global COVID-19 Pandemic. Obes. Facts 2020, 13, 292–296. [Google Scholar] [CrossRef]
- Herman, C.P.; Mack, D. Restrained and unrestrained eating1. J. Pers. 1975, 43, 647–660. [Google Scholar] [CrossRef]
- Zachary, Z.; Brianna, F.; Brianna, L.; Garrett, P.; Jade, W.; Alyssa, D.; Mikayla, K. Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obes. Res. Clin. Pr. 2020, 14, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz, C.; Gökmen, V. Neuroactive compounds in foods: Occurrence, mechanism and potential health effects. Food Res. Int. 2020, 128, 108744. [Google Scholar] [CrossRef] [PubMed]
- Rodrãguez-Martãn, B.C.; Emeule, A. Food craving: New contributions on its assessment, moderators, and consequences. Front. Psychol. 2015, 6, 21. [Google Scholar] [CrossRef]
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020, 180, 934–943. [Google Scholar] [CrossRef] [PubMed]
- Muscogiuri, G.; Barrea, L.; Savastano, S.; Colao, A. Nutritional recommendations for CoVID-19 quarantine. Eur. J. Clin. Nutr. 2020, 74, 850–851. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Obesity. Preventing and Managing the Global Epidemic. Report of a WHO Consultation. Available online: https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ (accessed on 10 August 2020).
- Garaulet, M.; Canteras, M.; Morales, E.; López-Guimera, G.; Sánchez-Carracedo, D.; Corbalán-Tutau, M.D. Validation of a questionnaire on emotional eating for use in cases of obesity: The Emotional Eater Questionnaire (EEQ). Nutr. Hosp. 2012, 27, 645–651. [Google Scholar]
- Mattioli, A.V.; Sciomer, S.; Cocchi, C.; Maffei, S.; Gallina, S. Quarantine during COVID-19 outbreak: Changes in diet and physical activity increase the risk of cardiovascular disease. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1409–1417. [Google Scholar] [CrossRef]
- Bennett, P.; Calman, K.; Curtis, S.; Fischbacher-Smith, D. Risk Communication and Public Health, 2nd ed.; Oxford University Press: Oxford, UK, 2010. [Google Scholar]
- Sánchez-Sánchez, E.; Ramírez-Vargas, G.; Avellaneda-López, Y.; Orellana-Pecino, J.I.; García-Marín, E.; Díaz-Jimenez, J. Eating Habits and Physical Activity of the Spanish Population during the COVID-19 Pandemic Period. Nutrients 2020, 12, 2826. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 1–15. [Google Scholar] [CrossRef]
- Földi, M.; Farkas, N.; Kiss, S.; Zádori, N.; Váncsa, S.; Szakó, L.; Dembrovszky, F.; Solymár, M.; Bartalis, E.; Szakács, Z.; et al. Obesity is a risk factor for developing critical condition in COVID-19 patients: A systematic review and meta-analysis. Obes. Rev. 2020, 21, e13095. [Google Scholar] [CrossRef]
- Sattar, N.; Ho, F.K.; Gill, J.M.; Ghouri, N.; Gray, S.R.; Celis-Morales, C.A.; Katikireddi, S.V.; Berry, C.; Pell, J.P.; McMurray, J.J.; et al. BMI and future risk for COVID-19 infection and death across sex, age and ethnicity: Preliminary findings from UK biobank. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1149–1151. [Google Scholar] [CrossRef] [PubMed]
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef] [PubMed]
- Verity, R.; Okell, L.C.; Dorigatti, I.; Winskill, P.; Whittaker, C.; Imai, N.; Cuomo-Dannenburg, G.; Thompson, H.; Walker, P.; Fu, H.; et al. Estimates of the severity of COVID-19 disease. medRxiv 2020. [Google Scholar] [CrossRef]
- Petrakis, D.; Margină, D.; Tsarouhas, K.; Tekos, F.; Stan, M.; Nikitovic, D.; Kouretas, D.; Spandidos, D.A.; Tsatsakis, A. Obesity-a risk factor for increased COVID-19 prevalence, severity and lethality (Review). Mol. Med. Rep. 2020, 22, 9–19. [Google Scholar] [CrossRef]
