Systematic Review with Meta-Analysis: Lactobacillus reuteri DSM 17938 for Treating Acute Gastroenteritis in Children. An Update
Abstract
1. Introduction
2. Material and Methods
2.1. Inclusion Criteria for This Review
2.2. Search Methods for Identification of Studies
2.3. Collection of Data and Analysis
2.4. Assessment of Risk of Bias in Included Studies
2.5. Dealing with Missing Data
2.6. Assessment of Heterogeneity and of Reporting Biases
2.7. Data Synthesis (Statistical Methods)
2.8. Certainty of Evidence
3. Results
3.1. Risk of Bias in Included Studies
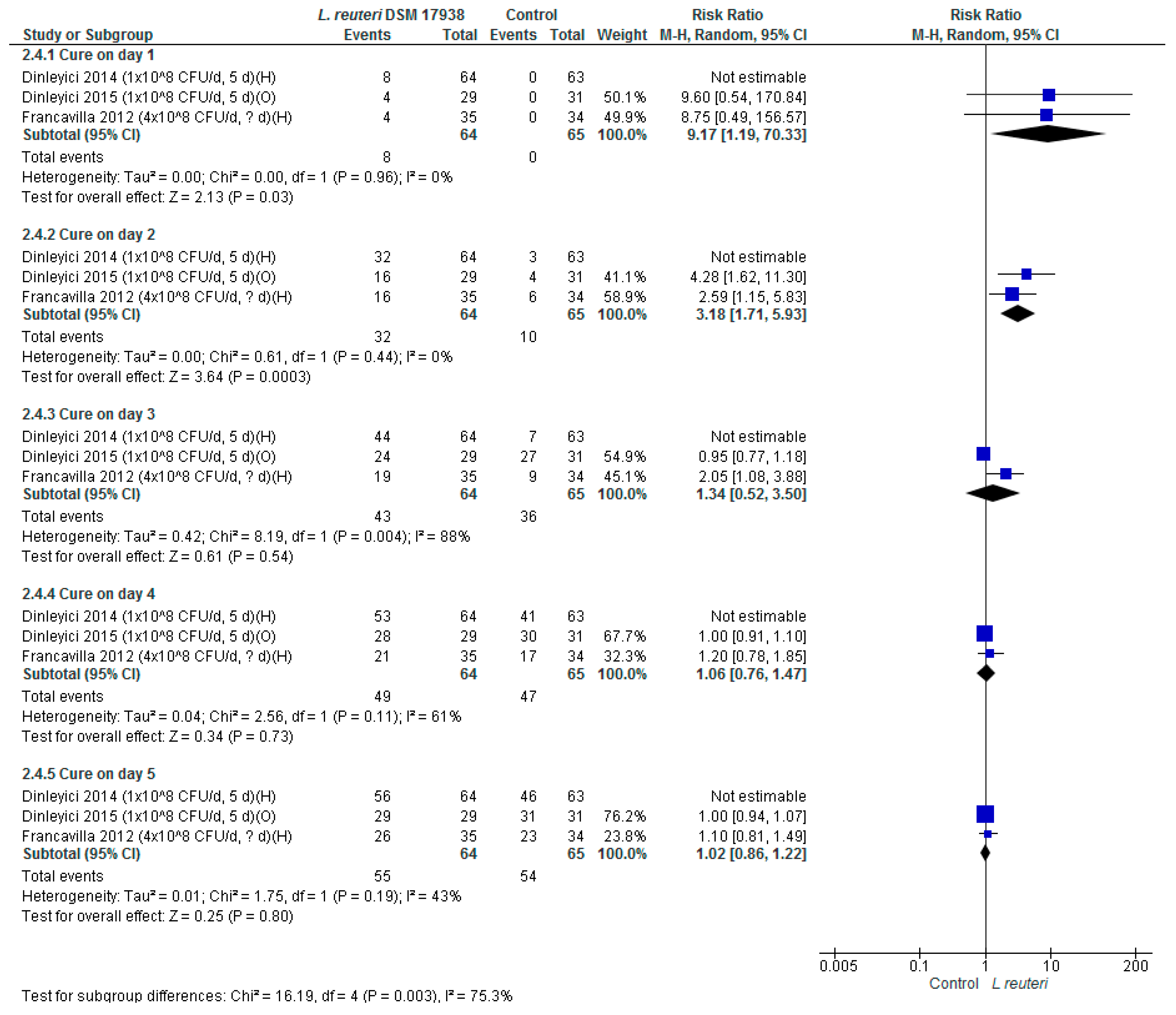
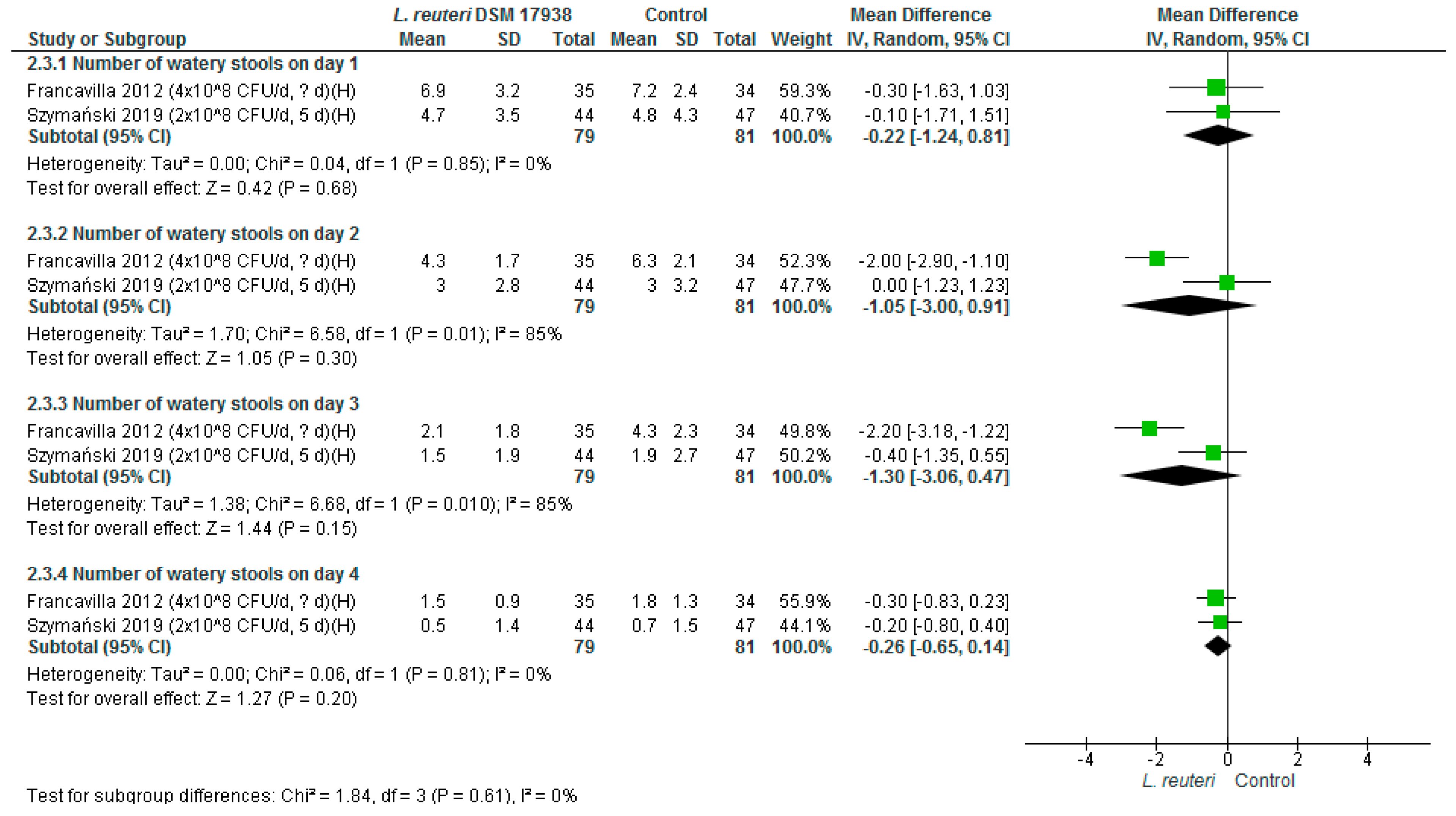
3.2. Main Effects
3.3. Subgroup and Sensitivity Analyses
3.4. Certainty of Evidence
4. Discussion
4.1. Principle Findings
4.2. Strengths and Limitations
4.3. Agreement and Disagreement with Other Studies or Reviews
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- GBD Diarrhoeal Disease Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis. 2018, 18, 1211–1228. [Google Scholar] [CrossRef]
- Barker, S.F.; Zomer, E.; O’Toole, J.; Sinclair, M.; Gibney, K.; Liew, D.; Leder, K. Cost of gastroenteritis in Australia: A healthcare perspective. PLoS ONE 2018, 13, e0195759. [Google Scholar] [CrossRef] [PubMed]
- Guarino, A.; Ashkenazi, S.; Gendrel, D.; Lo Vecchio, A.; Shamir, R.; Szajewska, H. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition/European Society for Pediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe: Update 2014. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 132–152. [Google Scholar] [CrossRef] [PubMed]
- Rosander, A.; Connolly, E.; Roos, S. Removal of antibiotic resistance gene-carrying plasmids from Lactobacillus reuteri ATCC 55730 and characterization of the resulting daughter strain, L. reuteri DSM 17938. Appl. Environ. Microbiol. 2008, 74, 6032–6040. [Google Scholar] [CrossRef] [PubMed]
- Mu, Q.; Tavella, V.J.; Luo, X.M. Role of Lactobacillus reuteri in Human Health and Diseases. Front. Microbiol. 2018, 9, 757. [Google Scholar] [CrossRef] [PubMed]
- Urbanska, M.; Gieruszczak-Bialek, D.; Szajewska, H. Systematic review with meta-analysis: Lactobacillus reuteri DSM 17938 for diarrhoeal diseases in children. Aliment. Pharmacol. Ther. 2016, 43, 1025–1034. [Google Scholar] [CrossRef]
