Renal Reabsorption of Folates: Pharmacological and Toxicological Snapshots
Abstract
1. Introduction
2. Mechanisms of Folate Tubular Reabsorption
3. Folic Acid Treatment in Patients with Chronic Kidney Disease (CKD)
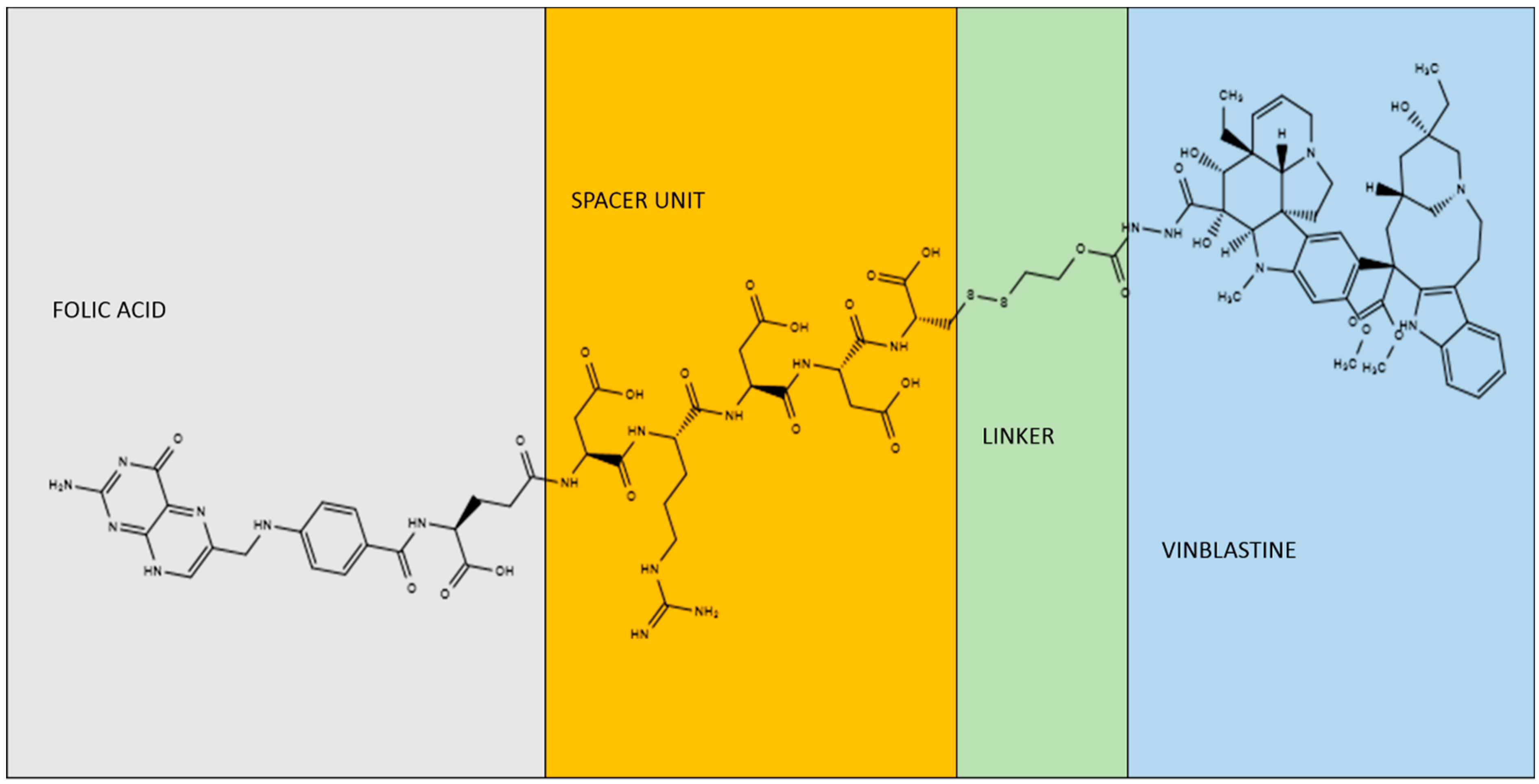
4. Folic Acid-Induced Acute Kidney Injury Model
5. Nephrotoxicity of Folate-Conjugated Chemotherapy and Radiotherapy
6. Folic Acid-Bound Drugs for the Treatment of Polycystic Kidney
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jeeja, M.C.; Jayakrishnan, T.; Narayanan, P.V.; Kumar, M.S.; Thejus, T.; Anilakumari, V.P. Folic acid supplementation on homocysteine levels in children taking antiepileptic drugs: A randomized controlled trial. J. Pharm. Pharm. 2014, 5, 93–99. [Google Scholar]
- den Heijer, M.; Brouwer, I.A.; Bos, G.M.; Blom, H.J.; van der Put, N.M.; Spaans, A.P.; Rosendaal, F.R.; Thomas, C.M.; Haak, H.L.; Wijermans, P.W.; et al. Vitamin supplementation reduces blood homocysteine levels: A controlled trial in patients with venous thrombosis and healthy volunteers. Arterioscler. Thromb. Vasc. Biol. 1998, 18, 356–361. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kronn, D.; Goldman, I.D. Hereditary Folate Malabsorption. In GeneReviews; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Stephens, K., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1993. [Google Scholar]
- Visentin, M.; Zhao, R.; Goldman, I.D. The antifolates. Hematol. Oncol. Clin. N. Am. 2012, 26, 629–648. [Google Scholar] [CrossRef] [PubMed]
- McKillop, D.J.; Pentieva, K.; Daly, D.; McPartlin, J.M.; Hughes, J.; Strain, J.J.; Scott, J.M.; McNulty, H. The effect of different cooking methods on folate retention in various foods that are amongst the major contributors to folate intake in the UK diet. Br. J. Nutr. 2002, 88, 681–688. [Google Scholar] [CrossRef] [PubMed]
- Czarnowska, M.; Gujska, E. Effect of freezing technology and storage conditions on folate content in selected vegetables. Plant Foods Hum. Nutr. 2012, 67, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, C.M.; Sternberg, M.R.; Fazili, Z.; Lacher, D.A.; Zhang, M.; Johnson, C.L.; Hamner, H.C.; Bailey, R.L.; Rader, J.I.; Yamini, S.; et al. Folate status and concentrations of serum folate forms in the US population: National Health and Nutrition Examination Survey 2011-2. Br. J. Nutr. 2015, 113, 1965–1977. [Google Scholar] [CrossRef] [PubMed]
- Kalmbach, R.D.; Choumenkovitch, S.F.; Troen, A.M.; D’Agostino, R.; Jacques, P.F.; Selhub, J. Circulating folic acid in plasma: Relation to folic acid fortification. Am. J. Clin. Nutr. 2008, 88, 763–768. [Google Scholar] [CrossRef]
- Visentin, M.; Diop-Bove, N.; Zhao, R.; Goldman, I.D. The intestinal absorption of folates. Annu. Rev. Physiol. 2014, 76, 251–274. [Google Scholar] [CrossRef]
- Qiu, A.; Jansen, M.; Sakaris, A.; Min, S.H.; Chattopadhyay, S.; Tsai, E.; Sandoval, C.; Zhao, R.; Akabas, M.H.; Goldman, I.D. Identification of an intestinal folate transporter and the molecular basis for hereditary folate malabsorption. Cell 2006, 127, 917–928. [Google Scholar] [CrossRef]
- Shin, D.S.; Min, S.H.; Russell, L.; Zhao, R.; Fiser, A.; Goldman, I.D. Functional roles of aspartate residues of the proton-coupled folate transporter (PCFT-SLC46A1); a D156Y mutation causing hereditary folate malabsorption. Blood 2010, 116, 5162–5169. [Google Scholar] [CrossRef]
- Salojin, K.V.; Cabrera, R.M.; Sun, W.; Chang, W.C.; Lin, C.; Duncan, L.; Platt, K.A.; Read, R.; Vogel, P.; Liu, Q.; et al. A mouse model of hereditary folate malabsorption: Deletion of the PCFT gene leads to systemic folate deficiency. Blood 2011, 117, 4895–4904. [Google Scholar] [CrossRef] [PubMed]
- Eloranta, J.J.; Zair, Z.M.; Hiller, C.; Hausler, S.; Stieger, B.; Kullak-Ublick, G.A. Vitamin D3 and its nuclear receptor increase the expression and activity of the human proton-coupled folate transporter. Mol. Pharmacol. 2009, 76, 1062–1071. [Google Scholar] [CrossRef] [PubMed]
- Kullak-Ublick, G.A.; Gubler, C.; Spanaus, K.; Ismair, M.G.; Claro da Silva, T.; Jetter, A. No major effects of vitamin D3 (1,25 dihydroxyvitamin D3) on absorption and pharmacokinetics of folic acid and fexofenadine in healthy volunteers. Eur. J. Clin. Pharmacol. 2016, 72, 797–805. [Google Scholar] [CrossRef] [PubMed]
