Relative Protein Intake and Physical Function in Older Adults: A Systematic Review and Meta-Analysis of Observational Studies
Abstract
1. Introduction
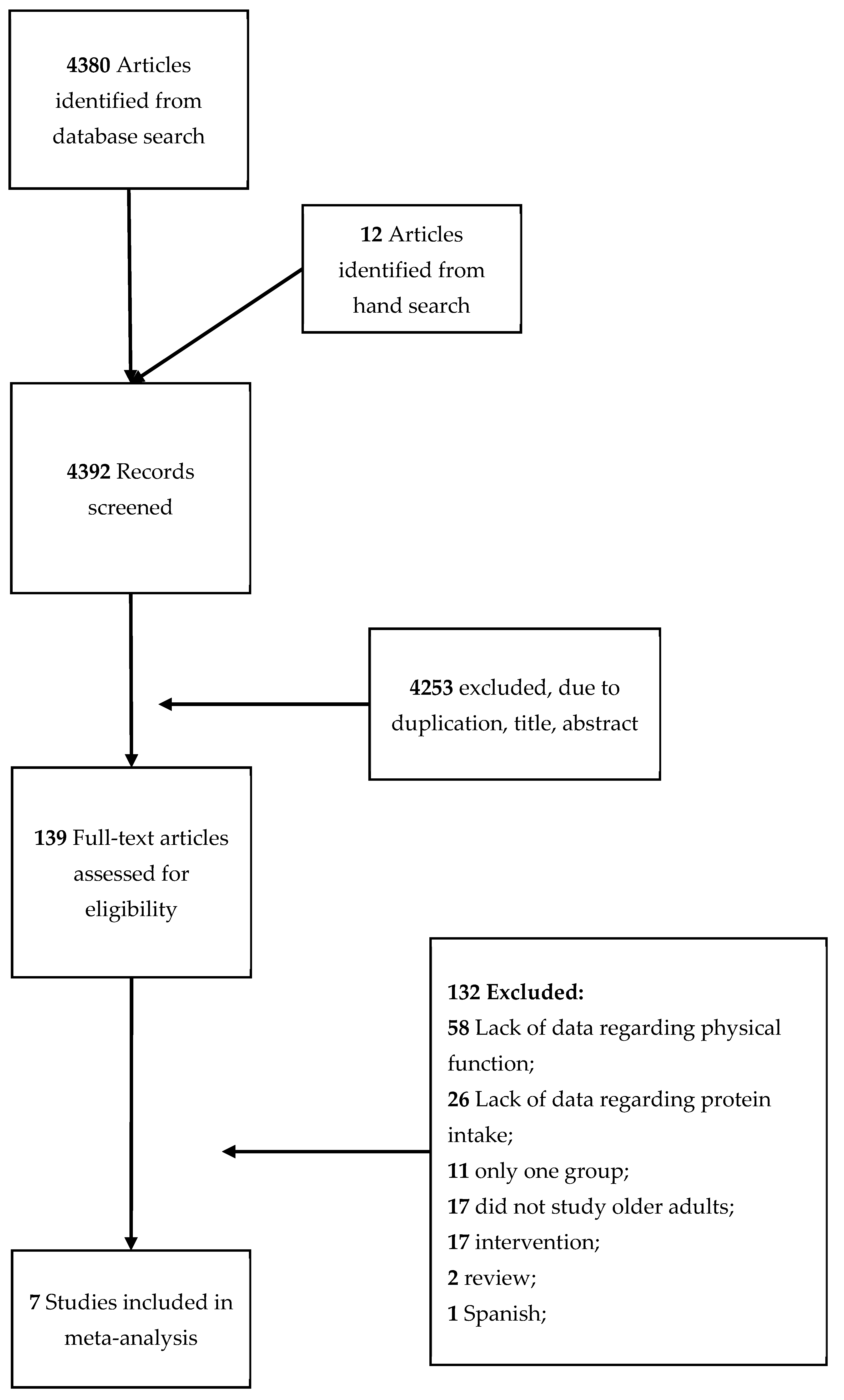
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy and Selection Criteria
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analysis
3. Results
3.1. Characteristics and Quality of Included Studies
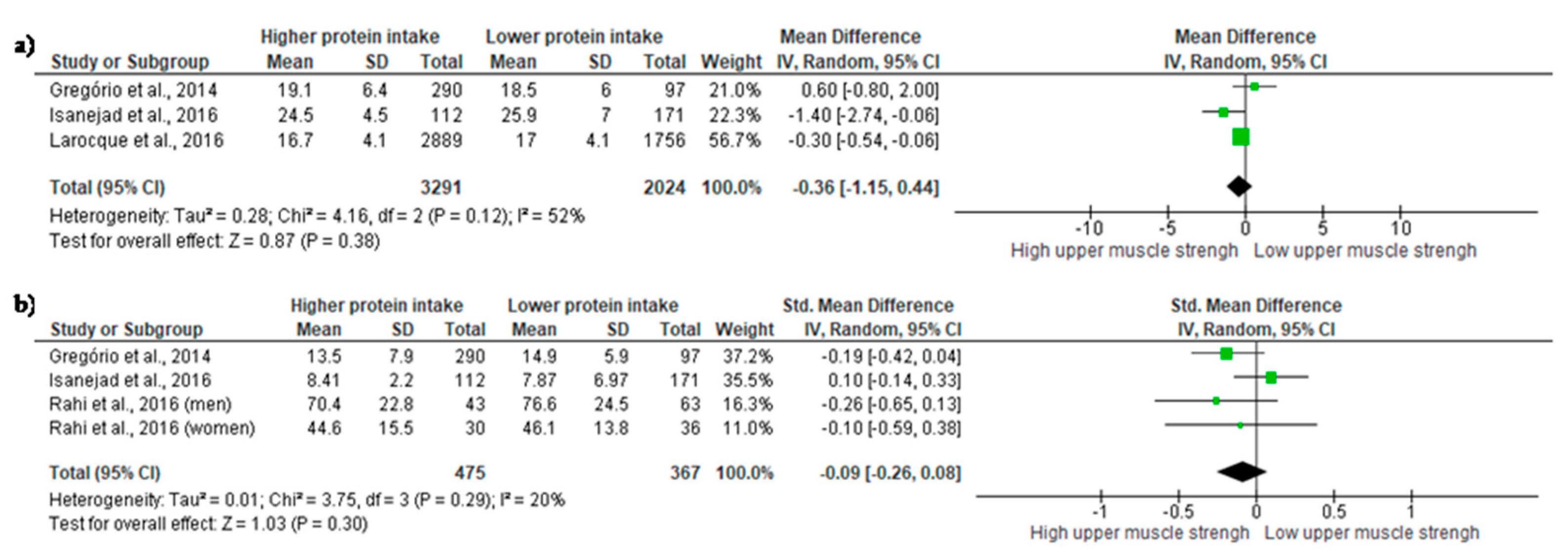
3.2. High Protein Intake verses Low Protein Intake
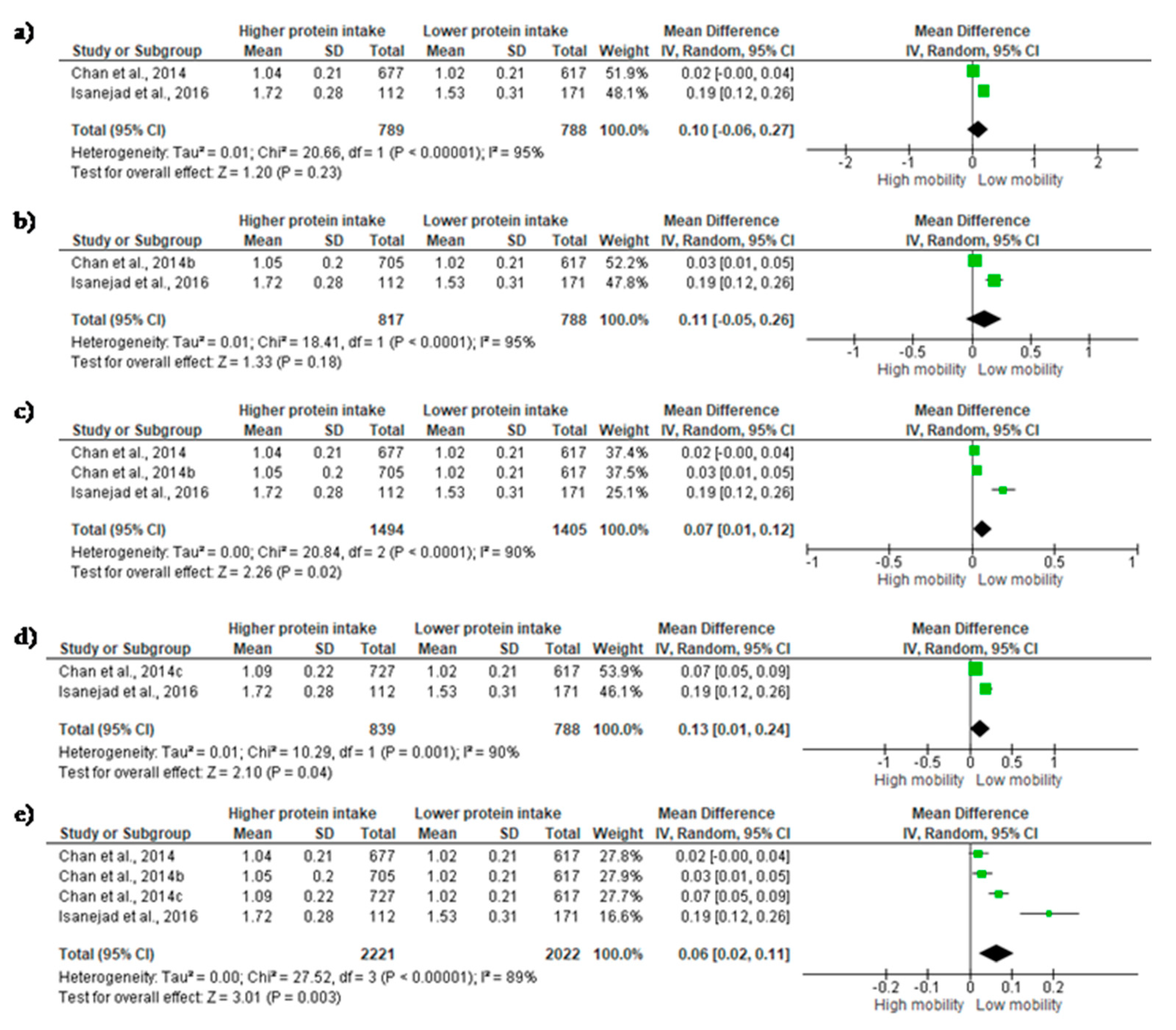
3.3. Mobility
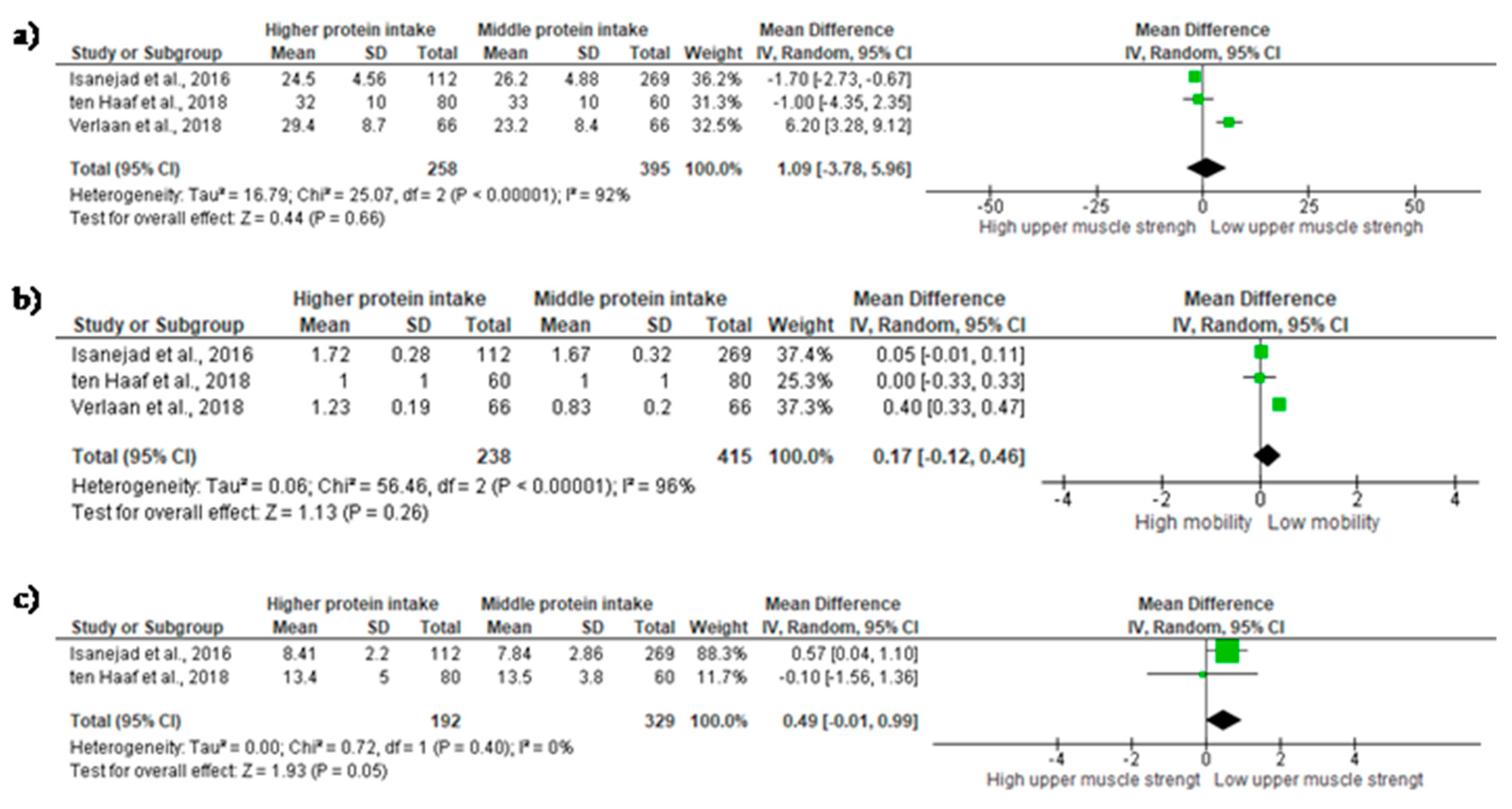
3.4. Middle Protein Intake verses High Protein Intake
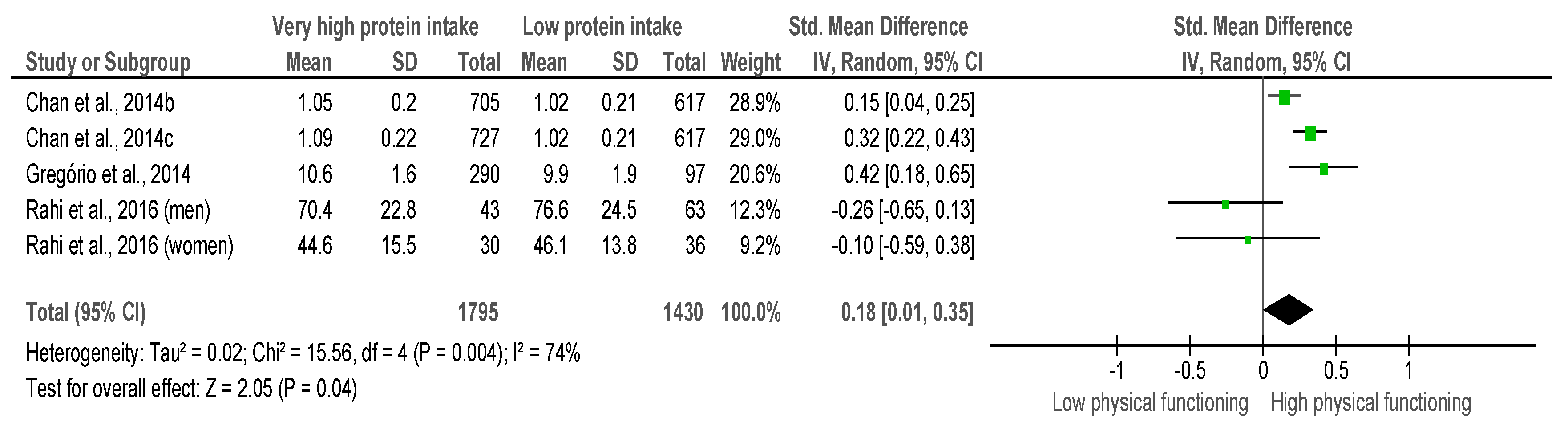
3.5. Very High Protein Intake verses Low Protein Intake
