Lactose Maldigestion, Malabsorption, and Intolerance: A Comprehensive Review with a Focus on Current Management and Future Perspectives
Abstract
1. Introduction
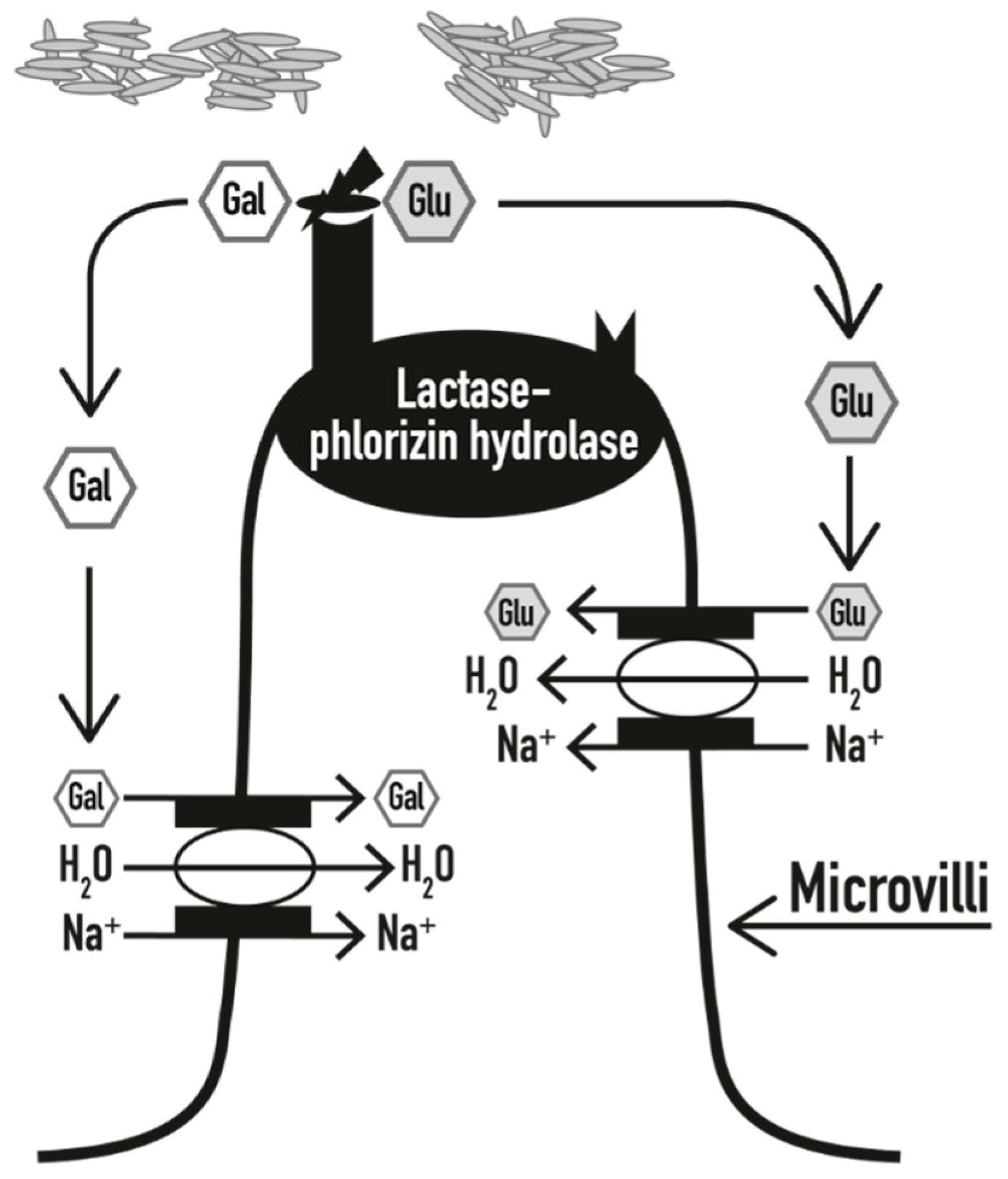
2. Molecular Mechanism of Lactose Maldigestion and Malabsorption
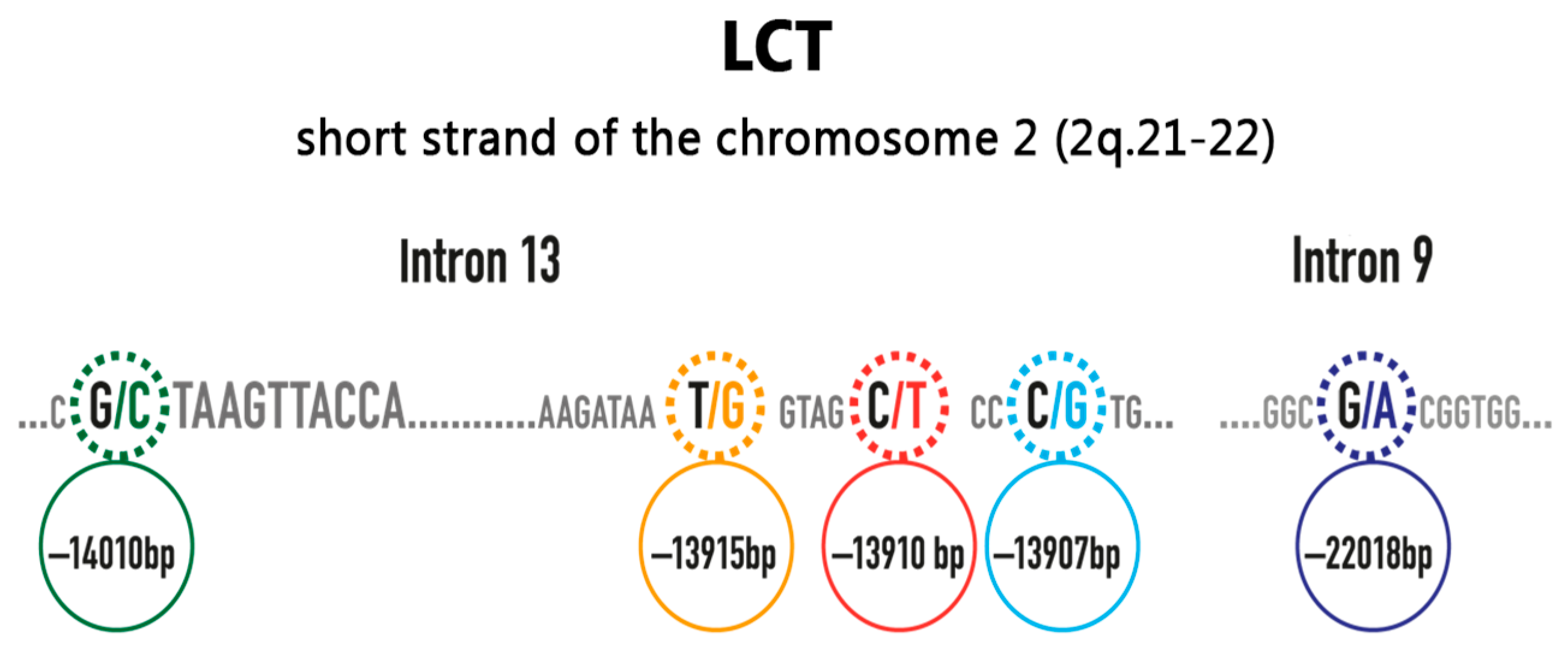
3. Genetic and Biochemical Background
4. Hypolactasia, Lactose Maldigestion, Malabsorption, and Intolerance
- Congenital lactase deficiency (alactasia), which is extremely rare, is due to the inheritance of 2 defective alleles of the LCT gene. The infant can suffer from watery diarrhoea after being fed with breast milk or food containing milk, and it can become a severe condition, as the shortage of nutritive ingredients can lead to growth delay, dehydration, and alkalosis; infants with congenital lactase deficiency were not expected to survive before the 20th century, when adequate lactose-free milk substitutes were not readily accessible [15]
- Primary lactase deficiency (adult-type hypolactasia) is caused by the non-persistence of lactase, with enzyme levels progressively reducing starting from the age of 2–5 years, depending on ethnicity [15]
- Secondary hypolactasia involves the loss of the lactase enzyme due to other clinical conditions affecting the intestinal tract. Since this enzyme is found on the apex of the duodenal villus, all pathological conditions involving the microvilli can result in the reduction of lactase. Once the primary problem is resolved, lactose-containing products can often be consumed normally. Clinical conditions leading to secondary hypolactasia include [5,15,16]:
- -
- severe malnutrition
- -
- celiac disease
- -
- inflammatory bowel diseases (Crohn’s disease, ulcerative colitis)
- -
- bacterial or viral enteritis (e.g., rotavirus), and parasitic disease (e.g., giardiasis, cryptosporidiosis)
- -
- actinic enteritis
- -
- some pharmacological treatments (kanamycin, neomycin, polymycin, tetracycline, colchicine, and other chemotherapeutic drugs)
- -
