Differential Impact of Malnutrition on Health Outcomes Among Indigenous and Non-Indigenous Adults Admitted to Hospital in Regional Australia—A Prospective Cohort Study
Abstract
1. Introduction
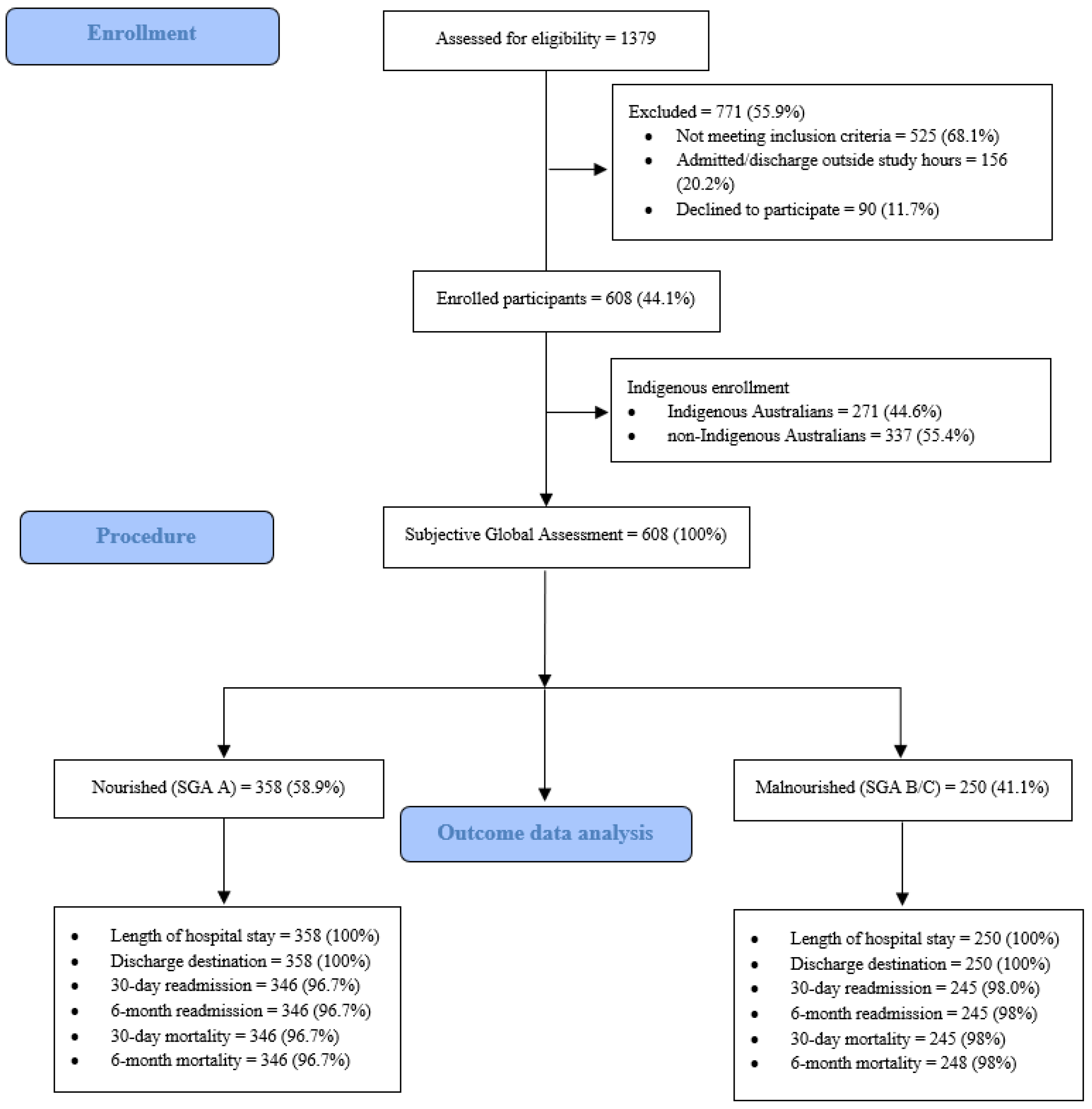
2. Materials and Methods
2.1. Study Design, Setting and Participants
2.2. Nutrion Status and Disease Serverity Outcomes
2.3. Health Outcomes
2.4. Statistical Analysis
2.5. Ethics Approval
3. Results
3.1. Participant Characteristics
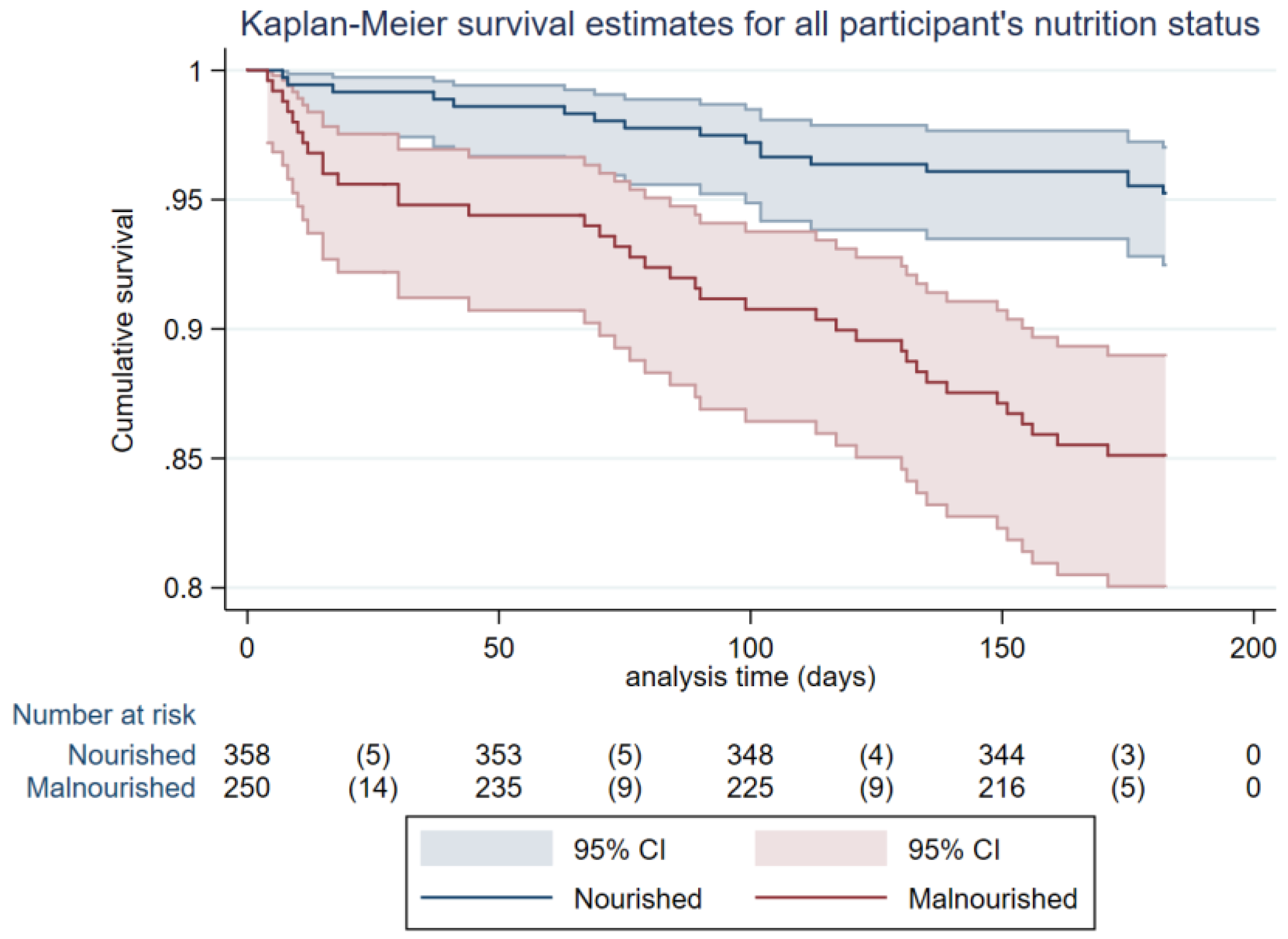
3.2. Health Outcomes for Nourished and Malnoursihed Participants
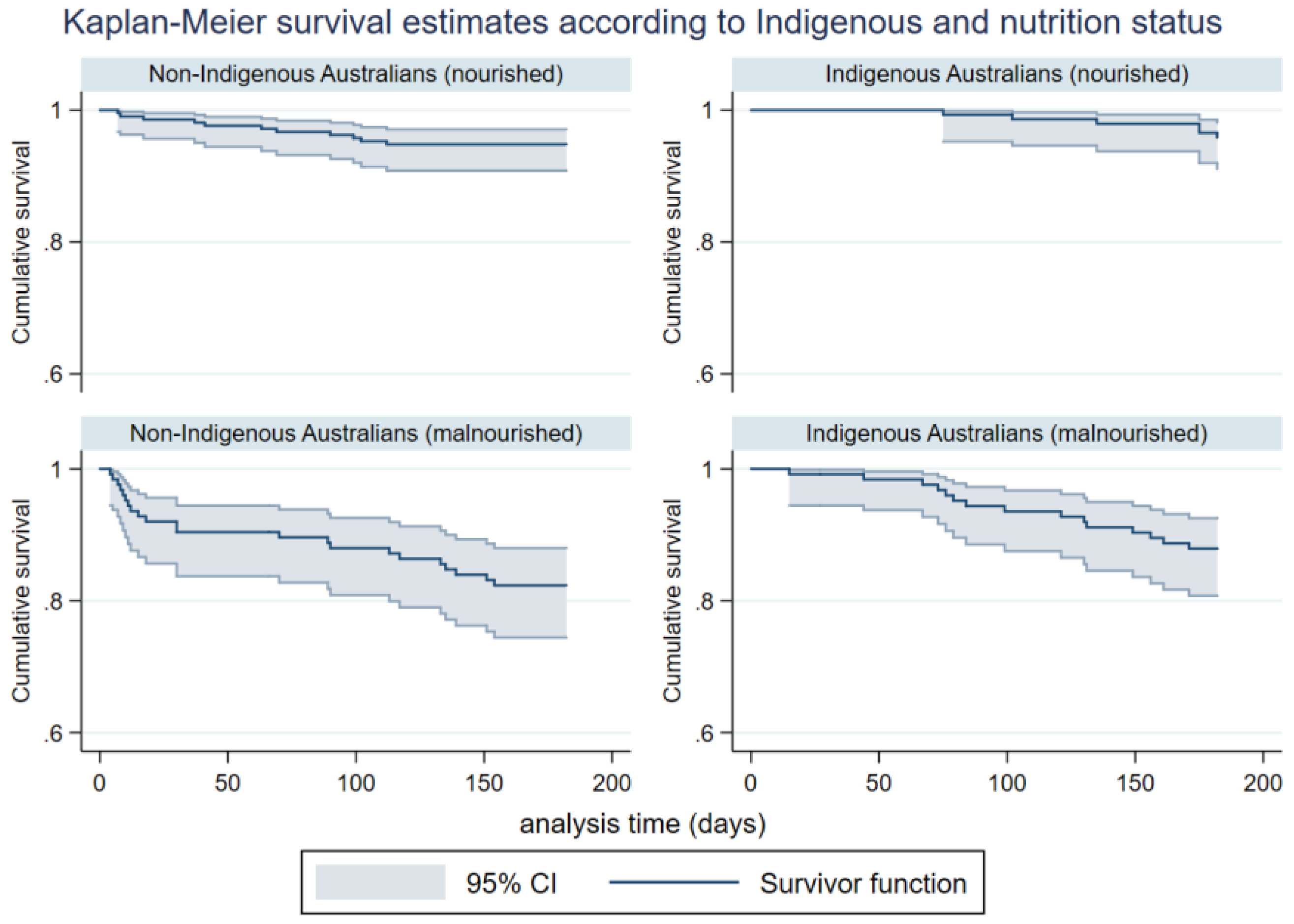
3.3. Health Outcomes Among Indigenous and Non-Indigenous Australian Participants
3.4. Independment Factors Associated with Healthcare Ultisation and Decreased Survival
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Da Silva Frank, J.; Daniel de Mello, P.; Daniel de Melllo, E. Subjective Global Assessment of nutrition status—A systematic review of the literature. Clin. Nutr. 2015, 35, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, E.; Ferguson, M.; Banks, M.; Bauer, J.; Capra, S.; Isenring, E. Malnutrition and poor food intake are associated with prolonged length of hospital stay, frequent readmissions, and greater in-hospital mortality: Results from the Nutrition Care Day survey 2010. Clin. Nutr. 2013, 32, 737–745. [Google Scholar] [CrossRef] [PubMed]
- Van der Schueren, M.A.E. The prevalence of malnutrition according to the new ESPEN definition in four diverse populations. Clin. Nutr. 2016, 35, 758–762. [Google Scholar]
- Lim, S.L.; Ong, K.C.B.; Chan, Y.H.; Loke, W.C.; Ferguson, M.; Daniels, L. Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin. Nutr. 2012, 31, 345–350. [Google Scholar] [CrossRef] [PubMed]
- Allard, J.P.; Keller, H.; Jeejeebhoy, K.N.; Laporte, M.; Duerksen, D.R.; Gramlich, L.; Payette, H.; Bernier, P.; Vesnaver, E.; Davidson, B.; Teterina, A.; Lou, W. Malnutrition at hospital admission-contributors and effect on length of stay: A prospective cohort study from the Canadian Malnutrition Task Force. J. Parenter. Enter. Nutr. 2016, 40, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Australian Government Geoscience Australia. Area of Australia—States and Territories. Commonwealth of Australia. Available online: http://www.ga.gov.au/scientific-topics/national-location-information/dimensions/area-of-australia-states-and-territories (accessed on 3 December 2017).
- Australian Bureau of Statistics. Aboriginal and Torres Strait Islander population. Oct 2017. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/mf/2071.0 (accessed on 3 December 2017).
- Morris, N.F.; Stewart, S.; Riley, M.D.; Maguire, G.P. The burden and nature of malnutrition among patients in regional hospital settings: A cross-sectional survey. Clin. Nutr. ESPEN 2018, 23, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Morris, N.F.; Stewart, S.; Riley, M.; Maguire, G.P. The Indigenous Australian Malnutrition Project: The burden and impact of malnutrition in Aboriginal Australian and Torres Strait Islander hospital inpatients, and validation of a malnutrition screening tool for use in hospitals—Study rationale and protocol. SpringerPlus 2016, 5, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Detsky, A.S.; McLaughlin, J.R.; Baker, J.P.; Johnston, N.; Whittaker, S.; Mendelson, R.A.; Jeejeebhoy, K.N. What is the Subjective Global Assessment of nutritional status? J. Parenter. Enter. Nutr. 1987, 11, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Knaus, W.A.; Wagner, D.P.; Draper, M.S.; Zimmerman, J.E.; Bergner, M.; Bastos, P.G.; Sirio, C.A.; Murphy, D.J.; Lotring, T.; Damiano, A.; et al. The APACHE III prognostic system, Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 1991, 100, 1619–1636. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pomper, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 37–383. [Google Scholar] [CrossRef]
- Northern Territory Government. Births, Deaths and Marriages. 2017 Northern Territory Government of Australia. Available online: https://nt.gov.au/law/bdm (accessed on 3 December 2017).
