Diet Quality Affects the Association between Census-Based Neighborhood Deprivation and All-Cause Mortality in Japanese Men and Women: The Japan Public Health Center-Based Prospective Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Measurement of Area Deprivation
2.3. Food Frequency Questionnaire and The Japanese Food Guide Spinning Top Score
2.4. Study Subjects
2.5. Follow-up and Outcome
2.6. Statistical Analysis
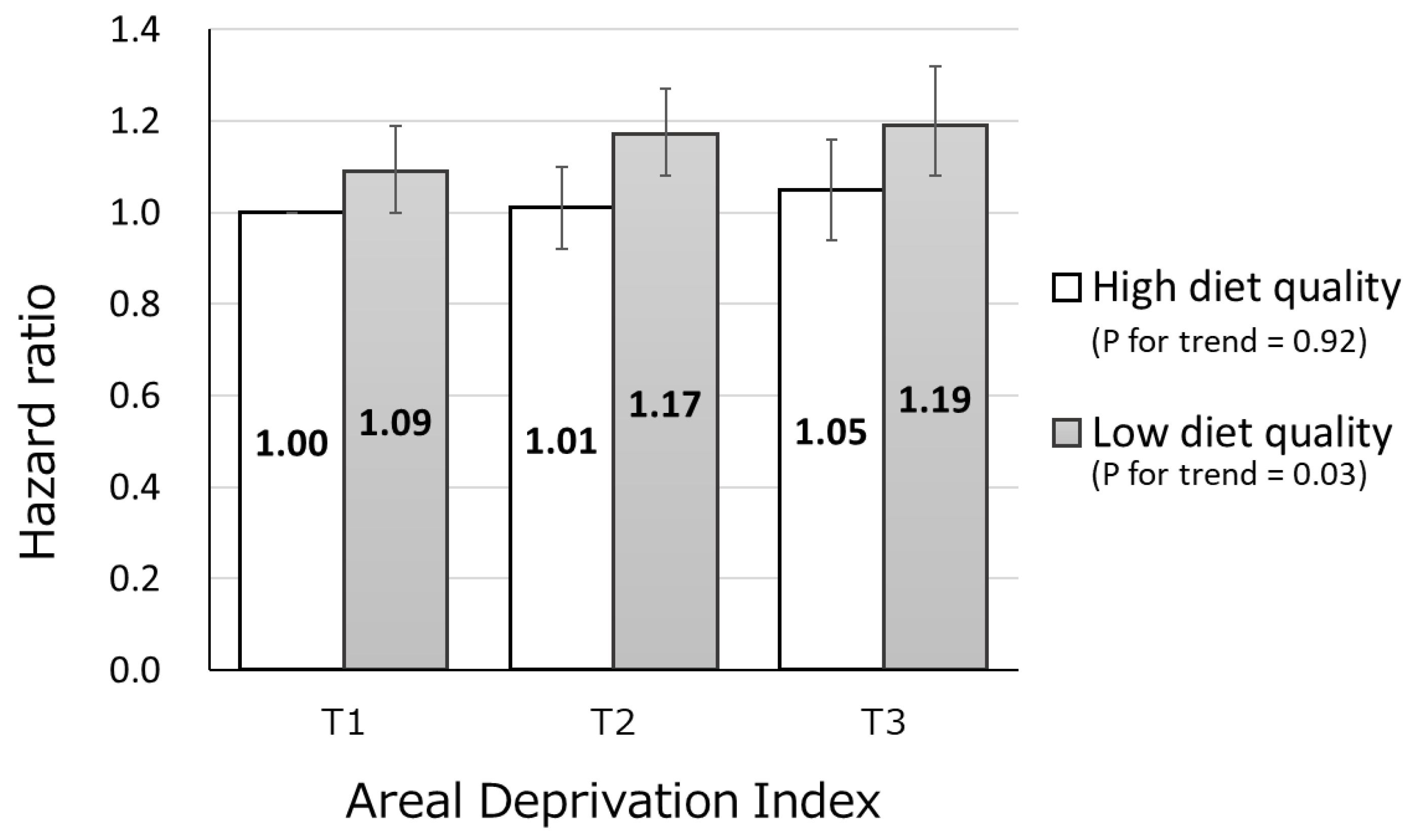
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Marmot, M. Social determinants of health inequalities. Lancet 2005, 365, 1099–1104. [Google Scholar] [CrossRef]
- Honjo, K.; Iso, H.; Nakaya, T.; Hanibuchi, T.; Ikeda, A.; Inoue, M.; Sawada, N.; Tsugane, S.; The Japan Public Health Center-based Prospective Study Group. Impact of Neighborhood Socioeconomic Conditions on the Risk of Stroke in Japan. J. Epidemiol. 2015, 25, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Ghosn, W.; Menvielle, G.; Rican, S.; Rey, G. Associations of cause-specific mortality with area level deprivation and travel time to health care in France from 1990 to 2007, a multilevel analysis. BMC Public Health 2017, 18, 86. [Google Scholar] [CrossRef] [PubMed]
- Bethea, T.N.; Palmer, J.R.; Rosenberg, L.; Cozier, Y.C. Neighborhood Socioeconomic Status in Relation to All-Cause, Cancer, and Cardiovascular Mortality in the Black Women’s Health Study. Ethn. Dis. 2016, 26, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Major, J.M.; Doubeni, C.A.; Freedman, N.D.; Park, Y.; Lian, M.; Hollenbeck, A.R.; Schatzkin, A.; Graubard, B.I.; Sinha, R. Neighborhood Socioeconomic Deprivation and Mortality: NIH-AARP Diet and Health Study. PLoS ONE 2010, 5, e15538. [Google Scholar] [CrossRef] [PubMed]
- Ito, Y.; Nakaya, T.; Nakayama, T.; Miyashiro, I.; Ioka, A.; Tsukuma, H.; Rachet, B. Socioeconomic inequalities in cancer survival: A population-based study of adult patients diagnosed in Osaka, Japan, during the period 1993-2004. Acta Oncol. 2014, 53, 1423–1433. [Google Scholar] [CrossRef]
- Li, X.; Sundquist, J.; Zöller, B.; Sundquist, K. Neighborhood Deprivation and Lung Cancer Incidence and Mortality: A Multilevel Analysis from Sweden. J. Thorac. Oncol. 2015, 10, 256–263. [Google Scholar] [CrossRef]
- Nakaya, T.; Honjo, K.; Hanibuchi, T.; Ikeda, A.; Iso, H.; Inoue, M.; Sawada, N.; Tsugane, S.; The Japan Public Health Center-based Prospective Study Group. Associations of All-Cause Mortality with Census-Based Neighbourhood Deprivation and Population Density in Japan: A Multilevel Survival Analysis. PLoS ONE 2014, 9, e97802. [Google Scholar] [CrossRef] [PubMed]
