Effects of the Daily Consumption of Stevia on Glucose Homeostasis, Body Weight, and Energy Intake: A Randomised Open-Label 12-Week Trial in Healthy Adults
Abstract
1. Introduction
2. Materials and Methods
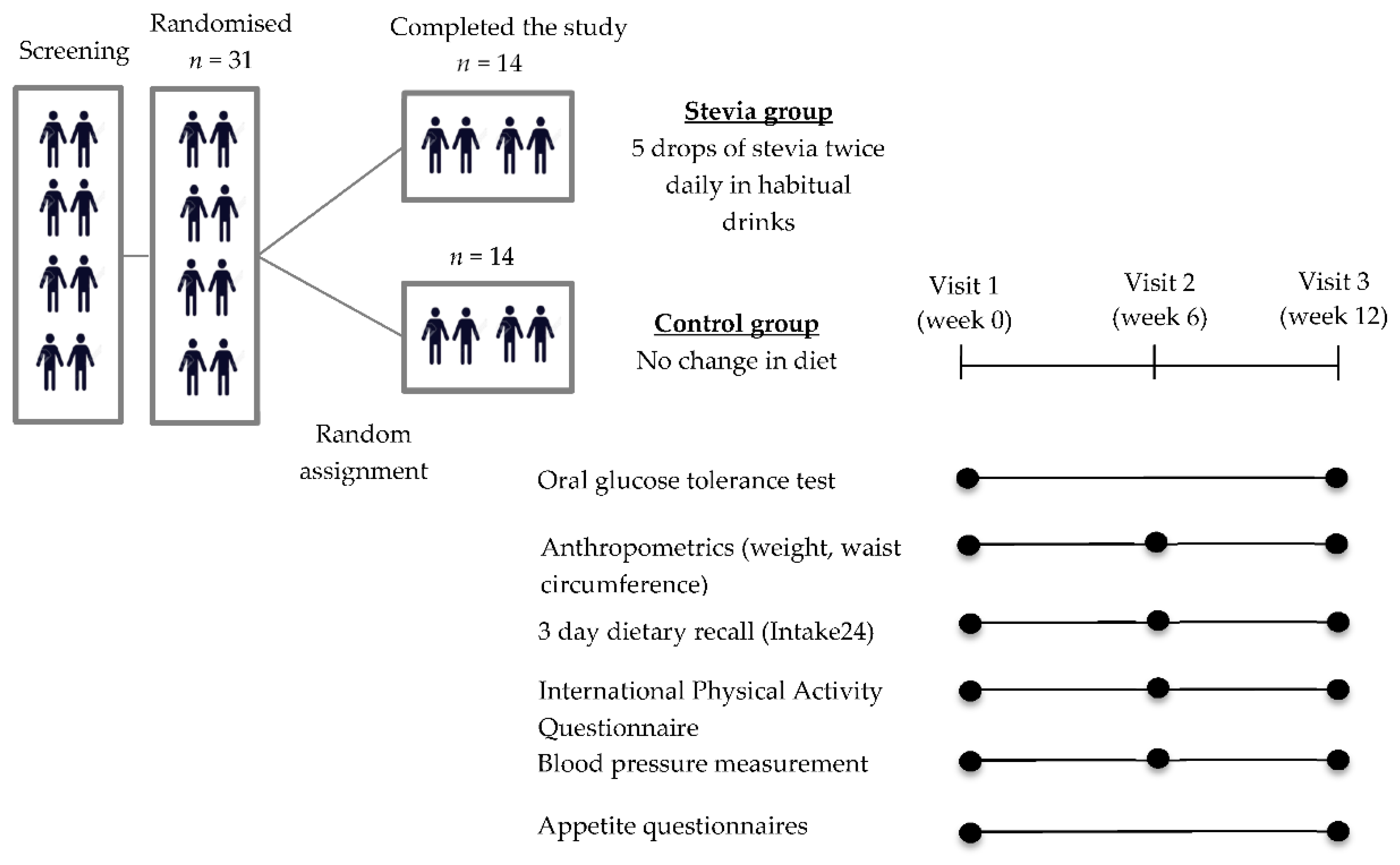
2.1. Study Design
2.2. Participants
2.3. Protocol
2.4. Analyte Assays
2.5. Compliance
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics
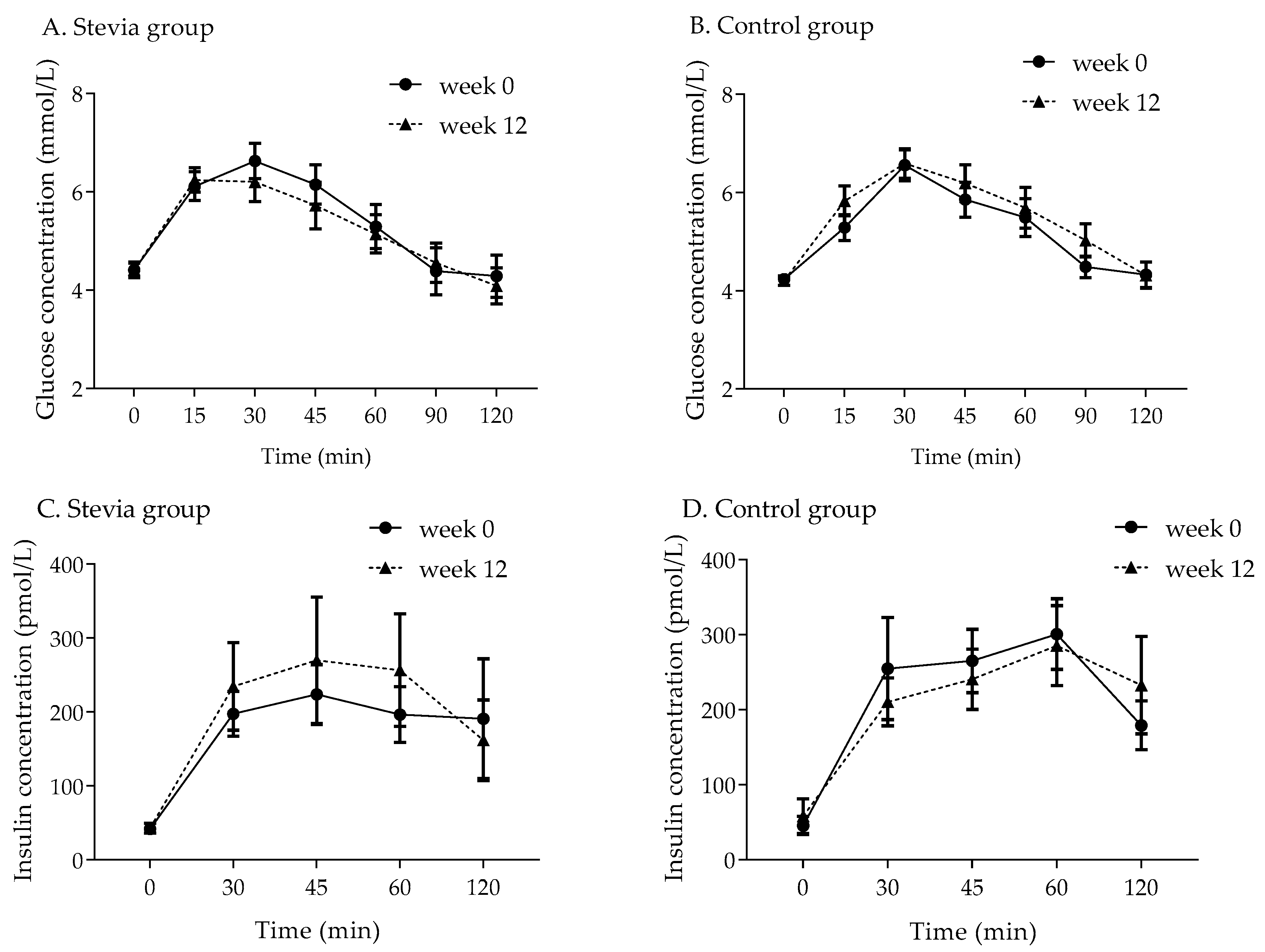
3.2. Glucose Response
3.3. Insulin Response
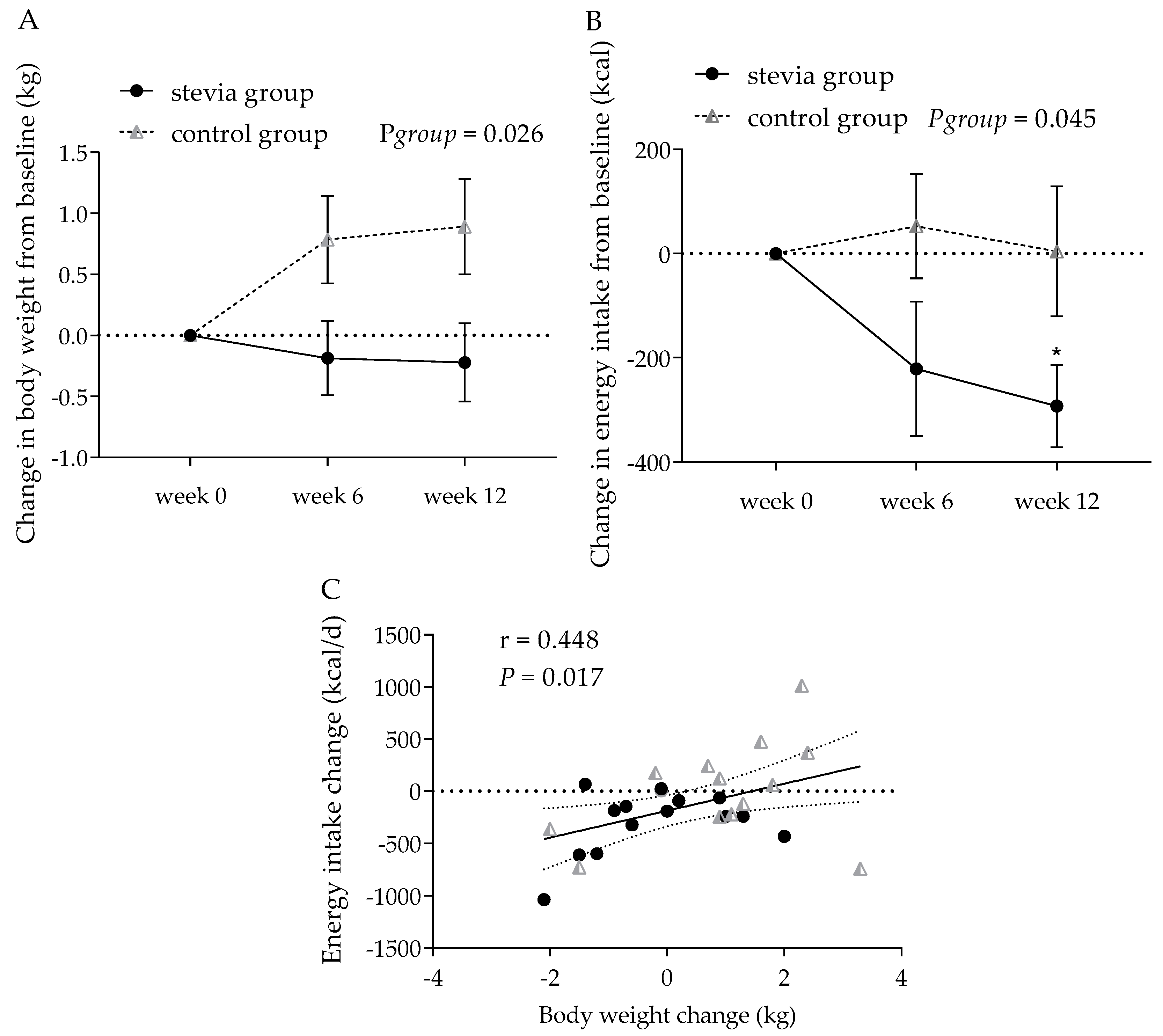
3.4. Body Weight and Other Anthropometric Indices
3.5. Energy Intake
3.6. Physical Activity
3.7. Appetite Expression
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Leung, C.W.; DiMatteo, S.G.; Gosliner, W.A.; Ritchie, L.D. Sugar-Sweetened Beverage and Water Intake in Relation to Diet Quality in U.S. Children. Am. J. Prev. Med. 2018, 54, 394–402. [Google Scholar] [CrossRef]
- Imamura, F.; O’Connor, L.; Ye, Z.; Mursu, J.; Hayashino, Y.; Bhupathiraju, S.N.; Forouhi, N.G. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: Systematic review, meta-analysis, and estimation of population attributable fraction. BMJ 2015, 351, h3576. [Google Scholar] [CrossRef]
- Pereira, M.A. Sugar-sweetened and artificially-sweetened beverages in relation to obesity risk. Adv. Nutr. 2014, 5, 797–808. [Google Scholar] [CrossRef] [PubMed]
- Nettleton, J.A.; Lutsey, P.L.; Wang, Y.; Lima, J.A.; Michos, E.D.; Jacobs, D.R. Diet Soda Intake and Risk of Incident Metabolic Syndrome and Type 2 Diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA)*. Diabetes Care 2009, 32, 688–694. [Google Scholar] [CrossRef]
- Fowler, S.P. Low-calorie sweetener use and energy balance: Results from experimental studies in animals, and large-scale prospective studies in humans. Physiol. Behav. 2016, 164, 517–523. [Google Scholar] [CrossRef]
- Miller, E.P.; Perez, V. Low-calorie sweeteners and body weight and composition: A meta-analysis of randomized controlled trials and prospective cohort studies. Am. J. Clin. Nutr. 2014, 100, 765–777. [Google Scholar] [CrossRef] [PubMed]
- Rogers, P.J.; Hogenkamp, P.S.; De Graaf, C.; Higgs, S.; Lluch, A.; Ness, A.R.; Penfold, C.; Perry, R.; Putz, P.; Yeomans, M.R.; et al. Does low-energy sweetener consumption affect energy intake and body weight? A systematic review, including meta-analyses, of the evidence from human and animal studies. Int. J. Obes. 2015, 40, 381–394. [Google Scholar] [CrossRef] [PubMed]
- Toews, I.; Lohner, S.; De Gaudry, D.K.; Sommer, H.; Meerpohl, M.J.J. Association between intake of non-sugar sweeteners and health outcomes: Systematic review and meta-analyses of randomised and non-randomised controlled trials and observational studies. BMJ 2019, 364, k4718. [Google Scholar] [CrossRef] [PubMed]
