Child-Sensitive WASH Composite Score and the Nutritional Status in Cambodian Children
Abstract
1. Introduction
2. Key Messages
3. Methods
3.1. Data Source
3.1.1. Anthropometric Measurements
3.1.2. Water, Sanitation and Hygiene Measurements
3.1.3. Variable Included in the Analyses
3.1.4. Statistical Analyses
4. Results
4.1. General Characteristics of Participants
4.2. Anthropometric Characteristics of Participants
4.3. Water, Sanitation and Hygiene Characteristics of Participants
4.4. Univariate and Multivariate Analyses for Wasting
4.5. Univariate and Multivariate Analyses for Stunting
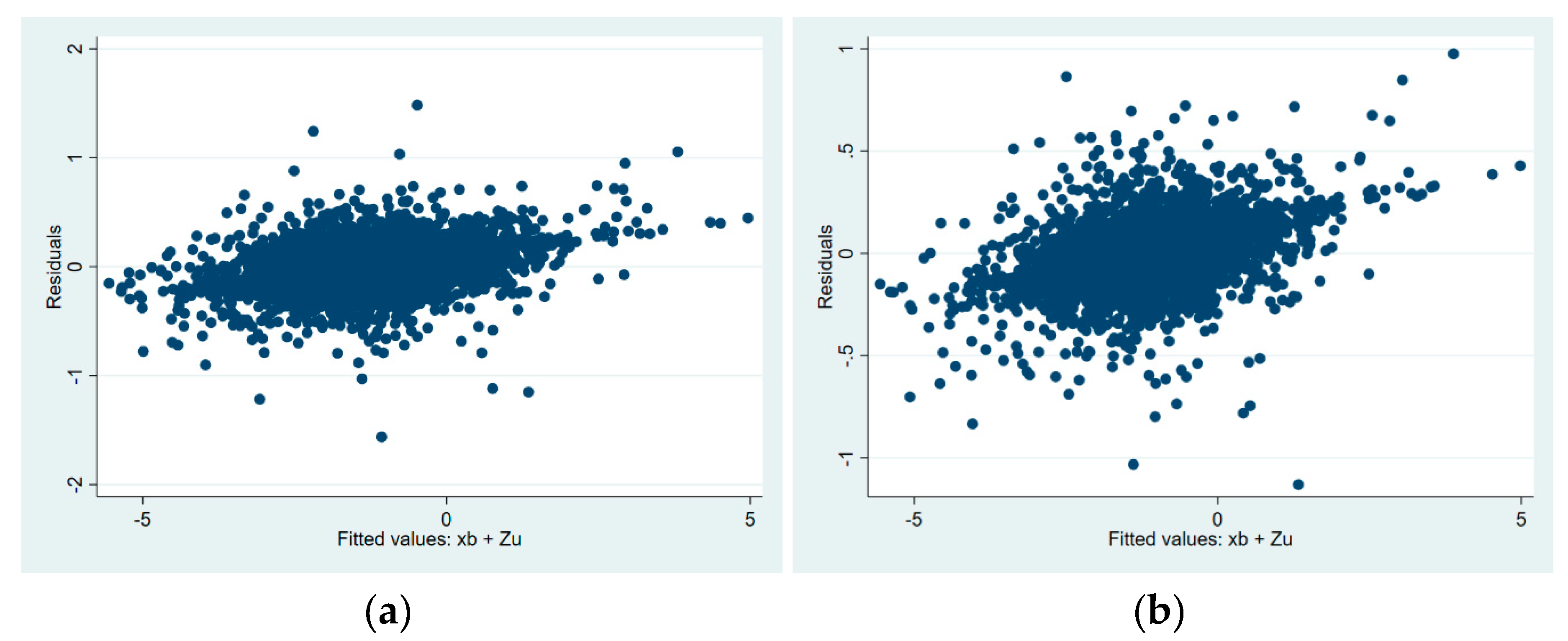
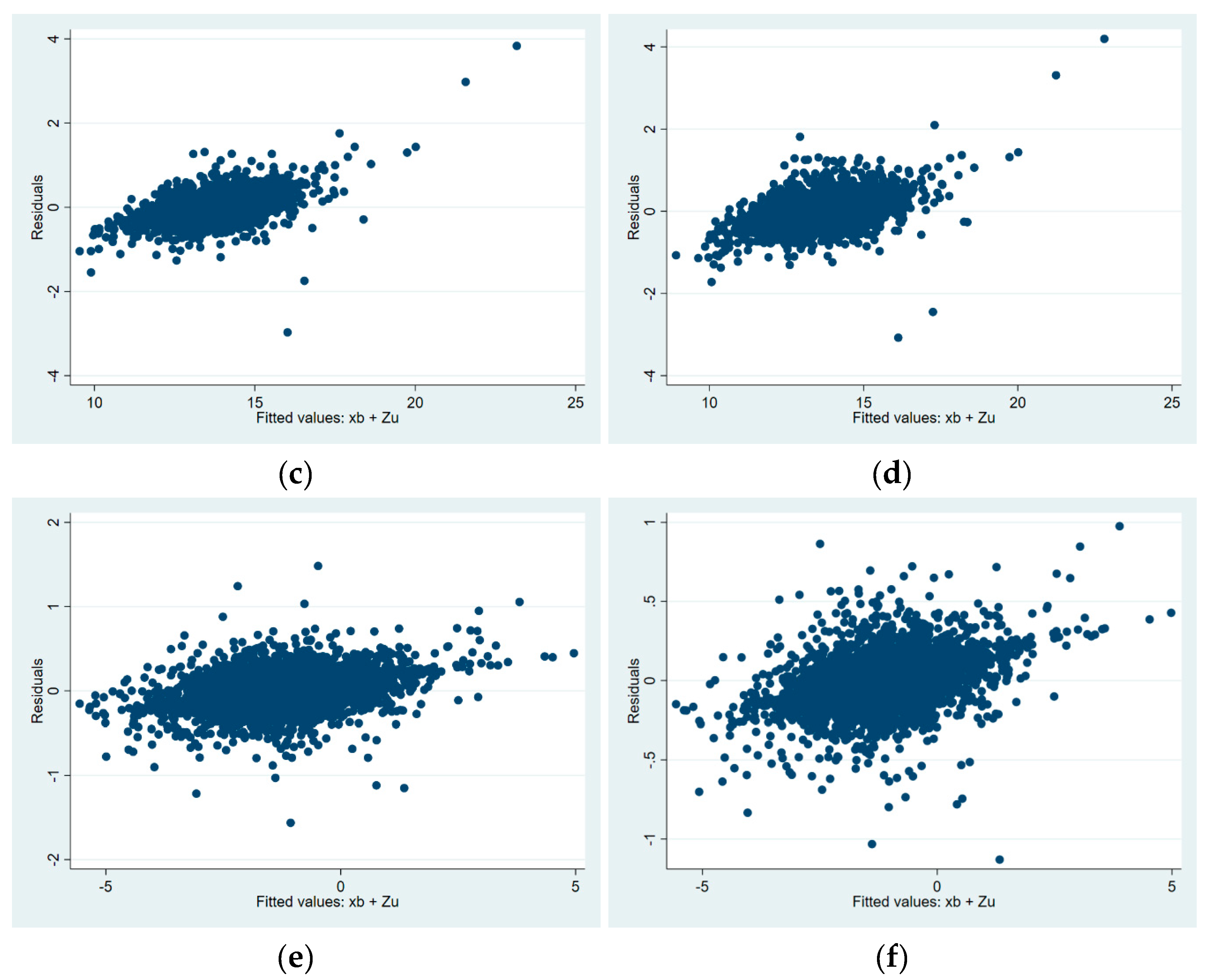
5. Model Diagnostics
6. Discussion
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Action Against Hunger. WASH’ Nutrition a Practical Guidebook on Increasing Nutritional Impact through Integration of Wash and Nutrition Programmes. 2017. Available online: https://www.actionagainsthunger.org/sites/default/files/publications/2017_ACF_WASH_Nutrition_Guidebook_BD.pdf (accessed on 16 January 2017).