- Wani, N.A.; Kaur, J. Reduced levels of folate transporters (PCFT and RFC) in membrane lipid rafts result in colonic folate malabsorption in chronic alcoholism. J. Cell. Physiol. 2011, 226, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Birn, H. The kidney in vitamin B12 and folate homeostasis: Characterization of receptors for tubular uptake of vitamins and carrier proteins. Am. J. Physiol. Ren. Physiol. 2006, 291, F22–F36. [Google Scholar] [CrossRef] [PubMed]
- Soliman, H.A.; Olesen, H. Folic acid binding by human plasma albumin. Scand. J. Clin. Lab. Investig. 1976, 36, 299–304. [Google Scholar] [CrossRef]
- Zhao, R.; Diop-Bove, N.; Visentin, M.; Goldman, I.D. Mechanisms of membrane transport of folates into cells and across epithelia. Annu. Rev. Nutr. 2011, 31, 177–201. [Google Scholar] [CrossRef] [PubMed]
- Gelineau-van Waes, J.; Heller, S.; Bauer, L.K.; Wilberding, J.; Maddox, J.R.; Aleman, F.; Rosenquist, T.H.; Finnell, R.H. Embryonic development in the reduced folate carrier knockout mouse is modulated by maternal folate supplementation. Birth Defects Res. Part A Clin. Mol. Teratol. 2008, 82, 494–507. [Google Scholar] [CrossRef]
- Birn, H.; Spiegelstein, O.; Christensen, E.I.; Finnell, R.H. Renal tubular reabsorption of folate mediated by folate binding protein 1. J. Am. Soc. Nephrol. JASN 2005, 16, 608–615. [Google Scholar] [CrossRef] [PubMed]
- Reddy, J.A.; Low, P.S. Folate-mediated targeting of therapeutic and imaging agents to cancers. Crit. Rev. Ther. Drug Carr. Syst. 1998, 15, 587–627. [Google Scholar] [CrossRef]
- Selhub, J.; Emmanouel, D.; Stavropoulos, T.; Arnold, R. Renal folate absorption and the kidney folate binding protein. I. Urinary clearance studies. Am. J. Physiol. 1987, 252 Pt 2, F750–F756. [Google Scholar] [CrossRef]
- Muldoon, R.T.; Eisenga, B.H.; Morshed, K.M.; McMartin, K.E. 5-Methyltetrahydrofolate is reabsorbed and metabolized in isolated perfused rat kidney. J. Nutr. 1992, 122, 2415–2423. [Google Scholar] [CrossRef] [PubMed]
- Birn, H.; Nielsen, S.; Christensen, E.I. Internalization and apical-to-basolateral transport of folate in rat kidney proximal tubule. Am. J. Physiol. 1997, 272 Pt 2, F70–F78. [Google Scholar] [CrossRef]
- Selhub, J.; Franklin, W.A. The folate-binding protein of rat kidney. Purification, properties, and cellular distribution. J. Biol. Chem. 1984, 259, 6601–6606. [Google Scholar] [PubMed]
- Kamen, B.A.; Smith, A.K. A review of folate receptor alpha cycling and 5-methyltetrahydrofolate accumulation with an emphasis on cell models in vitro. Adv. Drug Deliv. Rev. 2004, 56, 1085–1097. [Google Scholar] [CrossRef] [PubMed]
- Holm, J.; Bruun, S.W.; Hansen, S.I. The complex interplay between ligand binding and conformational structure of the folate binding protein (folate receptor): Biological perspectives. Biochim. Biophys. Acta 2015, 1854 Pt A, 1249–1259. [Google Scholar] [CrossRef]
- Smart, E.J.; Mineo, C.; Anderson, R.G. Clustered folate receptors deliver 5-methyltetrahydrofolate to cytoplasm of MA104 cells. J. Cell Biol. 1996, 134, 1169–1177. [Google Scholar] [CrossRef]
- Chang, W.J.; Rothberg, K.G.; Kamen, B.A.; Anderson, R.G. Lowering the cholesterol content of MA104 cells inhibits receptor-mediated transport of folate. J. Cell Biol. 1992, 118, 63–69. [Google Scholar] [CrossRef]
- Mayor, S.; Maxfield, F.R. Insolubility and redistribution of GPI-anchored proteins at the cell surface after detergent treatment. Mol. Biol. Cell 1995, 6, 929–944. [Google Scholar] [CrossRef]
- Rijnboutt, S.; Jansen, G.; Posthuma, G.; Hynes, J.B.; Schornagel, J.H.; Strous, G.J. Endocytosis of GPI-linked membrane folate receptor-alpha. J. Cell Biol. 1996, 132, 35–47. [Google Scholar] [CrossRef]
- Sabharanjak, S.; Mayor, S. Folate receptor endocytosis and trafficking. Adv. Drug Deliv. Rev. 2004, 56, 1099–1109. [Google Scholar] [CrossRef] [PubMed]
- Sandoval, R.M.; Kennedy, M.D.; Low, P.S.; Molitoris, B.A. Uptake and trafficking of fluorescent conjugates of folic acid in intact kidney determined using intravital two-photon microscopy. Am. J. Physiol. Cell Physiol. 2004, 287, C517–C526. [Google Scholar] [CrossRef] [PubMed]
- Birn, H.; Zhai, X.; Holm, J.; Hansen, S.I.; Jacobsen, C.; Christensen, E.I.; Moestrup, S.K. Megalin binds and mediates cellular internalization of folate binding protein. FEBS J. 2005, 272, 4423–4430. [Google Scholar] [CrossRef] [PubMed]