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.-P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European working group on sarcopenia in older people. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [PubMed]
- Diz, J.B.M.; Leopoldino, A.A.O.; Moreira, B.D.S.; Henschke, N.; Dias, R.C.; Pereira, L.S.M.; Oliveira, V.C. Prevalence of sarcopenia in older Brazilians: A systematic review and meta-analysis. Geriatr. Gerontol. Int. 2017, 17, 5–16. [Google Scholar] [CrossRef] [PubMed]
- Coelho Júnior, H.J.; Aguiar, S.D.S.; Gonçalves, I.D.O.; Sampaio, R.A.C.; Uchida, M.C.; Moraes, M.R.; Asano, R.Y. Sarcopenia is associated with high pulse pressure in older women. J. Aging Res. 2015, 2015. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Lim, S.; Choi, S.H.; Kim, K.M.; Yoon, J.W.; Kim, K.W.; Lim, J.-Y.; Park, K.S.; Jang, H.C.; Kritchevsky, S. Sarcopenia: An independent predictor of mortality in community-dwelling older Korean men. J. Gerontol. Ser. A 2014, 69, 1244–1252. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.C.; Harhay, M.O.; Harhay, M.N. Sarcopenia and mortality among a population-based sample of community-dwelling older adults. J. Cachexia. Sarcopenia Muscle 2016, 7, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Benjumea, A.-M.; Curcio, C.-L.; Duque, G.; Gómez, F. Dynapenia and sarcopenia as a risk factor for disability in a falls and fractures clinic in older persons. Open Access Maced. J. Med. Sci. 2018, 6, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Martone, A.M.; Marzetti, E.; Calvani, R.; Picca, A.; Tosato, M.; Santoro, L.; Di Giorgio, A.; Nesci, A.; Sisto, A.; Santoliquido, A.; et al. Exercise and protein intake: A synergistic approach against sarcopenia. BioMed Res. Int. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Marzetti, E.; Calvani, R.; Tosato, M.; Cesari, M.; Di Bari, M.; Cherubini, A.; Collamati, A.; D’Angelo, E.; Pahor, M.; Bernabei, R.; et al. SPRINTT consortium sarcopenia: An overview. Aging Clin. Exp. Res. 2017, 29, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Nutrient Reference Values. Available online: https://www.nrv.gov.au/nutrients/protein (accessed on 26 August 2018).