- Mela, D.J.; McLaughlin, J.; Rogers, P.J. Perspective: Standards for Research and Reporting on Low-Energy (“Artificial”) Sweeteners. Adv. Nutr. 2020, 11, 484–491. [Google Scholar] [CrossRef]
- Tucker, R.M.; Tan, S.-Y. Do non-nutritive sweeteners influence acute glucose homeostasis in humans? A systematic review. Physiol. Behav. 2017, 182, 17–26. [Google Scholar] [CrossRef]
- Nichol, A.D.; Holle, M.J.; An, R. Glycemic impact of non-nutritive sweeteners: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Clin. Nutr. 2018, 72, 796–804. [Google Scholar] [CrossRef] [PubMed]
- Romo-Romo, A.; Aguilar-Salinas, C.A.; Brito-Córdova, G.X.; Díaz, R.A.G.; Valentín, D.V.; Almeda-Valdés, P. Effects of the Non-Nutritive Sweeteners on Glucose Metabolism and Appetite Regulating Hormones: Systematic Review of Observational Prospective Studies and Clinical Trials. PLoS ONE 2016, 11, e0161264. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, Y.; Nagasawa, M.; Yamada, S.; Hara, A.; Mogami, H.; Nikolaev, V.O.; Lohse, M.J.; Shigemura, N.; Ninomiya, Y.; Kojima, I. Sweet Taste Receptor Expressed in Pancreatic β-Cells Activates the Calcium and Cyclic AMP Signaling Systems and Stimulates Insulin Secretion. PLoS ONE 2009, 4, e5106. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.-J.; Kokrashvili, Z.; Theodorakis, M.J.; Carlson, O.D.; Kim, B.-J.; Zhou, J.; Kim, H.H.; Xu, X.; Chan, S.L.; Juhaszova, M.; et al. Gut-expressed gustducin and taste receptors regulate secretion of glucagon-like peptide-1. Proc. Natl. Acad. Sci. USA 2007, 104, 15069–15074. [Google Scholar] [CrossRef]
- Bryant, C.; McLaughlin, J. Low calorie sweeteners: Evidence remains lacking for effects on human gut function. Physiol. Behav. 2016, 164, 482–485. [Google Scholar] [CrossRef]
- Mace, O.J.; Affleck, J.; Patel, N.; Kellett, G.L. Sweet taste receptors in rat small intestine stimulate glucose absorption through apical GLUT2. J. Physiol. 2007, 582, 379–392. [Google Scholar] [CrossRef]
- Bryant, C.E.; Wasse, L.K.; Astbury, N.M.; Nandra, G.; McLaughlin, J.T. Non-nutritive sweeteners: No class effect on the glycaemic or appetite responses to ingested glucose. Eur. J. Clin. Nutr. 2014, 68, 629–631. [Google Scholar] [CrossRef]
- Temizkan, S.; Deyneli, O.; Yasar, M.; Arpa, M.; Gunes, M.; Yazici, D.; Sirikçi, Ö.; Haklar, G.; Imeryuz, N.; Yavuz, D.G. Sucralose enhances GLP-1 release and lowers blood glucose in the presence of carbohydrate in healthy subjects but not in patients with type 2 diabetes. Eur. J. Clin. Nutr. 2014, 69, 162–166. [Google Scholar] [CrossRef]