- Algren, M.H.; Bak, C.K.; Berg-Beckhoff, G.; Andersen, P.T. Health-Risk Behaviour in Deprived Neighbourhoods Compared with Non-Deprived Neighbourhoods: A Systematic Literature Review of Quantitative Observational Studies. PLoS ONE 2015, 10, e0139297. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Bogensberger, B.; Hoffmann, G. Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: An Updated Systematic Review and Meta-Analysis of Cohort Studies. J. Acad. Nutr. Diet. 2018, 118, 74–100. [Google Scholar] [CrossRef]
- Kurotani, K.; Akter, S.; Kashino, I.; Goto, A.; Mizoue, T.; Noda, M.; Sasazuki, S.; Sawada, N.; Tsugane, S. Quality of diet and mortality among Japanese men and women: Japan Public Health Center based prospective study. BMJ 2016, 352, i1209. [Google Scholar] [CrossRef]
- Yu, D.; Zhang, X.; Xiang, Y.B.; Yang, G.; Li, H.; Gao, Y.T.; Zheng, W.; Shu, X.O. Adherence to dietary guidelines and mortality: A report from prospective cohort studies of 134,000 Chinese adults in urban Shanghai. Am. J. Clin. Nutr. 2014, 100, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Oba, S.; Nagata, C.; Nakamura, K.; Fujii, K.; Kawachi, T.; Takatsuka, N.; Shimizu, H. Diet based on the Japanese Food Guide Spinning Top and subsequent mortality among men and women in a general Japanese population. J. Am. Diet. Assoc. 2009, 109, 1540–1547. [Google Scholar] [CrossRef] [PubMed]
- Forouzanfar, M.H.; Alexander, L.; Anderson, H.R.; Bachman, V.F.; Biryukov, S.; Brauer, M.; Burnett, R.; Casey, D.; Coates, M.M.; Cohen, A.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar] [CrossRef]
- Yoshiike, N.; Hayashi, F.; Takemi, Y.; Mizoguchi, K.; Seino, F. A new food guide in Japan: The Japanese food guide Spinning Top. Nutr. Rev. 2007, 65, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Tsugane, S.; Sobue, T. Baseline survey of JPHC study—Design and participation rate. Japan Public Health Center-based Prospective Study on Cancer and Cardiovascular Diseases. J. Epidemiol. 2001, 11, S24–S29. [Google Scholar] [CrossRef] [PubMed]
- Nakaya, T. Evaluating Socio-economic Inequalities in Cancer Mortality by Using Areal Statistics in Japan: A Note on the Relation between Municipal Cancer Mortality and Areal Deprivation Index. Proc. Inst. Stat. Math. 2011, 59, 239–265. [Google Scholar]
- Gordon, D. Census based deprivation indices: Their weighting and validation. J. Epidemiol. Community Health 1995, 49, S39–S44. [Google Scholar] [CrossRef]