- Protein—British Nutrition Foundation. Available online: https://www.nutrition.org.uk/nutritionscience/nutrients-food-and-ingredients/protein.html?start=1 (accessed on 26 August 2018).
- Volpi, E.; Campbell, W.W.; Dwyer, J.T.; Johnson, M.A.; Jensen, G.L.; Morley, J.E.; Wolfe, R.R. Is the optimal level of protein intake for older adults greater than the recommended dietary allowance? J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2013, 68, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Landi, F.; Calvani, R.; Tosato, M.; Martone, A.M.; Ortolani, E.; Savera, G.; D’Angelo, E.; Sisto, A.; Marzetti, E. Protein intake and muscle health in old age: From biological plausibility to clinical evidence. Nutrients 2016, 8, 295. [Google Scholar] [CrossRef] [PubMed]
- Bauer, J.; Biolo, G.; Cederholm, T.; Cesari, M.; Cruz-Jentoft, A.J.; Morley, J.E.; Phillips, S.; Sieber, C.; Stehle, P.; Teta, D.; et al. Evidence-based recommendations for optimal dietary protein intake in older people: A position paper from the prot-age study group. J. Am. Med. Dir. Assoc. 2013, 14, 542–559. [Google Scholar] [CrossRef] [PubMed]
- Calvani, R.; Miccheli, A.; Landi, F.; Bossola, M.; Cesari, M.; Leeuwenburgh, C.; Sieber, C.C.; Bernabei, R.; Marzetti, E. Current nutritional recommendations and novel dietary strategies to manage sarcopenia. J. Frailty Aging 2013, 2, 38–53. [Google Scholar] [PubMed]
- Bartali, B.; Frongillo, E.A.; Bandinelli, S.; Lauretani, F.; Semba, R.D.; Fried, L.P.; Ferrucci, L. Low nutrient intake is an essential component of frailty in older persons. J. Gerontol. A. Biol. Sci. Med. Sci. 2006, 61, 589–593. [Google Scholar] [CrossRef] [PubMed]
- Lana, A.; Rodriguez-Artalejo, F.; Lopez-Garcia, E. Dairy consumption and risk of frailty in older adults: A prospective cohort study. J. Am. Geriatr. Soc. 2015, 63, 1852–1860. [Google Scholar] [CrossRef] [PubMed]
- Isanejad, M.; Mursu, J.; Sirola, J.; Kröger, H.; Rikkonen, T.; Tuppurainen, M.; Erkkilä, A.T. Dietary protein intake is associated with better physical function and muscle strength among elderly women. Br. J. Nutr. 2016, 115, 1281–1291. [Google Scholar] [CrossRef] [PubMed]
- Houston, D.K.; Schwartz, A.V.; Cauley, J.A.; Tylavsky, F.A.; Simonsick, E.M.; Harris, T.B.; De Rekeneire, N.; Schwartz, G.G.; Kritchevsky, S.B. Serum parathyroid hormone levels predict falls in older adults with diabetes mellitus. J. Am. Geriatr. Soc. 2008, 56, 2027–2032. [Google Scholar] [CrossRef] [PubMed]
- Farsijani, S.; Payette, H.; Morais, J.A.; Shatenstein, B.; Gaudreau, P.; Chevalier, S. Even mealtime distribution of protein intake is associated with greater muscle strength, but not with 3-y physical function decline, in free-living older adults: The quebec longitudinal study on nutrition as a determinant of successful aging (NuAge study). Am. J. Clin. Nutr. 2017, 106, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Gregorio, L.; Brindisi, J.; Kleppinger, A.; Sullivan, R.; Mangano, K.M.; Bihuniak, J.D.; Kenny, A.M.; Kerstetter, J.E.; Insogna, K.L. Adequate dietary protein is associated with better physical performance among post-menopausal women 60–90 years. J. Nutr. Health Aging 2014, 18, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Verlaan, S.; Aspray, T.J.; Bauer, J.M.; Cederholm, T.; Hemsworth, J.; Hill, T.R.; McPhee, J.S.; Piasecki, M.; Seal, C.; Sieber, C.C.; et al. Nutritional status, body composition, and quality of life in community-dwelling sarcopenic and non-sarcopenic older adults: A case-control study. Clin. Nutr. 2017, 36, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- Houston, D.K.; Nicklas, B.J.; Ding, J.; Harris, T.B.; Tylavsky, F.A.; Newman, A.B.; Lee, J.S.; Sahyoun, N.R.; Visser, M.; Kritchevsky, S.B. Health ABC study dietary protein intake is associated with lean mass change in older, community-dwelling adults: The health, aging, and body composition (Health ABC) study. Am. J. Clin. Nutr. 2008, 87, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Beasley, J.M.; Lacroix, A.Z.; Neuhouser, M.L.; Huang, Y.; Tinker, L.; Woods, N.; Michael, Y.; Curb, J.D.; Prentice, R.L. Protein intake and incident frailty in the women’s health initiative observational study. J. Am. Geriatr. Soc. 2010, 58, 1063–1071. [Google Scholar] [CrossRef] [PubMed]
