Spousal Concordance in Dietary Behaviors and Metabolic Components, and Their Association: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Metabolic Components
2.3. Dietary Behaviors
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Study Sample
3.2. Patterns of Dietary Behaviors among Spouses
3.3. Patterns of Metabolic Components among Spouses
3.4. Association between Concordant Dietary Behaviors and Concordant Composite MCs
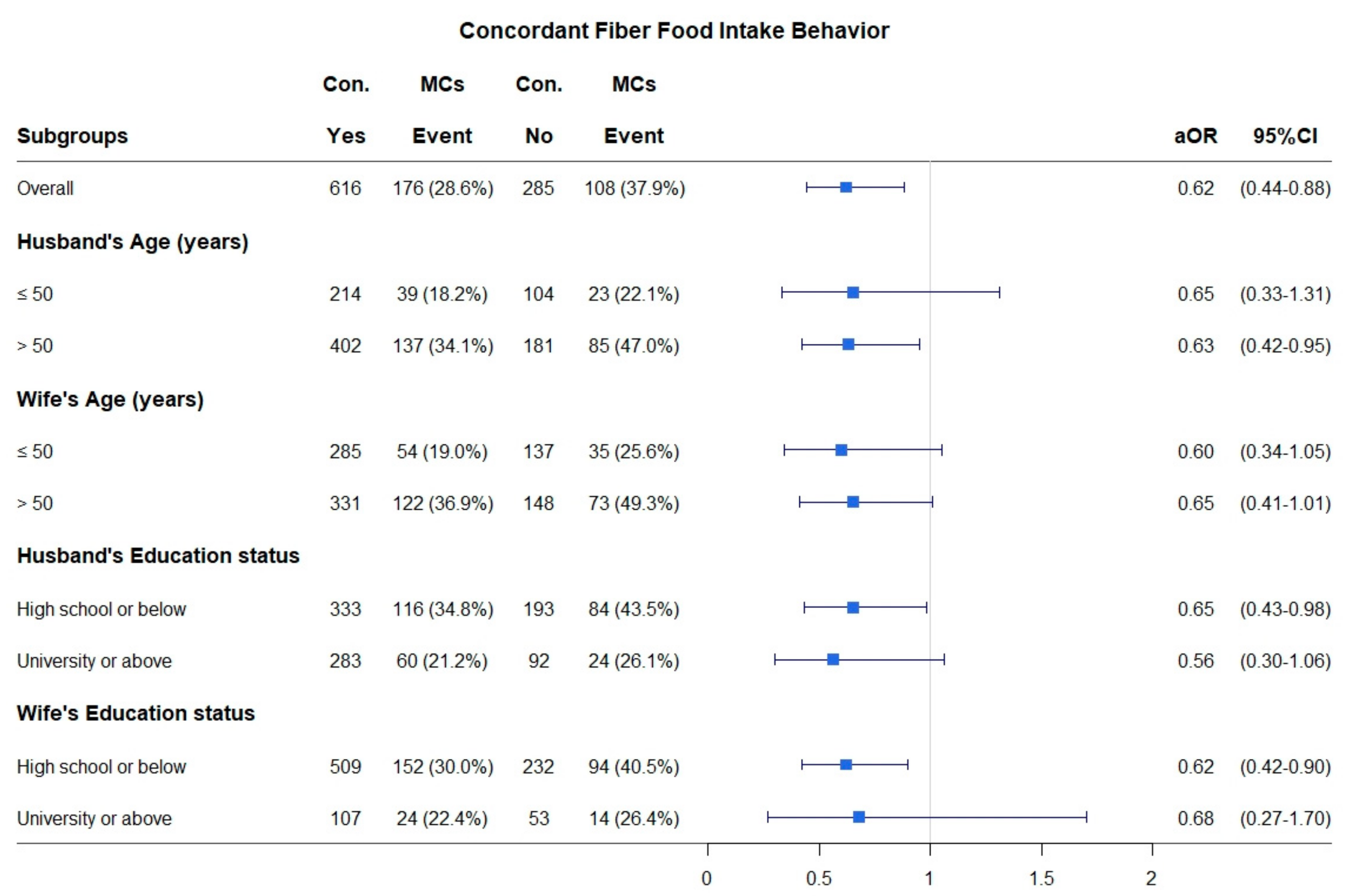
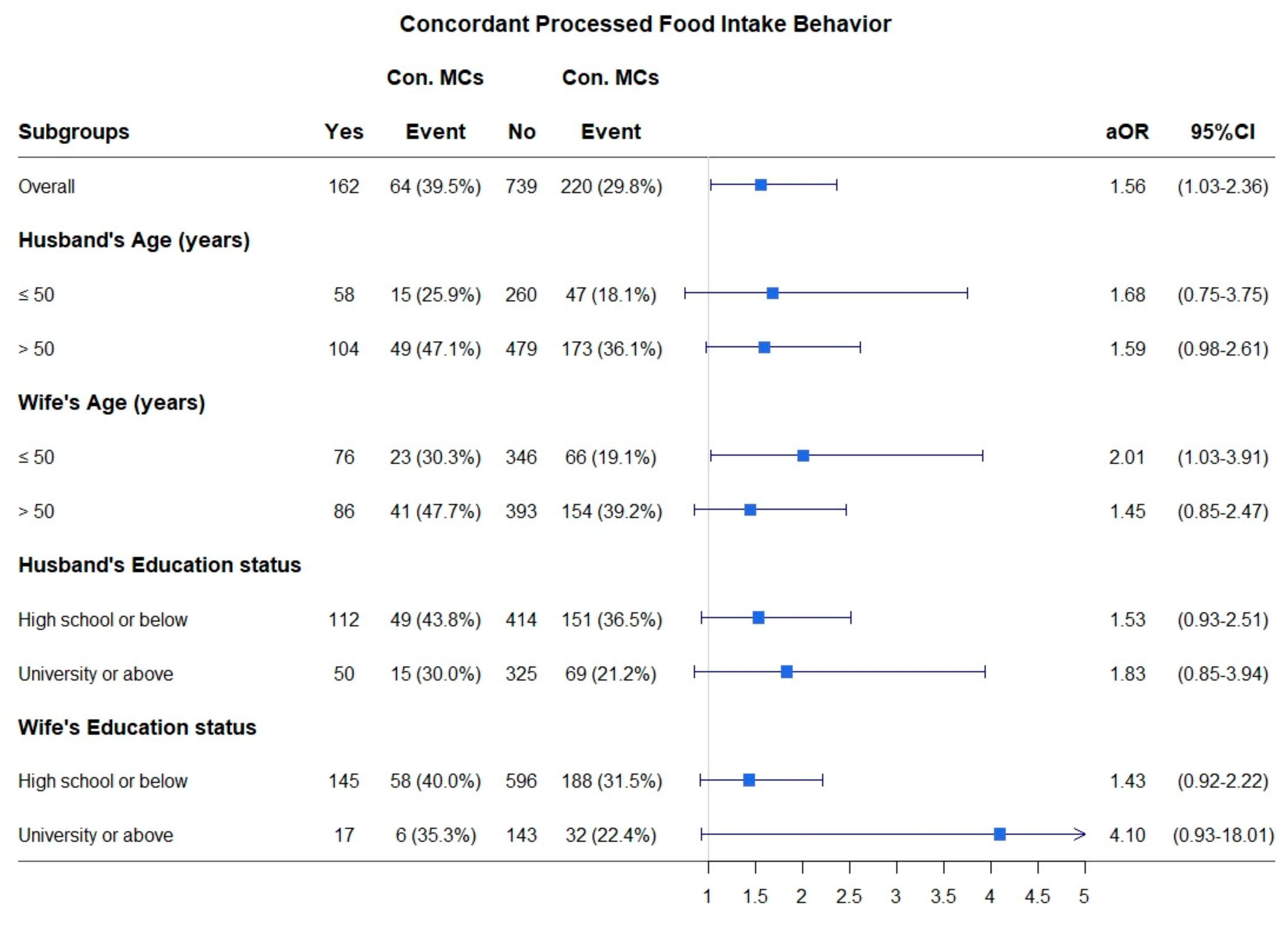
3.5. Stratified Analysis for the Association between Concordant Dietary Behaviors and Concordant Composite MCs
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Huang, P.L. A comprehensive definition for metabolic syndrome. Dis. Model. Mech. 2009, 2, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Kassi, E.; Pervanidou, P.; Kaltsas, G.; Chrousos, G.P. Metabolic syndrome: Definitions and controversies. BMC Med. 2011, 9, 48. [Google Scholar] [CrossRef] [PubMed]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef]
- Qin, Y.; Guo, Y.; Tang, Y.; Wu, C.; Zhang, X.; He, Q.; He, J. Concordance of chronic conditions among the household members in Shanghai: A cross-sectional study. BMJ Open 2019, 9, e031240. [Google Scholar] [CrossRef] [PubMed]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef]
- De La Iglesia, R.; Loria-Kohen, V.; Zulet, M.A.; Martínez, J.A.; Reglero, G.; De Molina, A.R. Dietary Strategies Implicated in the Prevention and Treatment of Metabolic Syndrome. Int. J. Mol. Sci. 2016, 17, 1877. [Google Scholar] [CrossRef]
- Dharavath, R.N.; Arora, S.; Bishnoi, M.; Kondepudi, K.K.; Chopra, K. High fat-low protein diet induces metabolic alterations and cognitive dysfunction in female rats. Metab. Brain Dis. 2019, 34, 1531–1546. [Google Scholar] [CrossRef]
- Boehm, B.O.; Claudi-Boehm, S. The Metabolic Syndrome. Scand. J. Clin. Lab. Investig. 2005, 65, 3–13. [Google Scholar] [CrossRef]
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef]
- Falba, T.A.; Sindelar, J.L. Spousal Concordance in Health Behavior Change. Health Serv. Res. 2007, 43, 96–116. [Google Scholar] [CrossRef]