- Christensen, E.I.; Birn, H. Megalin and cubilin: Multifunctional endocytic receptors. Nat. Rev. Mol. Cell Biol. 2002, 3, 256–266. [Google Scholar] [CrossRef] [PubMed]
- Waxman, S. Folate binding proteins. Br. J. Haematol. 1975, 29, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Morshed, K.M.; Ross, D.M.; McMartin, K.E. Folate transport proteins mediate the bidirectional transport of 5-methyltetrahydrofolate in cultured human proximal tubule cells. J. Nutr. 1997, 127, 1137–1147. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, R.; Russell, R.G.; Goldman, I.D. Localization of the murine reduced folate carrier as assessed by immunohistochemical analysis. Biochim. Biophys. Acta 2001, 1513, 49–54. [Google Scholar] [CrossRef]
- Weitman, S.D.; Lark, R.H.; Coney, L.R.; Fort, D.W.; Frasca, V.; Zurawski, V.R., Jr.; Kamen, B.A. Distribution of the folate receptor GP38 in normal and malignant cell lines and tissues. Cancer Res. 1992, 52, 3396–3401. [Google Scholar]
- Weitman, S.D.; Weinberg, A.G.; Coney, L.R.; Zurawski, V.R.; Jennings, D.S.; Kamen, B.A. Cellular localization of the folate receptor: Potential role in drug toxicity and folate homeostasis. Cancer Res. 1992, 52, 6708–6711. [Google Scholar]
- Matherly, L.H. Molecular and cellular biology of the human reduced folate carrier. Prog. Nucleic Acid Res. Mol. Biol. 2001, 67, 131–162. [Google Scholar]
- Matherly, L.H.; Goldman, D.I. Membrane transport of folates. Vitam. Horm. 2003, 66, 403–456. [Google Scholar]
- Zhao, R.; Matherly, L.H.; Goldman, I.D. Membrane transporters and folate homeostasis: Intestinal absorption and transport into systemic compartments and tissues. Expert Rev. Mol. Med. 2009, 11, e4. [Google Scholar] [CrossRef] [PubMed]
- Zhao, R.; Qiu, A.; Tsai, E.; Jansen, M.; Akabas, M.H.; Goldman, I.D. The proton-coupled folate transporter: Impact on pemetrexed transport and on antifolates activities compared with the reduced folate carrier. Mol. Pharmacol. 2008, 74, 854–862. [Google Scholar] [CrossRef] [PubMed]
- Bozard, B.R.; Ganapathy, P.S.; Duplantier, J.; Mysona, B.; Ha, Y.; Roon, P.; Smith, R.; Goldman, I.D.; Prasad, P.; Martin, P.M.; et al. Molecular and biochemical characterization of folate transport proteins in retinal Muller cells. Investig. Ophthalmol. Vis. Sci. 2010, 51, 3226–3235. [Google Scholar] [CrossRef] [PubMed]
- Wani, N.A.; Kaur, J. Adaptive transport of folic acid across renal epithelia in folate-deficient rats. J. Physiol. Sci. 2012, 62, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Damaraju, V.L.; Cass, C.E.; Sawyer, M.B. Renal conservation of folates role of folate transport proteins. Vitam. Horm. 2008, 79, 185–202. [Google Scholar]
- Chen, Z.S.; Lee, K.; Walther, S.; Raftogianis, R.B.; Kuwano, M.; Zeng, H.; Kruh, G.D. Analysis of methotrexate and folate transport by multidrug resistance protein 4 (ABCC4): MRP4 is a component of the methotrexate efflux system. Cancer Res. 2002, 62, 3144–3150. [Google Scholar] [PubMed]
- Hirohashi, T.; Suzuki, H.; Sugiyama, Y. Characterization of the transport properties of cloned rat multidrug resistance-associated protein 3 (MRP3). J. Biol. Chem. 1999, 274, 15181–15185. [Google Scholar] [CrossRef]
- Hooijberg, J.H.; Broxterman, H.J.; Kool, M.; Assaraf, Y.G.; Peters, G.J.; Noordhuis, P.; Scheper, R.J.; Borst, P.; Pinedo, H.M.; Jansen, G. Antifolate resistance mediated by the multidrug resistance proteins MRP1 and MRP2. Cancer Res. 1999, 59, 2532–2535. [Google Scholar]
- Kusuhara, H.; Han, Y.H.; Shimoda, M.; Kokue, E.; Suzuki, H.; Sugiyama, Y. Reduced folate derivatives are endogenous substrates for cMOAT in rats. Am. J. Physiol. 1998, 275, G789–G796. [Google Scholar] [CrossRef]
- Zeng, H.; Liu, G.; Rea, P.A.; Kruh, G.D. Transport of amphipathic anions by human multidrug resistance protein 3. Cancer Res. 2000, 60, 4779–4784. [Google Scholar] [PubMed]
- Zeng, H.; Chen, Z.S.; Belinsky, M.G.; Rea, P.A.; Kruh, G.D. Transport of methotrexate (MTX) and folates by multidrug resistance protein (MRP) 3 and MRP1: Effect of polyglutamylation on MTX transport. Cancer Res. 2001, 61, 7225–7232. [Google Scholar] [PubMed]
- van Aubel, R.A.; Smeets, P.H.; Peters, J.G.; Bindels, R.J.; Russel, F.G. The MRP4/ABCC4 gene encodes a novel apical organic anion transporter in human kidney proximal tubules: Putative efflux pump for urinary cAMP and cGMP. J. Am. Soc. Nephrol. JASN 2002, 13, 595–603. [Google Scholar]
