Oily Fish Consumption and the Risk of Dyslipidemia in Korean Adults: A Prospective Cohort Study Based on the Health Examinees Gem (HEXA-G) Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Diet Assessment
2.3. Definition of Dyslipidemia
2.4. Assessment of Other Variables
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Orho-Melander, M. Genetics of coronary heart disease: Towards causal mechanisms, novel drug targets and more personalized prevention. J. Intern. Med. 2015, 278, 433–446. [Google Scholar] [CrossRef] [PubMed]
- National Cholesterol Education Program. Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar] [CrossRef]
- Tóth, P.P.; Potter, D.; Ming, E.E. Prevalence of lipid abnormalities in the united states: The national health and nutrition examination survey 2003–2006. J. Clin. Lipidol. 2012, 6, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.H.; Kim, H.C.; Ahn, S.V.; Hur, N.W.; Choi, D.P.; Park, C.G.; Suh, I. Prevalence of dyslipidemia among Korean adults: Korea national health and nutrition survey 1998–2005. Diabetes Metab. J. 2012, 36, 43–55. [Google Scholar] [CrossRef]
- Ference, B.A.; Ginsberg, H.N.; Graham, I.; Ray, K.K.; Packard, C.J.; Bruckert, E.; Watts, G.F.; Boren, J.; Fazio, S.; Horton, J.D.; et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2017, 38, 2459–2472. [Google Scholar] [CrossRef]
- Nordestgaard, B.G.; Varbo, A. Triglycerides and cardiovascular disease. Lancet 2014, 384, 626–635. [Google Scholar] [CrossRef]
- Ooi, E.M.; Ng, T.W.; Watts, G.F.; Barrett, P.H. Dietary fatty acids and lipoprotein metabolism: New insights and updates. Curr. Opin. Lipidol. 2013, 24, 192–197. [Google Scholar] [CrossRef]
- Rimm, E.B.; Appel, L.J.; Chiuve, S.E.; Djoussé, L.; Engler, M.B.; Kris-Etherton, P.M.; Mozaffarian, D.; Siscovick, D.S.; Lichtenstein, A.H. Seafood long-chain n-3 polyunsaturated fatty acids and cardiovascular disease: A science advisory from the American Heart Association. Circulation 2018, 138, e35–e47. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Wu, J.H. Omega-3 fatty acids and cardiovascular disease: Effects on risk factors, molecular pathways, and clinical events. J. Am. Coll. Cardiol. 2011, 58, 2047–2067. [Google Scholar] [CrossRef]
- Ebbesson, S.O.; Tejero, M.E.; Nobmann, E.D.; Lopez-Alvarenga, J.C.; Ebbesson, L.; Romenesko, T.; Carter, E.A.; Resnick, H.E.; Devereux, R.B.; MacCluer, J.W.; et al. Fatty acid consumption and metabolic syndrome components: The gocadan study. J. Cardiometab. Syndr. 2007, 2, 244–249. [Google Scholar] [CrossRef]
- Xun, P.; Hou, N.; Daviglus, M.; Liu, K.; Morris, J.S.; Shikany, J.M.; Sidney, S.; Jacobs, D.R.; He, K. Fish oil, selenium and mercury in relation to incidence of hypertension: A 20-year follow-up study. J. Intern. Med. 2011, 270, 175–186. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Song, Y.; Ford, E.S.; Manson, J.E.; Buring, J.E.; Ridker, P.M. Dietary calcium, vitamin d, and the prevalence of metabolic syndrome in middle-aged and older U.S. Women. Diabetes Care 2005, 28, 2926–2932. [Google Scholar] [CrossRef]
- Wang, L.; Manson, J.E.; Buring, J.E.; Lee, I.M.; Sesso, H.D. Dietary intake of dairy products, calcium, and vitamin d and the risk of hypertension in middle-aged and older women. Hypertension 2008, 51, 1073–1079. [Google Scholar] [CrossRef] [PubMed]
- Korea Rural Economic Institute. 2013 Food Balance Sheet. Available online: https://www.krei.re.kr/web/www/23?p_p_id=EXT_BBS&p_p_lifecycle=0&p_p_state=normal&p_p_mode=view&_EXT_BBS_struts_action=%2Fext%2Fbbs%2Fview_message&_EXT_BBS_messageId=404443 (accessed on 20 April 2016).