- Vellas, B.J.; Hunt, W.C.; Romero, L.J.; Koehler, K.M.; Baumgartner, R.N.; Garry, P.J. Changes in nutritional status and patterns of morbidity among free-living elderly persons: A 10-year longitudinal study. Nutrition 1997, 13, 515–519. [Google Scholar] [CrossRef]
- Mustafa, J.; Ellison, R.C.; Singer, M.R.; Bradlee, M.L.; Kalesan, B.; Holick, M.F.; Moore, L.L. Dietary protein and preservation of physical functioning among middle-aged and older adults in the framingham offspring study. Am. J. Epidemiol. 2018, 187, 1411–1419. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Green, S.; Higgins, J. Cochrane Handbook for Systematic Reviews of Interventions; The Cochrane Collaboratrion: London, UK, 2005. [Google Scholar]
- Chan, R.; Leung, J.; Woo, J. Dietary patterns and risk of frailty in Chinese community-dwelling older people in Hong Kong: A prospective cohort study. Nutrients 2015, 7, 7070–7084. [Google Scholar] [CrossRef] [PubMed]
- Larocque, S.C.; Kerstetter, J.E.; Cauley, J.A.; Insogna, K.L.; Ensrud, K.; Lui, L.-Y.; Allore, H.G. Dietary protein and vitamin D intake and risk of falls: A secondary analysis of postmenopausal women from the study of osteoporotic fractures. J. Nutr. Gerontol. Geriatr. 2015, 34, 305–318. [Google Scholar] [CrossRef] [PubMed]
- Rahi, B.; Morais, J.A.; Gaudreau, P.; Payette, H.; Shatenstein, B. Energy and protein intakes and their association with a decline in functional capacity among diabetic older adults from the NuAge cohort. Eur. J. Nutr. 2016, 55, 1729–1739. [Google Scholar] [CrossRef] [PubMed]
- Ten Haaf, D.; van Dongen, E.; Nuijten, M.; Eijsvogels, T.; de Groot, L.; Hopman, M. Protein intake and distribution in relation to physical functioning and quality of life in community-dwelling elderly people: acknowledging the role of physical activity. Nutrients 2018, 10, 506. [Google Scholar] [CrossRef] [PubMed]
- Chan, R.; Leung, J.; Woo, J.; Kwok, T. Associations of dietary protein intake on subsequent decline in muscle mass and physical functions over four years in ambulant older Chinese people. J. Nutr. Health Aging 2014, 18, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Landi, F.; Calvani, R.; Cesari, M.; Tosato, M.; Martone, A.M.; Ortolani, E.; Savera, G.; Salini, S.; Sisto, A.; Picca, A.; et al. Sarcopenia: An overview on current definitions, diagnosis and treatment. Curr. Protein Pept. Sci. 2018, 19, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Katsanos, C.S.; Kobayashi, H.; Sheffield-Moore, M.; Aarsland, A.; Wolfe, R.R. Aging is associated with diminished accretion of muscle proteins after the ingestion of a small bolus of essential amino acids. Am. J. Clin. Nutr. 2005, 82, 1065–1073. [Google Scholar] [CrossRef] [PubMed]
- Katsanos, C.S.; Kobayashi, H.; Sheffield-Moore, M.; Aarsland, A.; Wolfe, R.R. A high proportion of leucine is required for optimal stimulation of the rate of muscle protein synthesis by essential amino acids in the elderly. Am. J. Physiol. Metab. 2006, 291, E381–E387. [Google Scholar] [CrossRef] [PubMed]
- Campbell, W.W.; Trappe, T.A.; Wolfe, R.R.; Evans, W.J. The recommended dietary allowance for protein may not be adequate for older people to maintain skeletal muscle. J. Gerontol. A. Biol. Sci. Med. Sci. 2001, 56, M373–M380. [Google Scholar] [CrossRef] [PubMed]
- Martin, W.F.; Armstrong, L.E.; Rodriguez, N.R. Dietary protein intake and renal function. Nutr. Metab. 2005, 2, 25. [Google Scholar] [CrossRef] [PubMed]
- Hamacher, D.; Herold, F.; Wiegel, P.; Hamacher, D.; Schega, L. Brain activity during walking: A systematic review. Neurosci. Biobehav. Rev. 2015, 57, 310–327. [Google Scholar] [CrossRef] [PubMed]