- Schaub, T.P.; Kartenbeck, J.; Konig, J.; Vogel, O.; Witzgall, R.; Kriz, W.; Keppler, D. Expression of the conjugate export pump encoded by the mrp2 gene in the apical membrane of kidney proximal tubules. J. Am. Soc. Nephrol. JASN 1997, 8, 1213–1221. [Google Scholar] [PubMed]
- Takenaka, K.; Morgan, J.A.; Scheffer, G.L.; Adachi, M.; Stewart, C.F.; Sun, D.; Leggas, M.; Ejendal, K.F.; Hrycyna, C.A.; Schuetz, J.D. Substrate overlap between Mrp4 and Abcg2/Bcrp affects purine analogue drug cytotoxicity and tissue distribution. Cancer Res. 2007, 67, 6965–6972. [Google Scholar] [CrossRef] [PubMed]
- Scheffer, G.L.; Kool, M.; de Haas, M.; de Vree, J.M.; Pijnenborg, A.C.; Bosman, D.K.; Elferink, R.P.; van der Valk, P.; Borst, P.; Scheper, R.J. Tissue distribution and induction of human multidrug resistant protein 3. Lab. Investig. 2002, 82, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Masuda, S. Functional characteristics and pharmacokinetic significance of kidney-specific organic anion transporters, OAT-K1 and OAT-K2, in the urinary excretion of anionic drugs. Drug Metab. Pharmacokinet. 2003, 18, 91–103. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Uwai, Y.; Okuda, M.; Takami, K.; Hashimoto, Y.; Inui, K. Functional characterization of the rat multispecific organic anion transporter OAT1 mediating basolateral uptake of anionic drugs in the kidney. FEBS Lett. 1998, 438, 321–324. [Google Scholar] [CrossRef]
- Sun, W.; Wu, R.R.; van Poelje, P.D.; Erion, M.D. Isolation of a family of organic anion transporters from human liver and kidney. Biochem. Biophys. Res. Commun. 2001, 283, 417–422. [Google Scholar] [CrossRef]
- Takeda, M.; Babu, E.; Narikawa, S.; Endou, H. Interaction of human organic anion transporters with various cephalosporin antibiotics. Eur. J. Pharmacol. 2002, 438, 137–142. [Google Scholar] [CrossRef]
- Lu, R.; Chan, B.S.; Schuster, V.L. Cloning of the human kidney PAH transporter: Narrow substrate specificity and regulation by protein kinase C. Am. J. Physiol. 1999, 276, F295–F303. [Google Scholar] [CrossRef] [PubMed]
- Wyatt, C.M.; Spence, J.D. Folic acid supplementation and chronic kidney disease progression. Kidney Int. 2016, 90, 1144–1145. [Google Scholar] [CrossRef] [PubMed]
- Bravo-Soto, G.A.; Madrid, T. Is folic acid supplementation useful for chronic kidney disease? Medwave 2016, 16 (Suppl. S5), e6591. [Google Scholar] [CrossRef] [PubMed]
- Hill, N.R.; Fatoba, S.T.; Oke, J.L.; Hirst, J.A.; O’Callaghan, C.A.; Lasserson, D.S.; Hobbs, F.D. Global Prevalence of Chronic Kidney Disease-A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0158765. [Google Scholar] [CrossRef]
- Bostom, A.G.; Lathrop, L. Hyperhomocysteinemia in end-stage renal disease: Prevalence, etiology, and potential relationship to arteriosclerotic outcomes. Kidney Int. 1997, 52, 10–20. [Google Scholar] [CrossRef]
- Righetti, M. Homocysteine-lowering vitamin B treatment decreases cardiovascular events in hemodialysis patients. Clin. Chem. Lab. Med. 2007, 45, 1586–1589. [Google Scholar] [CrossRef]
- Chrysant, S.G.; Chrysant, G.S. The current status of homocysteine as a risk factor for cardiovascular disease: A mini review. Expert Rev. Cardiovasc. Ther. 2018, 16, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Koyama, K.; Ito, A.; Yamamoto, J.; Nishio, T.; Kajikuri, J.; Dohi, Y.; Ohte, N.; Sano, A.; Nakamura, H.; Kumagai, H.; et al. Randomized controlled trial of the effect of short-term coadministration of methylcobalamin and folate on serum ADMA concentration in patients receiving long-term hemodialysis. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2010, 55, 1069–1078. [Google Scholar] [CrossRef]
- Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine (SEARCH) Collaborative Group; Armitage, J.M.; Bowman, L.; Clarke, R.J.; Wallendszus, K.; Bulbulia, R.; Rahimi, K.; Haynes, R.; Parish, S.; Sleight, P.; et al. Effects of homocysteine-lowering with folic acid plus vitamin B12 vs placebo on mortality and major morbidity in myocardial infarction survivors: A randomized trial. JAMA J. Am. Med Assoc. 2010, 303, 2486–2494. [Google Scholar]
- Bazzano, L.A. Folic acid supplementation and cardiovascular disease: The state of the art. Am. J. Med Sci. 2009, 338, 48–49. [Google Scholar] [CrossRef]