- Adair, L.S. Long-Term Consequences of Nutrition and Growth in Early Childhood and Possible Preventive Interventions. Nestle Nutr. Inst. Workshop Ser. 2014, 78, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Arnold, B.; Arana, B.; Mäusezahl, D.; Hubbard, A.; Colford, J.M. Evaluation of a Pre-Existing, 3-Year Household Water Treatment and Handwashing Intervention in Rural Guatemala. Int. J. Epidemiol. 2009, 38, 1651–1661. [Google Scholar] [CrossRef] [PubMed]
- Bagriansky, J.; Champa, N.; Pak, K.; Whitney, S.; Laillou, A. The Economic Consequences of Malnutrition in Cambodia, More than 400 Million US Dollar Lost Annually. Asia Pac. J. Clin. Nutr. 2014, 23, 524–531. [Google Scholar] [PubMed]
- Bowen, A.; Agboatwalla, M.; Luby, S.; Tobery, T.; Ayers, T.; Hoekstra, R.M. Association Between Intensive Handwashing Promotion and Child Development in Karachi, Pakistan. Arch. Pediatr. Adolesc. Med. 2012, 166, 1037–1044. [Google Scholar] [CrossRef] [PubMed]
- Cameron, L.; Shah, M.; Olivia, S. Impact Evaluation of a Large-Scale Rural Sanitation Project in Indonesia. The World Bank Sustainable Development Network Water and Sanitation Program Impact Evaluation Series No. 83. 2013. Available online: https://openknowledge.worldbank.org/bitstream/handle/10986/13166/wps6360.pdf?sequence=1&isAllowed=y (accessed on 1 January 2013).
- Caulfield, L.E.; de Onis, M.; Blössner, M.; Black, R.E. Undernutrition as an Underlying Cause of Child Deaths Associated with Diarrhea, Pneumonia, Malaria, and Measles. Am. J. Clin. Nutr. 2004, 80, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Dangour, A.D.; Watson, L.; Cumming, O.; Boisson, S.; Che, Y.; Velleman, Y.; Cavill, S.; Allen, E.; Uauy, R. Interventions to Improve Water Quality and Supply, Sanitation and Hygiene Practices, and Their Effects on the Nutritional Status of Children. Cochrane Database Syst. Rev. 2013, CD009382. [Google Scholar] [CrossRef] [PubMed]
- Dewey, K.G.; Begum, K. Long-Term Consequences of Stunting in Early Life. Matern. Child Nutr. 2011, 7, 5–18. [Google Scholar] [CrossRef]
- Dewey, K.G.; Mayers, D.R. Early Child Growth: How Do Nutrition and Infection Interact? Matern. Child Nutr. 2011, 7, 129–142. [Google Scholar] [CrossRef]
- FAO. Guidelines for Measuring Household and Individual Dietary Diversity; FAO: Roma, Italy, 2010. [Google Scholar]
- Fenn, B.; Bulti, A.T.; Nduna, T.; Duffield, A.; Watson, F. An Evaluation of an Operations Research Project to Reduce Childhood Stunting in a Food-Insecure Area in Ethiopia. Public Health Nutr. 2012, 15, 1746–1754. [Google Scholar] [CrossRef]
- Filmer, D.; Pritchett, L.H. Estimating Wealth Effects without Expenditure Data-or Tears: An Application to Educational Enrollments in States of India. Demography 2001, 38, 115–132. [Google Scholar]
- de Gier, B.; Pita-Rodríguez, G.M.; Campos-Ponce, M.; van de Bor, M.; Chamnan, C.; Junco-Díaz, R.; Doak, C.M.; Fiorentino, M.; Kuong, K.; Angel-Núñez, F.; et al. Soil-Transmitted Helminth Infections and Intestinal and Systemic Inflammation in Schoolchildren. Acta Trop. 2018, 182, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Guerrant, R.L.; Oriá, R.B.; Moore, S.R.; Oriá, M.O.; Lima, A.A. Malnutrition as an Enteric Infectious Disease with Long-Term Effects on Child Development. Nutr. Rev. 2008, 66, 487–505. [Google Scholar] [CrossRef] [PubMed]
- Hammer, J.; Spears, D. Evidence from a Randomized Experiment by the Maharashtra Government. The World Bank Sustainable Development Network Water and Sanitation Program. 2013. Available online: http://documents.worldbank.org/curated/en/443941468042021369/pdf/WPS6580.pdf (accessed on 1 August 2013).