- Sylvetsky, A.C.; Brown, R.J.; Blau, J.E.; Walter, M.; Rother, K.I. Hormonal responses to non-nutritive sweeteners in water and diet soda. Nutr. Metab. 2016, 13, 71. [Google Scholar] [CrossRef]
- Gregersen, S.; Jeppesen, P.B.; Holst, J.J.; Hermansen, K. Antihyperglycemic effects of stevioside in type 2 diabetic subjects. Metabolism 2004, 53, 73–76. [Google Scholar] [CrossRef]
- Anton, S.D.; Martin, C.K.; Han, H.; Coulon, S.; Cefalu, W.T.; Geiselman, P.; Williamson, D.A. Effects of stevia, aspartame, and sucrose on food intake, satiety, and postprandial glucose and insulin levels. Appetite 2010, 55, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Maki, K.; Curry, L.; Reeves, M.; Toth, P.; McKenney, J.; Farmer, M.; Schwartz, S.; Lubin, B.; Boileau, A.; Dicklin, M.; et al. Chronic consumption of rebaudioside A, a steviol glycoside, in men and women with type 2 diabetes mellitus. Food Chem. Toxicol. 2008, 46, S47–S53. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.H.; Lee, J.H.; Kang, M.S.; Kim, T.H.; Jeong, S.J.; Kim, C.H.; Kim, S.S.; Kim, I.-J. Glycemic Effects of Rebaudioside A and Erythritol in People with Glucose Intolerance. Diabetes Metab. J. 2016, 40, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Stamataki, N.S.; Scott, C.; Elliott, R.; McKie, S.; Bosscher, D.; McLaughlin, J.T. Stevia Beverage Consumption prior to Lunch Reduces Appetite and Total Energy Intake without Affecting Glycemia or Attentional Bias to Food Cues: A Double-Blind Randomized Controlled Trial in Healthy Adults. J. Nutr. 2020, 150, 1126–1134. [Google Scholar] [CrossRef]
- Higgins, K.A.; Mattes, R.D. A randomized controlled trial contrasting the effects of 4 low-calorie sweeteners and sucrose on body weight in adults with overweight or obesity. Am. J. Clin. Nutr. 2019, 109, 1288–1301. [Google Scholar] [CrossRef]
- Maki, K.; Curry, L.; Carakostas, M.; Tarka, S.; Reeves, M.; Farmer, M.; McKenney, J.; Toth, P.; Schwartz, S.; Lubin, B.; et al. The hemodynamic effects of rebaudioside A in healthy adults with normal and low-normal blood pressure. Food Chem. Toxicol. 2008, 46, S40–S46. [Google Scholar] [CrossRef]
- Hsieh, M.-H.; Chan, P.; Sue, Y.-M.; Liu, J.-C.; Liang, T.H.; Huang, T.-Y.; Tomlinson, B.; Chow, M.S.S.; Kao, P.-F.; Chen, Y.-J. Efficacy and tolerability of oral stevioside in patients with mild essential hypertension: A two-year, randomized, placebo-controlled study. Clin. Ther. 2003, 25, 2797–2808. [Google Scholar] [CrossRef]
- Stamataki, N.S.; Nikolidaki, E.K.; Yanni, A.E.; Stoupaki, M.; Konstantopoulos, P.; Tsigkas, A.-P.; Perrea, D.; Tentolouris, N.; Karathanos, V.T. Evaluation of a high nutritional quality snack based on oat flakes and inulin: Effects on postprandial glucose, insulin and ghrelin responses of healthy subjects. Food Funct. 2016, 7, 3295–3303. [Google Scholar] [CrossRef]