- Dorling, D.; Rigby, J.; Wheeler, B.; Ballas, D.; Thomas, B.; Fahmy, E.; Gordon, D.; Lupton, R. Poverty and wealth across Britain 1968 to 2005. Available online: https://www.jrf.org.uk/sites/default/files/jrf/migrated/files/2019-poverty-wealth-place.pdf (accessed on 20 August 2009).
- Guillaume, E.; Pornet, C.; Dejardin, O.; Launay, L.; Lillini, R.; Vercelli, M.; Marí-Dell’Olmo, M.; Fernández Fontelo, A.; Borrell, C.; Ribeiro, A.I.; et al. Development of a cross-cultural deprivation index in five European countries. J. Epidemiol. Community Health 2016, 70, 493–499. [Google Scholar] [CrossRef]
- Sasaki, S.; Kobayashi, M.; Ishihara, J.; Tsugane, S. Self-administered food frequency questionnaire used in the 5-year follow-up survey of the JPHC Study: Questionnaire structure, computation algorithms, and area-based mean intake. J. Epidemiol. 2003, 13, S13–S22. [Google Scholar] [CrossRef]
- Sasaki, S.; Ishihara, J.; Tsugane, S. Reproducibility of a self-administered food frequency questionnaire used in the 5-year follow-up survey of the JPHC Study Cohort I to assess food and nutrient intake. J. Epidemiol. 2003, 13, S115–S124. [Google Scholar] [CrossRef]
- Sasaki, S.; Kobayashi, M.; Tsugane, S. Validity of a self-administered food frequency questionnaire used in the 5-year follow-up survey of the JPHC Study Cohort I: Comparison with dietary records for food groups. J. Epidemiol. 2003, 13, S57–S63. [Google Scholar] [CrossRef]
- Ishihara, J.; Sobue, T.; Yamamoto, S.; Yoshimi, I.; Sasaki, S.; Kobayashi, M.; Takahashi, T.; Iitoi, Y.; Akabane, M.; Tsugane, S. Validity and reproducibility of a self-administered food frequency questionnaire in the JPHC Study Cohort II: Study design, participant profile and results in comparison with Cohort I. J. Epidemiol. 2003, 13, S134–S147. [Google Scholar] [CrossRef]
- World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems: 10th Revision; World Health Organization: Geneva, Switzerland, 1992. [Google Scholar]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; Wiley: New York, NY, USA, 1987. [Google Scholar]
- Wrigley, N.; Warm, D.; Margetts, B. Deprivation, Diet, and Food-Retail Access: Findings from the Leeds ‘Food Deserts’ Study. Environ. Plan. A Econ. Space 2003, 35, 151–188. [Google Scholar] [CrossRef]
- Caspi, C.E.; Sorensen, G.; Subramanian, S.V.; Kawachi, I. The local food environment and diet: A systematic review. Health Place 2012, 18, 1172–1187. [Google Scholar] [CrossRef]