- Queensland Government. Births, Deaths, Marriages and Divorces. The State of Queensland 1995–2017. Available online: https://www.qld.gov.au/law/births-deaths-marriages-and-divorces (accessed on 3 December 2017).
- Whyatt, D.; Yap, M.; Tenneti, R.; Pearson, G.; Vickery, A. Hospital use in Aboriginal and non-Aboriginal patients with chronic disease. Emergency Med. Australas. 2017, 29, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Diplock, G.; Ward, J.; Stewart, S.; Scuffham, P.; Stewart, P.; Reeve, C.; Davidson, L.; Maguire, G. The Alice Springs Hospital Readmission Prevention Project (ASHRAPP): A randomised control trial. BMC Health Serv. Res. 2017, 17, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Independent Hospital Pricing Authority (AU). National Hospital Cost Data Collection Cost Report: Round 20 Financial Year 2015–16. Available online: https://www.ihpa.gov.au/sites/g/files/net636/f/publications/nhcdc_cost_report_round_20_financial_year_2015-16.pdf (accessed on 5 May 2018).
- Li, J.Y.Z.; Yong, T.Y.; Hakendorf, P.; Ben-Tovim, D.I.; Tovim, B.; Thompson, C.H. Identifying risk factors and patterns for unplanned readmission to a general medical service. Aust. Health Rev. 2015, 39, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Ride, K. Review of nutrition among Aboriginal and Torres Strait Islander people. Australian Indigenous HealthReviews. 2018. Available online: https://healthinfonet.ecu.edu.au/uploads/docs/nutrition_review_2017.pdf (accessed on 5 May 2018).
- Australian Commission on Safety and Quality in Health Care. Malnutrition. Available online: https://www.safetyandquality.gov.au/wp-content/uploads/2018/03/Malnutrition-detailed-fact-sheet.pdf (accessed on 5 May 2018).
- Van Bokhorst-de van der Schueren, M.A.E.; Guaitoli, P.R.; Jansma, E.P.; de Vet, H.C.E. Nutrition screening tools: Does one size fit all? A systematic review of screening tools for the hospital setting. Clin. Nutr. 2014, 33, 39–58. [Google Scholar] [CrossRef] [PubMed]
| All n = 608 | Nourished (SGA A) n (%) = 358 (58.9) | Malnourished (SGA B or C) n (%) = 250 (41.1) | p Value | ||||
|---|---|---|---|---|---|---|---|
| Age, median (IQR) | 61.6 (49.1–72.2) | 59.2 (48.0–70.5) | 63.4 (50.9–73.3) | 0.009 | |||
| Gender (female), n (%), 95% CI | 294 (48.4) | 44.3–52.4 | 179 (50.0) | 44.7–55.3 | 115 (46.0) | 39.7–52.4 | 0.331 |
| Indigenous status (Indigenous Australian) n (%) 95% CI | 271 (44.6) | 40.6–48.6 | 146 (53.9) | 47.7–59.9 | 125 (46.1) | 40.1–52.3 | 0.024 |
| BMI (kg/m2), median (IQR) | 26.3 (21.6–31.2) | 28.8 (25.4–34.2) | 21.6 (18.8–25.4) | <0.001 | |||
| APACHE III, median (IQR) | 30 (20–30) | 27 (19–36) | 34 (24–44) | <0.001 | |||