- some post-surgical conditions, such as stagnant loop syndrome or short bowel syndrome
5. Epidemiology of Lactose Intolerance
6. Clinical Manifestations
7. Diagnosis
8. Management
Probiotics as a Future Option in the Management of Lactose Intolerance
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Franzè, A.; Bertelè, A. Intolleranza al lattosio nella pratica clinica. Rivista della Società Italiana di Medicina Generale 2010, 3, 36–40. [Google Scholar]
- Harrington, L.K.; Mayberry, J.F. A re-appraisal of lactose intolerance. Int. J. Clin. Pract. 2008, 62, 1541–1546. [Google Scholar] [CrossRef] [PubMed]
- Matthews, S.B.; Waud, J.P.; Roberts, A.G.; Campbell, A.K. Systemic lactose intolerance: A new perspective on an old problem. Postgrad. Med. J. 2005, 81, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Brüssow, H. Nutrition, population growth and disease: A short history of lactose. Environ. Microbiol. 2013, 15, 2154–2161. [Google Scholar] [CrossRef] [PubMed]
- Lomer, M.C.E.; Parkes, G.C.; Sanderson, J.D. Review article: Lactose intolerance in clinical practice—And realities. Aliment. Pharmacol. Ther. 2008, 27, 93–103. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.; Misselwitz, B.; Dai, N.; Fox, M. Lactose intolerance in adults: Biological mechanism and dietary management. Nutrients 2015, 7, 8020–8035. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.K.; Waud, J.P.; Matthews, S.B. The molecular basis of lactose intolerance. Sci. Prog. 2009, 92, 241–287. [Google Scholar] [CrossRef] [PubMed]
- Oftedal, O.T. The evolution of milk secretion and its ancient origins. Animal 2012, 6, 355–368. [Google Scholar] [CrossRef] [PubMed]
- Enattah, N.S.; Sahi, T.; Savilahti, E.; Terwilliger, J.D.; Peltonen, L.; Järvelä, I. Identification of a variant associated with adult-type hypolactasia. Nat. Genet. 2002, 30, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Itan, Y.; Jones, B.L.; Ingram, C.J.; Swallow, D.M.; Thomas, M.G. A worldwide correlation of lactase persistence phenotype and genotypes. BMC Evol. Biol. 2010, 10, 36. [Google Scholar] [CrossRef] [PubMed]