- Langford, R.; Lunn, P.; Brick, C.P. Hand-Washing, Subclinical Infections, and Growth: A Longitudinal Evaluation of an Intervention in Nepali Slums. Am. J. Hum. Biol. 2011, 23, 621–629. [Google Scholar] [CrossRef] [PubMed]
- Leroy, J. ZSCORE06: Stata Module to Calculate Anthropometric z-Scores Using the 2006 WHO Child Growth Standards. Stat. Softw. Compon. 2011. Available online: https://econpapers.repec.org/software/bocbocode/s457279.htm (accessed on 27 April 2011).
- Luby, S.P.; Rahman, M.; Arnold, B.F.; Unicomb, L.; Ashraf, S.; Winch, P.J.; Stewart, C.P.; Begum, F.; Hussain, F.; Benjamin-Chung, J.; et al. Effects of Water Quality, Sanitation, Handwashing, and Nutritional Interventions on Diarrhoea and Child Growth in Rural Bangladesh: A Cluster Randomised Controlled Trial. Lancet Glob. Health 2018, 6, 302–317. [Google Scholar] [CrossRef]
- Martins, V.J.; Toledo Florêncio, T.M.; Grillo, L.P.; Do Carmo, P.F.; Martins, P.A.; Clemente, A.P.G.; Santos, C.D.; Vieira, M.D.F.A.; Sawaya, A.L. Long-Lasting Effects of Undernutrition. Int. J. Environ. Res. Public Health 2011, 8, 1817–1846. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Cambodia. Cambodia Demographic and Health Survey 2014. 2015. Available online: www.nis.gov.kh (accessed on 1 October 2017).
- National Institute of Statistics Ministry of Planning. Cambodia Socio-Economic Survey 2015, No. 1. 2015. Available online: www.nis.gov.kh/nis/CSES/Final Report CSES 2015.pdf (accessed on 17 October 2016).
- Null, C.; Stewart, C.P.; Pickering, A.J.; Dentz, H.N.; Arnold, B.F.; Arnold, C.D.; Benjamin-Chung, J.; Clasen, T.; Dewey, K.G.; Fernald, L.C.; et al. Effects of Water Quality, Sanitation, Handwashing, and Nutritional Interventions on Diarrhoea and Child Growth in Rural Kenya: A Cluster-Randomised Controlled Trial. Lancet Glob. Health 2018, 6, 316–329. [Google Scholar] [CrossRef]
- O’lorcain, P.; Holland, C.V. The Public Health Importance of Ascaris Lumbricoides. Parasitology 2000, 121, S51–S71. [Google Scholar] [CrossRef]
- Patil, S.R.; Arnold, B.F.; Salvatore, A.L.; Briceno, B.; Ganguly, S.; Colford, J.M.; Gertler, P.J. The Effect of India’s Total Sanitation Campaign on Defecation Behaviors and Child Health in Rural Madhya Pradesh: A Cluster Randomized Controlled Trial. PLoS Med. 2014, 11, e1001709. [Google Scholar] [CrossRef]
- Pickering, A.J.; Djebbari, H.; Lopez, C.; Coulibaly, M.; Alzua, M.L. Effect of a Community-Led Sanitation Intervention on Child Diarrhoea and Child Growth in Rural Mali: A Cluster-Randomised Controlled Trial. Lancet Glob. Health 2015, 3, e701–e711. [Google Scholar] [CrossRef]
- Sahiledengle, B. Prevalence and Associated Factors of Safe and Improved Infant and Young Children Stool Disposal in Ethiopia: Evidence from Demographic and Health Survey. BMC Public Health 2019, 19, 970. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. Improving Child Nutrition the Achievable Imperative for Global Progress. 2013. Available online: www.unicef.org/publications/index.html (accessed on 8 April 2013).