- Petrova, D.; Salamanca-Fernández, E.; Barranco, M.R.; Pérez, P.N.; Moleón, J.J.J.; Sánchez, M.J. La obesidad como factor de riesgo en personas con COVID-19: Posibles mecanismos e implicaciones. Atención Primaria 2020. [Google Scholar] [CrossRef]
- Ruiz-Roso, M.B.; Padilha, P.D.C.; Mantilla-Escalante, D.C.; Ulloa, N.; Brun, P.; Acevedo-Correa, D.; Peres, W.A.F.; Martorell, M.; Aires, M.T.; Cardoso, L.D.O.; et al. Covid-19 Confinement and Changes of Adolescent’s Dietary Trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients 2020, 12, 1807. [Google Scholar] [CrossRef]
- Zhao, A.; Li, Z.; Ke, Y.; Huo, S.; Ma, Y.; Zhang, Y.; Zhang, J.; Ren, Z. Dietary Diversity among Chinese Residents during the COVID-19 Outbreak and Its Associated Factors. Nutrients 2020, 12, 1699. [Google Scholar] [CrossRef]
- Butler, M.J.; Barrientos, R.M. The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain, Behav. Immun. 2020, 87, 53–54. [Google Scholar] [CrossRef]
- Michienzi, S.M.; Badowski, M.E. Can vitamins and/or supplements provide hope against coronavirus? Drugs Context 2020, 9, 1–29. [Google Scholar] [CrossRef]
- Grant, W.B.; Lahore, H.; McDonnell, S.L.; Baggerly, C.A.; French, C.B.; Aliano, J.L.; Bhattoa, H.P. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients 2020, 12, 988. [Google Scholar] [CrossRef]
- Chodkiewicz, J.; Talarowska, M.; Miniszewska, J.; Nawrocka, N.; Bilinski, P. Alcohol Consumption Reported during the COVID-19 Pandemic: The Initial Stage. Int. J. Environ. Res. Public Health 2020, 17, 4677. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Olavarría, D.; Latorre-Román, P.Á.; Guzmán-Guzmán, I.P.; Jerez-Mayorga, D.; Caamaño-Navarrete, F.; Delgado-Floody, P. Positive and Negative Changes in Food Habits, Physical Activity Patterns, and Weight Status during COVID-19 Confinement: Associated Factors in the Chilean Population. Int. J. Environ. Res. Public Health 2020, 17, 5431. [Google Scholar] [CrossRef]
- Scarmozzino, F.; Visioli, F. Covid-19 and the Subsequent Lockdown Modified Dietary Habits of Almost Half the Population in an Italian Sample. Foods 2020, 9, 675. [Google Scholar] [CrossRef] [PubMed]
- López-Bueno, R.; Calatayud, J.; Ezzatvar, Y.; Casajús, J.A.; Smith, L.; Andersen, L.L.; López-Sánchez, G.F. Association Between Current Physical Activity and Current Perceived Anxiety and Mood in the Initial Phase of COVID-19 Confinement. Front. Psychiatry 2020, 11, 729. [Google Scholar] [CrossRef]
- Clay, J.M.; O Parker, M. Alcohol use and misuse during the COVID-19 pandemic: A potential public health crisis? Lancet Public Health 2020, 5, e259. [Google Scholar] [CrossRef]
- Pérez-Rodrigo, C.; Citores, M.G.; Hervás Bárbara, G.; Litago, F.R.; Casis Sáenz, L.; Aranceta-Bartrina, J.; Val, V.A.; López-Sobaler, A.M.; Martínez De Victoria, E.; Ortega, R.M.; et al. Cambios en los hábitos alimentarios durante el periodo de confinamiento por la pandemia COVID-19 en Espanña. Rev. Esp. Nutr. Comunitaria 2020, 26, 28010. [Google Scholar] [CrossRef]
- Ozamiz-Etxebarria, N.; Dosil-Santamaria, M.; Picaza-Gorrochategui, M.; Idoiaga-Mondragon, N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad. Saúde Pública 2020, 36, e00054020. [Google Scholar] [CrossRef]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, Anxiety and Stress during COVID-19: Associations with Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef]
- González-Sanguino, C.; Ausín, B.; ÁngelCastellanos, M.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain, Behav. Immun. 2020, 87, 172–176. [Google Scholar] [CrossRef]