- Health Examinees Study Group. The Health Examinees (HEXA) study: Rationale, study design and baseline characteristics. Asian Pac. J. Cancer Prev. APJCP 2015, 16, 1591. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Han, B.-G.; Group, K. Cohort profile: The Korean genome and epidemiology study (KoGES) consortium. Int. J. Epidemiol. 2016, 46, e20. [Google Scholar] [CrossRef]
- Shin, S.; Lee, H.-W.; Kim, C.; Lim, J.; Lee, J.-K.; Lee, S.-A.; Kang, D. Egg consumption and risk of metabolic syndrome in Korean adults: Results from the Health Examinees Study. Nutrients 2017, 9, 687. [Google Scholar] [CrossRef] [PubMed]
- International Obesity Task Force; World Health Organization. The Asian-Pacific Perspective: Redefining Obesity and its Treatment; Health Communications Australia: Melbourne, Australia, 2000. [Google Scholar]
- Wang, F.; Wang, Y.; Zhu, Y.; Liu, X.; Xia, H.; Yang, X.; Sun, G. Treatment for 6 months with fish oil-derived n-3 polyunsaturated fatty acids has neutral effects on glycemic control but improves dyslipidemia in type 2 diabetic patients with abdominal obesity: A randomized, double-blind, placebo-controlled trial. Eur. J. Nutr. 2017, 56, 2415–2422. [Google Scholar] [CrossRef]
- Petersen, M.; Pedersen, H.; Major-Pedersen, A.; Jensen, T.; Marckmann, P. Effect of fish oil versus corn oil supplementation on LDL and HDL subclasses in type 2 diabetic patients. Diabetes Care 2002, 25, 1704–1708. [Google Scholar] [CrossRef]
- Harris, W.S.; Connor, W.E.; Illingworth, D.R.; Rothrock, D.W.; Foster, D.M. Effects of fish oil on VLDL triglyceride kinetics in humans. J. Lipid Res. 1990, 31, 1549–1558. [Google Scholar]
- Goldberg, R.B.; Sabharwal, A.K. Fish oil in the treatment of dyslipidemia. Curr. Opin. Endocrinol. Diabetes Obes. 2008, 15, 167–174. [Google Scholar] [CrossRef]
- Klop, B.; Elte, J.; Cabezas, M. Dyslipidemia in obesity: Mechanisms and potential targets. Nutrients 2013, 5, 1218–1240. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, J.C.; Crook, D.; Godsland, I.F. Influence of age and menopause on serum lipids and lipoproteins in healthy women. Atherosclerosis 1993, 98, 83–90. [Google Scholar] [CrossRef]
- Carpentier, Y.A.; Portois, L.; Malaisse, W.J. n−3 Fatty acids and the metabolic syndrome. Am. J. Clin. Nutr. 2006, 83, 1499S–1504S. [Google Scholar] [CrossRef] [PubMed]