- Ishikawa, M.; Takemi, Y.; Yokoyama, T.; Kusama, K.; Fukuda, Y.; Nakaya, T.; Nozue, M.; Yoshiike, N.; Yoshiba, K.; Hayashi, F.; et al. “Eating Together” Is Associated with Food Behaviors and Demographic Factors of Older Japanese People Who Live Alone. J. Nutr. Health Aging 2017, 21, 662–672. [Google Scholar] [CrossRef]
| Area Deprivation Index | |||
|---|---|---|---|
| Tertile 1 (Low) | Tertile 2 | Tertile 3 (High) | |
| N | 20,522 | 20,314 | 20,431 |
| Area Deprivation index * | 165.8–514.3 | 514.3–589.0 | 589.1–983.3 |
| Population density | 1640 (12.5) | 1067 (12.5) | 1173 (12.5) |
| Age (years) † | 51.1 (7.74) | 50.8 (7.33) | 52.2 (7.92) |
| Men (%) | 46.8 | 45.5 | 44.8 |
| Body mass index (kg/m2) ‡, ¶ | 23.3 (0.02) | 23.5 (0.02) | 24.0 (0.02) |
| Total physical activity (metabolic equivalents hours/week) ‡, ¶ | 32.9 (0.05) | 33.4 (0.05) | 33.8 (0.05) |
| Current smoker (%) ¶, § | 16.8 | 15.8 | 12.2 |
| Alcohol consumption ≥1 d/wk (%) ¶, § | 35.1 | 32.0 | 23.1 |
| History of hypertension (%) § | 17.8 | 16.6 | 17.3 |
| History of dyslipidemia (%) § | 5.5 | 4.8 | 3.2 |
| History of diabetes (%) § | 5.7 | 5.8 | 5.7 |
| Occupation (agriculture, forestry and fishery, %) § | 13.8 | 20.4 | 26.6 |
| Living alone (%) § | 2.8 | 3.4 | 4.4 |
| Age- and Sex-Adjusted Mean (Standard Error) | p Trend * | |||
|---|---|---|---|---|
| Area Deprivation Index | ||||
| Tertile 1 (Low) | Tertile 2 | Tertile 3 (High) | ||
| Energy (kcal) | 2034 (4.1) | 2070 (4.1) | 1951 (4.1) | <0.0001 |
| Nutrient intake (/1000kcal) | ||||
| Total protein (g) | 36.9 (0.04) | 36.7 (0.04) | 35.1 (0.04) | <0.0001 |
| Total fat (g) | 27.6 (0.05) | 27.7 (0.05) | 29.8 (0.05) | <0.0001 |
| Saturated fat (g) | 8.3 (0.02) | 8.3 (0.02) | 9.2 (0.02) | <0.0001 |
| Monounsaturated fat (g) | 9.5 (0.02) | 9.5 (0.02) | 10.4 (0.02) | <0.0001 |
| Polyunsaturated fat (g) | 6.4 (0.01) | 6.4 (0.01) | 6.7 (0.01) | <0.0001 |
| Cholesterol (mg) | 146 (0.5) | 149 (0.5) | 143 (0.5) | <0.0001 |
| Total carbohydrate (g) | 137 (0.2) | 138 (0.2) | 134 (0.2) | <0.0001 |
| Dietary fiber (g) | 6.9 (0.01) | 6.7 (0.02) | 6.3 (0.01) | <0.0001 |
| Calcium (mg) | 272 (0.7) | 269 (0.7) | 252 (0.7) | <0.0001 |
| Sodium (mg) | 2502 (13.1) | 2452 (13.2) | 2420 (13.2) | <0.0001 |
| Food intake (g) | ||||
| Grains | 550.1 (1.17) | 571.9 (1.17) | 527.4 (1.17) | <0.0001 |
| Potatoes | 30.1 (0.18) | 29.0 (0.18) | 24.5 (0.18) | <0.0001 |
| Vegetables | 226.0 (0.99) | 227.7 (1.00) | 222.0 (0.99) | 0.005 |
| Green and yellow vegetables | 102.6 (0.54) | 103.9 (0.54) | 98.4 (0.54) | <0.0001 |
