Psychiatric Manifestations of Coeliac Disease, a Systematic Review and Meta-Analysis
Abstract
1. Introduction
Interaction between CD and Psychiatric Disorders
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Inclusion and Exclusion Criteria
- Articles needed to provide original data.
- Articles needed to concern the relationship of CD and psychiatric disorders.
- CD should have been confirmed, either serologically with anti-endomysial (EMA), or a duodenum biopsy.
- Formal diagnosis of psychiatric disorders should have been made.
2.3. Statistical Analyses
2.4. Compliance with Ethical Guidelines
3. Results
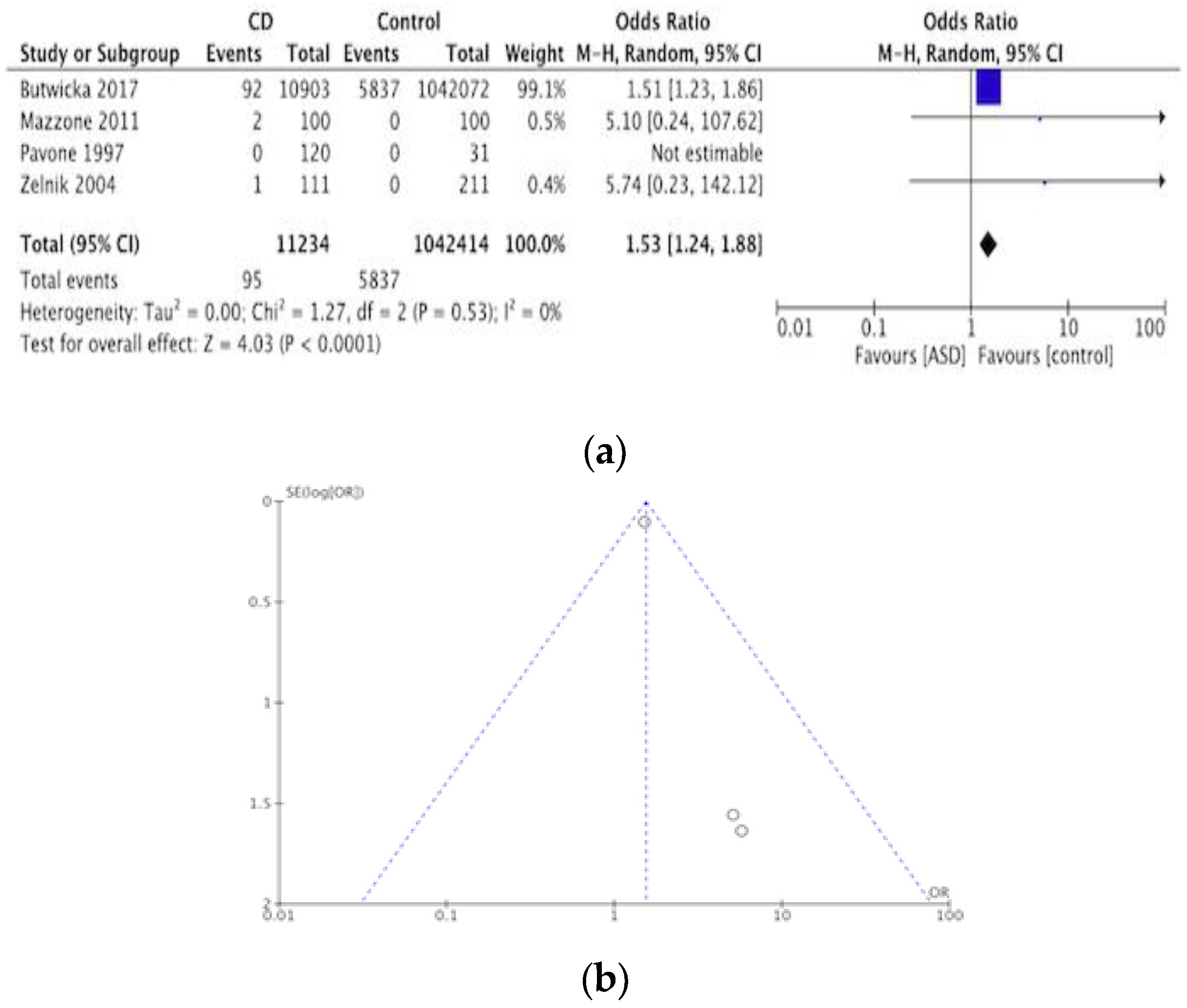
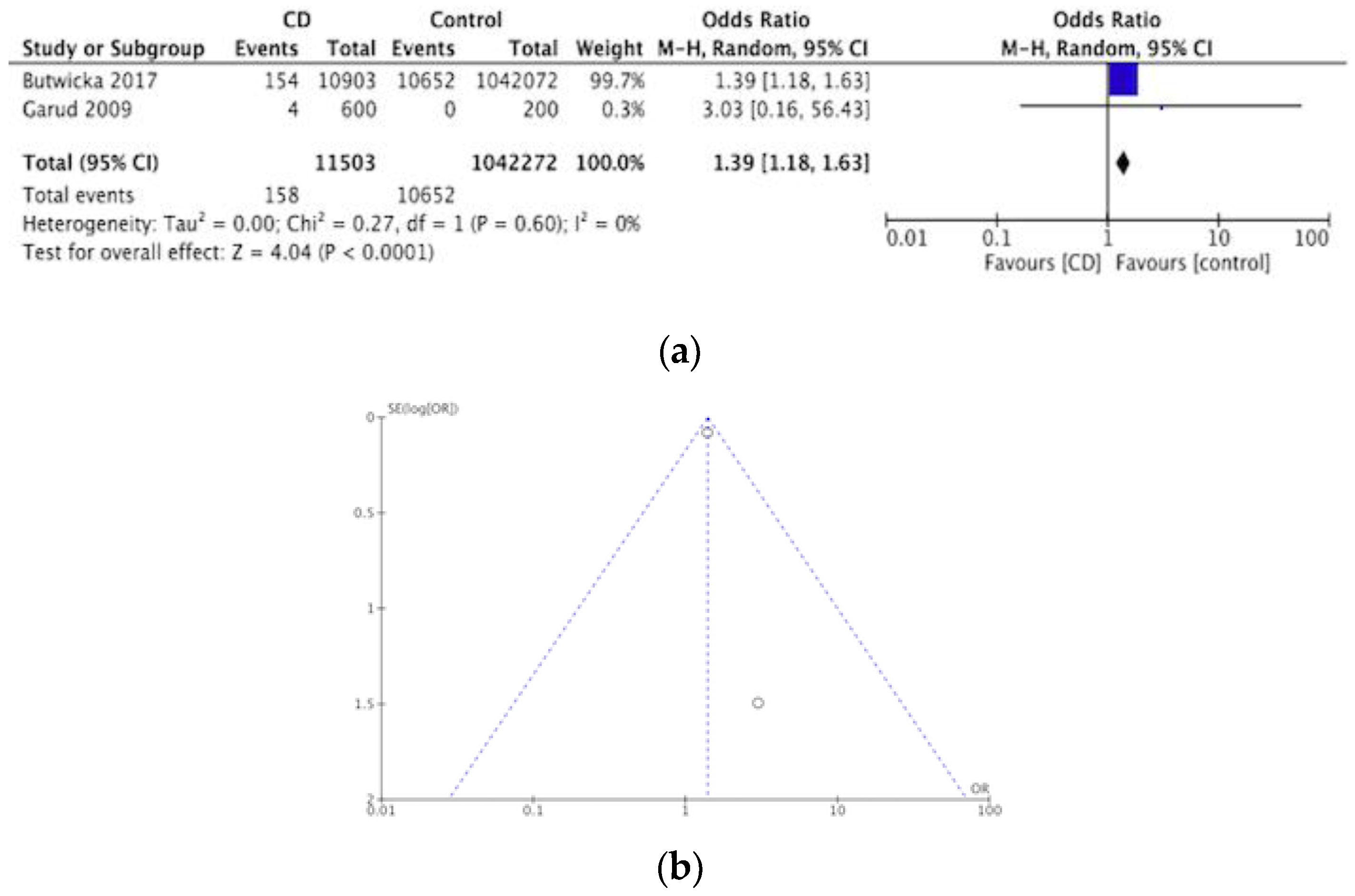
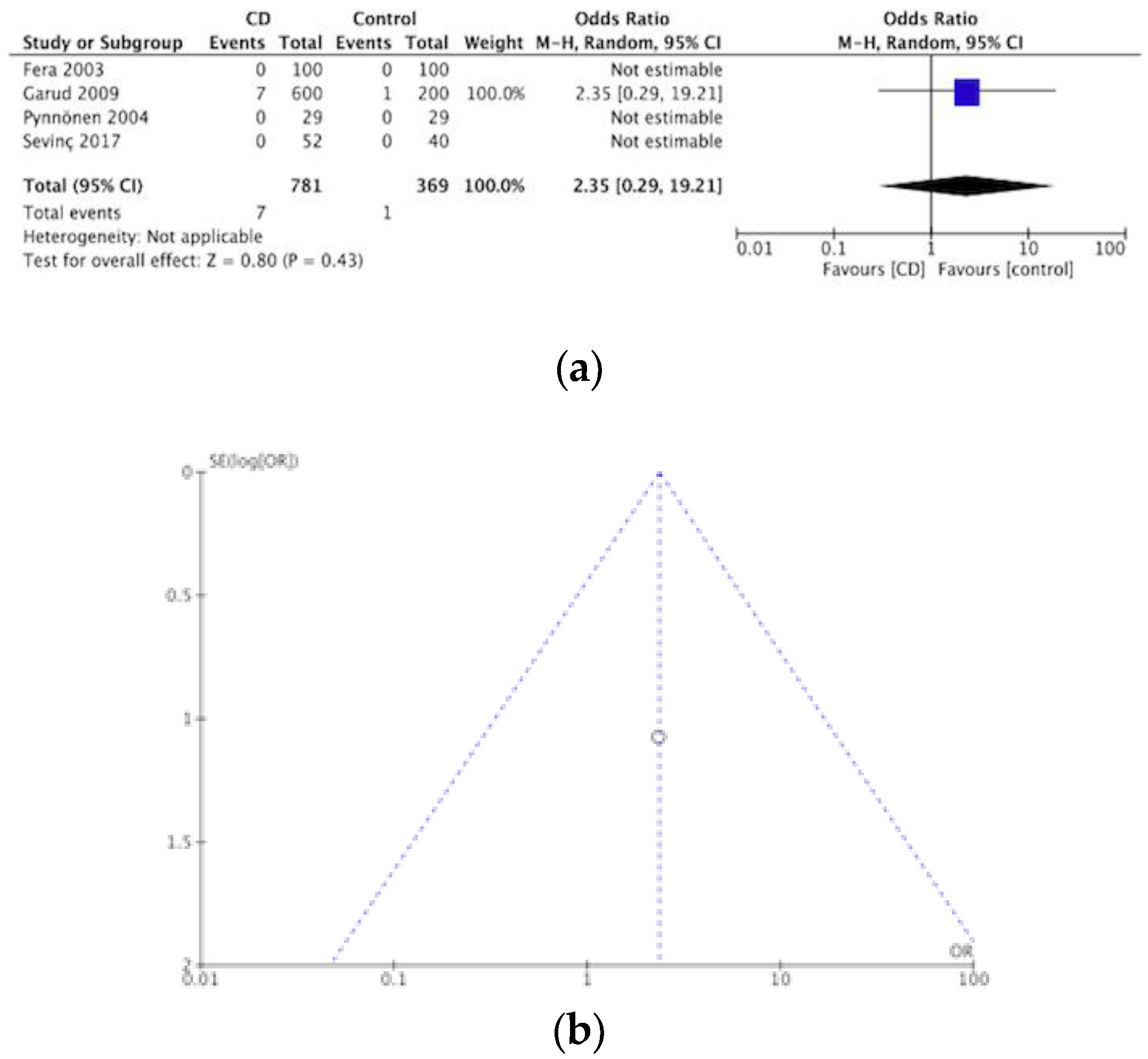
3.1. ASD and ADHD
3.1.1. GFD in ASD and ADHD
3.1.2. Limitations of Studies in ADHD and ASD
3.2. Mood Disorders
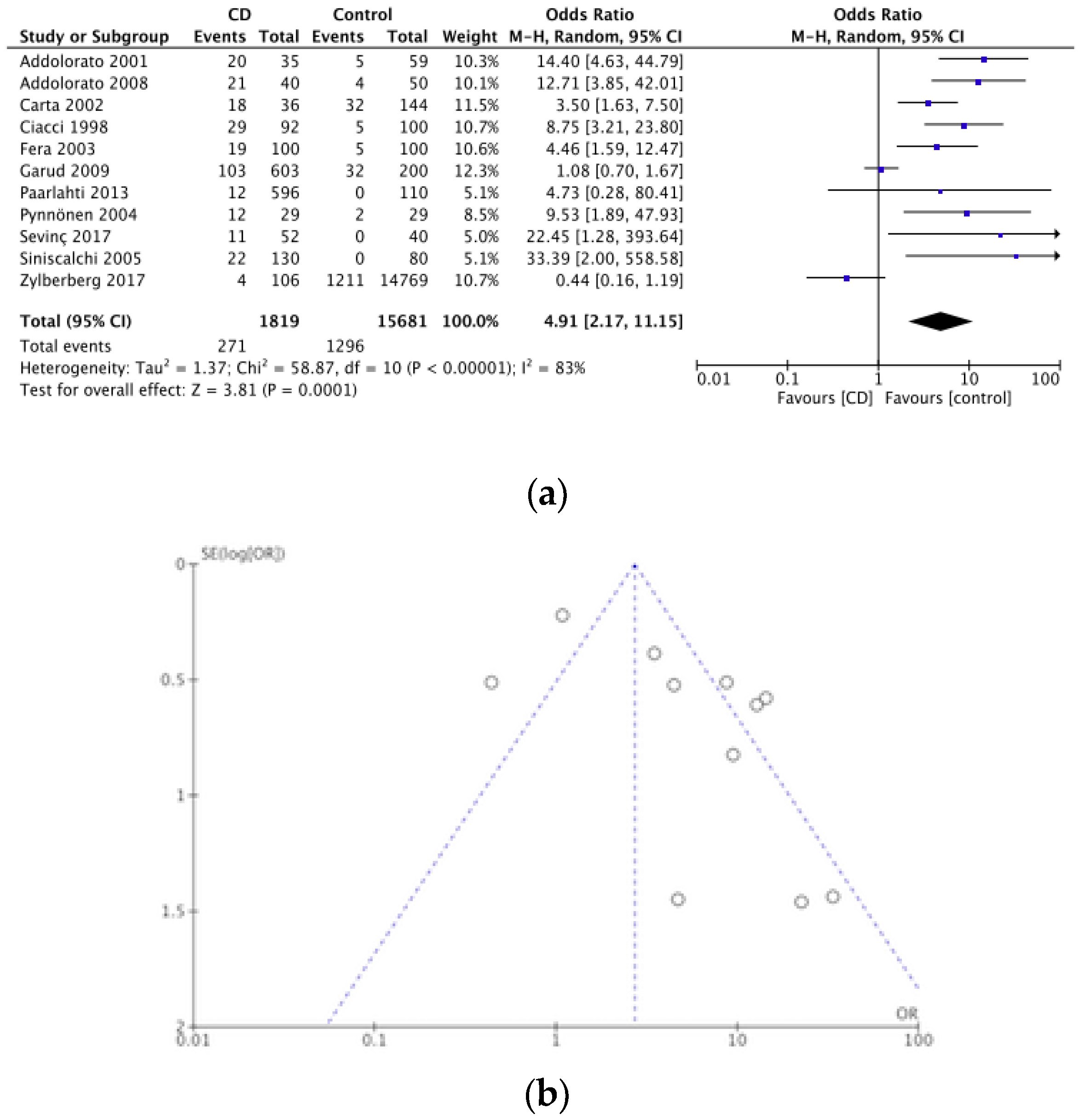
3.2.1. Depression
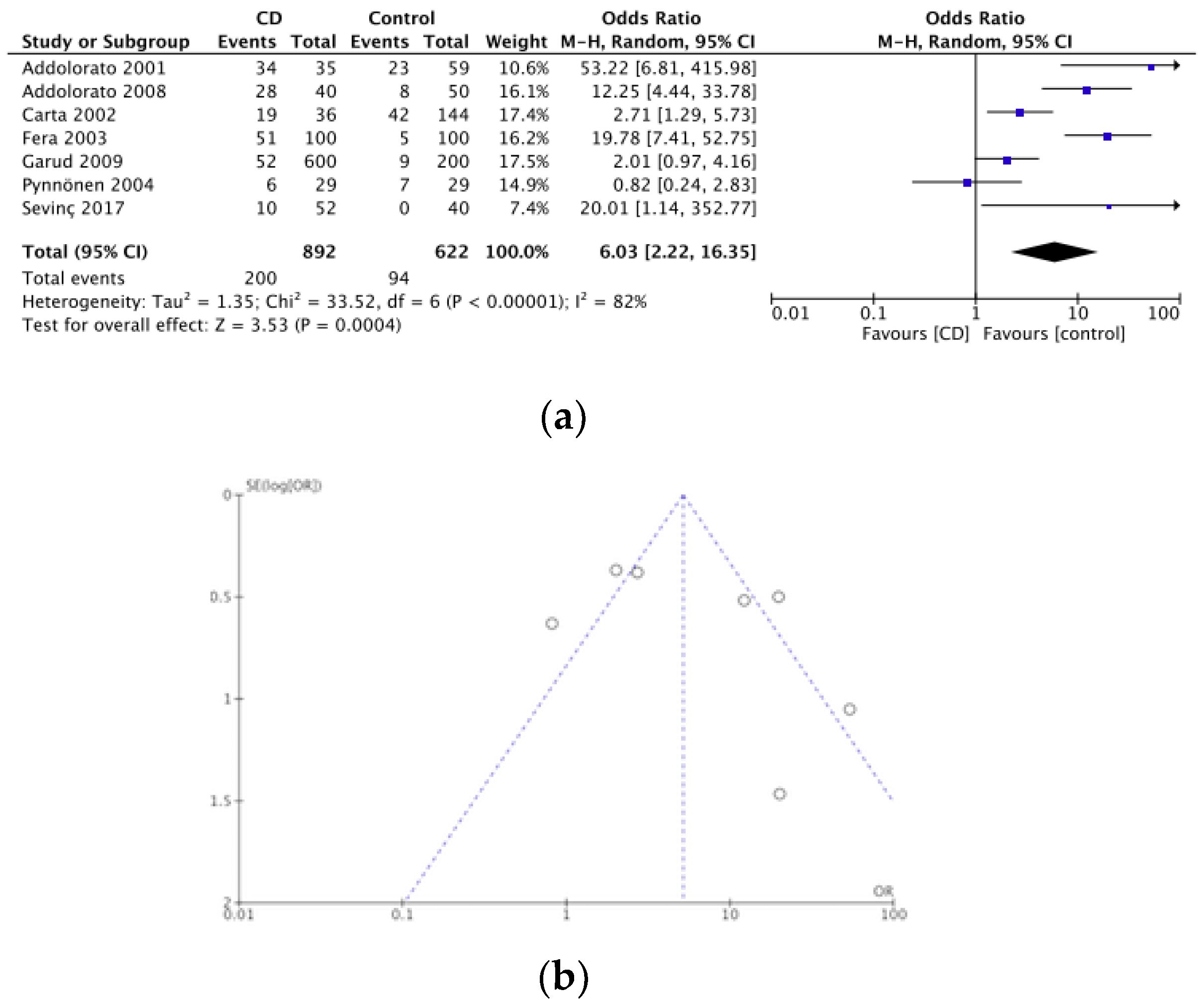
3.2.2. Anxiety
3.2.3. Bipolar Disorder
3.2.4. GFD in Mood Disorders
3.2.5. Limitations in Studies of Mood Disorders
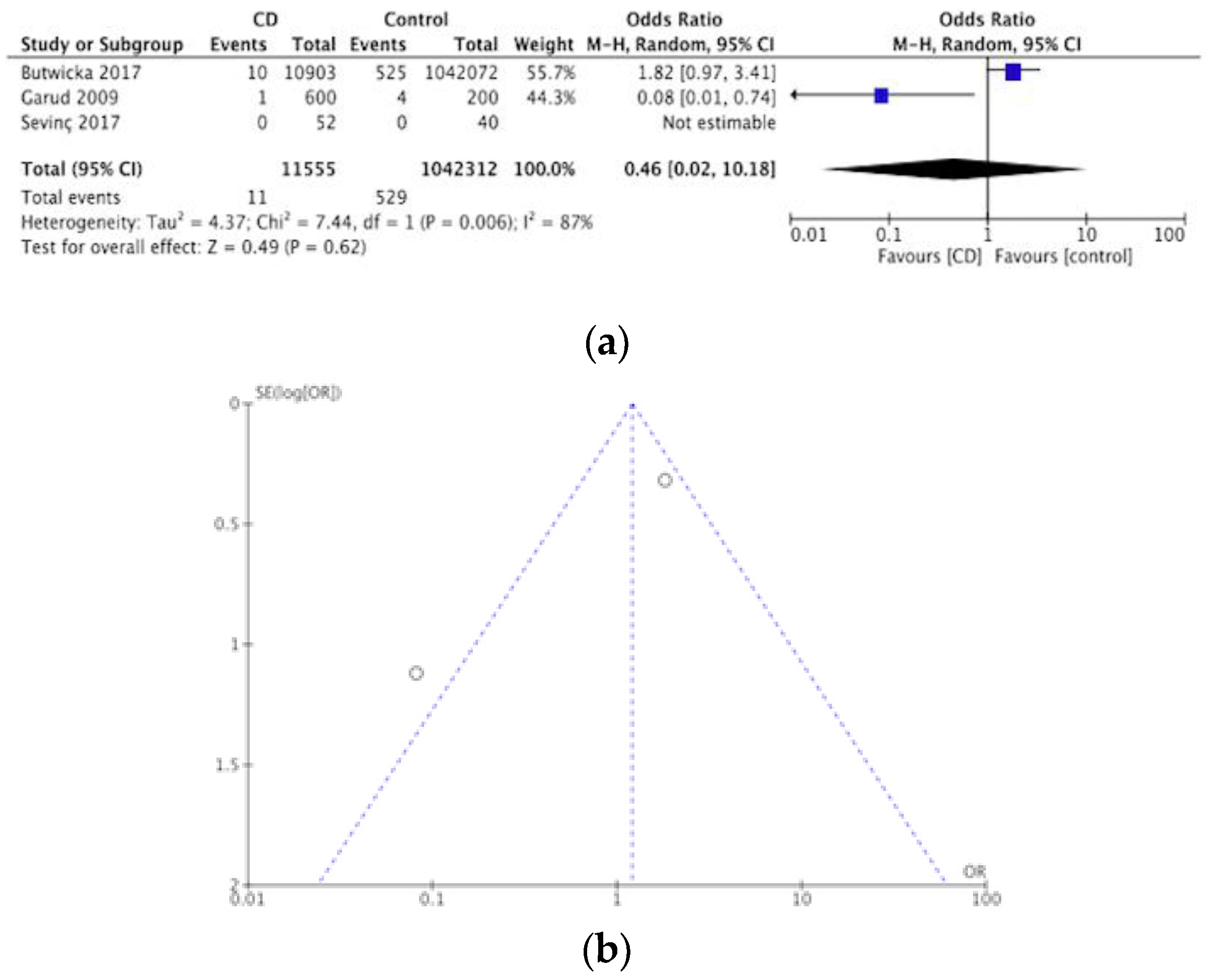
3.3. Schizophrenia and Other Psychotic Disorders
3.3.1. GFD in Schizophrenia and Other Psychotic Disorders
3.3.2. Limitations in Studies on Schizophrenia and Other Psychotic Disorders
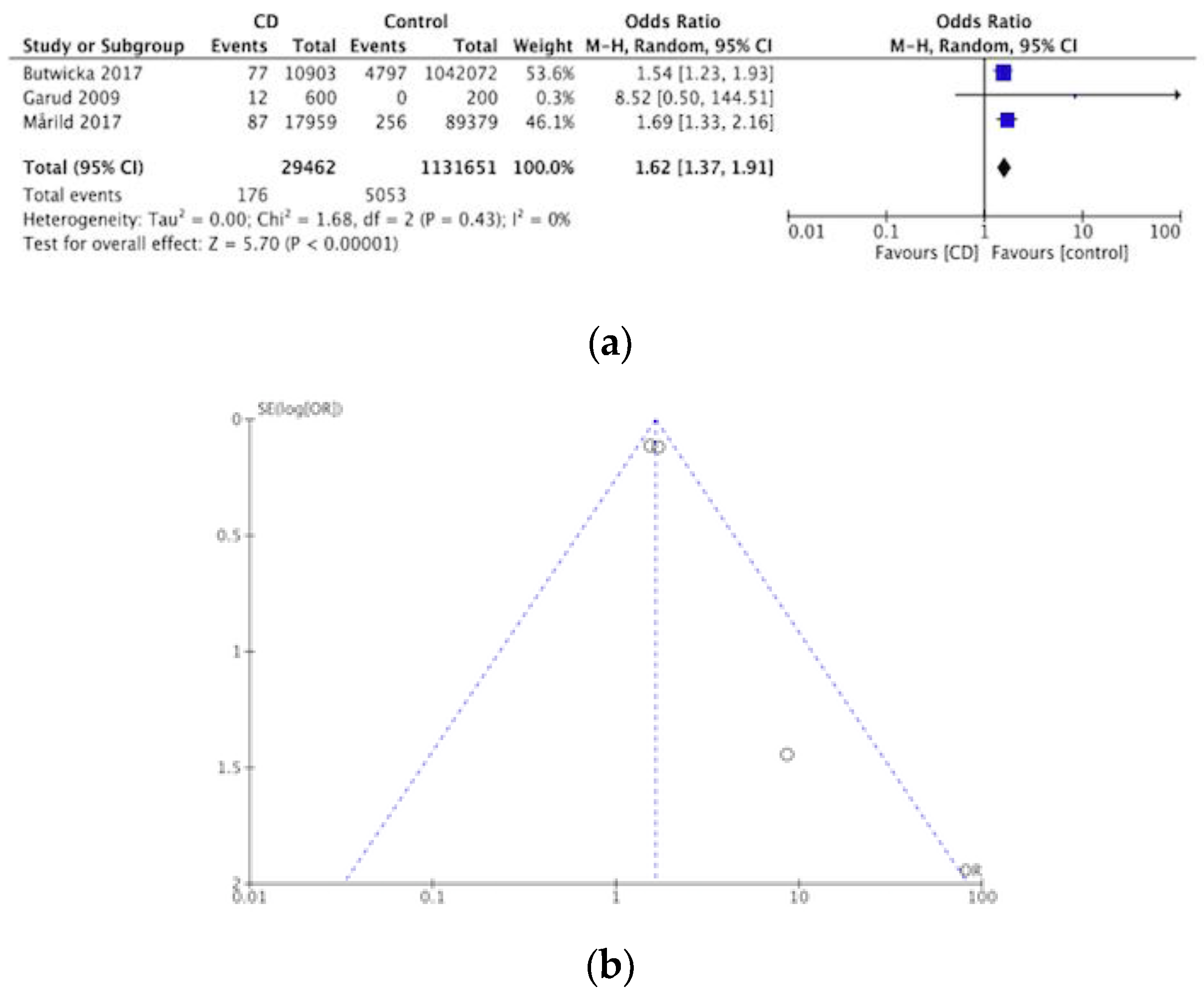
3.4. Eating Disorders
3.4.1. GFD in Eating Disorders
3.4.2. Limitations in Studies on Eating Disorders
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cossu, G.; Carta, M.G.; Contu, F.; Mela, Q.; Demelia, L.; Elli, L.; Dell’Osso, B. Coeliac disease and psychiatric comorbidity: Epidemiology, pathophysiological mechanisms, quality-of-life, and gluten-free diet effects. Int. Rev. Psychiatry 2017, 29, 489–503. [Google Scholar] [CrossRef]
- Zysk, W.; Głąbska, D.; Guzek, D. Social and Emotional Fears and Worries Influencing the Quality of Life of Female Celiac Disease Patients Following a Gluten-Free Diet. Nutrients 2018, 10, 1414. [Google Scholar] [CrossRef]
- Wolf, R.L.; Lebwohl, B.; Lee, A.R.; Zybert, P.; Reilly, N.R.; Cadenhead, J.; Amengual, C.; Green, P.H. Hypervigilance to a gluten-free diet and decreased quality of life in teenagers and adults with celiac disease. Dig. Dis. Sci. 2018, 63, 1438–1448. [Google Scholar] [CrossRef] [PubMed]