- Heinz, J.; Kropf, S.; Domrose, U.; Westphal, S.; Borucki, K.; Luley, C.; Neumann, K.H.; Dierkes, J. B vitamins and the risk of total mortality and cardiovascular disease in end-stage renal disease: Results of a randomized controlled trial. Circulation 2010, 121, 1432–1438. [Google Scholar] [CrossRef] [PubMed]
- Jamison, R.L.; Hartigan, P.; Kaufman, J.S.; Goldfarb, D.S.; Warren, S.R.; Guarino, P.D.; Gaziano, J.M.; Veterans Affairs Site Investigators. Effect of homocysteine lowering on mortality and vascular disease in advanced chronic kidney disease and end-stage renal disease: A randomized controlled trial. JAMA J. Am. Med. Assoc. 2007, 298, 1163–1170. [Google Scholar] [CrossRef] [PubMed]
- Bostom, A.G.; Carpenter, M.A.; Kusek, J.W.; Levey, A.S.; Hunsicker, L.; Pfeffer, M.A.; Selhub, J.; Jacques, P.F.; Cole, E.; Gravens-Mueller, L.; et al. Homocysteine-lowering and cardiovascular disease outcomes in kidney transplant recipients: Primary results from the Folic Acid for Vascular Outcome Reduction in Transplantation trial. Circulation 2011, 123, 1763–1770. [Google Scholar] [CrossRef] [PubMed]
- Qin, X.; Huo, Y.; Langman, C.B.; Hou, F.; Chen, Y.; Matossian, D.; Xu, X.; Wang, X. Folic acid therapy and cardiovascular disease in ESRD or advanced chronic kidney disease: A meta-analysis. Clin. J. Am. Soc. Nephrol. 2011, 6, 482–488. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D.M.; Threlfall, G.; Buck, A.T. Stimulation of renal growth in the rat by folic acid. Nature 1966, 212, 472–474. [Google Scholar] [CrossRef] [PubMed]
- Threlfall, G.; Taylor, D.M.; Buck, A.T. Studies of the changes in growth and DNA synthesis in the rat kidney during experimentally induced renal hypertrophy. Am. J. Pathol. 1967, 50, 1–14. [Google Scholar] [PubMed]
- Threlfall, G.; Taylor, D.M.; Buck, A.T. The effect of folic acid on growth and deoxyribonucleic acid synthesis in the rat kidney. Lab. Investig. 1966, 15, 1477–1485. [Google Scholar]
- Fontecha-Barriuso, M.; Martin-Sanchez, D.; Martinez-Moreno, J.M.; Carrasco, S.; Ruiz-Andres, O.; Monsalve, M.; Sanchez-Ramos, C.; Gomez, M.J.; Ruiz-Ortega, M.; Sanchez-Nino, M.D.; et al. PGC-1alpha deficiency causes spontaneous kidney inflammation and increases the severity of nephrotoxic AKI. J. Pathol. 2019, 249, 65–78. [Google Scholar] [CrossRef]
- Fu, H.; Zhou, D.; Zhu, H.; Liao, J.; Lin, L.; Hong, X.; Hou, F.F.; Liu, Y. Matrix metalloproteinase-7 protects against acute kidney injury by priming renal tubules for survival and regeneration. Kidney Int. 2019, 95, 1167–1180. [Google Scholar] [CrossRef]
- Li, Y.; Hu, Q.; Li, C.; Liang, K.; Xiang, Y.; Hsiao, H.; Nguyen, T.K.; Park, P.K.; Egranov, S.D.; Ambati, C.R.; et al. PTEN-induced partial epithelial-mesenchymal transition drives diabetic kidney disease. J. Clin. Investig. 2019, 129, 1129–1151. [Google Scholar] [CrossRef]
- Aparicio-Trejo, O.E.; Reyes-Fermin, L.M.; Briones-Herrera, A.; Tapia, E.; Leon-Contreras, J.C.; Hernandez-Pando, R.; Sanchez-Lozada, L.G.; Pedraza-Chaverri, J. Protective effects of N-acetyl-cysteine in mitochondria bioenergetics, oxidative stress, dynamics and S-glutathionylation alterations in acute kidney damage induced by folic acid. Free Radic. Biol. Med. 2019, 130, 379–396. [Google Scholar] [CrossRef] [PubMed]
- Brade, W.; Herken, H.; Merker, H.J. Regeneration of renal tubular cells after lesion by temporary ischaemia, folic acid, and 2,4,5-triamino 6-styrylpyrimidine. Naunyn Schmiedebergs Arch. Pharmakol. 1970, 266, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Byrnes, K.A.; Ghidoni, J.J.; Suzuki, M.; Thomas, H.; Mayfield, E.D., Jr. Response of the rat kidney to folic acid administration. II. Morphologic studies. Lab. Investig. 1972, 26, 191–200. [Google Scholar] [PubMed]
- Schmidt, U.; Torhorst, J.; Huguenin, M.; Dubach, U.C. Acute renal failure after folate: NaK ATPase in isolated rat renal tubule. Ultramicrochemical and clinical studies. Eur. J. Clin. Investig. 1973, 3, 169–178. [Google Scholar] [CrossRef]
- Jiang, K.; Ponzo, T.A.; Tang, H.; Mishra, P.K.; Macura, S.I.; Lerman, L.O. Multiparametric MRI detects longitudinal evolution of folic acid-induced nephropathy in mice. Am. J. Physiol. Ren. Physiol. 2018, 315, F1252–F1260. [Google Scholar] [CrossRef]
- Ortiz, A.; Husi, H.; Gonzalez-Lafuente, L.; Valino-Rivas, L.; Fresno, M.; Sanz, A.B.; Mullen, W.; Albalat, A.; Mezzano, S.; Vlahou, T.; et al. Mitogen-Activated Protein Kinase 14 Promotes AKI. J. Am. Soc. Nephrol. JASN 2017, 28, 823–836. [Google Scholar] [CrossRef]