- Eslick, G.D.; Howe, P.R.; Smith, C.; Priest, R.; Bensoussan, A. Benefits of fish oil supplementation in hyperlipidemia: A systematic review and meta-analysis. Int. J. Cardiol. 2009, 136, 4–16. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, C.; Li, L.; Man, Q.; Song, P.; Meng, L.; Du, Z.-Y.; Frøyland, L. Inclusion of Atlantic salmon in the Chinese diet reduces cardiovascular disease risk markers in dyslipidemic adult men. Nutr. Res. 2010, 30, 447–454. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, C.; Li, L.; Man, Q.; Meng, L.; Song, P.; Frøyland, L.; Du, Z.-Y. Dietary inclusion of salmon, herring and pompano as oily fish reduces CVD risk markers in dyslipidaemic middle-aged and elderly Chinese women. Br. J. Nutr. 2012, 108, 1455–1465. [Google Scholar] [CrossRef]
- Ganther, H.E. Modification of methylmercury toxicity and metabolism by selenium and vitamin E: Possible mechanisms. Environ. Health Perspect. 1978, 25, 71–76. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Rimm, E.B. Fish intake, contaminants, and human health: Evaluating the risks and the benefits. JAMA 2006, 296, 1885–1899. [Google Scholar] [CrossRef]
- He, K. Fish, long-chain omega-3 polyunsaturated fatty acids and prevention of cardiovascular disease—eat fish or take fish oil supplement? Prog. Cardiovasc. Dis. 2009, 52, 95–114. [Google Scholar] [CrossRef]
- Aung, T.; Halsey, J.; Kromhout, D.; Gerstein, H.C.; Marchioli, R.; Tavazzi, L.; Geleijnse, J.M.; Rauch, B.; Ness, A.; Galan, P.; et al. Associations of omega-3 fatty acid supplement use with cardiovascular disease risks: Meta-analysis of 10 trials involving 77 917 individuals. JAMA Cardiol. 2018, 3, 225–233. [Google Scholar] [CrossRef]
- Abdelhamid, A.S.; Brown, T.J.; Brainard, J.S.; Biswas, P.; Thorpe, G.C.; Moore, H.J.; Deane, K.H.O.; AlAbdulghafoor, F.K.; Summerbell, C.D.; Worthington, H.V.; et al. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2018, 7, CD003177. [Google Scholar] [CrossRef] [PubMed]
- D’Ascoli, T.A.; Mursu, J.; Voutilainen, S.; Kauhanen, J.; Tuomainen, T.P.; Virtanen, J.K. Association between serum long-chain omega-3 polyunsaturated fatty acids and cognitive performance in elderly men and women: The Kuopio Ischaemic Heart Disease Risk Factor Study. Eur. J. Clin. Nutr. 2016, 70, 970. [Google Scholar] [CrossRef] [PubMed]
| Men | Women | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | p Value | Q1 | Q2 | Q3 | Q4 | Q5 | p value | |
| N | 1120 | 1146 | 1239 | 1089 | 1116 | 3044 | 2940 | 2989 | 2983 | 3004 | ||