- Dinleyici, E.C.; Vandenplas, Y. Lactobacillus reuteri DSM 17938 effectively reduces the duration of acute diarrhoea in hospitalised children. Acta Paediatr. 2014, 103, e300–e305. [Google Scholar] [CrossRef]
- Dinleyici, E.C.; Dalgic, N.; Guven, S.; Metin, O.; Yasa, O.; Kurugol, Z.; Turel, O.; Tanir, G.; Yazar, A.S.; Arica, V.; et al. Lactobacillus reuteri DSM 17938 shortens acute infectious diarrhea in a pediatric outpatient setting. Jornal Pediatria (Versão Português) 2015, 91, 392–396. [Google Scholar] [CrossRef]
- Francavilla, R.; Lionetti, E.; Castellaneta, S.; Ciruzzi, F.; Indrio, F.; Masciale, A.; Fontana, C.; La Rosa, M.M.; Cavallo, L.; Francavilla, A. Randomised clinical trial: Lactobacillus reuteri DSM 17938 vs. placebo in children with acute diarrhea—A double-blind study. Aliment. Pharmacol. Ther. 2012, 36, 363–369. [Google Scholar] [CrossRef]
- Schnadower, D.; Tarr, P.I.; Casper, T.C.; Gorelick, M.H.; Dean, J.M.; O’Connell, K.J.; Mahajan, P.; Levine, A.C.; Bhatt, S.R.; Roskind, C.G.; et al. Lactobacillus rhamnosus GG versus Placebo for Acute Gastroenteritis in Children. N. Engl. J. Med. 2018, 379, 2002–2014. [Google Scholar] [CrossRef]
- Freedman, S.B.; Williamson-Urquhart, S.; Farion, K.J.; Gouin, S.; Willan, A.R.; Poonai, N.; Hurley, K.; Sherman, P.M.; Finkelstein, Y.; Lee, B.E.; et al. Multicenter Trial of a Combination Probiotic for Children with Gastroenteritis. N. Engl. J. Med. 2018, 379, 2015–2026. [Google Scholar] [CrossRef] [PubMed]
- Szymanski, H.; Szajewska, H. Lack of Efficacy of Lactobacillus reuteri DSM 17938 for the Treatment of Acute Gastroenteritis: A Randomized Controlled Trial. Pediatr. Infect. Dis. J. 2019, 38, e237–e242. [Google Scholar] [CrossRef] [PubMed]
- Szajewska, H.; Guarino, A.; Hojsak, I.; Indrio, F.; Kolacek, S.; Shamir, R.; Vandenplas, Y.; Weizman, Z. Use of probiotics for management of acute gastroenteritis: A position paper by the ESPGHAN Working Group for Probiotics and Prebiotics. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schunemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Ruzhentsova, T.A.; Ploskireva, A.A.; Popova, R.V.; Nuribekov, S.A.; Gorelov, A.V. Optimization of Pathogenetic Therapy of Acute Intestinal Infections in Children: Results of a Randomised Trial. Infect. Dis. 2018, 1670–1676. [Google Scholar] [CrossRef]
