Low-Salt Intake Suggestions in Hypertensive Patients Do not Jeopardize Urinary Iodine Excretion
Abstract
:1. Introduction
2. Materials and Methods
Statistics
3. Results
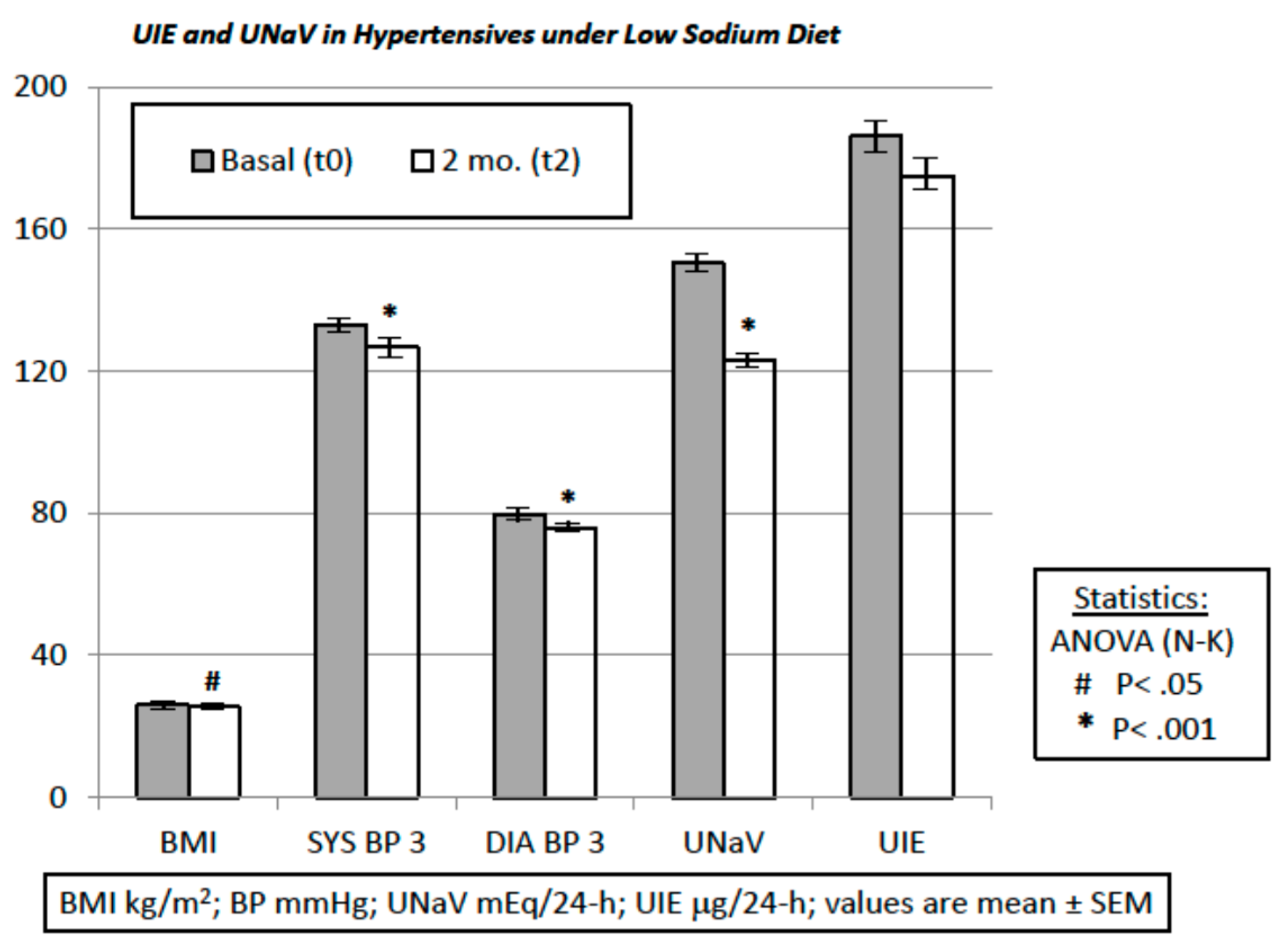
- BMI was 25.86 ± 0.40 kg/m2 before the dietary suggestions (visit t0) and 25.38 ± 0.37 kg/m2 afterwards (visit t2) (t-test and repeated-measures ANOVA and Newman-Keuls post-test, p < 0.05).