- Bradley, J.; Simpson, E.; Poliakov, I.; Matthews, J.N.S.; Olivier, P.; Adamson, A.J.; Foster, E. Comparison of INTAKE24 (an Online 24-h Dietary Recall Tool) with Interviewer-Led 24-h Recall in 11–24 Year-Old. Nutr. 2016, 8, 358. [Google Scholar] [CrossRef]
- Stunkard, A.J.; Messick, S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J. Psychosom. Res. 1985, 29, 71–83. [Google Scholar] [CrossRef]
- Dalton, M.; Finlayson, G.; Hill, A.; Blundell, J. Preliminary validation and principal components analysis of the Control of Eating Questionnaire (CoEQ) for the experience of food craving. Eur. J. Clin. Nutr. 2015, 69, 1313–1317. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.H.; Peters, V.; Martin, N.M.; Sleeth, M.L.A.; Ghatei, M.; Frost, G.S.; Bloom, S.R. Effects of oral ingestion of sucralose on gut hormone response and appetite in healthy normal-weight subjects. Eur. J. Clin. Nutr. 2011, 65, 508–513. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.W.; Brown, M.M.B.; Onken, K.L.; Beitz, D.C. Short-term consumption of sucralose, a nonnutritive sweetener, is similar to water with regard to select markers of hunger signaling and short-term glucose homeostasis in women. Nutr. Res. 2011, 31, 882–888. [Google Scholar] [CrossRef] [PubMed]
- Dalenberg, J.R.; Patel, B.P.; Denis, R.; Veldhuizen, M.G.; Nakamura, Y.; Vinke, P.C.; Luquet, S.; Small, D.M. Short-Term Consumption of Sucralose with, but Not without, Carbohydrate Impairs Neural and Metabolic Sensitivity to Sugar in Humans. Cell Metab. 2020, 31, 493–502.e7. [Google Scholar] [CrossRef] [PubMed]
- Steinert, R.E.; Frey, F.; Töpfer, A.; Drewe, J.; Beglinger, C. Effects of carbohydrate sugars and artificial sweeteners on appetite and the secretion of gastrointestinal satiety peptides. Br. J. Nutr. 2011, 105, 1320–1328. [Google Scholar] [CrossRef]
- Ma, J.; Bellon, M.; Wishart, J.M.; Young, R.L.; Blackshaw, L.A.; Jones, K.L.; Horowitz, M.; Rayner, C.K. Effect of the artificial sweetener, sucralose, on gastric emptying and incretin hormone release in healthy subjects. Am. J. Physiol. Liver Physiol. 2009, 296, G735–G739. [Google Scholar] [CrossRef]
- Magnuson, B.A.; Carakostas, M.C.; Moore, N.H.; Poulos, S.; Renwick, A.G. Biological fate of low-calorie sweeteners. Nutr. Rev. 2016, 74, 670–689. [Google Scholar] [CrossRef]
- Philippaert, K.; Pironet, A.; Mesuere, M.; Sones, W.; Vermeiren, L.; Kerselaers, S.; Pinto, S.; Segal, A.; Antoine, N.; Gysemans, C.; et al. Steviol glycosides enhance pancreatic beta-cell function and taste sensation by potentiation of TRPM5 channel activity. Nat. Commun. 2017, 8, 14733. [Google Scholar] [CrossRef]