- Husi, H.; Sanchez-Nino, M.D.; Delles, C.; Mullen, W.; Vlahou, A.; Ortiz, A.; Mischak, H. A combinatorial approach of Proteomics and Systems Biology in unravelling the mechanisms of acute kidney injury (AKI): Involvement of NMDA receptor GRIN1 in murine AKI. BMC Syst. Biol. 2013, 7, 110. [Google Scholar] [CrossRef]
- Petorak, I.; Imren, H.; Iplikci, A.; Turan, O. The occurrence of lipid droplets in the proximal and distal tubules of the rat kidney after folic acid treatment. Exp. Pathol. (Jena) 1979, 17, 208–214. [Google Scholar] [CrossRef]
- Tang, D.; Kang, R.; Berghe, T.V.; Vandenabeele, P.; Kroemer, G. The molecular machinery of regulated cell death. Cell Res. 2019, 29, 347–364. [Google Scholar] [CrossRef]
- Martin-Sanchez, D.; Ruiz-Andres, O.; Poveda, J.; Carrasco, S.; Cannata-Ortiz, P.; Sanchez-Nino, M.D.; Ruiz Ortega, M.; Egido, J.; Linkermann, A.; Ortiz, A.; et al. Ferroptosis, but Not Necroptosis, Is Important in Nephrotoxic Folic Acid-Induced AKI. J. Am. Soc. Nephrol. JASN 2017, 28, 218–229. [Google Scholar] [CrossRef]
- Mou, Y.; Wang, J.; Wu, J.; He, D.; Zhang, C.; Duan, C.; Li, B. Ferroptosis, a new form of cell death: Opportunities and challenges in cancer. J. Hematol. Oncol. 2019, 12, 34. [Google Scholar] [CrossRef] [PubMed]
- Martin-Sanchez, D.; Fontecha-Barriuso, M.; Carrasco, S.; Sanchez-Nino, M.D.; Massenhausen, A.V.; Linkermann, A.; Cannata-Ortiz, P.; Ruiz-Ortega, M.; Egido, J.; Ortiz, A.; et al. TWEAK and RIPK1 mediate a second wave of cell death during AKI. Proc. Natl. Acad. Sci. USA 2018, 115, 4182–4187. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Xiao, W.; Lee, K.; Salem, F.; Wen, J.; He, L.; Zhang, J.; Fei, Y.; Cheng, D.; Bao, H.; et al. Inhibition of Reticulon-1A-Mediated Endoplasmic Reticulum Stress in Early AKI Attenuates Renal Fibrosis Development. J. Am. Soc. Nephrol. JASN 2017, 28, 2007–2021. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, K.; Habu, S.; Ueda, J. Effects of folic acid on glucose-6-phosphate dehydrogenase and renin activities of the rat kidney. Osaka City Med. J. 1974, 20, 23–31. [Google Scholar] [PubMed]
- Jiang, C.; Zhu, W.; Yan, X.; Shao, Q.; Xu, B.; Zhang, M.; Gong, R. Rescue therapy with Tanshinone IIA hinders transition of acute kidney injury to chronic kidney disease via targeting GSK3beta. Sci. Rep. 2016, 6, 36698. [Google Scholar] [CrossRef] [PubMed]
- Stallons, L.J.; Whitaker, R.M.; Schnellmann, R.G. Suppressed mitochondrial biogenesis in folic acid-induced acute kidney injury and early fibrosis. Toxicol. Lett. 2014, 224, 326–332. [Google Scholar] [CrossRef]
- Craciun, F.L.; Bijol, V.; Ajay, A.K.; Rao, P.; Kumar, R.K.; Hutchinson, J.; Hofmann, O.; Joshi, N.; Luyendyk, J.P.; Kusebauch, U.; et al. RNA Sequencing Identifies Novel Translational Biomarkers of Kidney Fibrosis. J. Am. Soc. Nephrol. JASN 2016, 27, 1702–1713. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.T.; Li, X.Z.; Pitera, J.E.; Long, D.A.; Woolf, A.S. Peritubular capillary loss after mouse acute nephrotoxicity correlates with down-regulation of vascular endothelial growth factor-A and hypoxia-inducible factor-1 alpha. Am. J. Pathol. 2003, 163, 2289–2301. [Google Scholar] [CrossRef]
- Parker, N.; Turk, M.J.; Westrick, E.; Lewis, J.D.; Low, P.S.; Leamon, C.P. Folate receptor expression in carcinomas and normal tissues determined by a quantitative radioligand binding assay. Anal. Biochem. 2005, 338, 284–293. [Google Scholar] [CrossRef]
- Holm, J.; Hansen, S.I.; Hoier-Madsen, M.; Bostad, L. High-affinity folate binding in human choroid plexus. Characterization of radioligand binding, immunoreactivity, molecular heterogeneity and hydrophobic domain of the binding protein. Biochem. J. 1991, 280 Pt 1, 267–271. [Google Scholar] [CrossRef]
- Antony, A.C.; Utley, C.; Van Horne, K.C.; Kolhouse, J.F. Isolation and characterization of a folate receptor from human placenta. J. Biol. Chem. 1981, 256, 9684–9692. [Google Scholar] [PubMed]
- Grapp, M.; Wrede, A.; Schweizer, M.; Huwel, S.; Galla, H.J.; Snaidero, N.; Simons, M.; Buckers, J.; Low, P.S.; Urlaub, H.; et al. Choroid plexus transcytosis and exosome shuttling deliver folate into brain parenchyma. Nat. Commun. 2013, 4, 2123. [Google Scholar] [CrossRef] [PubMed]