| Other vegetables | 123.4 (0.58) | 123.8 (0.58) | 123.6 (0.58) | 0.78 |
| Pickled vegetables | 44.2 (0.29) | 41.4 (0.29) | 23.4 (0.29) | <0.0001 |
| Fruit | 243.3 (1.20) | 238.2 (1.21) | 185.9 (1.20) | <0.0001 |
| Mushroom | 11.5 (0.08) | 11.6 (0.08) | 8.1 (0.08) | <0.0001 |
| Pulses | 89.4 (0.60) | 91.4 (0.60) | 94.0 (0.60) | <0.0001 |
| Fish and shellfish | 100.8 (0.45) | 103.7 (0.45) | 81.5 (0.45) | <0.0001 |
| Meat | 60.7 (0.38) | 62.4 (0.38) | 71.6 (0.38) | <0.0001 |
| Eggs | 29.7 (0.22) | 31.8 (0.22) | 30.0 (0.22) | 0.24 |
| Dairy products | 191.1 (1.34) | 192.0 (1.35) | 167.5 (1.35) | <0.0001 |
| Coffee (≥1 cup/day, %) | 28.5 | 32.3 | 36.3 | <0.0001 |
| Green tea (≥1 cup/day, %) | 71.4 | 62.9 | 45.3 | <0.0001 |
| Japanese Food Guide Spinning Top score | 48.3 (0.06) | 48.5 (0.06) | 46.6 (0.06) | <0.0001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kurotani, K.; Honjo, K.; Nakaya, T.; Ikeda, A.; Mizoue, T.; Sawada, N.; Tsugane, S.; Japan Public Health Center-based Prospective Study Group. Diet Quality Affects the Association between Census-Based Neighborhood Deprivation and All-Cause Mortality in Japanese Men and Women: The Japan Public Health Center-Based Prospective Study. Nutrients 2019, 11, 2194. https://doi.org/10.3390/nu11092194
Kurotani K, Honjo K, Nakaya T, Ikeda A, Mizoue T, Sawada N, Tsugane S, Japan Public Health Center-based Prospective Study Group. Diet Quality Affects the Association between Census-Based Neighborhood Deprivation and All-Cause Mortality in Japanese Men and Women: The Japan Public Health Center-Based Prospective Study. Nutrients. 2019; 11(9):2194. https://doi.org/10.3390/nu11092194
Chicago/Turabian StyleKurotani, Kayo, Kaori Honjo, Tomoki Nakaya, Ai Ikeda, Tetsuya Mizoue, Norie Sawada, Shoichiro Tsugane, and Japan Public Health Center-based Prospective Study Group. 2019. "Diet Quality Affects the Association between Census-Based Neighborhood Deprivation and All-Cause Mortality in Japanese Men and Women: The Japan Public Health Center-Based Prospective Study" Nutrients 11, no. 9: 2194. https://doi.org/10.3390/nu11092194
APA StyleKurotani, K., Honjo, K., Nakaya, T., Ikeda, A., Mizoue, T., Sawada, N., Tsugane, S., & Japan Public Health Center-based Prospective Study Group. (2019). Diet Quality Affects the Association between Census-Based Neighborhood Deprivation and All-Cause Mortality in Japanese Men and Women: The Japan Public Health Center-Based Prospective Study. Nutrients, 11(9), 2194. https://doi.org/10.3390/nu11092194