- Szajewska, H.; Urbanska, M.; Chmielewska, A.; Weizman, Z.; Shamir, R. Meta-analysis: Lactobacillus reuteri strain DSM 17938 (and the original strain ATCC 55730) for treating acute gastroenteritis in children. Benef. Microbes 2014, 5, 285–293. [Google Scholar] [CrossRef]
- Ahmadi, E.; Alizadeh-Navaei, R.; Rezai, M.S. Efficacy of probiotic use in acute rotavirus diarrhea in children: A systematic review and meta-analysis. Casp. J. Intern. Med. 2015, 6, 187–195. [Google Scholar]
- Allen, S.J.; Martinez, E.G.; Gregorio, G.V.; Dans, L.F. Probiotics for treating acute infectious diarrhoea. Cochrane Database Syst. Rev. 2010. [Google Scholar] [CrossRef]
- Applegate, J.A.; Fischer Walker, C.L.; Ambikapathi, R.; Black, R.E. Systematic review of probiotics for the treatment of community-acquired acute diarrhea in children. BMC Public Health 2013, 13 (Suppl. 3), S16. [Google Scholar] [CrossRef] [PubMed]
- Florez, I.D.; Veroniki, A.A.; Al Khalifah, R.; Yepes-Nunez, J.J.; Sierra, J.M.; Vernooij, R.W.M.; Acosta-Reyes, J.; Granados, C.M.; Perez-Gaxiola, G.; Cuello-Garcia, C.; et al. Comparative effectiveness and safety of interventions for acute diarrhea and gastroenteritis in children: A systematic review and network meta-analysis. PLoS ONE 2018, 13, e0207701. [Google Scholar] [CrossRef] [PubMed]
- Freedman, S.B.; Pasichnyk, D.; Black, K.J.; Fitzpatrick, E.; Gouin, S.; Milne, A.; Hartling, L. Gastroenteritis Therapies in Developed Countries: Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0128754. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez-Castrellon, P.; Ortiz-Hernandez, A.A.; Llamosas-Gallardo, B.; Acosta-Bastidas, M.A.; Jimenez-Gutierrez, C.; Diaz-Garcia, L.; Anzo-Osorio, A.; Estevez-Jimenez, J.; Jimenez-Escobar, I.; Vidal-Vazquez, R.P. Efficacy of racecadotril vs. smectite, probiotics or zinc as an integral part of treatment of acute diarrhea in children under five years: A meta-analysis of multiple treatments. Gac. Med. Mex. 2015, 151, 329–337. [Google Scholar] [PubMed]
- Salari, P.; Nikfar, S.; Abdollahi, M. A meta-analysis and systematic review on the effect of probiotics in acute diarrhea. Inflamm. Allergy Drug Targets 2012, 11, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Sniffen, J.C.; McFarland, L.V.; Evans, C.T.; Goldstein, E.J.C. Choosing an appropriate probiotic product for your patient: An evidence-based practical guide. PLoS ONE 2018, 13, e0209205. [Google Scholar] [CrossRef]