| Age (years) | 55.2 ± 8.6 | 54.2 ± 8.2 | 54.7 ± 8.2 | 53.9 ± 8.5 | 53.8 ± 8.1 | <0.0001 | 50.2 ± 7.5 | 49.7 ± 7.2 | 50.0 ± 7.4 | 49.4 ± 7.1 | 50.3 ± 7.0 | <0.0001 |
| Age (years), n (%) | ||||||||||||
| 40–49 | 312 (27.9) | 348 (30.4) | 351 (28.3) | 361 (33.2) | 365 (32.7) | <0.0010 | 1564 (51.4) | 1561 (53.1) | 1536 (51.4) | 1654 (55.5) | 1491 (49.6) | <0.0001 |
| 50–59 | 389 (34.7) | 435 (38.0) | 477 (38.5) | 405 (37.2) | 423 (37.9) | 1044 (34.3) | 1045 (35.5) | 1065 (35.6) | 1005 (33.7) | 1145 (38.1) | ||
| 60–69 | 419 (37.4) | 363 (31.7) | 411 (33.2) | 323 (29.7) | 328 (29.4) | 436 (14.3) | 334 (11.4) | 388 (13.0) | 324 (10.9) | 368 (12.3) | ||
| Education level, n (%) | ||||||||||||
| Under middle school | 321 (28.7) | 241 (21.0) | 272 (22.0) | 213 (19.6) | 184 (16.5) | <0.0001 | 1032 (33.9) | 811 (27.6) | 874 (29.2) | 738 (24.7) | 751 (25.0) | <0.0001 |
| High school | 413 (36.9) | 473 (41.3) | 485 (39.1) | 431 (39.6) | 472 (42.3) | 1314 (43.2) | 1382 (47.0) | 1374 (46.0) | 1493 (50.1) | 1497 (49.8) | ||
| Over college | 370 (33.0) | 419 (36.6) | 466 (37.6) | 435 (39.9) | 448 (40.1) | 665 (21.9) | 716 (24.4) | 706 (23.6) | 729 (24.4) | 719 (23.9) | ||
| BMI (kg/m2) | 23.2 ± 2.7 | 23.4 ± 2.6 | 23.5 ± 2.6 | 23.8 ± 2.6 | 23.9 ± 2.6 | <0.0001 | 22.7 ± 2.7 | 22.9 ± 2.8 | 22.9 ± 2.7 | 23.0 ± 2.7 | 23.1 ± 2.7 | <0.0001 |
| Obesity, n (%) | ||||||||||||
| Underweight | 37 (3.3) | 29 (2.5) | 26 (2.1) | 15 (1.4) | 20 (1.8) | <0.0001 | 126 (4.1) | 94 (3.2) | 81 (2.7) | 78 (2.6) | 66 (2.2) | 0.0003 |
| Normal | 497 (44.4) | 476 (41.5) | 500 (40.4) | 425 (39.0) | 407 (36.5) | 1623 (53.3) | 1590 (54.1) | 1577 (52.8) | 1571 (52.7) | 1525 (50.8) | ||
| Overweight | 314 (28.0) | 350 (30.5) | 393 (31.7) | 301 (27.6) | 301 (27.0) | 706 (23.2) | 680 (23.1) | 743 (24.9) | 749 (25.1) | 779 (25.9) | ||
| Obese | 272 (24.3) | 291 (25.4) | 320 (25.8) | 348 (32.0) | 388 (34.8) | 589 (19.4) | 576 (19.6) | 588 (19.7) | 585 (19.6) | 634 (21.1) | ||
| Alcohol consumption | ||||||||||||
| Non-drinker | 377 (33.7) | 298 (26.0) | 332 (26.8) | 252 (23.1) | 254 (22.8) | <0.0001 | 2104 (69.1) | 1925 (65.5) | 1966 (65.8) | 1893 (63.5) | 2008 (66.8) | 0.0008 |
| Current drinker | 740 (66.1) | 847 (73.9) | 901 (72.7) | 831 (76.3) | 857 (76.8) | 929 (30.5) | 1001 (34.1) | 1011 (33.8) | 1081 (36.2) | 979 (32.6) | ||
| Current smoking status | ||||||||||||
| Never smoker | 410 (36.6) | 423 (36.9) | 436 (35.2) | 364 (33.4) | 366 (32.8) | 0.5620 | 2955 (97.1) | 2858 (97.2) | 2914 (97.5) | 2910 (97.6) | 2908 (96.8) | 0.5502 |