- Mattar, R.; do Socorro Monteiro, M.; Villares, C.A.; dos Santos, A.F.; Carrilho, F.J. Single nucleotide polymorphism c/t-13910, located upstream of the lactase gene, associated with adult-type hypolactasia: Validation for clinical practice. Clin. Biochem. 2008, 41, 628–630. [Google Scholar] [CrossRef] [PubMed]
- Troelsen, J.T. Adult-type hypolactasia and regulation of lactase expression. Biochim. Biophys. Acta 2005, 1723, 19–32. [Google Scholar] [CrossRef] [PubMed]
- Tishkoff, S.A.; Reed, F.A.; Ranciaro, A.; Voight, B.F.; Babbitt, C.C.; Silverman, J.S.; Powell, K.; Mortensen, H.M.; Hirbo, J.B.; Osman, M.; et al. Convergent adaptation of human lactase persistence in Africa and Europe. Nat. Genet. 2007, 39, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Misselwitz, B.; Pohl, D.; Frühauf, H.; Fried, M.; Vavricka, S.R.; Fox, M. Lactose malabsorption and intolerance: Pathogenesis, diagnosis and treatment. United Eur. Gastroenterol. J. 2013, 1, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Heyman, M.B. Committee on Nutrition. Lactose intolerance in infants, children, and adolescents. Pediatrics 2006, 118, 1279–1286. [Google Scholar] [CrossRef] [PubMed]
- Saavedra, J.M.; Perman, J.A. Current concepts in lactose malabsorption and intolerance. Annu. Rev. Nutr. 1989, 9, 475–502. [Google Scholar] [CrossRef] [PubMed]
- Swallow, D.M. Genetics of lactase persistence and lactose intolerance. Annu. Rev. Genet. 2003, 37, 197–219. [Google Scholar] [CrossRef] [PubMed]
- European Food Safety Authority (EFSA). Scientific opinion on lactose thresholds in lactose intolerance and galactosaemia. EFSA J. 2010, 8, 1777. [Google Scholar] [CrossRef]
- Dainese, R.; Casellas, F.; Mariné–Barjoan, E.; Vivinus-Nébot, M.; Schneider, S.M.; Hébuterne, X.; Piche, T. Perception of lactose intolerance in irritable bowel syndrome patients. Eur. J. Gastroenterol. Hepatol. 2014, 26, 1167–1175. [Google Scholar] [CrossRef] [PubMed]