- Leffler, D.A.; Acaster, S.; Gallop, K.; Dennis, M.; Kelly, C.P.; Adelman, D.C. A novel patient-derived conceptual model of the impact of celiac disease in adults: Implications for patient-reported outcome and health-related quality-of-life instrument development. Value Health 2017, 20, 637–643. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Arora, A.; Strand, T.A.; Leffler, D.A.; Catassi, C.; Green, P.H.; Kelly, C.P.; Ahuja, V.; Makharia, G.K. Global prevalence of celiac disease: Systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 2018, 16, 823–836. [Google Scholar] [CrossRef] [PubMed]
- Roncoroni, L.; Bascuñán, K.; Doneda, L.; Scricciolo, A.; Lombardo, V.; Branchi, F.; Ferretti, F.; Dell’Osso, B.; Montanari, V.; Bardella, M.; et al. A low FODMAP gluten-free diet improves functional gastrointestinal disorders and overall mental health of celiac disease patients: A randomized controlled trial. Nutrients 2018, 10, 1023. [Google Scholar] [CrossRef] [PubMed]
- Mirijello, A.; d’Angelo, C.; De Cosmo, S.; Gasbarrini, A.; Addolorato, G. Management of celiac disease in daily clinical practice: Do not forget depression! Eur. J. Intern. Med. 2019, 62, e17. [Google Scholar] [CrossRef]
- Nardecchia, S.; Auricchio, R.; Discepolo, V.; Troncone, R. Extraintestinal manifestations of coeliac disease in children: Clinical features and mechanisms. Front. Pediatr. 2019, 7, 56. [Google Scholar] [CrossRef]
- Grode, L.; Bech, B.H.; Plana-Ripoll, O.; Bliddal, M.; Agerholm, I.E.; Humaidan, P.; Ramlau-Hansen, C.H. Reproductive life in women with celiac disease; a nationwide, population-based matched cohort study. Hum. Reprod. 2018, 33, 1538–1547. [Google Scholar] [CrossRef]
- Zingone, F.; Swift, G.L.; Card, T.R.; Sanders, D.S.; Ludvigsson, J.F.; Bai, J.C. Psychological morbidity of celiac disease: A review of the literature. United Eur. Gastroenterol. J. 2015, 3, 136–145. [Google Scholar] [CrossRef]
- Porcelli, B.; Verdino, V.; Ferretti, F.; Bizzaro, N.; Terzuoli, L.; Cinci, F.; Bossini, L.; Fagiolini, A. A study on the association of mood disorders and gluten-related diseases. Psychiatry Res. 2018, 260, 366–370. [Google Scholar] [CrossRef] [PubMed]
- Parisi, P. The relationship between mucosal damage in celiac disease and the risk of neurological and psychiatric conditions is much more complex than previously thought. Eur. J. Neurol. 2018, 25, 797–798. [Google Scholar] [CrossRef] [PubMed]