- Tey, S.L.; Salleh, N.B.; Henry, C.J.; Forde, C.G. Effects of aspartame-, monk fruit-, stevia- and sucrose-sweetened beverages on postprandial glucose, insulin and energy intake. Int. J. Obes. 2016, 41, 450–457. [Google Scholar] [CrossRef]
- Van Avesaat, M.; Troost, F.J.; Ripken, D.; Peters, J.; Hendriks, H.F.; Masclee, A.A. Intraduodenal infusion of a combination of tastants decreases food intake in humans. Am. J. Clin. Nutr. 2015, 102, 729–735. [Google Scholar] [CrossRef]
- Anker, C.C.B.; Rafiq, S.; Jeppesen, P.B.; Anker, B. Effect of Steviol Glycosides on Human Health with Emphasis on Type 2 Diabetic Biomarkers: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2019, 11, 1965. [Google Scholar] [CrossRef] [PubMed]
- Barriocanal, L.A.; Palacios, M.; Benitez, G.; Benitez, S.; Jimenez, J.T.; Jimenez, N.; Rojas, V. Apparent lack of pharmacological effect of steviol glycosides used as sweeteners in humans. A pilot study of repeated exposures in some normotensive and hypotensive individuals and in Type 1 and Type 2 diabetics. Regul. Toxicol. Pharm. 2008, 51, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Higgins, K.A.; Considine, R.V.; Mattes, R.D. Aspartame Consumption for 12 Weeks Does Not Affect Glycemia, Appetite, or Body Weight of Healthy, Lean Adults in a Randomized Controlled Trial. J. Nutr. 2018, 148, 650–657. [Google Scholar] [CrossRef] [PubMed]
- Grotz, V.L.; Pi-Sunyer, X.; Porte, D.; Roberts, A.; Trout, J.R. A 12-week randomized clinical trial investigating the potential for sucralose to affect glucose homeostasis. Regul. Toxicol. Pharm. 2017, 88, 22–33. [Google Scholar] [CrossRef]
- Thomson, P.; Santibañez, R.; Aguirre, C.; Galgani, J.E.; Garrido, D. Short-term impact of sucralose consumption on the metabolic response and gut microbiome of healthy adults. Br. J. Nutr. 2019, 122, 856–862. [Google Scholar] [CrossRef]
- Lertrit, A.; Srimachai, S.; Saetung, S.; Chanprasertyothin, S.; Chailurkit, L.-O.; Areevut, C.; Katekao, P.; Ongphiphadhanakul, B.; Sriprapadang, C. Effects of sucralose on insulin and glucagon-like peptide-1 secretion in healthy subjects: A randomized, double-blind, placebo-controlled trial. Nutrients 2018, 56, 125–130. [Google Scholar] [CrossRef]
- Romo-Romo, A.; Aguilar-Salinas, C.A.; Brito-Córdova, G.X.; Gómez-Díaz, R.A.; Almeda-Valdés, P. Sucralose decreases insulin sensitivity in healthy subjects: A randomized controlled trial. Am. J. Clin. Nutr. 2018, 108, 485–491. [Google Scholar] [CrossRef]