- Szajewska, H.; Kolodziej, M.; Gieruszczak-Bialek, D.; Skorka, A.; Ruszczynski, M.; Shamir, R. Systematic review with meta-analysis: Lactobacillus rhamnosus GG for treating acute gastroenteritis in children—A 2019 update. Aliment. Pharmacol. Ther. 2019, 49, 1376–1384. [Google Scholar] [CrossRef]
- Schnadower, D.; Tarr, P.I.; Freedman, S.B. Letter: Lactobacillus rhamnosus GG offers no benefit over placebo in children with acute gastroenteritis. Aliment. Pharmacol. Ther. 2019, 50, 620–622. [Google Scholar] [CrossRef]
- Dinleyici, E.C.; Kara, A.; Ozen, M.; Vandenplas, Y. Saccharomyces boulardii CNCM I-745 in different clinical conditions. Expert Opin. Biol. Ther. 2014, 14, 1593–1609. [Google Scholar] [CrossRef]
- Feizizadeh, S.; Salehi-Abargouei, A.; Akbari, V. Efficacy and safety of Saccharomyces boulardii for acute diarrhea. Pediatrics 2014, 134, e176–e191. [Google Scholar] [CrossRef]
- Padayachee, M.; Visser, J.; Viljoen, E.; Musekiwa, A.; Blaauw, R. Efficacy and safety of Saccharomyces boulardii in the treatment of acute gastroenteritis in the paediatric population: A systematic review. S. Afr. J. Clin. Nutr. 2019, 32, 58–69. [Google Scholar] [CrossRef]
- Ianiro, G.; Rizzatti, G.; Plomer, M.; Lopetuso, L.; Scaldaferri, F.; Franceschi, F.; Cammarota, G.; Gasbarrini, A. Bacillus clausii for the Treatment of Acute Diarrhea in Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2018, 10, 1074. [Google Scholar] [CrossRef] [PubMed]
- Tlaskal, P.; Schramlova, J.; Kokesova, A.; Adamus, J.; Bubakova, D.; Kocnarova, N.; Kopecka, K.; Muckova, M.; Pacovska, J.; Sladkova, E. Probiotics in the treatment of diarrheal disease of viral etiology in children. NAFAS 2005, 3, 25–28. [Google Scholar]
- Hegar, B.; Waspada, I.M.; Gunardi, H.; Vandenplas, Y. A double blind randomized trial showing probiotics to be ineffective in acute diarrhea in Indonesian children. Indian J. Pediatr. 2015, 82, 410–414. [Google Scholar] [CrossRef]
- Freedman, S.B.; Sherman, P.M.; Willan, A.; Johnson, D.; Gouin, S.; Schuh, S.; Pediatric Emergency Research Canada. Emergency Department Treatment of Children with Diarrhea Who Attend Day Care: A Randomized Multidose Trial of a Lactobacillus helveticus and Lactobacillus rhamnosus Combination Probiotic. Clin. Pediatr. 2015, 54, 1158–1166. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeldt, V.; Michaelsen, K.F.; Jakobsen, M.; Larsen, C.N.; Moller, P.L.; Pedersen, P.; Tvede, M.; Weyrehter, H.; Valerius, N.H.; Paerregaard, A. Effect of probiotic Lactobacillus strains in young children hospitalized with acute diarrhea. Pediatr. Infect. Dis. J. 2002, 21, 411–416. [Google Scholar] [CrossRef]