- Bojović, K.; Stanković, B.; Kotur, N.; Krstić-Milošević, D.; Gašić, V.; Pavlović, S.; Zukić, B.; Ignjatović, Đ. Genetic predictors of celiac disease, lactose intolerance, and vitamin D function and presence of peptide morphins in urine of children with neurodevelopmental disorders. Nutr. Neurosci. 2019, 22, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Babio, N.; Alcázar, M.; Castillejo, G.; Recasens, M.; Martínez-Cerezo, F.; Gutiérrez-Pensado, V.; Vaqué, C.; Vila-Martí, A.; Torres-Moreno, M.; Sánchez, E.; et al. Risk of eating disorders in patients with celiac disease. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Brietzke, E.; Cerqueira, R.O.; Mansur, R.B.; McIntyre, R.S. Gluten related illnesses and severe mental disorders: A comprehensive review. Neurosci. Biobehav. Rev. 2018, 84, 368–375. [Google Scholar] [CrossRef]
- Smith, D.F.; Gerdes, L.U. Meta-analysis on anxiety and depression in adult celiac disease. Acta Psychiatr. Scand. 2012, 125, 189–193. [Google Scholar] [CrossRef]
- Miller, K.; Driscoll, D.; Smith, L.M.; Ramaswamy, S. The role of inflammation in late-life post-traumatic stress disorder. Mil. Med. 2017, 182, e1815–e1818. [Google Scholar] [CrossRef]
- Alabaf, S.; Gillberg, C.; Lundström, S.; Lichtenstein, P.; Kerekes, N.; Råstam, M.; Anckarsäter, H. Physical health in children with neurodevelopmental disorders. J. Autism Dev. Disord. 2019, 49, 83–95. [Google Scholar] [CrossRef]
- Severance, E.G.; Yolken, R.H.; Eaton, W.W. Autoimmune diseases, gastrointestinal disorders and the microbiome in schizophrenia: More than a gut feeling. Schizophr. Res. 2016, 176, 23–35. [Google Scholar] [CrossRef]
- Oliveira-Maia, A.J.; Andrade, I.; Barahona-Corrêa, J.B. Case of coeliac disease presenting in the psychiatry ward. Case Rep. 2016. [Google Scholar] [CrossRef]
- Fiorentino, M.; Sapone, A.; Senger, S.; Camhi, S.S.; Kadzielski, S.M.; Buie, T.M.; Kelly, D.L.; Cascella, N.; Fasano, A. Blood–brain barrier and intestinal epithelial barrier alterations in autism spectrum disorders. Mol. Autism 2016, 7, 49. [Google Scholar] [CrossRef] [PubMed]
- Kelly, D.L.; Demyanovich, H.K.; Eaton, W.W.; Cascella, N.; Jackson, J.; Fasano, A.; Carpenter, W.T. Anti gliadin antibodies (AGA IgG) related to peripheral inflammation in schizophrenia. Brain Behav. Immun. 2018, 69, 57–59. [Google Scholar] [CrossRef] [PubMed]
- Pellicano, R.; Durazzo, M. Schizophrenia and celiac disease. Eur. J. Gastroenterol. Hepatol. 2018, 30, 806–807. [Google Scholar] [CrossRef]