| CCI, median (IQR) | 2 (1–3) | 2 (1–3) | 2 (1–4) | <0.001 | |||
| All n = 608 | Nourished (SGA A) n (%) = 358 (58.9) | Malnourished (SGA B or C) n (%) = 250 (41.1) | p Value | ||||
|---|---|---|---|---|---|---|---|
| Length of stay median (IQR) | 4.7 (2.6–9.1) | 4.1 (2.2–7.7) | 5.9 (2.9–11.1) | <0.001 | |||
| Discharge destination n (%), 95% CI | |||||||
| Usual residential address | 503 (82.7) | 79.5–85.7 | 291 (81.3) | 76.9-85.2 | 212 (84.8) | 79.7–89.0 | 0.259 |
| Hospital readmissions n (%), 95% CI | |||||||
| 30 days | 145/591 (24.3) | 20.9–8.0 | 64–346 (18.4) | 14.5–22.9 | 81/245 (32.6) | 26.9–38.8 | <0.001 |
| 6 months | 323/591 (54.2) | 50.1–58.2 | 165/346 (47.4) | 42.1–52.8 | 158/245 (63.7) | 57.4–69.7 | <0.001 |
| Mortality n (%), 95% CI | |||||||
| 30 days | 22/591 (3.7) | 2.3–5.5 | 4/346 (1.2) | 0.3–2.9 | 12/245 (4.9) | 2.6–8.4 | 0.006 |
| 6 months | 55/591 (9.2) | 7.0–11.8 | 14/346 (4.0) | 2.2–6.7 | 35/245 (14.3) | 10.2–19.3 | <0.001 |
| Indigenous Australian n (%) = 271 (44.6) | Non-Indigenous Australian n (%) = 337 (55.4) | p Value | |||
|---|---|---|---|---|---|
| Length of stay, median (IQR) | 5.0 (2.3–9.0) | 4.6 (2.5–9.1) | 0.186 | ||
| Discharge destination n (%), 95% CI | |||||
| usual residential address | 217 (80.1) | 74.8–84.7 | 286 (84.9) | 80.6–88.5 | 0.120 |
| Hospital readmissions n (%), 95% CI | |||||
| 30 days | 73 (27.0) | 21.8–32.8 | 72 (22.1) | 17.7–27.1 | 0.195 |
| 6 months | 169 (62.6) | 56.5–68.4 | 154 (48.0) | 42.4–53.6 | <0.001 |
| Mortality n (%), 95% CI | |||||
| 30 days | 3 (1.1) | 0.2–3.2 | 13 (4.0) | 2.2–6.8 | 0.028 |
| 6 months | 21 (7.8) | 4.9–11.6 | 28 (8.7) | 5.9–12.4 | 0.678 |
| Indigenous Australians n (%) = 271 (44.6) | p Value | Non-Indigenous Australians n (%) = 337 (55.4) | p Value | |||
|---|---|---|---|---|---|---|
| Nourished n (%) = 146 (53.9) | Malnourished n (%) = 125 (46.1) | Nourished n (%) = 212 (62.9) | Malnourished n (%) = 125 (37.1) | |||
| Length of stay median (IQR) | 4.8 (2.3–8.1) | 5.8 (2.8–10.7) | 0.120 | 3.8 (2.0–6.9) | 6.2 (2.9–12.1) | 0.001 |
| Discharge destination (usual address) n (%), 95% CI | 109 (74.7) 66.8–81.5 | 108 (86.4) 79.1–91.9 | 0.016 | 182 (85.8) 80.4–90.2 | 104 (83.2) 75.5–89.3 | 0.512 |
| Hospital readmissions n (%), 95% CI | ||||||
| 30 days | 28 (19.2) 13.1–26.5 | 45 (36.3) 27.8–45.4 | 0.002 | 36 (18.0) 12.9–24.0 | 36 (29.8) 21.2–38.7 | 0.014 |
| 6 months | 82 (56.2) 47.7–64.4 | 87 (70.2) 61.3–78.0 | 0.018 | 83 (41.5) 34.6–48.7 | 71 (58.7) 49.4–67.5 | 0.003 |
| Mortality n (%), 95% CI | ||||||
| 30 days | 1 (0.7) 0.02–3.8 | 2 (1.6) 0.2–5.7 | 0.469 | 3 (1.5) 0.3–4.3 | 10 (8.3) 4.0–14.7 | 0.003 |