- Rosenfeldt, V.; Michaelsen, K.F.; Jakobsen, M.; Larsen, C.N.; Moller, P.L.; Tvede, M.; Weyrehter, H.; Valerius, N.H.; Paerregaard, A. Effect of probiotic Lactobacillus strains on acute diarrhea in a cohort of nonhospitalized children attending day-care centers. Pediatr. Infect. Dis. J. 2002, 21, 417–419. [Google Scholar] [CrossRef]
- Huang, Y.F.; Liu, P.Y.; Chen, Y.Y.; Nong, B.R.; Huang, I.F.; Hsieh, K.S.; Chen, K.T. Three-combination probiotics therapy in children with salmonella and rotavirus gastroenteritis. J. Clin. Gastroenterol. 2014, 48, 37–42. [Google Scholar] [CrossRef]
- Chen, C.C.; Kong, M.S.; Lai, M.W.; Chao, H.C.; Chang, K.W.; Chen, S.Y.; Huang, Y.C.; Chiu, C.H.; Li, W.C.; Lin, P.Y.; et al. Probiotics have clinical, microbiologic, and immunologic efficacy in acute infectious diarrhea. Pediatr. Infect. Dis J. 2010, 29, 135–138. [Google Scholar] [CrossRef]
- Athalye-Jape, G.; Rao, S.; Patole, S. Lactobacillus reuteri DSM 17938 as a Probiotic for Preterm Neonates: A Strain-Specific Systematic Review. JPEN J. Parenter. Enter. Nutr. 2016, 40, 783–794. [Google Scholar] [CrossRef]

| Study ID; Country | Participants (Exp/Cont) | Intervention— L. reuteri DSM 17938 (Dose; Duration) | Comparison | Inclusion Criteria | Sample Size Calculation | Funding | |
|---|---|---|---|---|---|---|---|
| Treatment of Acute Gastroenteritis | |||||||
| 1. | Dinleyici 2014; Turkey | 64/63 | 1 × 108 CFU; 5 days | No intervention | 3–60 months; acute diarrhea (no definition) lasting 12–72 h; mild to moderate dehydration; hospitalization | Yes | The study was not funded (except for the free medication) |
| 2. | Dinleyici 2015; Turkey | 29/31 | 1 × 108 CFU; 5 days | No intervention | 3–60 months; acute diarrhea (≥3 loose or watery stools per 24 h) lasting 12–72 h; outpatients | Yes | Not described |
| 3. | Francavilla 2012; Italy | 35/34 | 4 × 108 CFU; 7 days | Placebo (mixture of sunflower oil and medium-chain triglyceride oil) | Age 6–36 months; acute diarrhea (≥2 or watery stools per 24 h) of no more than 7 days duration; mild to moderate dehydration; hospitalization | Yes | Not described |