- Jeong, S.; Cho, S.-I. Concordance in the Health Behaviors of Couples by Age: A Cross-sectional Study. J. Prev. Med. Public Health 2017, 51, 6–14. [Google Scholar] [CrossRef]
- Jurj, A.L.; Wen, W.; Li, H.-L.; Zheng, W.; Yang, G.; Xiang, Y.-B.; Gao, Y.-T.; Shu, X.-O. Spousal Correlations for Lifestyle Factors and Selected Diseases in Chinese Couples. Ann. Epidemiology 2006, 16, 285–291. [Google Scholar] [CrossRef]
- Torvik, F.A.; Røysamb, E.; Gustavson, K.; Idstad, M.; Tambs, K. Discordant and Concordant Alcohol Use in Spouses as Predictors of Marital Dissolution in the General Population: Results from the Hunt Study. Alcohol. Clin. Exp. Res. 2013, 37, 877–884. [Google Scholar] [CrossRef]
- Virtue, S.M.; Manne, S.L.; Kashy, D.; Heckman, C.J.; Zaider, T.; Kissane, D.W.; Kim, I.; Lee, D.; Olekson, G. Correspondence of physical activity and fruit/vegetable consumption among prostate cancer survivors and their spouses. Eur. J. Cancer Care 2015, 24, 827–839. [Google Scholar] [CrossRef]
- Gallardo-Alfaro, L.; Bibiloni, M.D.M.; Mascaró, C.M.; Montemayor, S.; Ruiz-Canela, M.; Salas-Salvadó, J.; Corella, D.; Fitó, M.; Romaguera, D.; Vioque, J.; et al. Leisure-Time Physical Activity, Sedentary Behaviour and Diet Quality are Associated with Metabolic Syndrome Severity: The PREDIMED-Plus Study. Nutrients 2020, 12, 1013. [Google Scholar] [CrossRef]
- Bloch, K.V.; Klein, C.H.; Silva, N.A.D.S.E.; Nogueira, A.D.R.; Salis, L.H.A. Socioeconomic aspects of spousal concordance for hypertension, obesity, and smoking in a community of Rio de Janeiro, Brazil. Arq. Bras. Cardiol. 2003, 80, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Goyal, A.; Gupta, Y.; Kalaivani, M.; Sankar, M.J.; Kachhawa, G.; Bhatla, N.; Gupta, N.; Tandon, N. Concordance of glycaemic and cardiometabolic traits between Indian women with history of gestational diabetes mellitus and their spouses: An opportunity to target the household. Diabetologia 2019, 62, 1357–1365. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.A.; Dhillon, P.K.; Kondal, D.; Jeemon, P.; Kahol, K.; Manimunda, S.P.; Purty, A.J.; Deshpande, A.; Negi, P.C.; Ladhani, S.; et al. Chronic disease concordance within Indian households: A cross-sectional study. PLoS Med. 2017, 14, e1002395. [Google Scholar] [CrossRef]