- UNaV decreased from 150.3 ± 4.01 mEq/24-h at visit t0 to 122.8 ± 3.92 mEq/24-h at visit t2 (repeated-measures ANOVA and post-test, p < 0.001).
- Both systolic and diastolic BP values decreased significantly from visit t0 to visit t2 (by 6.15 ± 1.32 mmHg and by 3.75 ± 0.94 mmHg, respectively. ANOVA and post-test, p < 0.001) (Figure 1).
- Drug consumption also decreased from visit t0 to visit t2 (ΔDDD 0.29 ± 0.06, t-test, p < 0.05).
- Median UIE global values were 184.2 µg/24-h (lower and upper 95% CI 170.3 and 201.9) at t0, and 162.0 µg/24-h (lower and upper 95% CI 159.6 and 190.3) at t2.
- Median UIE values in females were 178.2 µg/24-h (lower and upper 95% CI 163.0 and 204.3) at t0, and 153.7 µg/24-h (lower and upper 95% CI 151.3 and 188.5) at t2.
- Median UIE values in males were 188.0 µg/24-h (lower and upper 95% CI 164.9 and 215.2) at t0, and 170.0 µg/24-h (lower and upper 95% CI 155.9 and 210.5) at t2. One way ANOVA (F = 0.6105, R square 0.006788) showed non-significant differences between UIE values in males vs. females both before and after the diet period (p = 0.6087). Bartlett’s test for equal variances gave non-significant results (Bartlett’s statistics 1.449, p = 0.6940, Newman-Keuls multiple comparison test p > 0.05).
- UIE was below 100 µg/24-h in 28 patients before the suggested diet, and in 28 patients thereafter (Fisher’s exact test: p = NS; Chi-square, df: 0.0, 1; p = NS).
- UIE decreased from 186.1 ± 7.95 µg/24-h at visit t0, to 175.0 ± 7.74 µg/24-h at visit t2 (repeated-measures ANOVA and post-test, p = NS). Furthermore, these data were reanalyzed with non-parametric tests (Mann-Whitney, or Welch correction, t = 1.002, df = 269, 95% C.I. −10.67 to +32.97), to avoid distributional assumptions (again, differences were non-significant: p = 0.2737 to p = 0.3173). A possible UIE variability induced by the dietary suggestions was challenged with an F test to compare variances before and after the observation period. F test showed non-significant differences (F, DFn, Dfd, 1057, 135, 135; p = 0.7484).
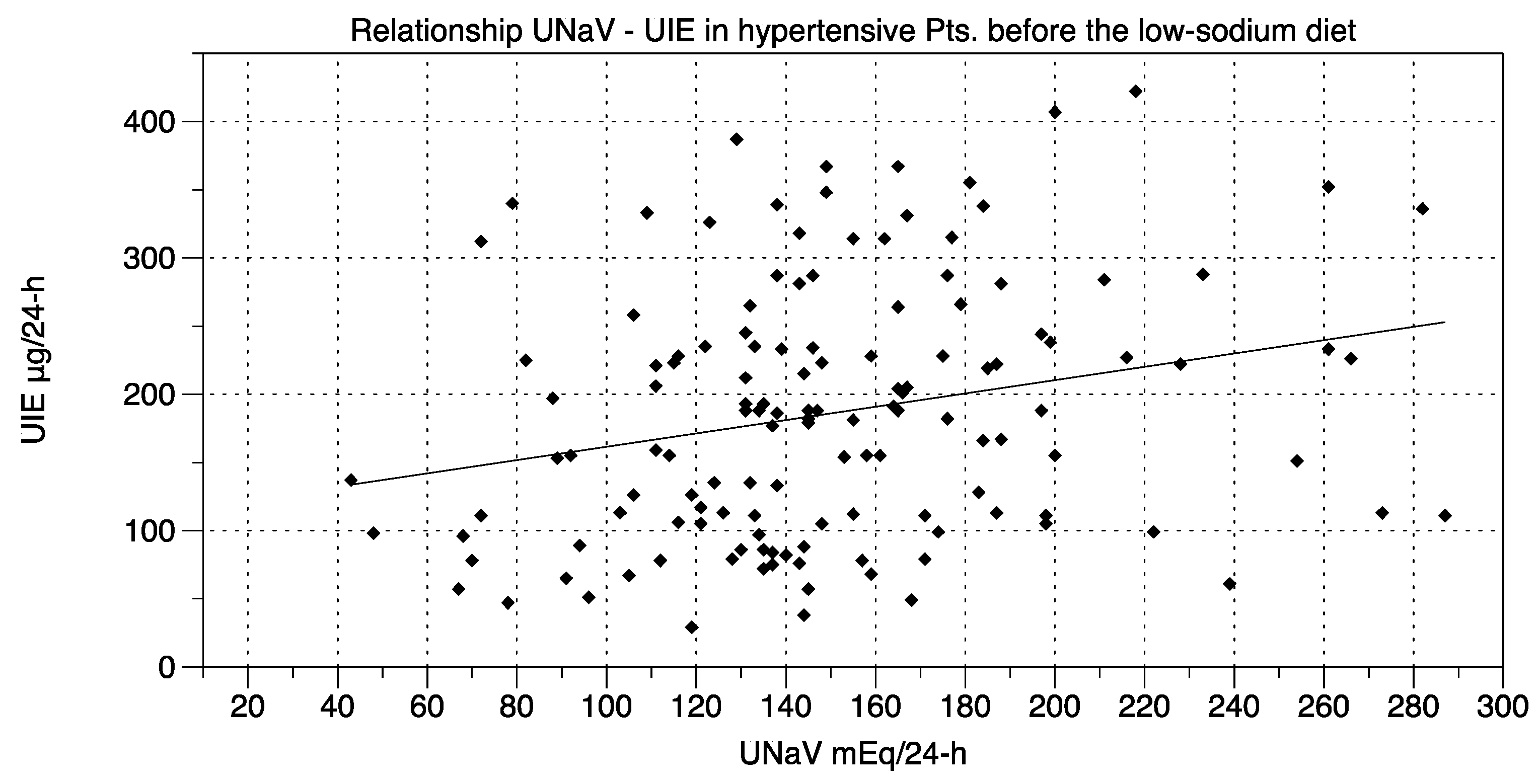
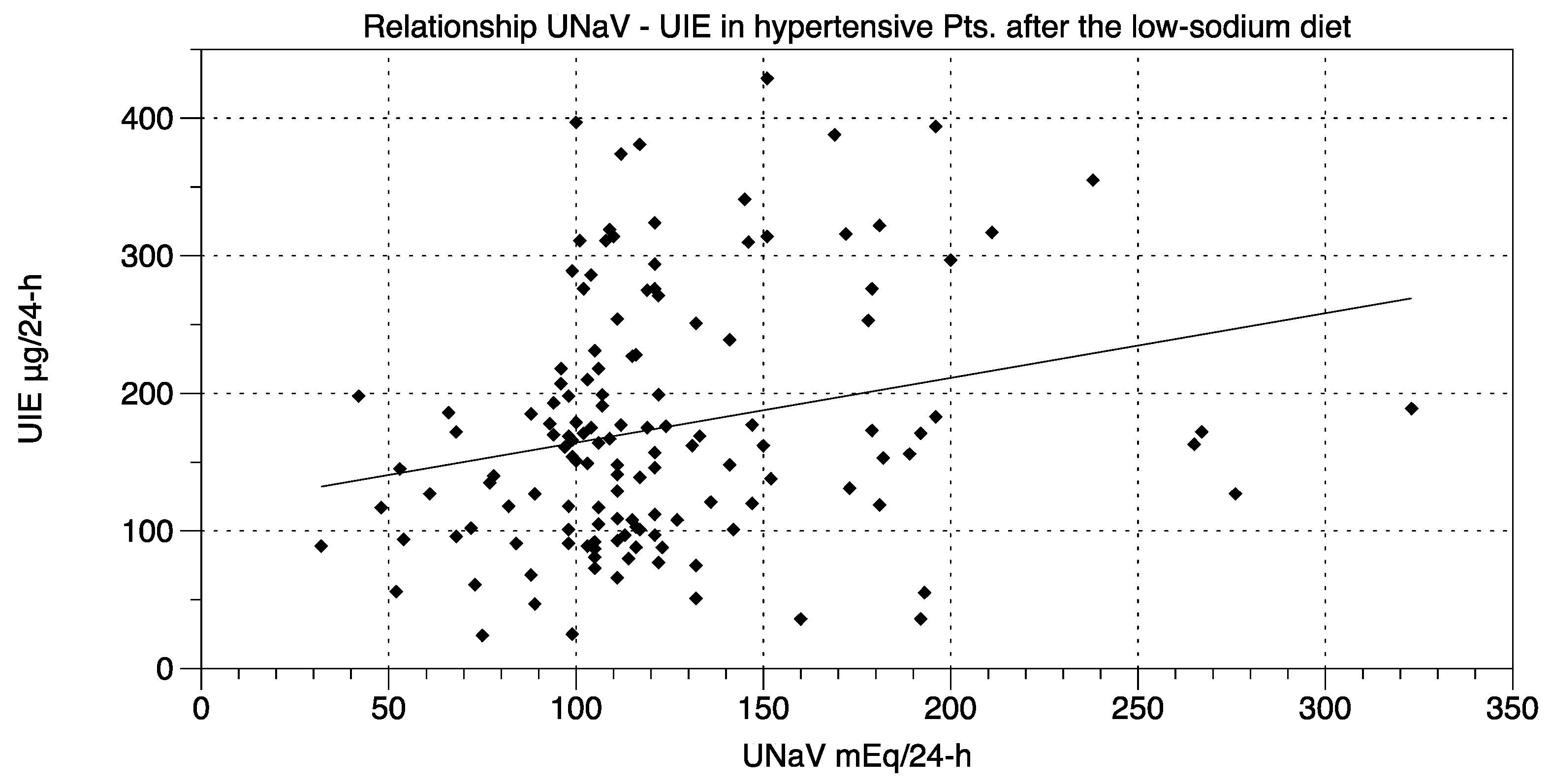