- Dohan, F.C. Genetic hypothesis of idiopathic schizophrenia: Its exorphin connection. Schizophr. Bull. 1988, 14, 489–494. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dehhaghi, M.; Kazemi Shariat Panahi, H.; Guillemin, G.J. Microorganisms, tryptophan metabolism, and kynurenine pathway: A complex interconnected loop influencing human health status. Int. J. Tryptophan Res. 2019, 12, 1–10. [Google Scholar] [CrossRef]
- Groer, M.; Fuchs, D.; Duffy, A.; Louis-Jacques, A.; D’Agata, A.; Postolache, T.T. Associations Among Obesity, Inflammation, and Tryptophan Catabolism in Pregnancy. Biol. Res. Nurs. 2018, 20, 284–291. [Google Scholar] [CrossRef]
- Sacchetti, L.; Nardelli, C. Gut microbiome investigation in celiac disease: From methods to its pathogenetic role. Clin. Chem. Lab. Med. 2019. [Google Scholar] [CrossRef]
- Zylberberg, H.M.; Ludvigsson, J.F.; Green, P.H.; Lebwohl, B. Psychotropic medication use among patients with celiac disease. BMC Psychiatry 2018, 18, 76. [Google Scholar] [CrossRef]
- Wijarnpreecha, K.; Jaruvongvanich, V.; Cheungpasitporn, W.; Ungprasert, P. Response to: ‘Schizophrenia and celiac disease which is the role of the gluten-free diet? Eur. J. Gastroenterol. Hepatol. 2018, 30, 806. [Google Scholar] [CrossRef]
- Blackett, J.W.; Shamsunder, M.; Reilly, N.R.; Green, P.H.; Lebwohl, B. Characteristics and comorbidities of inpatients without celiac disease on a gluten-free diet. Eur. J. Gastroenterol. Hepatol. 2018, 30, 477–483. [Google Scholar] [CrossRef]
- Calderoni, S.; Santocchi, E.; Del Bianco, T.; Brunori, E.; Caponi, L.; Paolicchi, A.; Fulceri, F.; Prosperi, M.; Narzisi, A.; Cosenza, A.; et al. Serological screening for Celiac Disease in 382 pre-schoolers with Autism Spectrum Disorder. Ital. J. Pediatr. 2016, 42, 98. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, J.F.; Reichenberg, A.; Hultman, C.M.; Murray, J.A. A nationwide study of the association between celiac disease and the risk of autistic spectrum disorders. JAMA Psychiatry 2013, 70, 1224–1230. [Google Scholar] [CrossRef] [PubMed]
- Batista, I.C.; Gandolfi, L.; Nobrega, Y.K.M.; Almeida, R.C.; Almeida, L.M.; Campos Junior, D.; Pratesi, R. Autism spectrum disorder and celiac disease: No evidence for a link. Arq. Neuro-Psiquiatr. 2012, 70, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Butwicka, A.; Lichtenstein, P.; Frisén, L.; Almqvist, C.; Larsson, H.; Ludvigsson, J.F. Celiac disease is associated with childhood psychiatric disorders: A population-based study. J. Pediatr. 2017, 184, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Mazzone, L.; Reale, L.; Spina, M.; Guarnera, M.; Lionetti, E.; Martorana, S.; Mazzone, D. Compliant gluten-free children with celiac disease: An evaluation of psychological distress. BMC Pediatr. 2011, 11, 46. [Google Scholar] [CrossRef] [PubMed]