- Al-Sharbatti, S.S.; Abed, Y.I.; Al-Heety, L.M.; Basha, S.A. Spousal Concordance of Diabetes Mellitus among Women in Ajman, United Arab Emirates. Sultan Qaboos Univ. Med. J. 2016, 16, e197–e202. [Google Scholar] [CrossRef]
- Cunningham, S.A.; Adams, S.R.; Schmittdiel, J.A.; Ali, M.K. Incidence of diabetes after a partner’s diagnosis. Prev. Med. 2017, 105, 52–57. [Google Scholar] [CrossRef]
- Di Castelnuovo, A.; Quacquaruccio, G.; Donati, M.B.; De Gaetano, G.; Iacoviello, L. Spousal Concordance for Major Coronary Risk Factors: A Systematic Review and Meta-Analysis. Am. J. Epidemiol. 2008, 169, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hippisley-Cox, J.; Coupland, C.; Pringle, M.; Crown, N.; Hammersley, V. Married couples’ risk of same disease: Cross sectional study. BMJ 2002, 325, 636. [Google Scholar] [CrossRef]
- Meyler, D.; Stimpson, J.P.; Peek, M.K. Health concordance within couples: A systematic review. Soc. Sci. Med. 2007, 64, 2297–2310. [Google Scholar] [CrossRef] [PubMed]
- Regitz-Zagrosek, V.; Lehmkuhl, E.; Weickert, M.O. Gender differences in the metabolic syndrome and their role for cardiovascular disease. Clin. Res. Cardiol. 2006, 95, 136–147. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Gao, B.; Xing, Y.; Ming, J.; Bao, J.; Zhang, Q.; Wan, Y.; Ji, Q.; on behalf of the China National Diabetes and Metabolic Disorders Study Group. Gender Differences in the Prevalence and Development of Metabolic Syndrome in Chinese Population with Abdominal Obesity. PLoS ONE 2013, 8, e78270. [Google Scholar] [CrossRef]
- Novak, M.; Björck, L.; Welin, L.; Welin, C.; Manhem, K.; Rosengren, A. Gender differences in the prevalence of metabolic syndrome in 50-year-old Swedish men and women with hypertension born in 1953. J. Hum. Hypertens. 2011, 27, 56–61. [Google Scholar] [CrossRef]
- Beigh, S.H.; Jain, S. Prevalence of metabolic syndrome and gender differences. Bioinformation 2012, 8, 613–616. [Google Scholar] [CrossRef]
- Di Daniele, N.; Noce, A.; Vidiri, M.F.; Moriconi, E.; Marrone, G.; Annicchiarico-Petruzzelli, M.; D’Urso, G.; Tesauro, M.; Rovella, V.; De Lorenzo, A. Impact of Mediterranean diet on metabolic syndrome, cancer and longevity. Oncotarget 2016, 8, 8947–8979. [Google Scholar] [CrossRef]