- Victora, C.G.; Adair, L.; Fall, C.; Hallal, P.C.; Martorell, R.; Richter, L.; Sachdev, H.S.; for the Maternal and Child Undernutrition Study Maternal and Child Undernutrition Study Group. Maternal and Child Undernutrition: Consequences for Adult Health and Human Capital. Lancet 2008, 371, 340–357. [Google Scholar] [CrossRef]
- WHO/UNICEF/World Bank Group. Levels and Trends in Child Malnutrition. 2018. Available online: www.who.int/nutgrowthdb/2018-jme-brochure.pdf (accessed on 17 August 2018).
- WHO/UNICEF. Joint Monitoring Programme for Water Supply, Sanitation and Hygiene. 2017. Available online: https://washdata.org/ (accessed on 17 August 2018).
- Joint Monitoring Programme Methodology 2017 Update. 2017. Available online: https://washdata.org/sites/default/files/documents/reports/2018-04/JMP-2017-update-methodology.pdf (accessed on 17 October 2014).
- Joint Monitoring Programme Progress on Drinking Water, Sanitation and Hygiene. 2017. Available online: https://doi.org/10.1111/tmi.12329 (accessed on 27 April 2011).
- WHO. WHO Child Growth Standards Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age Methods and Development Department of Nutrition for Health and Development. 2006. Available online: http://www.who.int/childgrowth/standards/Technical_report.pdf (accessed on 17 August 2018).
- World Health Organization. WHA Global Nutrition Targets 2025: Stunting Policy Brief; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Cambodia Malaria Profile. 2017. Available online: http://www.who.int/malaria/publications/country-profiles/profile_khm_en.pdf (accessed on 17 August 2018).
- Wieringa, F.; Gauthier, L.; Greffeuille, V.; Som, S.; Dijkhuizen, M.; Laillou, A.; Chamnan, C.; Berger, J.; Poirot, E. Identification of Acute Malnutrition in Children in Cambodia Requires Both Mid Upper Arm Circumference and Weight-For-Height to Offset Gender Bias of Each Indicator. Nutrients 2018, 10, 786. [Google Scholar] [CrossRef] [PubMed]
| Baseline | Follow-Up 2 | Follow-Up 3 | |
|---|---|---|---|
| Female | 2654/5310 (50%) | 2654/5310 (50%) | 2654/5310 (50%) |
| Age of study population (months) 1 | 11.8 ± 7 | 16.2 ± 8.5 | 19.8 ± 8.9 |
| WHZ of study population 1 | −0.8 ± 1.1 | −0.7 ± 1 | −0.8 ± 1 |
| Normal | 3719/4343 (85.6%) | 3148/3441 (91.5%) | 3052/3357 (90.9%) |
| Wasted (WHZ < –2 SD) | 624/4343 (14.4%) | 293/3441 (8.5%) | 305/3357 (9.1%) |
| MUAC of study population (6.0–59.9 months) 1 | 13.8 ± 1.2 | 14 ± 1.1 | 14.1 ± 1.1 |
| Normal | 2914/3239 (90%) | 2786/2981 (93.5%) | 2969/3149 (94.3%) |
| Wasted (MUAC < 125 mm) | 325/3239 (10%) | 195/2981 (6.5%) | 180/3149 (5.7%) |
| HAZ of study population 1 | −1 ± 1.3 | −1.3 ± 1.1 | −1.4 ± 1.1 |
| Normal | 3515/4351 (80.8%) | 2552/3445 (74.1%) | 2397/3358 (71.4%) |