| 6 months | 6 (4.1) 1.5–8.7 | 15 (12.1) 6.9–19.2 | 0.015 | 8 (4.0) 1.7–7.7 | 20 (16.5) 10.4–24.4 | <0.001 |
| All n = 608 | Indigenous Australian n = 271 (44.6%) | Non-Indigenous Australian n = 337 (55.4%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Length of hospital stay | Coef | 95% CI | p value | Coef | 95% CI | p value | Coef | 95% CI | p value |
| APACHE III | 15.0 | 7.8–22.3 | <0.001 | 12.1 | 2.2–22.0 | 0.017 | 17.1 | 6.6–27.5 | 0.001 |
| Psuedo R2 % | 2.7 | 2.1 | 3.0 | ||||||
| Six-month readmission | OR | 95% CI | p value | OR | 95% CI | p value | OR | 95% CI | p value |
| Malnourished (SGA B/C) | 1.62 | 1.13–2.31 | 0.008 | 1.75 | 1.05–2.94 | 0.033 | 1.71 | 1.07–2.74 | 0.026 |
| Indigenous Australian (yes) | 1.60 | 1.12–2.27 | 0.009 | - | - | - | - | - | - |
| APACHE III | 1.01 | 1.00–1.03 | 0.045 | - | - | - | - | - | - |
| CCI | 1.23 | 1.10–1.37 | <0.001 | 1.23 | 1.11–1.49 | 0.001 | 1.23 | 1.10–1.47 | 0.001 |
| Psuedo R2 (%) | 6.8 | 5.1 | 4.5 | ||||||
| Six-month mortality | HR | 95% CI | p value | HR | 95% CI | p value | HR | 95% CI | p value |
| Malnourished (SGA B/C) | 2.10 | 1.16–3.79 | 0.014 | 2.72 | 1.04–7.10 | 0.041 | - | - | - |
| Age (years) | 1.04 | 1.02–1.06 | 0.001 | - | - | - | - | - | - |
| APACHE III | 1.03 | 1.01–1.05 | 0.002 | - | - | - | 1.06 | 1.03–1.08 | <0.001 |
| CCI | 1.36 | 1.16–3.79 | 0.014 | 1.48 | 1.27–1.74 | <0.001 | 1.48 | 1.28–1.71 | <0.001 |
| Psuedo R2 (%) | 24.1 | 16.6 | 33.2 | ||||||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morris, N.; Stewart, S.; Riley, M.; Maguire, G. Differential Impact of Malnutrition on Health Outcomes Among Indigenous and Non-Indigenous Adults Admitted to Hospital in Regional Australia—A Prospective Cohort Study. Nutrients 2018, 10, 644. https://doi.org/10.3390/nu10050644
Morris N, Stewart S, Riley M, Maguire G. Differential Impact of Malnutrition on Health Outcomes Among Indigenous and Non-Indigenous Adults Admitted to Hospital in Regional Australia—A Prospective Cohort Study. Nutrients. 2018; 10(5):644. https://doi.org/10.3390/nu10050644
Chicago/Turabian StyleMorris, Natasha, Simon Stewart, Malcolm Riley, and Graeme Maguire. 2018. "Differential Impact of Malnutrition on Health Outcomes Among Indigenous and Non-Indigenous Adults Admitted to Hospital in Regional Australia—A Prospective Cohort Study" Nutrients 10, no. 5: 644. https://doi.org/10.3390/nu10050644
APA StyleMorris, N., Stewart, S., Riley, M., & Maguire, G. (2018). Differential Impact of Malnutrition on Health Outcomes Among Indigenous and Non-Indigenous Adults Admitted to Hospital in Regional Australia—A Prospective Cohort Study. Nutrients, 10(5), 644. https://doi.org/10.3390/nu10050644