- Ros, E.; Martínez-González, M.Á.; Estruch, R.; Salas-Salvadó, J.; Fitó, M.; Martínez, J.A.; Corella, D. Mediterranean Diet and Cardiovascular Health: Teachings of the PREDIMED Study. Adv. Nutr. 2014, 5, 330S–336S. [Google Scholar] [CrossRef]
- Aleixandre, A.; Miguel, M. Dietary Fiber in the Prevention and Treatment of Metabolic Syndrome: A Review. Crit. Rev. Food Sci. Nutr. 2008, 48, 905–912. [Google Scholar] [CrossRef]
- Sekgala, M.D.; Mchiza, Z.J.; Parker, W.-A.; Monyeki, K.D. Dietary Fiber Intake and Metabolic Syndrome Risk Factors among Young South African Adults. Nutrients 2018, 10, 504. [Google Scholar] [CrossRef] [PubMed]
- Julibert, A.; Bibiloni, M.D.M.; Mateos, D.; Angullo-Martinez, E.; Tur, J.A. Dietary Fat Intake and Metabolic Syndrome in Older Adults. Nutrients 2019, 11, 1901. [Google Scholar] [CrossRef]
- Wang, J.-Y.; Liang, Y.-W.; Yeh, C.-C.; Liu, C.-S.; Wang, C.-Y. Time-dependent risks of cancer clustering among couples: A nationwide population-based cohort study in Taiwan. BMJ Open 2018, 8, e018968. [Google Scholar] [CrossRef] [PubMed]
- Jun, S.Y.; Kang, M.; Kang, S.Y.; Lee, J.A.; Kim, Y.S. Spousal Concordance regarding Lifestyle Factors and Chronic Diseases among Couples Visiting Primary Care Providers in Korea. Korean J. Fam. Med. 2020, 41, 183–188. [Google Scholar] [CrossRef]
- Wang, J.-Y.; Hsieh, M.-H.; Lin, P.-C.; Liu, C.-S.; Chen, J.-D. Parallel contagion phenomenon of concordant mental disorders among married couples: A nationwide cohort study. J. Epidemiol. Community Health 2017, 71, 640–647. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Kim, M.; Won, C.W. Spousal Concordance of Physical Frailty in Older Korean Couples. Int. J. Environ. Res. Public Health 2020, 17, 4574. [Google Scholar] [CrossRef]
- Wang, J.-Y.; Liu, C.-S.; Lung, C.-H.; Yang, Y.-T.; Lin, M.-H. Investigating spousal concordance of diabetes through statistical analysis and data mining. PLoS ONE 2017, 12, e0183413. [Google Scholar] [CrossRef]
- Okuda, T.; Miyazaki, T.; Sakuragi, S.; Moriguchi, J.; Tachibana, H.; Ohashi, F.; Ikeda, M. Significant but weak spousal concordance of metabolic syndrome components in Japanese couples. Environ. Health Prev. Med. 2013, 19, 108–116. [Google Scholar] [CrossRef]