- Paraskevoudi, N.; Balcı, F.; Vatakis, A. “Walking” through the sensory, cognitive, and temporal degradations of healthy aging. Ann. N. Y. Acad. Sci. 2018. [Google Scholar] [CrossRef] [PubMed]
- EI Khoudary, S.R.; Chen, H.-Y.; Barinas-Mitchell, E.; McClure, C.; Selzer, F.; Karvonen-Gutierrez, C.; Jackson, E.A.; Ylitalo, K.R.; Sternfeld, B. Simple physical performance measures and vascular health in late midlife women: The study of women’s health across the nation. Int. J. Cardiol. 2015, 182, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Su, N.; Zhai, F.-F.; Zhou, L.-X.; Ni, J.; Yao, M.; Li, M.-L.; Jin, Z.-Y.; Gong, G.-L.; Zhang, S.-Y.; Cui, L.-Y.; et al. Cerebral small vessel disease burden is associated with motor performance of lower and upper extremities in community-dwelling populations. Front. Aging Neurosci. 2017, 9, 313. [Google Scholar] [CrossRef] [PubMed]
- Nolan, C.M.; Maddocks, M.; Maher, T.M.; Canavan, J.L.; Jones, S.E.; Barker, R.E.; Patel, S.; Jacob, J.; Cullinan, P.; Man, W.D.-C. Phenotypic characteristics associated with slow gait speed in idiopathic pulmonary fibrosis. Respirology 2018, 23, 498–506. [Google Scholar] [CrossRef] [PubMed]
- Vandervoort, A.A. Aging of the human neuromuscular system. Muscle Nerve 2002, 25, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Rosso, A.L.; Sanders, J.L.; Arnold, A.M.; Boudreau, R.M.; Hirsch, C.H.; Carlson, M.C.; Rosano, C.; Kritchevsky, S.B.; Newman, A.B. Multisystem physiologic impairments and changes in gait speed of older adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2015, 70, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Castro, L.A.; Padilla-Gómez, E.; Parga-Martínez, N.J.; Castro-Rodríguez, D.C.; Quirarte, G.L.; Díaz-Cintra, S.; Nathanielsz, P.W.; Zambrano, E. Hippocampal mechanisms in impaired spatial learning and memory in male offspring of rats fed a low-protein isocaloric diet in pregnancy and/or lactation. Hippocampus 2018, 28, 18–30. [Google Scholar] [CrossRef] [PubMed]
- Madani, Z.; Malaisse, W.J.; Ait-Yahia, D. A comparison between the impact of two types of dietary protein on brain glucose concentrations and oxidative stress in high fructose-induced metabolic syndrome rats. Biomed. Rep. 2015, 3, 731–735. [Google Scholar] [CrossRef] [PubMed]
- Fernando, W.M.A.D.; Rainey-Smith, S.R.; Gardener, S.L.; Villemagne, V.L.; Burnham, S.C.; Macaulay, S.L.; Brown, B.M.; Gupta, V.B.; Sohrabi, H.R.; Weinborn, M.; et al. Associations of dietary protein and fiber intake with brain and blood amyloid-β. J. Alzheimer’s Dis. 2018, 61, 1589–1598. [Google Scholar] [CrossRef] [PubMed]
- Koh, F.; Charlton, K.; Walton, K.; McMahon, A.-T. Role of dietary protein and thiamine intakes on cognitive function in healthy older people: A systematic review. Nutrients 2015, 7, 2415–2439. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Dang, S.; Yan, H.; Wang, D.; Zhao, Y.; Li, Q.; Liu, X. Association between dietary protein intake and the risk of hypertension: A cross-sectional study from rural western China. Hypertens. Res. 2013, 36, 972. [Google Scholar] [CrossRef] [PubMed]
- Tielemans, S.M.A.J.; Altorf-van der Kuil, W.; Engberink, M.F.; Brink, E.J.; van Baak, M.A.; Bakker, S.J.L.; Geleijnse, J.M. Intake of total protein, plant protein and animal protein in relation to blood pressure: A meta-analysis of observational and intervention studies. J. Hum. Hypertens. 2013, 27, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Guligowska, A.; Pigłowska, M.; Fife, E.; Kostka, J.; Sołtysik, B.K.; Kroc, Ł.; Kostka, T. Inappropriate nutrients intake is associated with lower functional status and inferior quality of life in older adults with depression. Clin. Interv. Aging 2016, 11, 1505–1517. [Google Scholar] [CrossRef] [PubMed]
| Year | Authors | Country | Study Design | Population | Setting | Sample Size | Age | Female (%) | BMI | Lean Mass | Appendicular Muscle Mass | Dietary Intake Assessment Method | Total Protein Intake (g/Day) | STROBE Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2018 | ten Haaf et al. | Netherland | Cross-sectional | Healthy | Community-dwelling | HP: 80; LP: 60 | 83.0 | 10 | 26.1 | — | — | 24-h dietary recall | HP: 89.5; LP: 64.7 | 19 |