- Zelnik, N.; Pacht, A.; Obeid, R.; Lerner, A. Range of neurologic disorders in patients with celiac disease. Pediatrics 2004, 113, 1672–1676. [Google Scholar] [CrossRef]
- Pavone, L.; Fiumara, A.; Bottaro, G.; Mazzone, D.; Coleman, M. Autism and celiac disease: Failure to validate the hypothesis that a link might exist. Biol. Psychiatry 1997, 42, 72–75. [Google Scholar] [CrossRef]
- Juneja, M.; Venkatakrishnan, A.; Kapoor, S.; Jain, R. Autism Spectrum Disorders and Celiac Disease: Is there an Association? Ind. Pediatr. 2018, 55, 912–914. [Google Scholar]
- Józefczuk, J.; Konopka, E.; Bierła, J.B.; Trojanowska, I.; Sowińska, A.; Czarnecki, R.; Sobol, L.; Józefczuk, P.; Surdy, W.; Cukrowska, B. The occurrence of antibodies against gluten in children with autism spectrum disorders does not correlate with serological markers of impaired intestinal permeability. J. Med. Food 2018, 21, 181–187. [Google Scholar] [CrossRef]
- Sel, Ç.G.; Aksoy, E.; Aksoy, A.; Yüksel, D.; Özbay, F. Neurological manifestations of atypical celiac disease in childhood. Acta Neurol. Belg. 2017, 117, 719–727. [Google Scholar] [CrossRef]
- Pynnönen, P.A.; Isometsä, E.T.; Verkasalo, M.A.; Kähkönen, S.A.; Sipilä, I.; Savilahti, E.; Aalberg, V.A. Gluten-free diet may alleviate depressive and behavioural symptoms in adolescents with coeliac disease: A prospective follow-up case-series study. BMC Psychiatry 2005, 5, 14. [Google Scholar] [CrossRef]
- Işikay, S.; Kocamaz, H. The neurological face of celiac disease. Arq. Gastroenterol. 2015, 52, 167–170. [Google Scholar] [CrossRef]
- Vaknin, A.; Eliakim, R.; Ackerman, Z.; Steiner, I. Neurological abnormalities associated with celiac disease. J. Neurol. 2004, 251, 1393–1397. [Google Scholar] [CrossRef]
- Garud, S.; Leffler, D.; Dennis, M.; Edwards-George, J.; Saryan, D.; Sheth, S.; Schuppan, D.; Jamma, S.; Kelly, C.P. Interaction between psychiatric and autoimmune disorders in coeliac disease patients in the Northeastern United States. Aliment. Pharmacol. Ther. 2009, 29, 898–905. [Google Scholar] [CrossRef]