- Dhingra, D.; Michael, M.; Rajput, H.; Patil, R.T. Dietary fibre in foods: A review. J. Food Sci. Technol. 2011, 49, 255–266. [Google Scholar] [CrossRef]
- Syauqy, A.; Hsu, C.-Y.; Rau, H.-H.; Chao, J.C.J. Association of Dietary Patterns with Components of Metabolic Syndrome and Inflammation among Middle-Aged and Older Adults with Metabolic Syndrome in Taiwan. Nutrients 2018, 10, 143. [Google Scholar] [CrossRef]
- Giugliano, D.; Ceriello, A.; Esposito, K. The Effects of Diet on Inflammation. J. Am. Coll. Cardiol. 2006, 48, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Zou, J.; Chassaing, B.; Singh, V.; Pellizzon, M.; Ricci, M.; Fythe, M.D.; Kumar, M.V.; Gewirtz, A.T. Fiber-Mediated Nourishment of Gut Microbiota Protects against Diet-Induced Obesity by Restoring IL-22-Mediated Colonic Health. Cell Host Microbe 2018, 23, 41–53.e4. [Google Scholar] [CrossRef]
- Rinaldi, A.E.M.; Gabriel, G.F.C.P.; Moreto, F.; Corrente, J.E.; McLellan, K.C.P.; Burini, R.C. Dietary factors associated with metabolic syndrome and its components in overweight and obese Brazilian schoolchildren: A cross-sectional study. Diabetol. Metab. Syndr. 2016, 8, 58. [Google Scholar] [CrossRef] [PubMed]
- Steele, E.M.; Juul, F.; Neri, D.; Rauber, F.; Monteiro, C.A. Dietary share of ultra-processed foods and metabolic syndrome in the US adult population. Prev. Med. 2019, 125, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Tavares, L.F.; Fonseca, S.C.; Rosa, M.L.G.; Yokoo, E.M. Relationship between ultra-processed foods and metabolic syndrome in adolescents from a Brazilian Family Doctor Program. Public Health Nutr. 2011, 15, 82–87. [Google Scholar] [CrossRef]
- Joung, H.; Hong, S.; Song, Y.; Ahn, B.C.; Park, M.J. Dietary patterns and metabolic syndrome risk factors among adolescents. Korean J. Pediatr. 2012, 55, 128–135. [Google Scholar] [CrossRef]
- Chassaing, B.; Koren, O.; Goodrich, J.K.; Poole, A.C.; Srinivasan, S.; Ley, R.E.; Gewirtz, A.T. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nat. Cell Biol. 2015, 519, 92–96. [Google Scholar] [CrossRef]
- Spitzer, S.; Weber, D. Reporting biases in self-assessed physical and cognitive health status of older Europeans. PLoS ONE 2019, 14, e0223526. [Google Scholar] [CrossRef]