- Little, T.J.; McKie, S.; Jones, R.B.; D’Amato, M.; Smith, C.; Kiss, O.; Thompson, D.G.; McLaughlin, J.T. Mapping glucose-mediated gut-to-brain signalling pathways in humans. NeuroImage 2014, 96, 1–11. [Google Scholar] [CrossRef]
- Smeets, P.A.M.; De Graaf, C.; Stafleu, A.; Van Osch, M.J.P.; Van Der Grond, J. Functional magnetic resonance imaging of human hypothalamic responses to sweet taste and calories. Am. J. Clin. Nutr. 2005, 82, 1011–1016. [Google Scholar] [CrossRef]
- Van Opstal, A.M.; Kaal, I.; Berg-Huysmans, A.V.D.; Hoeksma, M.; Blonk, C.; Pijl, H.; Rombouts, S.A.; Van Der Grond, J. Dietary sugars and non-caloric sweeteners elicit different homeostatic and hedonic responses in the brain. Nutrients 2019, 60, 80–86. [Google Scholar] [CrossRef]
- Chambers, E.S.; Bridge, M.W.; Jones, D.A. Carbohydrate sensing in the human mouth: Effects on exercise performance and brain activity. J. Physiol. 2009, 587, 1779–1794. [Google Scholar] [CrossRef] [PubMed]
- Frank, G.K.; Oberndorfer, T.A.; Simmons, A.N.; Paulus, M.P.; Fudge, J.L.; Yang, T.T.; Kaye, W.H. Sucrose activates human taste pathways differently from artificial sweetener. NeuroImage 2008, 39, 1559–1569. [Google Scholar] [CrossRef] [PubMed]
- Green, E.; Murphy, C. Altered processing of sweet taste in the brain of diet soda drinkers. Physiol. Behav. 2012, 107, 560–567. [Google Scholar] [CrossRef]
- Hansen, T.T.; Hjorth, M.F.; Sandby, K.; Andersen, S.V.; Astrup, A.; Ritz, C.; Bulló, M.; Camacho-Barcia, L.; García-Gavilán, J.; Salas-Salvadó, J.; et al. Predictors of successful weight loss with relative maintenance of fat-free mass in individuals with overweight and obesity on an 8-week low-energy diet. Br. J. Nutr. 2019, 122, 468–479. [Google Scholar] [CrossRef] [PubMed]
- Dykes, J.; Brunner, E.J.; Martikainen, P.; Wardle, J. Socioeconomic gradient in body size and obesity among women: The role of dietary restraint, disinhibition and hunger in the Whitehall II study. Int. J. Obes. 2003, 28, 262–268. [Google Scholar] [CrossRef]
- Maloney, N.G.; Christiansen, P.; Harrold, J.A.; Halford, J.C.; Hardman, C.A. Do low-calorie sweetened beverages help to control food cravings? Two experimental studies. Physiol. Behav. 2019, 208, 112500. [Google Scholar] [CrossRef]
- Fontaine, K.R.; Williams, M.S.; Hoenemeyer, T.W.; Kaptchuk, T.J.; Dutton, G.R. Placebo effects in obesity research. Obesity 2016, 24, 769–771. [Google Scholar] [CrossRef]
- Johns, D.J.; Hartmann-Boyce, J.; Jebb, S.A.; Aveyard, P. Weight change among people randomized to minimal intervention control groups in weight loss trials. Obesity 2016, 24, 772–780. [Google Scholar] [CrossRef]
| Stevia Group (n = 14) | Control Group (n = 14) | p Value | |
|---|---|---|---|