| Past smoker | 448 (40.0) | 458 (40.0) | 508 (41.0) | 445 (40.9) | 455 (40.8) | 28 (0.9) | 29 (1.0) | 23 (0.8) | 24 (0.8) | 37 (1.2) | ||
| Current smoker | 258 (23.0) | 261 (22.8) | 289 (23.3) | 276 (25.3) | 287 (25.7) | 51 (1.7) | 40 (1.4) | 40 (1.3) | 39 (1.3) | 40 (1.3) | ||
| Physical activity | ||||||||||||
| Active | 217 (19.4) | 224 (19.6) | 241 (19.5) | 237 (21.8) | 288 (25.8) | 0.0002 | 485 (15.9) | 467 (15.9) | 522 (17.5) | 520 (17.4) | 651 (21.7) | <0.0001 |
| Inactive | 885 (79.0) | 895 (78.1) | 960 (77.5) | 819 (75.2) | 793 (71.1) | 2519 (82.8) | 2426 (82.5) | 2425 (81.1) | 2390 (80.1) | 2274 (75.7) | ||
| Nutrient intake | ||||||||||||
| Total energy (Kcal/d) | 1658.6 ± 436.3 | 1754.3 ± 437.2 | 1816.8 ± 406.4 | 1913.0 ± 460.6 | 2057.5 ± 492.8 | <0.0001 | 1534.4 ± 431.2 | 1600.8 ± 445.5 | 1678.4 ± 456.7 | 1758.0 ± 481.0 | 1921.0 ± 7.0 | <0.0001 |
| Carbohydrates (g/d) | 309.0 ± 76.8 | 317.6 ± 77.6 | 326.5 ± 72.4 | 335.4 ± 78.4 | 348.8 ± 80.1 | <0.0001 | 286.4 ± 79.8 | 292.9 ± 82.3 | 301.4 ± 82.1 | 310.2 ± 85.5 | 327.3 ± 90.6 | <0.0001 |
| Protein (g/d) | 49.3 ± 16.8 | 56.0 ± 17.6 | 59.5 ± 16.9 | 65.6 ± 20.5 | 76.7 ± 26.0 | <0.0001 | 46.7 ± 16.0 | 51.1 ± 16.6 | 56.0 ± 18.5 | 60.8 ± 19.4 | 72.2 ± 25.3 | <0.0001 |
| Fat (g/d) | 22.3 ± 13.1 | 26.3 ± 13.0 | 27.8 ± 12.4 | 32.0 ± 14.8 | 37.4 ± 17.1 | <0.0001 | 20.6 ± 11.6 | 23.2 ± 12.1 | 26.0 ± 13.3 | 29.0 ± 140 | 34.8 ± 17.0 | < .0001 |
| Oily Fish Consumption (g/d) | ||||||
|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | P for Trend | |
| Men (n = 5710) | ||||||
| Median (range) | 1.7 (0.0–2.6) | 3.5 (2.7–4.9) | 6.0 (5.0-6.8) | 8.6 (6.8-10.7) | 16.0 (10.7-116.4) | |
| Person-years, mean (sum) | 5.0 (5579.4) | 4.9 (5658.3) | 5.0 (6138.7) | 4.9 (5350.0) | 5.0 (5589.6) | |
| Hypercholesterolemia | ||||||
| Cases, n | 287 | 292 | 313 | 275 | 313 | |
| Model 1 | 1.00 (Ref.) | 1.00 (0.85-1.18) | 0.97 (0.83-1.14) | 1.00 (0.85-1.19) | 1.06 (0.90-1.24) | 0.3829 |
| Model 2 | 1.00 (Ref.) | 0.99 (0.84-1.17) | 0.96 (0.82-1.13) | 0.99 (0.84-1.17) | 1.04 (0.88-1.23) | 0.5078 |
| Hyper-LDL cholesterolemia | ||||||
| Cases, n | 164 | 155 | 168 | 174 | 186 | |
| Model 1 | 1.00 (Ref.) | 0.92 (0.74-1.15) | 0.90 (0.73-1.12) | 1.11 (0.89-1.37) | 1.09 (0.88-1.35) | 0.1160 |
| Model 2 | 1.00 (Ref.) | 0.92 (0.74-1.15) | 0.90 (0.72-1.12) | 1.11 (0.89-1.38) | 1.10 (0.88-1.37) | 0.1072 |
| Hypo-HDL cholesterolemia | ||||||