- Güngör, S.; Celiloglu, Ö.S.; Özcan, Ö.Ö.; Raif, S.G.; Selimoglu, M.A. Frequency of celiac disease in attention-deficit/hyperactivity disorder. J. Pediatr. Gastroenterol. Nutr. 2013, 56, 211–214. [Google Scholar] [CrossRef]
- Lahat, E.; Broide, E.; Leshem, M.; Evans, S.; Scapa, E. Prevalence of celiac antibodies in children with neurologic disorders. Pediatr. Neurol. 2000, 22, 393–396. [Google Scholar] [CrossRef]
- Ramírez-Cervantes, K.L.; Remes-Troche, J.M.; del Pilar Milke-García, M.; Romero, V.; Uscanga, L.F. Characteristics and factors related to quality of life in Mexican Mestizo patients with celiac disease. BMC Gastroenterol. 2015, 15, 4. [Google Scholar] [CrossRef]
- Sevinç, E.; Çetin, F.H.; Coşkun, B.D. Psychopathology, quality of life, and related factors in children with celiac disease. J. Pediatr. 2017, 93, 267–273. [Google Scholar] [CrossRef]
- Briani, C.; Zara, G.; Alaedini, A.; Grassivaro, F.; Ruggero, S.; Toffanin, E.; Albergoni, M.P.; Luca, M.; Giometto, B.; Ermani, M.; et al. Neurological complications of celiac disease and autoimmune mechanisms: A prospective study. J. Neuroimmunol. 2008, 195, 171–175. [Google Scholar] [CrossRef]
- Ludvigsson, J.F.; Reutfors, J.; Ösby, U.; Ekbom, A.; Montgomery, S.M. Coeliac disease and risk of mood disorders—a general population-based cohort study. J. Affect. Disord. 2007, 99, 117–126. [Google Scholar] [CrossRef]
- Siniscalchi, M.; Iovino, P.; Tortora, R.; Forestiero, S.; Somma, A.; Capuano, L.; Franzese, M.D.; Sabbatini, F.; Ciacci, C. Fatigue in adult coeliac disease. Aliment. Pharmacol. Ther. 2005, 22, 489–494. [Google Scholar] [CrossRef]
- Pynnönen, P.A.; Isometsä, E.T.; Aronen, E.T.; Verkasalo, M.A.; Savilahti, E.; Aalberg, V.A. Mental disorders in adolescents with celiac disease. Psychosomatics 2004, 45, 325–335. [Google Scholar] [CrossRef]
- Fera, T.; Cascio, B.; Angelini, G.; Martini, S.; Guidetti, C.S. Affective disorders and quality of life in adult coeliac disease patients on a gluten-free diet. Eur. J. Gastroenterol. Hepatol. 2003, 15, 1287–1292. [Google Scholar] [CrossRef]
- Carta, M.G.; Hardoy, M.C.; Boi, M.F.; Mariotti, S.; Carpiniello, B.; Usai, P. Association between panic disorder, major depressive disorder and celiac disease: A possible role of thyroid autoimmunity. J. Psychosom. Res. 2002, 53, 789–793. [Google Scholar] [CrossRef]
- Addolorato, G. Anxiety but not depression decreases in coeliac patients after one-year gluten-free diet: A longitudinal study. Scand. J. Gastroenterol. 2001, 36, 502–506. [Google Scholar] [CrossRef]