- Reddy, J.A.; Dorton, R.; Westrick, E.; Dawson, A.; Smith, T.; Xu, L.C.; Vetzel, M.; Kleindl, P.; Vlahov, I.R.; Leamon, C.P. Preclinical evaluation of EC145, a folate-vinca alkaloid conjugate. Cancer Res. 2007, 67, 4434–4442. [Google Scholar] [CrossRef] [PubMed]
- Lorusso, P.M.; Edelman, M.J.; Bever, S.L.; Forman, K.M.; Pilat, M.; Quinn, M.F.; Li, J.; Heath, E.I.; Malburg, L.M.; Klein, P.J.; et al. Phase I study of folate conjugate EC145 (Vintafolide) in patients with refractory solid tumors. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2012, 30, 4011–4016. [Google Scholar] [CrossRef] [PubMed]
- Naumann, R.W.; Coleman, R.L.; Burger, R.A.; Sausville, E.A.; Kutarska, E.; Ghamande, S.A.; Gabrail, N.Y.; Depasquale, S.E.; Nowara, E.; Gilbert, L.; et al. PRECEDENT: A randomized phase II trial comparing vintafolide (EC145) and pegylated liposomal doxorubicin (PLD) in combination versus PLD alone in patients with platinum-resistant ovarian cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2013, 31, 4400–4406. [Google Scholar] [CrossRef]
- Leamon, C.P.; Reddy, J.A.; Vlahov, I.R.; Kleindl, P.J.; Vetzel, M.; Westrick, E. Synthesis and biological evaluation of EC140: A novel folate-targeted vinca alkaloid conjugate. Bioconjug Chem. 2006, 17, 1226–1232. [Google Scholar] [CrossRef] [PubMed]
- Reddy, J.A.; Westrick, E.; Santhapuram, H.K.; Howard, S.J.; Miller, M.L.; Vetzel, M.; Vlahov, I.; Chari, R.V.; Goldmacher, V.S.; Leamon, C.P. Folate receptor-specific antitumor activity of EC131, a folate-maytansinoid conjugate. Cancer Res. 2007, 67, 6376–6382. [Google Scholar] [CrossRef]
- Leamon, C.P.; Reddy, J.A.; Vetzel, M.; Dorton, R.; Westrick, E.; Parker, N.; Wang, Y.; Vlahov, I. Folate targeting enables durable and specific antitumor responses from a therapeutically null tubulysin B analogue. Cancer Res. 2008, 68, 9839–9844. [Google Scholar] [CrossRef]
- Leamon, C.P.; Reddy, J.A. Folate-targeted chemotherapy. Adv. Drug Deliv. Rev. 2004, 56, 1127–1141. [Google Scholar] [CrossRef]
- Reddy, J.A.; Xu, L.C.; Parker, N.; Vetzel, M.; Leamon, C.P. Preclinical evaluation of (99m)Tc-EC20 for imaging folate receptor-positive tumors. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 2004, 45, 857–866. [Google Scholar]
- Muller, C.; Hohn, A.; Schubiger, P.A.; Schibli, R. Preclinical evaluation of novel organometallic 99mTc-folate and 99mTc-pteroate radiotracers for folate receptor-positive tumour targeting. Eur. J. Nucl. Med. Mol. Imaging 2006, 33, 1007–1016. [Google Scholar] [CrossRef] [PubMed]
- Zhao, R.; Visentin, M.; Goldman, I.D. Determinants of the activities of antifolates delivered into cells by folate-receptor-mediated endocytosis. Cancer Chemother. Pharmacol. 2015, 75, 1163–1173. [Google Scholar] [CrossRef] [PubMed]
- Muller, C.; Bruhlmeier, M.; Schubiger, P.A.; Schibli, R. Effects of antifolate drugs on the cellular uptake of radiofolates in vitro and in vivo. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 2006, 47, 2057–2064. [Google Scholar]
- Muller, C.; Mindt, T.L.; de Jong, M.; Schibli, R. Evaluation of a novel radiofolate in tumour-bearing mice: Promising prospects for folate-based radionuclide therapy. Eur. J. Nucl. Med. Mol. Imaging 2009, 36, 938–946. [Google Scholar] [CrossRef] [PubMed]
- Muller, C.; Schibli, R.; Forrer, F.; Krenning, E.P.; de Jong, M. Dose-dependent effects of (anti)folate preinjection on 99mTc-radiofolate uptake in tumors and kidneys. Nucl. Med. Biol. 2007, 34, 603–608. [Google Scholar] [CrossRef] [PubMed]
- Muller, C.; Reddy, J.A.; Leamon, C.P.; Schibli, R. Effects of the antifolates pemetrexed and CB3717 on the tissue distribution of (99m)Tc-EC20 in xenografted and syngeneic tumor-bearing mice. Mol. Pharm. 2010, 7, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Reber, J.; Struthers, H.; Betzel, T.; Hohn, A.; Schibli, R.; Muller, C. Radioiodinated folic acid conjugates: Evaluation of a valuable concept to improve tumor-to-background contrast. Mol. Pharm. 2012, 9, 1213–1221. [Google Scholar] [CrossRef] [PubMed]
- Ghata, J.; Cowley, B.D., Jr. Polycystic Kidney Disease. Compr. Physiol. 2017, 7, 945–975. [Google Scholar] [PubMed]
- Torres, V.E.; Abebe, K.Z.; Chapman, A.B.; Schrier, R.W.; Braun, W.E.; Steinman, T.I.; Winklhofer, F.T.; Brosnahan, G.; Czarnecki, P.G.; Hogan, M.C.; et al. Angiotensin blockade in late autosomal dominant polycystic kidney disease. N. Engl. J. Med. 2014, 371, 2267–2276. [Google Scholar] [CrossRef] [PubMed]