| Cases, n | 65 | 51 | 80 | 55 | 47 | |
| Model 1 | 1.00 (Ref.) | 0.75 (0.52-1.09) | 1.06 (0.76-1.47) | 0.84 (0.59-1.21) | 0.66 (0.45-0.96) | 0.0507 |
| Model 2 | 1.00 (Ref.) | 0.79 (0.55-1.14) | 1.11 (0.79-1.54) | 0.87 (0.60-1.27) | 0.68 (0.46-1.01) | 0.0762 |
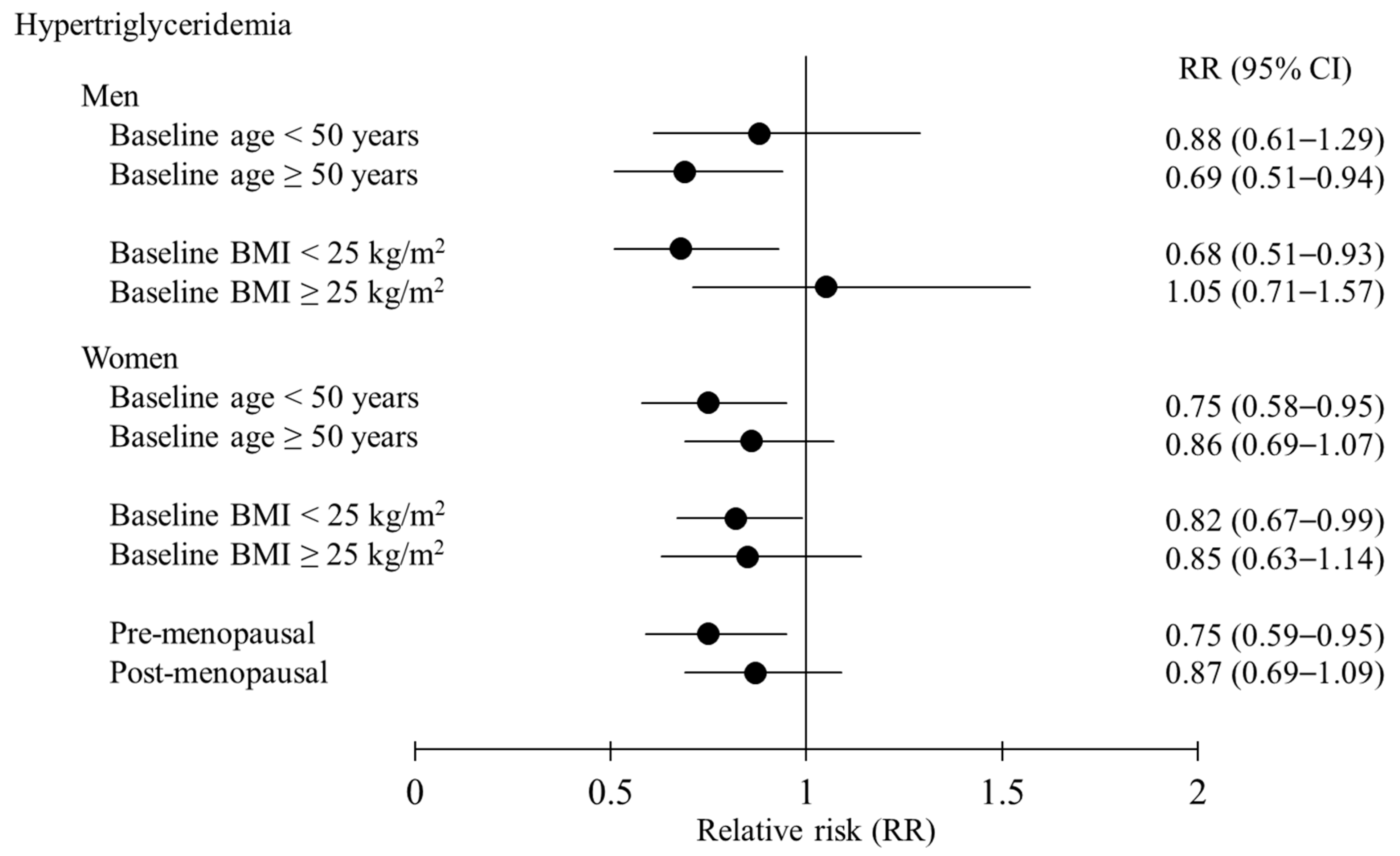
| Hypertriglyceridemia | ||||||
| Cases, n | 159 | 166 | 175 | 163 | 146 | |
| Model 1 | 1.00 (Ref.) | 0.99 (0.80-1.23) | 0.93 (0.75-1.16) | 0.99 (0.79-1.23) | 0.80 (0.64-1.01) | 0.0419 |
| Model 2 | 1.00 (Ref.) | 0.98 (0.78-1.21) | 0.91 (0.73-1.13) | 0.94 (0.75-1.17) | 0.75 (0.60-0.95) | 0.0121 |
| Dyslipidemia | ||||||
| Cases, n | 418 | 420 | 462 | 411 | 431 | |
| Model 1 | 1.00 (Ref.) | 0.98 (0.86-1.12) | 0.98 (0.85-1.11) | 1.01 (0.89-1.16) | 0.98 (0.86-1.13) | 0.9710 |
| Model 2 | 1.00 (Ref.) | 0.97 (0.85-1.12) | 0.97 (0.84-1.11) | 1.00 (0.87-1.14) | 0.96 (0.84-1.11) | 0.7353 |
| Women (n = 14,960) | ||||||
| Median (range) | 1.5 (0.0-2.3) | 3.3 (2.3-4.3) | 5.8 (4.3-6.7) | 8.5 (6.8-10.7) | 15.0 (10.7-102.1) | |
| Person-years, mean (sum) | 5.0 (15232.7) | 5.1 (14975.6) | 5.1 (15171.8) | 5.1 (15261.0) | 5.3 (15969.5) | |
| Hypercholesterolemia | ||||||
| Cases, n | 1104 | 1080 | 1081 | 1156 | 1226 | |
| Model 1 | 1.00 (Ref.) | 0.97 (0.89-1.06) | 0.95 (0.87-1.03) | 1.02 (0.94-1.11) | 0.97 (0.89-1.05) | 0.7576 |
| Model 2 | 1.00 (Ref.) | 0.96 (0.89-1.05) | 0.94 (0.86-1.02) | 1.00 (0.92-1.09) | 0.97 (0.89-1.05) | 0.8116 |
| Hyper-LDL cholesterolemia | ||||||
| Cases, n | 603 | 598 | 575 | 617 | 683 | |
| Model 1 | 1.00 (Ref.) | 0.98 (0.88-1.10) | 0.91 (0.81-1.02) | 0.99 (0.88-1.11) | 0.97 (1.01-1.02) | 0.7691 |
| Model 2 | 1.00 (Ref.) | 0.97 (0.87-1.09) | 0.91 (0.81-1.02) | 0.98 (0.88-1.10) | 0.97 (0.87-1.09) | 0.9111 |
| Hypo-HDL cholesterolemia | ||||||
| Cases, n | 76 | 81 | 70 | 72 | 77 | |
| Model 1 | 1.00 (Ref.) | 1.05 (0.77-1.44) | 0.87 (0.63-1.20) | 0.91 (0.66-1.26) | 0.84 (0.61-1.16) | 0.1915 |
| Model 2 | 1.00 (Ref.) | 1.05 (0.77-1.44) | 0.87 (0.63-1.20) | 0.91 (0.66-1.26) | 0.83 (0.60-1.15) | 0.1699 |
| Hypertriglyceridemia | ||||||
| Cases, n | 320 | 297 | 294 | 267 | 300 | |
| Model 1 | 1.00 (Ref.) | 0.92 (0.78-1.08) | 0.87 (0.74-1.02) | 0.80 (0.68-0.95) | 0.79 (0.67-0.92) | 0.0024 |
| Model 2 | 1.00 (Ref.) | 0.92 (0.78-1.08) | 0.88 (0.75-1.04) | 0.81 (0.69-0.96) | 0.81 (0.69-0.96) | 0.0110 |
| Dyslipidemia | ||||||
| Cases, n | 1299 | 1294 | 1263 | 1329 | 1424 | |