- Shaukat, A.; Levitt, M.D.; Taylor, B.C.; MacDonald, R.; Shamliyan, T.A.; Kane, R.L.; Wilt, T.J. Systematic review: Effective management strategies for lactose intolerance. Ann. Intern. Med. 2010, 152, 797–803. [Google Scholar] [CrossRef] [PubMed]
- Furnari, M.; Bonfanti, D.; Parodi, A.; Franzè, J.; Savarino, E.; Bruzzone, L.; Moscatelli, A.; Di Mario, F.; Dulbecco, P.; Savarino, V. A comparison between lactose breath test and quick test on duodenal biopsies for diagnosing lactase deficiency in patients with self-reported lactose intolerance. J. Clin. Gastroenterol. 2013, 47, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Law, D.; Conklin, J.; Pimentel, M. Lactose intolerance and the role of the lactose breath test. Am. J. Gastroenterol. 2010, 105, 1726–1728. [Google Scholar] [CrossRef] [PubMed]
- Rezaie, A.; Buresi, M.; Lembo, A.; Lin, H.; McCallum, R.; Rao, S.; Schmulson, M.; Valdovinos, M.; Zakko, S.; Pimentel, M. Hydrogen and methane-based breath testing in gastrointestinal disorders: The North American consensus. Am. J. Gastroenterol. 2017, 112, 775–784. [Google Scholar] [CrossRef] [PubMed]
- Wilder-Smith, C.H.; Materna, A.; Wermelinger, C.; Schuler, J. Fructose and lactose intolerance and malabsorption testing: The relationship with symptoms in functional gastrointestinal disorders. Aliment. Pharmacol. Ther. 2013, 37, 1074–1083. [Google Scholar] [CrossRef] [PubMed]
- Pohl, D.; Savarino, E.; Hersberger, M.; Behlis, Z.; Stutz, B.; Goetze, O.; Eckardstein, A.V.; Fried, M.; Tutuian, R. Excellent agreement between genetic and hydrogen breath tests for lactase deficiency and the role of extended symptom assessment. Columbia J. Nutr. 2010, 104, 900–907. [Google Scholar] [CrossRef] [PubMed]
- The European Parliament and the Council of the European Union: Regulation (EU) No 1169/2011 of the European Parliament and of the Council of 25 October 2011 on the provision of food information to Consumers, Amending Regulations (EC) No 1924/2006 and (EC) No 1925/2006 of the European Parliament and of the Council. Available online: https://eur-lex.europa.eu/eli/reg/2011/1169/oj (accessed on 1 May 2018).