| Age, y | 25 (6) | 25 (4) | 0.795 |
| Weight, kg | 59.50 (9.00) | 57.83 (7.98) | 0.428 |
| Height, m | 1.65 (0.09) | 1.67 (0.08) | 0.934 |
| BMI, kg/m2 | 21.71 (1.81) | 20.73 (1.46) | 0.122 |
| Waist circumference, cm | 71.64 (6.53) | 70.57 (5.81) | 0.651 |
| Female (count) | 11 | 11 | |
| BMR (kcal) 1 | 1379 (197) | 1368 (181) | 0.880 |
| Daily energy needs (kcal) 2 | 1930 (276) | 1915 (253) | 0.882 |
| DEBQ scores | |||
| Restraint eating | 2.06 (0.43) | 1.90 (0.59) | 0.484 |
| Emotional eating | 2.26 (0.63) | 2.28 (0.45) | 0.947 |
| External eating | 3.09 (0.56) | 3.11 (0.43) | 0.930 |
| Stevia Group (n = 14) | Control Group (n = 14) | p Values | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Week 0 | Week 6 | Week 12 | Week 0 | Week 6 | Week 12 | Session | Group | Session × Group | |
| Body weight, kg | 59.50 (2.40) | 59.31 (2.40) | 59.27 (2.49) | 57.83 (2.13) | 58.61 (2.32) | 58.72 (2.23) | 0.289 | 0.769 | 0.040 |
| Δ Body weight, kg | - | −0.19 (0.30) | −0.22 (0.32) | - | 0.79 (0.36) | 0.89 (0.39) | 0.289 | 0.026 | 0.040 |
| BMI, kg/m2 | 21.71 (0.48) | 21.64 (0.48) | 21.62 (0.49) | 20.73 (0.39) | 20.99 (0.42) | 21.03 (0.40) | 0.389 | 0.247 | 0.053 |
| Δ BMI, kg/m2 | - | −0.07 (0.11) | −0.09 (0.12) | - | 0.26 (0.13) | 0.31 (0.14) | 0.388 | 0.035 | 0.054 |
| Waist circumference, cm | 71.64 (1.75) | 71.93 (1.61) | 71.11 (1.65) | 70.57 (1.55) | 71.18 (1.66) | 71.00 (1.66) | 0.135 | 0.783 | 0.199 |
| Systolic blood pressure, mmHg | 119.14 (2.46) | 117.71 (3.60) | 118.07 (2.78) | 114.00 (1.95) | 114.21 (2.81) | 112.71 (2.58) | 0.732 | 0.191 | 0.792 |
| Diastolic blood pressure, mmHg | 67.57 (1.76) | 64.57 (1.51) | 65.93 (1.17) | 70.11 (1.24) | 68.79 (1.51) | 69.29 (1.93) | 0.159 | 0.069 | 0.750 |
| Pulses, beats per min | 72.39 (2.52) | 69.57 (2.46) | 74.75 (2.14) | 70.07 (1.49) | 74.14 (3.66) | 73.68 (2.33) | 0.264 | 0.889 | 0.165 |
| Stevia Group (n = 14) | Control Group (n = 14) | p Values | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Week 0 | Week 6 | Week 12 | Week 0 | Week 6 | Week 12 | Session | Group | Session × Group | |
| Energy intake, kcal × d−1 | 1659 (102.9) | 1437 (106.2) | 1366 (115.6) | 1674 (137.7) | 1727 (154.4) | 1678 (167.2) | 0.185 | 0.224 | 0.114 |
| Δ Energy intake, kcal × d−1 | −221.2 (129.3) | −292.8 (78.81) | - | 52.52 (100.3) | 4.36 (124.8) | 0.185 | 0.045 | 0.114 | |
| Carbohydrates, g | 193 (10.9) | 175 (16.6) | 170 (12.3) | 205 (15.2) | 206 (16.2) | 208 (23.3) | 0.643 | 0.164 | 0.533 |
| Carbohydrates, % | 47.9 (2.52) | 48.7 (2.61) | 51.6 (2.81) | 50.3 (2.48) | 48.7 (1.86) | 49.4 (2.47) | 0.586 | 0.975 | 0.440 |