- UNaV and UIE were significantly associated both before and after the dietary suggestions (Chi-square test; df at t0 75.55, 1; df at t2 205.6, 1; p < 0.0001 for both).
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- James, P.A.; Oparil, S.; Carter, B.L.; Cushman, W.C.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, D.T.; LeFevre, M.L.; MacKenzie, T.D.; Ogedegbe, O.; et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014, 311, 507–520. [Google Scholar] [CrossRef] [PubMed]
- Van Horn, L.; Carson, J.A.S.; Appel, L.J.; Burke, L.E.; Economos, C.; Karmally, W.; Lancaster, K.; Lichtenstein, A.H.; Johnson, R.K.; Thomas, R.J.; et al. Recommended dietary pattern to achieve adherence to the American Heart Association/American College of Cardiology (AHA/ACC) Guidelines: A scientific statement from the American Heart Association. Circulation 2016, 134, e505–e529. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. Hypertension 2018. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Strazzullo, P.; D’Elia, L.; Kandala, N.B.; Cappuccio, F.P. Salt intake, stroke, and cardiovascular disease: Meta-analysis of prospective studies. BMJ 2009, 339, b4567. [Google Scholar] [CrossRef] [PubMed]
- He, F.J.; MacGregor, G.A. Salt reduction lowers cardiovascular risk: Meta-analysis of outcome trials. Lancet 2011, 378, 380–382. [Google Scholar] [CrossRef]
- Taylor, R.S.; Ashton, K.E.; Moxham, T.; Hooper, L.; Ebrahim, S. Reduced dietary salt for the prevention of cardiovascular disease: A meta-analysis of randomized controlled trials (Cochrane review). Am. J. Hypertens. 2011, 24, 843–853. [Google Scholar] [CrossRef] [PubMed]
- Bram, B.; Huang, X.; Cupples, W.A.; Hamza, S.M. Understanding the two faces of low-salt intake. Curr. Hypertens. Rep. 2017, 19, 49. [Google Scholar] [CrossRef] [PubMed]
- Graudal, N.; Jurgens, G.; Baslund, B.; Alderman, M.H. Compared with usual sodium intake, low- and excessive-sodium diets are associated with increased mortality: A meta-analysis. Am. J. Hypertens. 2014, 27, 1129–1137. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M.; Mente, A.; Rangarajan, S.; McQueen, M.J.; Wang, X.; Liu, L.; Yan, H.; Lee, S.F.; Mony, P.; Devanath, A.; et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N. Engl. J. Med. 2014, 371, 612–623. [Google Scholar] [CrossRef] [PubMed]