- Ojetti, V.; Gigante, G.; Gabrielli, M.; Ainora, M.E.; Mannocci, A.; Lauritano, E.C.; Gasbarrini, G.; Gasbarrini, A. The effect of oral supplementation with Lactobacillus reuteri or tilactase in lactose intolerant patients: Randomized trial. Eur. Rev. Med. Pharmacol. Sci. 2010, 14, 163–170. [Google Scholar] [PubMed]
- Montalto, M.; Nucera, G.; Santoro, L.; Curigliano, V.; Vastola, M.; Covino, M.; Cuoco, L.; Manna, R.; Gasbarrini, A.; Gasbarrini, G. Effect of exogenous β-galactosidase in patients with lactose malabsorption and intolerance: A crossover double-blind placebo-controlled study. Eur. J. Clin. Nutr. 2005, 59, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Hertzler, S.R.; Savaiano, D.A. Colonic adaptation to daily lactose feeding in lactose maldigesters reduces lactose intolerance. Am. J. Clin. Nutr. 1996, 64, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Briet, F.; Pochart, P.; Marteau, P.; Flourie, B.; Arrigoni, E.; Rambaud, J.C. Improved clinical tolerance to chronic lactose ingestion in subjects with lactose intolerance: A placebo effect? Gut 1997, 41, 632–635. [Google Scholar] [CrossRef] [PubMed]
- Cappello, G.; Marzio, L. Rifaximin in patients with lactose intolerance. Dig. Liver Dis. 2005, 37, 316–319. [Google Scholar] [CrossRef] [PubMed]
- Joint FAO/WHO Expert Consultation. Health and Nutritional Properties of Probiotics in Food including Powder Milk with Live Lactic Acid Bacteria; FAO/WHO: Cordoba, Argentina, 2001. [Google Scholar]
- Gallagher, C.R.; Molleson, A.L.; Caldwell, J.H. Lactose intolerance and fermented dairy products. J. Am. Diet. Assoc. 1974, 65, 418–419. [Google Scholar] [PubMed]
- Savaiano, D.A. Lactose digestion from yogurt: Mechanism and relevance. Am. J. Clin. Nutr. 2014, 99 (Suppl. 5), 1251S–1255S. [Google Scholar] [CrossRef] [PubMed]
- Almeida, C.C.; Lorena, S.L.S.; Pavan, C.R.; Akasaka, H.M.I.; Mesquita, M.A. Beneficial effects of long-term consumption of a probiotic combination of lactobacillus casei shirota and bifidobacterium breve yakult may persist after suspension of therapy in lactose-intolerant patients. Nutr. Clical Pr. 2012, 27, 247–251. [Google Scholar] [CrossRef] [PubMed]
- He, T.; Priebe, M.G.; Zhong, Y.; Huang, C.; Harmsen, H.J.M.; Raangs, G.C.; Antoine, J.-M.; Welling, G.W.; Vonk, R.J. Effects of yogurt and bifidobacteria supplementation on the colonic microbiota in lactose-intolerant subjects. J. Appl. Microbiol. 2007, 104, 595–604. [Google Scholar] [CrossRef] [PubMed]
- FAO/WHO. Guidelines for the Evaluation of Probiotics in Food; Joint FAO/WHO Working Group Report on Drafting Guidelines for the Evaluation of Probiotics in Food; FAO/WHO: London, ON, Canada, 2002. [Google Scholar]
- Hill, C.; Guarner, F.; Reid, G.; Gibson, G.R.; Merenstein, D.J.; Pot, B.; Morelli, L.; Canani, R.B.; Flint, H.J.; Salminen, S.; et al. Expert consensus document: The international scientific association for probiotics and prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 506–514. [Google Scholar] [CrossRef] [PubMed]
- Ducrotté, P. Clinical trial: Lactobacillus plantarum 299v (dsm 9843) improves symptoms of irritable bowel syndrome. World J. Gastroenterol. 2012, 18, 4012. [Google Scholar] [CrossRef] [PubMed]