- Rosenman, R.; Tennekoon, V.; Hill, L.G. Measuring bias in self-reported data. Int. J. Behav. Health Res. 2011, 2, 320–332. [Google Scholar] [CrossRef]
- Hsiao, Y.C.; Wang, K.; Bair, M.-J. Prevalence of obesity and metabolic syndrome in aboriginals in southeastern Taiwan—A hospital-based study. J. Intern. Med. Taiwan 2011, 22, 48–56. [Google Scholar]
- Camhi, S.M.; Bray, G.A.; Bouchard, C.; Greenway, F.L.; Johnson, W.D.; Newton, R.L.; Ravussin, E.; Ryan, D.H.; Smith, S.R.; Katzmarzyk, P.T. The Relationship of Waist Circumference and BMI to Visceral, Subcutaneous, and Total Body Fat: Sex and Race Differences. Obesity 2011, 19, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Flegal, K.M.; Shepherd, J.A.; Looker, A.C.; Graubard, B.I.; Borrud, L.G.; Ogden, C.L.; Harris, T.B.; Everhart, J.E.; Schenker, N. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. Am. J. Clin. Nutr. 2008, 89, 500–508. [Google Scholar] [CrossRef] [PubMed]
- Sardinha, L.B.; Santos, D.A.; Silva, A.M.; Grøntved, A.; Andersen, L.B.; Ekelund, U. A Comparison between BMI, Waist Circumference, and Waist-to-Height Ratio for Identifying Cardio-Metabolic Risk in Children and Adolescents. PLoS ONE 2016, 11, e0149351. [Google Scholar] [CrossRef] [PubMed]
| Variables | Husband n (%) | Wife n (%) | Spousal Concordance * Pairs (%) |
|---|---|---|---|
| Age (years) | |||
| ≤50 | 318 (35.3) | 422 (46.8) | |
| 51–60 | 310 (34.4) | 284 (31.5) | |
| >60 | 273 (30.3) | 195 (21.6) | |
| Education status | |||
| High school or below | 526 (58.4) | 591 (65.6) | |
| University or above | 375 (41.6) | 310 (34.4) | |
| Dietary behaviors | |||
| High-fiber food intake | 665 (73.8) | 781 (86.7) | 616 (68.4) |
| Fish intake | 643 (71.4) | 684 (75.9) | 528 (58.6) |
| Red meat intake | 606 (67.3) | 587 (65.2) | 472 (52.4) |
| Processed food intake | 285 (31.6) | 277 (30.7) | 162 (18.0) |
| Biscuit or cake intake | 251 (27.9) | 333 (37.0) | 127 (14.1) |
| High-fat food intake | 195 (21.6) | 216 (24.0) | 88 (9.8) |
| Fast food intake | 99 (11.0) | 130 (14.4) | 42 (4.7) |
| Metabolic components | |||
| Overweight | 470 (52.2) | 300 (33.3) | 173 (19.2) |