- Oparil, S. Low sodium intake-Cardiovascular health benefit or risk? N. Engl. J. Med. 2014, 371, 677–679. [Google Scholar] [CrossRef] [PubMed]
- Kimball, O.P. Endemic goiter and public health. Am. J. Public Health Nations Health 1928, 18, 587–601. [Google Scholar] [CrossRef] [PubMed]
- Bath, S.C. The challenges of harmonising the iodine supply across Europe. Lancet Diabetes Endocrinol. 2017, 5, 411–412. [Google Scholar] [CrossRef]
- Lazarus, J.H. Iodine status in Europe in 2014. Eur. Thyroid J. 2014, 3, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Olivieri, A.; Di Cosmo, C.; De Angelis, S.; Da Cas, R.; Stacchini, P.; Pastorelli, A.; Vitti, P. Regional Observatory for Goiter Prevention. The way forward in Italy for iodine. Minerva Med. 2017, 108, 159–168. [Google Scholar] [PubMed]
- World Health Organization. Salt Reduction and Iodine Fortification Strategies in Public Health; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Tayie, F.A.; Jourdan, K. Hypertension, dietary salt restriction and iodine deficiency among adults. Am. J. Hypertens. 2010, 23, 1095–1102. [Google Scholar] [CrossRef] [PubMed]
- Pearce, E.N.; Andersson, M.; Zimmermann, M.B. Global iodine nutrition: Where do we stand in 2013? Thyroid 2013, 23, 523–528. [Google Scholar] [CrossRef] [PubMed]
- McLean, R.M.; Farmer, V.L.; Nettleton, A.; Cameron, C.M.; Cook, N.R.; Campbell, N.R.C.; TRUE Consortium. Assessment of dietary sodium intake using food frequency questionnaires and 24-hour urinary sodium excretion: A systematic literature review. J. Clin. Hypertens. 2017, 19, 1214–1230. [Google Scholar] [CrossRef] [PubMed]
- Ji, C.; Lu, T.; Dary, O.; Legetic, B.; Campbell, N.R.; Cappuccio, F.P. Systematic review of studies evaluating urinary iodine concentration as a predictor of 24 hour urinary iodine excretion for estimating population iodine intake. Rev. Panam. Salud Publica 2015, 38, 73–81. [Google Scholar] [PubMed]