- Ciacci, C.; Iavarone, A.; Mazzacca, G.; De Rosa, A. Depressive symptoms in adult coeliac disease. Scand. J. Gastroenterol. 1998, 33, 247–250. [Google Scholar] [CrossRef]
- Paarlahti, P.; Kurppa, K.; Ukkola, A.; Collin, P.; Huhtala, H.; Mäki, M.; Kaukinen, K. Predictors of persistent symptoms and reduced quality of life in treated coeliac disease patients: A large cross-sectional study. BMC Gastroenterol. 2013, 13, 75. [Google Scholar] [CrossRef]
- Addolorato, G.; Mirijello, A.; D’Angelo, C.; Leggio, L.; Ferrulli, A.; Vonghia, L.; Cardone, S.; Leso, V.; Miceli, A.; Gasbarrini, G. Social phobia in coeliac disease. Scand. J. Gastroenterol. 2008, 43, 410–415. [Google Scholar] [CrossRef]
- Joelson, A.; Geller, M.; Zylberberg, H.; Green, P.; Lebwohl, B. The effect of depressive symptoms on the association between gluten-free diet adherence and symptoms in celiac disease: Analysis of a patient powered research network. Nutrients 2018, 10, 538. [Google Scholar] [CrossRef]
- Kotze, L.M.D.S. Celiac disease in Brazilian patients: Associations, complications and causes of death. Forty years of clinical experience. Arq. Gastroenterol. 2009, 46, 261–269. [Google Scholar] [CrossRef][Green Version]
- Saleem, A.; Connor, H.J.O.; Regan, P.O. Adult coeliac disease in Ireland: A case series. Ir. J. Med. Sci. 2012, 181, 225–229. [Google Scholar] [CrossRef]
- Addolorato, G.; De Lorenzi, G.; Abenavoli, L.; Leggio, L.; Capristo, E.; Gasbarrini, G. Psychological support counselling improves gluten-free diet compliance in coeliac patients with affective disorders. Aliment. Pharmacol. Ther. 2004, 20, 777–782. [Google Scholar] [CrossRef]
- Mårild, K.; Størdal, K.; Bulik, C.M.; Rewers, M.; Ekbom, A.; Liu, E.; Ludvigsson, J.F. Celiac disease and anorexia nervosa: A nationwide study. Pediatrics 2017, 139, e20164367. [Google Scholar] [CrossRef]
- Karwautz, A.; Wagner, G.; Berger, G.; Sinnreich, U.; Grylli, V.; Huber, W.D. Eating pathology in adolescents with celiac disease. Psychosomatics 2008, 49, 399–406. [Google Scholar] [CrossRef]
- Bonamico, M.; Mariani, P.; Danesi, H.M.; Crisogianni, M.; Failla, P.; Gemme, G.; Quartino, A.R.; Giannotti, A.; Castro, M.; Balli, F.; et al. Prevalence and clinical picture of celiac disease in Italian Down syndrome patients: A multicenter study. J. Pediatr. Gastroenterol. Nutr. 2001, 33, 139–143. [Google Scholar] [CrossRef]