- Morin, C.M.; On behalf of the Canadian Sleep and Circadian Network; Carrier, J.; Bastien, C.; Godbout, R. Sleep and circadian rhythm in response to the COVID-19 pandemic. Can. J. Public Health 2020, 111, 654–657. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Jiang, Y.; Wang, G.; Meng, M.; Zhu, Q.; Mei, H.; Liu, S.; Jiang, F. Associations of short sleep duration with appetite-regulating hormones and adipokines: A systematic review and meta-analysis. Obes. Rev. 2020, 21. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain. Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Chen, P.; Mao, L.; Nassis, G.P.; Harmer, P.; Ainsworth, B.E.; Li, F. Coronavirus disease (COVID-19): The need to maintain regular physical activity while taking precautions. J. Sport Health Sci. 2020, 9, 103–104. [Google Scholar] [CrossRef]
- Schuch, F.B.; Stubbs, B. The Role of Exercise in Preventing and Treating Depression. Curr. Sports Med. Rep. 2019, 18, 299–304. [Google Scholar] [CrossRef]
- Marques, A.; De Matos, M.G.; Bordado, J.; Gouveia, É.R.; Peralta, M.; Gomez-Baya, D. Different levels of physical activity and depression symptoms among older adults from 18 countries: A population-based study from the Survey of Health, Ageing and Retirement in Europe (SHARE). Eur. J. Sport Sci. 2020, 1–8. [Google Scholar] [CrossRef]
- Andrade, E.; Andrade, E.; Arce, C.; Francisco, C.; De Torrado, J.; Garrido, J. Abbreviated version in spanish of the POMS questionnaire for adult athletes and general population. Rev. Psicol. Deport. 2013, 22, 95–102. [Google Scholar]
- Casagrande, M.; Favieri, F.; Tambelli, R.; Forte, G. The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020, 75, 12–20. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Mikolajczyk, R.T.; El Ansari, W.; Maxwell, A.E. Food consumption frequency and perceived stress and depressive symptoms among students in three European countries. Nutr. J. 2009, 8, 31. [Google Scholar] [CrossRef] [PubMed]
- Bellisle, F. Meals and snacking, diet quality and energy balance. Physiol. Behav. 2014, 134, 38–43. [Google Scholar] [CrossRef]
- Bilici, S.; Ayhan, B.; Karabudak, E.; Koksal, E. Factors affecting emotional eating and eating palatable food in adults. Nutr. Res. Pr. 2020, 14, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Antunes, R.; Frontini, R.; Amaro, N.; Salvador, R.; Matos, R.; Morouço, P.; Rebelo-Gonçalves, R. Exploring Lifestyle Habits, Physical Activity, Anxiety and Basic Psychological Needs in a Sample of Portuguese Adults during COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 4360. [Google Scholar] [CrossRef] [PubMed]
- Ferrell, E.L.; Watford, T.S.; Braden, A. Emotion regulation difficulties and impaired working memory interact to predict boredom emotional eating. Appetite 2020, 144, 104450. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
| All (n = 675) | Women (N = 472) | Men (N = 203) | p-Value * | |
|---|---|---|---|---|
| Age (years) | 39.1 (SD 12.9) | 39 (SD 12.8) | 39.2 (SD 13.2) | 0.888 |
| Education, N (%) | 0.138 | |||
| Until middle School | 6 (0.9) | 2 (0.4) | 4 (2.0) | |
| High School | 31 (4.6) | 19 (4.0) | 12 (5.9) | |
| Vocational Training | 58 (8.6) | 36 (7.6) | 22 (10.8) | |
| Undergraduate | 329 (48.7) | 238 (50.4) | 91 (44.8) | |
| Postgraduate | 181 (26.8) | 127 (26.9) | 54 (26.6) | |
| PhD | 65 (9.6) | 45 (9.5) | 20 (9.9) | |
| Others | 5 (0.7) | 5 (1.1) | 0 (0.0) | |
| Living status during confinement | 0.659 | |||
| Alone | 69 (10.2) | 50 (10.6) | 19 (9.4) | |
| 1 person | 161 (23.9) | 109 (23.1) | 52 (25.6) | |
| 2 people | 158 (23.4) | 106 (22.5) | 52 (25.6) | |
| 3 people | 151 (22.4) | 106 (22.5) | 45 (22.2) | |
| ≥4 people | 136 (20.1) | 101 (21.4) | 35 (17.2) | |
| Home-office, N (%) | 0.707 | |||
| Yes | 472 (69.9) | 328 (69.5) | 59 (29.1) | |
| No | 203 (30.1) | 144 (30.5) | 144 (70.9) | |
| Protection used after lockdown N (%) | ||||