| Stunted (HAZ < –2SD) | 836/4351 (19.2%) | 893/3445 (25.9%) | 961/3358 (28.6%) |
| Weight-for-Height z-Score | |||||||||
| Crude Analyses | Adjusted Analyses (JMP-CS) | Adjusted Analyses (National-CS) | |||||||
| Estimate | 95% CI | p-Value | Estimate | 95% CI | p-Value | Estimate | 95% CI | p-Value | |
| JMP-CS composite score | 0.28 | 0.18–0.38 | <0.001 | 0.14 | 0.01–0.27 | 0.03 | |||
| National-CS composite score | 0.55 | 0.4–0.69 | <0.001 | 0.4 | 0.2–0.58 | <0.001 | |||
| Gender | |||||||||
| Male | ref. | ||||||||
| Female | 0.06 | 0.002–0.11 | 0.04 | 0.06 | 0.004–0.12 | 0.051 | 0.08 | 0.01–0.15 | 0.021 |
| Age | −0.016 | −0.02–−0.012 | <0.001 | −0.028 | −0.03–−0.02 | <0.001 | −0.028 | −0.03–−0.02 | <0.001 |
| Exclusive breastfeeding | |||||||||
| Exclusive breastfeeding | ref. | ||||||||
| Other food/drinks | −0.27 | −0.33–0.21 | <0.001 | −0.35 | −0.43–0.27 | <0.001 | −0.35 | −0.45–0.25 | <0.001 |
| Dietary diversity intake | −0.02 | −0.03–−0.007 | 0.001 | 0.01 | −0.006–0.02 | 0.268 | 0.01 | −0.01–0.02 | 0.516 |
| Mother education | |||||||||
| No-low education | ref. | ||||||||
| Higher education | 0.22 | 0.16–0.28 | <0.001 | 0.1 | 0.04–0.18 | 0.001 | 0.1 | 0.001–0.15 | 0.052 |
| Wealth index | 0.14 | 0.12–0.16 | <0.001 | 0.09 | 0.07–0.12 | <0.001 | 0.1 | 0.07–0.12 | <0.001 |
| Province | |||||||||
| Phnom Penh | ref. | ||||||||
| Kratie | −0.4 | −0.5–0.34 | <0.001 | −0.31 | −0.4–0.22 | <0.001 | −0.24 | −0.34–0.14 | <0.001 |
| Ratanakiri | −0.35 | −0.4–0.3 | <0.001 | −0.16 | −0.25–0.06 | 0.001 | −0.07 | −0.17–0.04 | 0.234 |
| Mid-Upper Arm Circumference | |||||||||
| Crude analyses | Adjusted analyses (JMP-CS) | Adjusted analyses (National-CS) | |||||||
| Estimate | 95% CI | p-value | Estimate | 95% CI | p-value | Estimate | 95% CI | p-value | |
| JMP-CS composite score | 0.54 | 0.43–0.65 | <0.001 | 0.18 | 0.04–0.31 | 0.013 | |||
| National-CS composite score | 0.95 | 0.78–1.12 | <0.001 | 0.4 | 0.16–0.58 | 0.001 | |||
| Gender | |||||||||
| Male | ref. | ||||||||
| Female | −0.36 | −0.42–0.29 | <0.001 | −0.39 | −0.45–−0.32 | <0.001 | −0.39 | −0.46–0.31 | <0.001 |
| Age | 0.04 | 0.037–0.05 | <0.001 | 0.02 | 0.017–0.03 | <0.001 | 0.02 | 0.016–0.3 | <0.001 |
| Exclusive breastfeeding | |||||||||
| Exclusive breastfeeding | ref. | ||||||||
| Other food/drinks | 0.61 | 0.54–0.68 | <0.001 | 0.55 | 0.46–0.63 | <0.001 | 0.51 | 0.4–0.6 | <0.001 |
| Dietary diversity intake | 0.07 | 0.05–0.08 | <0.001 | 0.02 | 0.002–0.03 | 0.027 | 0.01 | −0.003–0.03 | 0.102 |
| Mother education | |||||||||
| No-low education | ref. | ||||||||
| Higher education | 0.33 | 0.27–0.4 | <0.001 | 0.14 | 0.06–0.21 | <0.001 | 0.1 | 0.03–0.2 | 0.008 |
| Wealth index | 0.19 | 0.17–0.22 | <0.001 | 0.1 | 0.08–0.14 | <0.001 | 0.1 | 0.08–0.14 | <0.001 |
| Province | |||||||||
| Phnom Penh | ref. | ||||||||