- Sinn, D.H.; Song, J.H.; Kim, H.J.; Lee, J.H.; Son, H.J.; Chang, D.K.; Kim, Y.-H.; Kim, J.J.; Rhee, J.C.; Rhee, P.-L. Therapeutic effect of lactobacillus acidophilus-sdc 2012, 2013 in patients with irritable bowel syndrome. Dig. Dis. Sci. 2008, 53, 2714–2718. [Google Scholar] [CrossRef] [PubMed]
- Rossi, R.; Rossi, L.; Fassio, F. Clinical follow-up of 96 patients affected by irritable bowel syndrome treated with a novel multi-strain symbiotic. J. Contemp. Immunol. 2015. [Google Scholar] [CrossRef]
- Li, J.; Zhang, W.; Wang, C.; Yu, Q.; Dai, R.; Pei, X. Lactococcus lactis expressing food-grade β-galactosidase alleviates lactose intolerance symptoms in post-weaning Balb/c mice. Appl. Microbiol. Biotechnol. 2012, 96, 1499–1506. [Google Scholar] [CrossRef] [PubMed]
- Saltzman, J.R.; Russell, R.M.; Golner, B.; Barakat, S.; Dallal, G.E.; Goldin, B.R. A randomized trial of Lactobacillus acidophilus BG2FO4 to treat lactose intolerance. Am. J. Clin. Nutr. 1999, 69, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Masood, M.I.; Qadir, M.I.; Shirazi, J.H.; Khan, I.U. Beneficial effects of lactic acid bacteria on human beings. Crit. Rev. Microbiol. 2011, 37, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Sanders, M.E.; Guarner, F.; Guerrant, R.; Holt, P.R.; Quigley, E.M.M.; Sartor, R.B.; Sherman, P.M.; Mayer, E.A. An update on the use and investigation of probiotics in health and disease. Gut 2013, 62, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Besseling-van der Vaart, I.; Heath, M.D.; Guagnini, F.; Kramer, M.F. In vitro evidence for efficacy in food intolerance for the multispecies probiotic formulation ecologic® tolerance (syngutTM). Benef. Microbes 2016, 7, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Miller, F. Glycopeptides of human immunoglobulins. 3. The use and preparation of specific glycosidases. Immunochemistry 1972, 9, 217–228. [Google Scholar] [CrossRef]
- Oak, S.J.; Jha, R. The effects of probiotics in lactose intolerance: A systematic review. Crit. Rev. Food Sci. Nutr. 2018, 8398, 1–9. [Google Scholar] [CrossRef] [PubMed]
| Hypolactasia | Any deficiency of the lactase enzyme |
| Lactase non-persistence | This is considered the “wild-type” condition, as most individuals have reduced lactase activity at the jejunal border after weaning. In a minority of humans, a high level of activity of the lactase enzyme is present through all adulthood (lactase persistence phenotype) |
| Lactose maldigestion | Inefficient digestion of lactose, due to lactase deficiency (either lactase non-persistence or other intestinal conditions) |
| Lactose malabsorption | Inefficient absorption of lactose, due to lactose maldigestion, as lactose cannot be absorbed in the undigested form |
| Lactose intolerance | Gastrointestinal symptoms due to lactose malabsorption |
| Symptoms of Lactose Intolerance | Frequency (% of Total) | |
|---|---|---|
| Gut-related symptoms | Abdominal pain | ~100 |
| Gut distension | ~100 | |
| Borborygmi | ~100 | |
| Flatulence | ~100 | |
| Diarrhoea | 70 | |
| Constipation | 30 | |
| Nausea | 78 | |
| Vomiting | 78 | |
| Systemic symptoms | Headache | 86 |
| Loss of concentration | 82 | |