| Hypertension | 223 (24.8) | 135 (15.0) | 58 (2.6) |
| Hypercholesterolemia | 121 (13.4) | 79 (8.8) | 23 (6.4) |
| Hyperlipidemia | 80 (8.9) | 33 (3.7) | 9 (1.0) |
| Variables | Comparison of Different Patterns among Couples | |||||
|---|---|---|---|---|---|---|
| H + W + | H − W − | H + W − | H − W + | ORMP | McNemar’s Test | |
| n (%) | n (%) | n (%) | n (%) | p Value | ||
| High-fiber food intake | 616 (68.4) | 71 (7.9) | 49 (5.4) | 165 (18.3) | 0.30 | <0.0001 *** |
| Fish intake | 528 (58.6) | 102 (11.3) | 115 (12.8) | 156 (17.3) | 0.74 | 0.0128 * |
| Red meat intake | 472 (52.4) | 180 (20.0) | 134 (14.9) | 115 (12.7) | 1.17 | 0.2286 |
| Processed food intake | 162 (18.0) | 501 (55.6) | 123 (13.6) | 115 (12.8) | 1.07 | 0.6041 |
| Biscuit or cake intake | 127 (14.1) | 444 (49.3) | 124 (13.8) | 206 (22.8) | 0.60 | <0.0001 *** |
| High-fat food intake | 88 (9.8) | 578 (64.1) | 107 (11.9) | 128 (14.2) | 0.84 | 0.1707 |
| Fast food intake | 42 (4.7) | 714 (79.2) | 57 (6.3) | 88 (9.8) | 0.65 | 0.0100 * |
| Variables | Comparison of Different Patterns among Couples | |||||
|---|---|---|---|---|---|---|
| H + W + | H − W − | H + W − | H − W + | ORMP | McNemar’s Test | |
| n (%) | n (%) | n (%) | n (%) | p Value | ||
| Overweight a | 173 (19.2) | 304 (33.7) | 297 (33.0) | 127 (14.1) | 2.34 | <0.0001 *** |
| Hypertension | 58 (6.4) | 601 (66.7) | 165 (18.3) | 77 (8.6) | 2.14 | <0.0001 *** |
| Hypercholesterolemia | 23 (2.5) | 723 (80.4) | 98 (10.9) | 56 (6.2) | 1.75 | 0.0007 *** |
| Hyperlipidemia | 9 (1.0) | 796 (88.4) | 71 (7.9) | 24 (2.7) | 2.96 | <0.0001 *** |
| Composite Metabolic Components b | 284 (31.5) | 204 (22.7) | 295 (32.7) | 118 (13.1) | 2.50 | <0.0001 *** |
| Variables | Crude | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | aOR | 95% CI | p Value | |
| Husband’s Age (years) | ||||||
| >50 vs. ≤50 (Reference) | 2.54 | (1.84, 3.51) | <0.0001 *** | 1.49 | (0.90, 2.48) | 0.1214 |
| Wife’s Age (years) | ||||||
| >50 vs. ≤50 (Reference) | 2.57 | (1.91, 3.46) | <0.0001 *** | 1.80 | (1.14, 2.85) | 0.0123 * |
| Husband’s Education level | ||||||
| University or above vs. High school or below (Reference) | 0.47 | (0.35, 0.64) | <0.0001 *** | 0.62 | (0.43, 0.88) | 0.0074 ** |