| Kratie | −0.52 | −0.6–0.45 | <0.001 | −0.28 | −0.37–0.18 | <0.001 | −0.24 | −0.35–0.13 | <0.001 |
| Ratanakiri | −0.65 | −0.73–0.58 | <0.001 | −0.38 | −0.48–0.28 | <0.001 | −0.31 | −0.43–0.2 | <0.001 |
| Height-for-Age Z-Score | |||||||||
| Crude Analyses | Adjusted Analyses (JMP-CS) | Adjusted Analyses (National-CS) | |||||||
| Estimate | 95% CI | p-Value | Estimate | 95% CI | p-Value | Estimate | 95% CI | p-Value | |
| JMP-CS composite score | 0.21 | 0.13–0.29 | <0.001 | 0.15 | 0.04–0.25 | 0.006 | |||
| National-CS composite score | 0.35 | 0.22–0.47 | <0.001 | 0.15 | −0.02–0.32 | 0.081 | |||
| Gender | |||||||||
| Male | ref. | ||||||||
| Female | 0.1 | 0.04–0.17 | 0.002 | 0.12 | 0.5–0.18 | 0.001 | 0.11 | 0.03–0.19 | 0.004 |
| Age | −0.025 | −0.03–-0.02 | <0.001 | −0.03 | −0.04–−0.029 | <0.001 | −0.038 | −0.04–−0.03 | <0.001 |
| Exclusive breastfeeding | |||||||||
| Exclusive breastfeeding | ref. | ||||||||
| Other food/drinks | −0.18 | −0.23–−0.12 | <0.001 | −0.07 | −0.13–0.003 | 0.04 | −0.11 | −0.2–-0.03 | 0.009 |
| Dietary diversity intake | −0.02 | −0.03–−0.008 | <0.001 | −0.01 | −0.02–−0.003 | 0.012 | −0.01 | −0.02–0.004 | 0.173 |
| Mother education | |||||||||
| No-low education | ref. | ||||||||
| Higher education | 0.4 | 0.33–0.47 | <0.001 | 0.18 | 0.1–0.26 | <0.001 | 0.17 | 0.09–0.26 | <0.001 |
| Wealth index | 0.19 | 0.16–0.2 | <0.001 | 0.13 | 0.1–0.16 | <0.001 | 0.13 | 0.09–0.16 | <0.001 |
| Province | |||||||||
| Phnom Penh | ref. | ||||||||
| Kratie | −0.41 | −0.49–−0.34 | <0.001 | −0.14 | −0.24–−0.04 | 0.007 | −0.16 | −0.26–-0.05 | 0.005 |
| Ratanakiri | −0.62 | −0.7–−0.54 | <0.001 | −0.36 | −0.46–−0.26 | <0.001 | −0.37 | −0.49–-0.25 | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manzoni, G.; Laillou, A.; Samnang, C.; Hong, R.; Wieringa, F.T.; Berger, J.; Poirot, E.; Checchi, F. Child-Sensitive WASH Composite Score and the Nutritional Status in Cambodian Children. Nutrients 2019, 11, 2142. https://doi.org/10.3390/nu11092142
Manzoni G, Laillou A, Samnang C, Hong R, Wieringa FT, Berger J, Poirot E, Checchi F. Child-Sensitive WASH Composite Score and the Nutritional Status in Cambodian Children. Nutrients. 2019; 11(9):2142. https://doi.org/10.3390/nu11092142
Chicago/Turabian StyleManzoni, Giulia, Arnaud Laillou, Chea Samnang, Rathmony Hong, Frank T. Wieringa, Jacques Berger, Etienne Poirot, and Francesco Checchi. 2019. "Child-Sensitive WASH Composite Score and the Nutritional Status in Cambodian Children" Nutrients 11, no. 9: 2142. https://doi.org/10.3390/nu11092142
APA StyleManzoni, G., Laillou, A., Samnang, C., Hong, R., Wieringa, F. T., Berger, J., Poirot, E., & Checchi, F. (2019). Child-Sensitive WASH Composite Score and the Nutritional Status in Cambodian Children. Nutrients, 11(9), 2142. https://doi.org/10.3390/nu11092142