| Mask | 667 (99.4) | 469 (99.4) | 202 (99.5) | 0.044 |
| Gloves | 167 (24.7) | 120 (25.4) | 47 (23.2) | 0.531 |
| All (n = 675) | Women (N = 472) | Men (N = 203) | p-Value * | Effect Size | |
|---|---|---|---|---|---|
| Weight before (kg) | 68.7 (SD 15.3) | 63.5 (SD 13.4) | 80.5 (SD 13.4) | <0.001 | 0.056 |
| Weight after (kg) | 68.8 (SD 15.8) | 63.7 (SD 14.2) | 80.5 (SD 13.5) | <0.001 | 0.234 |
| Height (m) | 170.3 (SD 35.5) | 166.7 (SD 41.5) | 178.8 (SD 9.9) | <0.001 | 0.024 |
| BMI before (kg/m2) | 23.9 (SD 4.9) | 23.4 (SD 5.2) | 25.2 (SD 4.0) | <0.001 | 0.031 |
| BMI after (kg/m2) | 24.2 (SD 10.8) | 23.8 (SD 12.6) | 25.2 (SD 4.0) | <0.001 | 0.037 |
| Change in body weight (kg) | 0.12 (SD 2.7) | 0.15 (SD 2.6) | 0.07 (SD 2.8) | 0.758 | 0.001 |
| Variable | Weight Variation | BMI before Confinement | BMI during Confinement | |||
|---|---|---|---|---|---|---|
| Rs | p-Value | Rs | p-Value | Rs | p-Value | |
| Age | 0.138 | <0.01 | 0.297 | <0.01 | 0.318 | <0.01 |
| Number of meals | −0.055 | 0.15 | −0.089 | 0.02 | −0.104 | <0.01 |
| Sleep (h/day) | −0.064 | 0.09 | −0.204 | <0.01 | −0.202 | <0.01 |
| EEQ | 0.192 | <0.01 | 0.185 | <0.01 | 0.223 | <0.01 |
| Variable | Number (%) | Weight Change (kg) | p-Value | Effect Size |
|---|---|---|---|---|
| Gender | ||||
| Men | 472 (69.9) | 0.15 | ||
| Women | 203 (30.1) | 0.07 | 0.758 | 0.001 |
| Age (years) * | 0.012 | 0.089 | ||
| 18–30 | 167 (24.7) | −0.26 | ||
| 30–65 | 487 (72.1) | 0.27 | ||
| >65 | 21 (3.1) | −0.14 | ||
| Living alone | 0.913 | 0.001 | ||
| No | 69 (10.2) | 0.12 | ||
| Yes | 606 (89.8) | 0.13 | ||
| BMI before confinement | 0.02 | |||
| ≤25 | 455 (67.4) | 0.14 | ||
| >25 | 220 (32.6) | 0.09 | 0.41 | |
| Dietary | 0.009 | |||
| supplements | ||||
| Yes | 137 (20.3) | 0.01 | ||
| No | 538 (79.7) | 0.62 | 0.013 | |
| Active smokers | 0.003 | |||
| Yes | 116 (17.2) | 0.33 | ||
| No | 559 (82.8) | 0.08 | 0.985 | |
| Active alcohol drinkers | 0.002 | |||
| Yes | 185 (27.4) | 0.13 | ||
| No | 490 (72.6) | 0.12 | 0.758 | |
| Sleep during confinement | 0.04 | 0.006 | ||
| <7 h/day | 143 (21.2) | 0.47 | ||
| ≥7 h/day | 532 (78.8) | 0.03 | ||
| Exercise during confinement | 0.02 | |||
| Yes | 559 (82.8) | −0.05 | ||
| No | 116 (17.2) | 0.9 | 0.01 | |
| EEQ * | 0.031 | |||
| Non-emotional eater | 186 (27.6) | −0.37 | ||
| Low emotional eater | 268 (39.7) | −0.06 | ||
| Emotional eater | 147 (21.8) | 0.64 | ||
| Very emotional eater | 74 (11.0) | 1.03 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Moreno, M.; López, M.T.I.; Miguel, M.; Garcés-Rimón, M. Physical and Psychological Effects Related to Food Habits and Lifestyle Changes Derived from COVID-19 Home Confinement in the Spanish Population. Nutrients 2020, 12, 3445. https://doi.org/10.3390/nu12113445
López-Moreno M, López MTI, Miguel M, Garcés-Rimón M. Physical and Psychological Effects Related to Food Habits and Lifestyle Changes Derived from COVID-19 Home Confinement in the Spanish Population. Nutrients. 2020; 12(11):3445. https://doi.org/10.3390/nu12113445
Chicago/Turabian StyleLópez-Moreno, Miguel, Maria Teresa Iglesias López, Marta Miguel, and Marta Garcés-Rimón. 2020. "Physical and Psychological Effects Related to Food Habits and Lifestyle Changes Derived from COVID-19 Home Confinement in the Spanish Population" Nutrients 12, no. 11: 3445. https://doi.org/10.3390/nu12113445
APA StyleLópez-Moreno, M., López, M. T. I., Miguel, M., & Garcés-Rimón, M. (2020). Physical and Psychological Effects Related to Food Habits and Lifestyle Changes Derived from COVID-19 Home Confinement in the Spanish Population. Nutrients, 12(11), 3445. https://doi.org/10.3390/nu12113445