- Torres, V.E.; Chapman, A.B.; Devuyst, O.; Gansevoort, R.T.; Grantham, J.J.; Higashihara, E.; Perrone, R.D.; Krasa, H.B.; Ouyang, J.; Czerwiec, F.S.; et al. Tolvaptan in patients with autosomal dominant polycystic kidney disease. N. Engl. J. Med. 2012, 367, 2407–2418. [Google Scholar] [CrossRef]
- Tao, Y.; Kim, J.; Schrier, R.W.; Edelstein, C.L. Rapamycin markedly slows disease progression in a rat model of polycystic kidney disease. J. Am. Soc. Nephrol. JASN 2005, 16, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Wahl, P.R.; Serra, A.L.; Le Hir, M.; Molle, K.D.; Hall, M.N.; Wuthrich, R.P. Inhibition of mTOR with sirolimus slows disease progression in Han:SPRD rats with autosomal dominant polycystic kidney disease (ADPKD). Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc.-Eur. Ren. Assoc. 2006, 21, 598–604. [Google Scholar] [CrossRef] [PubMed]
- Shillingford, J.M.; Murcia, N.S.; Larson, C.H.; Low, S.H.; Hedgepeth, R.; Brown, N.; Flask, C.A.; Novick, A.C.; Goldfarb, D.A.; Kramer-Zucker, A.; et al. The mTOR pathway is regulated by polycystin-1, and its inhibition reverses renal cystogenesis in polycystic kidney disease. Proc. Natl. Acad. Sci. USA 2006, 103, 5466–5471. [Google Scholar] [CrossRef] [PubMed]
- Serra, A.L.; Poster, D.; Kistler, A.D.; Krauer, F.; Raina, S.; Young, J.; Rentsch, K.M.; Spanaus, K.S.; Senn, O.; Kristanto, P.; et al. Sirolimus and kidney growth in autosomal dominant polycystic kidney disease. N. Engl. J. Med. 2010, 363, 820–829. [Google Scholar] [CrossRef] [PubMed]
- Walz, G.; Budde, K.; Mannaa, M.; Nurnberger, J.; Wanner, C.; Sommerer, C.; Kunzendorf, U.; Banas, B.; Horl, W.H.; Obermuller, N.; et al. Everolimus in patients with autosomal dominant polycystic kidney disease. N. Engl. J. Med. 2010, 363, 830–840. [Google Scholar] [CrossRef] [PubMed]
- Watnick, T.; Germino, G.G. mTOR inhibitors in polycystic kidney disease. N. Engl. J. Med. 2010, 363, 879–881. [Google Scholar] [CrossRef] [PubMed]
- Shillingford, J.M.; Leamon, C.P.; Vlahov, I.R.; Weimbs, T. Folate-conjugated rapamycin slows progression of polycystic kidney disease. J. Am. Soc. Nephrol. JASN 2012, 23, 1674–1681. [Google Scholar] [CrossRef]
- Kipp, K.R.; Kruger, S.L.; Schimmel, M.F.; Parker, N.; Shillingford, J.M.; Leamon, C.P.; Weimbs, T. Comparison of folate-conjugated rapamycin versus unconjugated rapamycin in an orthologous mouse model of polycystic kidney disease. Am. J. Physiol. Ren. Physiol. 2018, 315, F395–F405. [Google Scholar] [CrossRef]
- Shi, H.; Leonhard, W.N.; Sijbrandi, N.J.; van Steenbergen, M.J.; Fens, M.; van de Dikkenberg, J.B.; Torano, J.S.; Peters, D.J.M.; Hennink, W.E.; Kok, R.J. Folate-dactolisib conjugates for targeting tubular cells in polycystic kidneys. J. Control. Release Off. J. Control. Release Soc. 2019, 293, 113–125. [Google Scholar] [CrossRef]
- Chandrupatla, D.; Molthoff, C.F.M.; Lammertsma, A.A.; van der Laken, C.J.; Jansen, G. The folate receptor beta as a macrophage-mediated imaging and therapeutic target in rheumatoid arthritis. Drug Deliv. Transl. Res. 2019, 9, 366–378. [Google Scholar] [CrossRef]
- Chu, H.; Shillingford, J.M.; Reddy, J.A.; Westrick, E.; Nelson, M.; Parker, N.; Felten, A.E.; Vaughn, J.F.; Xu, L.C.; Lu, Y.J.; et al. Detecting Functional and Accessible Folate Receptor Expression in Cancer and Polycystic Kidneys. Mol. Pharm. 2019, 16, 3985–3995. [Google Scholar] [CrossRef] [PubMed]

© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Samodelov, S.L.; Gai, Z.; Kullak-Ublick, G.A.; Visentin, M. Renal Reabsorption of Folates: Pharmacological and Toxicological Snapshots. Nutrients 2019, 11, 2353. https://doi.org/10.3390/nu11102353
Samodelov SL, Gai Z, Kullak-Ublick GA, Visentin M. Renal Reabsorption of Folates: Pharmacological and Toxicological Snapshots. Nutrients. 2019; 11(10):2353. https://doi.org/10.3390/nu11102353
Chicago/Turabian StyleSamodelov, Sophia L, Zhibo Gai, Gerd A Kullak-Ublick, and Michele Visentin. 2019. "Renal Reabsorption of Folates: Pharmacological and Toxicological Snapshots" Nutrients 11, no. 10: 2353. https://doi.org/10.3390/nu11102353
APA StyleSamodelov, S. L., Gai, Z., Kullak-Ublick, G. A., & Visentin, M. (2019). Renal Reabsorption of Folates: Pharmacological and Toxicological Snapshots. Nutrients, 11(10), 2353. https://doi.org/10.3390/nu11102353