| Tiredness | 63 | |
| Muscle pain | 71 | |
| Joint pain/stiffness | 71 | |
| Mouth ulcers | 30 | |
| Increased frequency of micturition | <20 | |
| Summary of Available Tests for Assessing Lactose Malabsorption/Intolerance | ||||
|---|---|---|---|---|
| Lactose Tolerance Test | H2-Breath Test (HBT) | Genetic Test | Lactose Activity at Jejunal Brush Border | |
| Test principle | Increase of glycaemia after lactose challenge | Increase of H2 in expirate after lactose challenge | Assessment of 13910C/T polymorphism | Lactase enzymatic activity in bioptic sample |
| Cut-off criterion | <1.1 mmol/L within 3 h | >20 ppm within 3 h | C:C13910 Lactase non-persistence phenotype | <17–20 IU/g |
| Availability | Excellent | Good | Good | Rare |
| False positives | Rapid GI-transit, impaired glucose tolerance | Rapid GI-transit, SIBO | Rare (<5%) in Caucasians | Most likely, rare |
| False negatives | Fluctuations in glycaemia | Non-H2-producers, full colonic adaptation | All causes of secondary lactose malabsorption | Patchy enzyme expression |
| Secondary causes | Cannot be excluded | Cannot be excluded, kinetics of H2-increase can be suggestive | Cannot be excluded | Can be excluded (histopathology during same procedure) |
| Symptoms assessment | Possible | Possible | Not possible | Not possible |
| Cost | Lowest | Low | Medium | Highest |
| Comment | Low sensitivity and specificity | Method of choice for assessment of primary and secondary lactose intolerance | Method of choice for assessment of primary lactase deficiency in Caucasians | Invasive and expensive testing |
| Probiotic Strains | β-Galactosidase Activity Level |
|---|---|
| Bifidobacterium lactis W52 | ++++ |
| Bifidobacterium lactis W51 | +++ |
| Lactobacillus acidophilus W22 | +++++ |
| Lactobacillus acidophilus W70 | +++++ |
| Lactobacillus brevis W78 | + |
| Lactobacillus casei W20 | + |
| Lactobacillus casei W79 | ++ |
| Lactobacillus plantarum W21 | + |
| Lactobacillus rhamnosus W71 | + |
| Lactobacillus salivarius W24 | +++++ |
| Lactococcus lactis W19 | + |
| Streptococcus thermophilus W69 | +++++ |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fassio, F.; Facioni, M.S.; Guagnini, F. Lactose Maldigestion, Malabsorption, and Intolerance: A Comprehensive Review with a Focus on Current Management and Future Perspectives. Nutrients 2018, 10, 1599. https://doi.org/10.3390/nu10111599
Fassio F, Facioni MS, Guagnini F. Lactose Maldigestion, Malabsorption, and Intolerance: A Comprehensive Review with a Focus on Current Management and Future Perspectives. Nutrients. 2018; 10(11):1599. https://doi.org/10.3390/nu10111599
Chicago/Turabian StyleFassio, Filippo, Maria Sole Facioni, and Fabio Guagnini. 2018. "Lactose Maldigestion, Malabsorption, and Intolerance: A Comprehensive Review with a Focus on Current Management and Future Perspectives" Nutrients 10, no. 11: 1599. https://doi.org/10.3390/nu10111599
APA StyleFassio, F., Facioni, M. S., & Guagnini, F. (2018). Lactose Maldigestion, Malabsorption, and Intolerance: A Comprehensive Review with a Focus on Current Management and Future Perspectives. Nutrients, 10(11), 1599. https://doi.org/10.3390/nu10111599