| 2016 | Isanejad et al. | Finland | Longitudinal | Healthy | Community-dwelling | HP = 112; MP = 269; LP = 171 | 67.8 | 100 | 26.6 | HP: 41.3, 16.4, 6.5; MP:40.1, 15.9, 6.7; LP: 39.1, 15.6, 6.6 | — | 3-day dietary intake record | HP: 83.4; MP:65.0; LP: 51.4 | 20 |
| 2016 | Rahi et al. | Canada | Longitudinal | Diabetic | Community-dwelling | HP: 73; LP: 99 | 75.0 | 62 | 29.5 | — | — | 24-h dietary recall | HP: 91; LP: 64.3 | 20 |
| 2015 | Larocque et al. | United States | Longitudinal | Post-menopausal women | Community-dwelling | LP = 1756; HP = 2889 | 80.1 | 100 | 26.8 | — | — | Food frequency questionnaire | LP = 42.6; HP = 71.6 | 17 |
| 2015 | Verlaan et al. | United Kingdom | Case-control | Sarcopenic and non-sarcopenic | Community-dwelling | Sarcopenic: 66; Non-sarcopenic: 66 | 71.1 | 39 | 26.1 | — | Sarcopenic:19.0; Non-sarcopenic: 20.4 | 3-day dietary intake record | Sarcopenic: 72.5; Non-sarcopenic: 75.3 | 19 |
| 2014 | Chan et al. | China | Longitudinal | Healthy | Community-dwelling | LP = 617; MP =677; HP = 705; HP2 = 727 | 71.6 | 49.8 | 23.7 | — | — | Semi Quantitative-Food Frequency Questionnaire (SQFFQ) | — | 19 |
| 2014 | Gregorio et al. | United States | Cross-sectional | Post-menopausal women | Community-dwelling | LP = 97; HP = 290 | 73.0 | 100 | 27.4 | LP = 40.7; HP = 38.2 | LP = 17.0; HP = 15.9 | 4-day dietary intake record | LP = 49.7; HP = 79.7 | 20 |
| Low Protein Intake (0.67) | Middle Protein Intake (0.88) | High Protein Intake (1.3) | Very High Protein Intake (1.5) | |
|---|---|---|---|---|
| Variables | n = 2641 | n = 395 | n = 5619 | n = 1145 |
| Anthropometric characteristics | ||||
| Age (years) | 73.8 | 74.0 | 74.6 | 73.5 |
| BMI (kg/m2) | 29.1 | 26.7 | 27 | 27.1 |
| Lean Mass (kg) (% in relation to weight) | 41.0 (53) | 40.1 (56.1) | 38.7 (58.7) | 38.2 (58.1) |
| Appendicular Muscle Mass (kg) (% in relation to weight) | — | 19.0 (25.5) | 20.4 (24.7) | 15.9 (24.2) |
| Physical functional tests | ||||
| IHG (kg) | 20.4 | 27.5 | 24.3 | 19.1 |
| Knee Extensor Strength (lb) | 54.5 | 44.5 | 52.1 | 57.5 |
| One-Leg Stand (s) | 13.5 | 19.3 | 18.4 | 15.3 |
| Chair Rises (s) | 11.4 | 10.6 | 11.8 | 13.5 |
| Tandem Walk Speed for 6 m (m/s) | 0.30 | 0.34 | 0.33 | — |
| Usual Walking Speed (m/s) | 1.1 | 1.2 | 1.2 | 1.07 |
| SPPB (points) | 9.9 | 9.0 | 11.0 | 10.6 |
| Timed 8-Foot Walk (m/s) | 1 | — | 1.1 | 1.1 |
| Dietary factors | ||||
| Protein (g/day) | 58.8 | 67.4 | 85.4 | 87.2 |
| Carbohydrate (g/day) | 162.6 | 199.8 | 215.9 | 220.6 |
| Fat (g/day) | 43.6 | 58.6 | 64.4 | — |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coelho-Júnior, H.J.; Milano-Teixeira, L.; Rodrigues, B.; Bacurau, R.; Marzetti, E.; Uchida, M. Relative Protein Intake and Physical Function in Older Adults: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients 2018, 10, 1330. https://doi.org/10.3390/nu10091330
Coelho-Júnior HJ, Milano-Teixeira L, Rodrigues B, Bacurau R, Marzetti E, Uchida M. Relative Protein Intake and Physical Function in Older Adults: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients. 2018; 10(9):1330. https://doi.org/10.3390/nu10091330
Chicago/Turabian StyleCoelho-Júnior, Hélio José, Luiz Milano-Teixeira, Bruno Rodrigues, Reury Bacurau, Emanuele Marzetti, and Marco Uchida. 2018. "Relative Protein Intake and Physical Function in Older Adults: A Systematic Review and Meta-Analysis of Observational Studies" Nutrients 10, no. 9: 1330. https://doi.org/10.3390/nu10091330
APA StyleCoelho-Júnior, H. J., Milano-Teixeira, L., Rodrigues, B., Bacurau, R., Marzetti, E., & Uchida, M. (2018). Relative Protein Intake and Physical Function in Older Adults: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients, 10(9), 1330. https://doi.org/10.3390/nu10091330