| Model 1 | 1.00 (Ref.) | 0.99 (0.92-1.07) | 0.94 (0.87-1.01) | 0.99 (0.92-1.07) | 0.95 (0.88-1.02) | 0.2516 |
| Model 2 | 1.00 (Ref.) | 0.98 (0.91-1.06) | 0.93 (0.86-1.01) | 0.98 (0.91-1.06) | 0.95 (0.88-1.03) | 0.3061 |
| Total Fish Consumption (g/d) | ||||||
|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | P for Trend | |
| Men (n = 5710) | ||||||
| Median (range) | 11.9 (0.2-16.8) | 21.0 (16.8–25.1) | 29.6 (25.1–34.8) | 40.8 (34.8–49.9) | 65.5 (49.9–292.2) | |
| Person-years, mean (sum) | 5.0 (5468.7) | 4.9 (5472.3) | 4.9 (5553.5) | 5.0 (5870.7) | 4.9 (5950.8) | |
| Hypercholesterolemia | ||||||
| Cases, n | 261 | 279 | 308 | 319 | 313 | |
| Model 1 | 1.00 (Ref.) | 1.05 (0.88–1.24) | 1.14 (0.97–1.35) | 1.13 (0.96–1.33) | 1.12 (0.95–1.32) | 0.1948 |
| Model 2 | 1.00 (Ref.) | 1.04 (0.88–1.23) | 1.13 (0.96–1.34) | 1.12 (0.95–1.32) | 1.11 (0.93–1.33) | 0.2593 |
| Hyper-LDL cholesterolemia | ||||||
| Cases, n | 151 | 140 | 169 | 192 | 195 | |
| Model 1 | 1.00 (Ref.) | 0.91 (0.72–1.15) | 1.08 (0.87–1.35) | 1.17 (0.95–1.45) | 1.20 (0.97–1.49) | 0.0145 |
| Model 2 | 1.00 (Ref.) | 0.91 (0.72–1.15) | 1.10 (0.88–1.37) | 1.19 (0.96–1.49) | 1.25 (1.00–1.58) | 0.0074 |
| Hypo-HDL cholesterolemia | ||||||
| Cases, n | 68 | 53 | 48 | 74 | 55 | |
| Model 1 | 1.00 (Ref.) | 0.77 (0.53–1.10) | 0.68 (0.47–0.99) | 0.99 (0.71–1.37) | 0.72 (0.50–1.03) | 0.3026 |
| Model 2 | 1.00 (Ref.) | 0.80 (0.56–1.15) | 0.74 (0.51–1.08) | 1.03 (0.73–1.44) | 0.72 (0.49–1.06) | 0.3069 |
| Hypertriglyceridemia | ||||||
| Cases, n | 157 | 148 | 147 | 188 | 169 | |
| Model 1 | 1.00 (Ref.) | 0.90 (0.71–1.12) | 0.89 (0.71–1.11) | 1.06 (0.86–1.31) | 0.93 (0.75–1.15) | 0.9930 |
| Model 2 | 1.00 (Ref.) | 0.89 (0.71–1.12) | 0.88 (0.70–1.11) | 1.02 (0.82–1.27) | 0.87 (0.69–1.10) | 0.5172 |
| Dyslipidemia | ||||||
| Cases, n | 396 | 403 | 409 | 478 | 456 | |
| Model 1 | 1.00 (Ref.) | 1.00 (0.87–1.15) | 1.00 (0.87–1.15) | 1.11 (0.97–1.27) | 1.06 (0.92–1.21) | 0.2005 |
| Model 2 | 1.00 (Ref.) | 0.99 (0.86-1.14) | 0.99 (0.86–1.14) | 1.09 (0.95–1.26) | 1.04 (0.90–1.20) | 0.3559 |
| Women (n = 14,960) | ||||||
| Median (range) | 11.9 (0.0-16.8) | 21.0 (16.8–25.1) | 29.6 (25.1–34.8) | 41.0 (34.8–49.9) | 65.5 (49.9–348.5) | |
| Person-years, mean (sum) | 5.1 (15389.3) | 5.1 (15350.3) | 5.1 (15201.3) | 5.1 (15218.5) | 5.3 (15451.2) | |
| Hypercholesterolemia | ||||||
| Cases, n | 1099 | 1082 | 1152 | 1158 | 1156 | |
| Model 1 | 1.00 (Ref.) | 0.98 (0.90–1.06) | 1.08 (0.99–1.17) | 1.04 (0.96–1.13) | 0.99 (0.91–1.07) | 0.9380 |