| 4. | Szymański 2019; Poland | 44/47 | 2 × 108 CFU; 5 days | Placebo | Age < 5 years; acute gastroenteritis (a change in stool consistency to a loose or liquid form [according to the BSF scale, or, in the case of infants, the ASF scale] and/or an increase in the frequency of evacuations, typically ≥ 3 in 24 h), lasting no longer than 5 days. | Yes | BioGaia provided the study products. The study received no external funding. |
| Patient or Population: Acute Gastroenteritis in Children Setting: Intervention: Lactobacillus reuteri DSM 17938 Comparison: Placebo/No Treatment | ||||||
|---|---|---|---|---|---|---|
| Outcomes | Anticipated Absolute Effects * (95% CI) | Relative Effect (95% CI) | № of Participants (Studies) | Certainty of the Evidence (GRADE) | Comments | |
| Risk With Placebo/No Treatment | Risk With Lactobacillus Reuteri DSM 17938 | |||||
| Lactobacillus reuteri DSM 17938 vs control. Duration of diarrhea (days) | The mean lactobacillus reuteri DSM 17938 vs control. Duration of diarrhea (days) ranged from 0.64 to 2.34 days | MD 0.87 days lower (1.43 lower to 0.31 lower) | - | 347 (4 RCTs) | ⨁◯◯◯ VERY LOW a,b,c,d | |
| Lactobacillus reuteri DSM 17938 vs. control. Duration of hospitalization | The mean lactobacillus reuteri DSM 17938 vs. control. Duration of hospitalization ranged from 2.55 to 5.46 days | MD 0.54 days lower (1.09 lower to 0) | - | 284 (3 RCTs) | ⨁◯◯◯ VERY LOW d,e,f,g | |
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patro-Gołąb, B.; Szajewska, H. Systematic Review with Meta-Analysis: Lactobacillus reuteri DSM 17938 for Treating Acute Gastroenteritis in Children. An Update. Nutrients 2019, 11, 2762. https://doi.org/10.3390/nu11112762
Patro-Gołąb B, Szajewska H. Systematic Review with Meta-Analysis: Lactobacillus reuteri DSM 17938 for Treating Acute Gastroenteritis in Children. An Update. Nutrients. 2019; 11(11):2762. https://doi.org/10.3390/nu11112762
Chicago/Turabian StylePatro-Gołąb, Bernadeta, and Hania Szajewska. 2019. "Systematic Review with Meta-Analysis: Lactobacillus reuteri DSM 17938 for Treating Acute Gastroenteritis in Children. An Update" Nutrients 11, no. 11: 2762. https://doi.org/10.3390/nu11112762
APA StylePatro-Gołąb, B., & Szajewska, H. (2019). Systematic Review with Meta-Analysis: Lactobacillus reuteri DSM 17938 for Treating Acute Gastroenteritis in Children. An Update. Nutrients, 11(11), 2762. https://doi.org/10.3390/nu11112762