| Fats, g | 67.6 (7.12) | 53.8 (5.00) | 52.3 (6.66) | 66.4 (7.55) | 68.7 (8.77) | 66.00 (10.0) | 0.241 | 0.338 | 0.174 |
| Fats, % | 35.9 (1.91) | 33.4 (1.83) | 32.8 (1.96) | 34.8 (1.82) | 34.8 (1.80) | 34.1 (2.05) | 0.500 | 0.787 | 0.691 |
| Proteins, g | 71.3 (8.99) | 69.3 (7.11) | 61.3 (7.00) | 68.1 (6.82) | 71.8 (6.82) | 73.8 (4.92) | 0.739 | 0.644 | 0.224 |
| Proteins, % | 16.8 (1.53) | 19.9 (2.39) | 17.9 (1.40) | 16.5 (1.14) | 16.8 (1.00) | 18.9 (1.61) | 0.282 | 0.635 | 0.253 |
| Sugars, g/1000 kcal | 49.3 (3.61) | 49.8 (3.59) | 49.2 (3.71) | 49.7 (6.24) | 43.5 (5.16) | 38.1 (5.03) | 0.395 | 0.230 | 0.435 |
| Fibres, g/1000 kcal | 8.29 (0.79) | 8.49 (1.11) | 7.79 (0.64) | 7.54 (1.15) | 8.53 (1.20) | 8.10 (0.87) | 0.487 | 0.911 | 0.648 |
| Stevia Group (n = 14) | Control Group (n = 14) | p Values | |||||
|---|---|---|---|---|---|---|---|
| Week 0 | Week 12 | Week 0 | Week 12 | Session | Group | Session × Group | |
| TFEQ subscales | |||||||
| Cognitive restraint | 5.93 (0.84) | 5.86 (0.64) | 4.79 (1.23) | 6.36 (1.40) | 0.226 | 0.819 | 0.186 |
| Disinhibition | 4.36 (0.74) | 4.79 (0.70) | 5.21 (0.59) | 5.57 (0.54) | 0.192 | 0.354 | 0.904 |
| Hunger | 4.86 (0.82) | 4.86 (0.76) | 7.36 (0.74) | 6.79 (0.82) | 0.504 | 0.041 | 0.504 |
| CoEQ subscales | |||||||
| Cravings for savoury | 32.3 (3.67) | 36.2 (4.50) | 52.6 (5.33) | 49.9 (4.27) | 0.845 | 0.006 | 0.243 |
| Cravings for sweet | 39.3 (4.96) | 40.4 (4.72) | 46.9 (5.16) | 36.1 (5.19) | 0.087 | 0.807 | 0.037 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stamataki, N.S.; Crooks, B.; Ahmed, A.; McLaughlin, J.T. Effects of the Daily Consumption of Stevia on Glucose Homeostasis, Body Weight, and Energy Intake: A Randomised Open-Label 12-Week Trial in Healthy Adults. Nutrients 2020, 12, 3049. https://doi.org/10.3390/nu12103049
Stamataki NS, Crooks B, Ahmed A, McLaughlin JT. Effects of the Daily Consumption of Stevia on Glucose Homeostasis, Body Weight, and Energy Intake: A Randomised Open-Label 12-Week Trial in Healthy Adults. Nutrients. 2020; 12(10):3049. https://doi.org/10.3390/nu12103049
Chicago/Turabian StyleStamataki, Nikoleta S., Benjamin Crooks, Abubaker Ahmed, and John T. McLaughlin. 2020. "Effects of the Daily Consumption of Stevia on Glucose Homeostasis, Body Weight, and Energy Intake: A Randomised Open-Label 12-Week Trial in Healthy Adults" Nutrients 12, no. 10: 3049. https://doi.org/10.3390/nu12103049
APA StyleStamataki, N. S., Crooks, B., Ahmed, A., & McLaughlin, J. T. (2020). Effects of the Daily Consumption of Stevia on Glucose Homeostasis, Body Weight, and Energy Intake: A Randomised Open-Label 12-Week Trial in Healthy Adults. Nutrients, 12(10), 3049. https://doi.org/10.3390/nu12103049