| Model 2 | 1.00 (Ref.) | 0.97 (0.90–1.06) | 1.07 (0.99–1.17) | 1.04 (0.95-1.13) | 1.00 (0.91–1.09) | 0.9228 |
| Hyper-LDL cholesterolemia | ||||||
| Cases, n | 586 | 582 | 631 | 631 | 646 | |
| Model 1 | 1.00 (Ref.) | 0.98 (0.88–1.10) | 1.11 (0.99–1.24) | 1.06 (0.95–1.19) | 1.02 (0.91–1.14) | 0.6460 |
| Model 2 | 1.00 (Ref.) | 0.99 (0.88–1.11) | 1.11 (0.99–1.25) | 1.07 (0.95–1.20) | 1.05 (0.93–1.18) | 0.4159 |
| Hypo-HDL cholesterolemia | ||||||
| Cases, n | 87 | 71 | 64 | 73 | 81 | |
| Model 1 | 1.00 (Ref.) | 0.82 (0.60–1.12) | 0.76 (0.55–1.05) | 0.83 (0.60–1.13) | 0.84 (0.62–1.14) | 0.5000 |
| Model 2 | 1.00 (Ref.) | 0.81 (0.59–1.10) | 0.76 (0.55–1.05) | 0.81 (0.59–1.12) | 0.82 (0.59–1.14) | 0.4593 |
| Hypertriglyceridemia | ||||||
| Cases, n | 307 | 304 | 297 | 273 | 297 | |
| Model 1 | 1.00 (Ref.) | 0.99 (0.84–1.16) | 1.00 (0.85–1.17) | 0.88 (0.75–1.03) | 0.88 (0.75–1.04) | 0.0537 |
| Model 2 | 1.00 (Ref.) | 1.00 (0.85–1.17) | 1.02 (0.87–1.20) | 0.90 (0.76–1.07) | 0.93 (0.78–1.10) | 0.2375 |
| Dyslipidemia | ||||||
| Cases, n | 1299 | 1282 | 1344 | 1338 | 1346 | |
| Model 1 | 1.00 (Ref.) | 0.98 (0.91–1.06) | 1.06 (0.98–1.15) | 1.02 (0.94–1.10) | 0.97 (0.90–1.05) | 0.4501 |
| Model 2 | 1.00 (Ref.) | 0.98 (0.91–1.06) | 1.06 (0.98–1.15) | 1.02 (0.94–1.10) | 0.98 (0.90–1.06) | 0.6362 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-A.; Lee, J.-k.; Kang, D.; Shin, S. Oily Fish Consumption and the Risk of Dyslipidemia in Korean Adults: A Prospective Cohort Study Based on the Health Examinees Gem (HEXA-G) Study. Nutrients 2019, 11, 2506. https://doi.org/10.3390/nu11102506
Kim S-A, Lee J-k, Kang D, Shin S. Oily Fish Consumption and the Risk of Dyslipidemia in Korean Adults: A Prospective Cohort Study Based on the Health Examinees Gem (HEXA-G) Study. Nutrients. 2019; 11(10):2506. https://doi.org/10.3390/nu11102506
Chicago/Turabian StyleKim, Seong-Ah, Jong-koo Lee, Daehee Kang, and Sangah Shin. 2019. "Oily Fish Consumption and the Risk of Dyslipidemia in Korean Adults: A Prospective Cohort Study Based on the Health Examinees Gem (HEXA-G) Study" Nutrients 11, no. 10: 2506. https://doi.org/10.3390/nu11102506
APA StyleKim, S.-A., Lee, J.-k., Kang, D., & Shin, S. (2019). Oily Fish Consumption and the Risk of Dyslipidemia in Korean Adults: A Prospective Cohort Study Based on the Health Examinees Gem (HEXA-G) Study. Nutrients, 11(10), 2506. https://doi.org/10.3390/nu11102506