| Wife’s Education level | ||||||
| University or above vs. High school or below (Reference) | 0.63 | (0.42, 0.93) | 0.0205 * | 1.22 | (0.76, 1.97) | 0.4138 |
| Dietary behaviors | ||||||
| High-fiber food intake | ||||||
| Yes vs. No (Reference) | 0.66 | (0.49, 0.88) | 0.0052 ** | 0.62 | (0.44, 0.88) | 0.0074 ** |
| Fish intake | ||||||
| Yes vs. No (Reference) | 1.01 | (0.76, 1.35) | 0.9337 | 1.17 | (0.83, 1.63) | 0.3691 |
| Red meat intake | ||||||
| Yes vs. No (Reference) | 0.79 | (0.59, 1.04) | 0.0911 | 0.82 | (0.59, 1.15) | 0.2554 |
| Processed food intake | ||||||
| Yes vs. No (Reference) | 1.54 | (1.08, 2.19) | 0.0162 * | 1.56 | (1.03, 2.36) | 0.0340 * |
| Biscuit or cake intake | ||||||
| Yes vs. No (Reference) | 1.00 | (0.67, 1.50) | 0.9949 | 1.28 | (0.82, 1.99) | 0.2762 |
| High-fat food intake | ||||||
| Yes vs. No (Reference) | 1.14 | (0.72, 1.81) | 0.5850 | 1.28 | (0.73, 2.22) | 0.3897 |
| Fast food intake | ||||||
| Yes vs. No (Reference) | 0.76 | (0.38, 1.54) | 0.4477 | 0.76 | (0.34, 1.69) | 0.5021 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shih, D.-P.; Wen, C.-T.; Kuo, H.-W.; Liang, W.-M.; Liu, L.-F.; Su, C.-T.; Wang, J.-Y. Spousal Concordance in Dietary Behaviors and Metabolic Components, and Their Association: A Cross-Sectional Study. Nutrients 2020, 12, 3332. https://doi.org/10.3390/nu12113332
Shih D-P, Wen C-T, Kuo H-W, Liang W-M, Liu L-F, Su C-T, Wang J-Y. Spousal Concordance in Dietary Behaviors and Metabolic Components, and Their Association: A Cross-Sectional Study. Nutrients. 2020; 12(11):3332. https://doi.org/10.3390/nu12113332
Chicago/Turabian StyleShih, Dann-Pyng, Chu-Ting Wen, Hsien-Wen Kuo, Wen-Miin Liang, Li-Fan Liu, Chien-Tien Su, and Jong-Yi Wang. 2020. "Spousal Concordance in Dietary Behaviors and Metabolic Components, and Their Association: A Cross-Sectional Study" Nutrients 12, no. 11: 3332. https://doi.org/10.3390/nu12113332
APA StyleShih, D.-P., Wen, C.-T., Kuo, H.-W., Liang, W.-M., Liu, L.-F., Su, C.-T., & Wang, J.-Y. (2020). Spousal Concordance in Dietary Behaviors and Metabolic Components, and Their Association: A Cross-Sectional Study. Nutrients, 12(11), 3332. https://doi.org/10.3390/nu12113332