- Basso, M.S.; Zanna, V.; Panetta, F.; Caramadre, A.M.; Ferretti, F.; Ottino, S.; Diamanti, A. Is the screening for celiac disease useful in anorexia nervosa? Eur. J. Pediatr. 2013, 172, 261–263. [Google Scholar] [CrossRef]
- Welch, E.; Ghaderi, A.; Swenne, I. A comparison of clinical characteristics between adolescent males and females with eating disorders. BMC Psychiatry 2015, 15, 45. [Google Scholar] [CrossRef]
- Nemani, K.; Hosseini Ghomi, R.; McCormick, B.; Fan, X. Schizophrenia and the gut–brain axis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2015, 56, 155–160. [Google Scholar] [CrossRef]
- Benros, M.E.; Eaton, W.W.; Mortensen, P.B. The epidemiologic evidence linking autoimmune diseases and psychosis. Biol. Psychiatry 2014, 75, 300–306. [Google Scholar] [CrossRef]
- Atkins, D.; Best, D.; Briss, P.A.; Eccles, M.; Falck-Ytter, Y.; Flottorp, S.; Guyatt, G.H.; Harbour, R.T.; Haugh, M.C.; Henry, D.; et al. Grading quality of evidence and strength of recommendations. BMJ 2004, 328, 1490. [Google Scholar]

| Parameter | Value |
|---|---|
| Number of papers | 37 |
| Population (%) | |
| Adult | 32 |
| Children | 46 |
| Mixed | 22 |
| Type of study | |
| Cohort | 2 |
| Case-controlled | 18 |
| Cohort and Case-controlled | 1 |
| Cross-sectional | 14 |
| Psychiatric disorder | |
| ASD | 9 |
| ADHD | 8 |
| Mood disorders | 20 |
| Schizophrenia and other psychotic disorders | 6 |
| Eating disorders | 9 |
| Year of publication (%) | |
| Until 2000 | 5 |
| 2000–2009 | 43 |
| 2010–2019 | 51 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clappison, E.; Hadjivassiliou, M.; Zis, P. Psychiatric Manifestations of Coeliac Disease, a Systematic Review and Meta-Analysis. Nutrients 2020, 12, 142. https://doi.org/10.3390/nu12010142
Clappison E, Hadjivassiliou M, Zis P. Psychiatric Manifestations of Coeliac Disease, a Systematic Review and Meta-Analysis. Nutrients. 2020; 12(1):142. https://doi.org/10.3390/nu12010142
Chicago/Turabian StyleClappison, Emma, Marios Hadjivassiliou, and Panagiotis Zis. 2020. "Psychiatric Manifestations of Coeliac Disease, a Systematic Review and Meta-Analysis" Nutrients 12, no. 1: 142. https://doi.org/10.3390/nu12010142
APA StyleClappison, E., Hadjivassiliou, M., & Zis, P. (2020). Psychiatric Manifestations of Coeliac Disease, a Systematic Review and Meta-Analysis. Nutrients, 12(1), 142. https://doi.org/10.3390/nu12010142