- Conkle, J.; van der Haar, F. The use and interpretation of sodium concentrations in casual (spot) urine collections for population surveillance and partitioning of dietary iodine intake sources. Nutrients 2017, 9, 7. [Google Scholar] [CrossRef] [PubMed]
- Charlton, K.E.; Jooste, P.L.; Steyn, K.; Levitt, N.S.; Ghosh, A. A lowered salt intake does not compromise iodine status in Capetown, South Africa, where salt iodization is mandatory. Nutrition 2013, 29, 630–634. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.; Lee, J.H.; Lee, J.; Baek, J.Y.; Song, E.; Oh, H.S.; Kim, M.; Park, S.; Jeon, M.J.; Kim, T.Y.; et al. Association between urinary sodium levels and iodine status in Korea. Korean J. Int. Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Simpson, F.O.; Thaler, B.I.; Paulin, J.M.; Phelan, E.L.; Cooper, G.J. Iodide excretion in a salt-restriction trial. N. Z. Med. J. 1984, 97, 890–893. [Google Scholar] [PubMed]
- He, F.J.; Ma, Y.; Feng, X.; Zhang, W.; Lin, L.; Guo, X.; Zhang, J.; Niu, W.; Wu, Y.; MacGregor, G.A. Effect of salt reduction on iodine status assessed by 24 hour urinary iodine excretion in children and their families in northern China: A substudy of a cluster randomised controlled trial. BMJ Open 2016, 6, e011168. [Google Scholar] [CrossRef] [PubMed]
- Vega-Vega, O.; Fonseca-Correa, J.I.; Mendoza-De la Garza, A.; Rincon-Pedrero, R.; Espinosa-Cuevas, A.; Baeza-Arias, Y.; Dary, O.; Herrero-Bervera, B.; Nieves-Anaya, I.; Correa-Rotter, R. Contemporary dietary intake: Too much sodium, not enough potassium, yet sufficient iodine: The SALMEX Cohort study. Nutrients 2018, 10, 816. [Google Scholar] [CrossRef] [PubMed]
- Charlton, K.; Ware, L.J.; Baumgartner, J.; Cockeran, M.; Schutte, A.E.; Naidoo, N.; Kowal, P. How will South Africa’s mandatory salt reduction policy affect its salt iodisation programme? A cross-sectional analysis from the WHO-SAGE Wave 2 Salt & Tobacco study. BMJ Open 2018, 8, e020404. [Google Scholar] [PubMed] [Green Version]
- Pastorelli, A.A.; Stacchini, P.; Olivieri, A. Daily iodine intake and the impact of salt reduction on iodine prophylaxis in the Italian population. Eur. J. Clin. Nutr. 2015, 69, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Monitoring of the Nationwide Program of Iodine Prophylaxis in Italy. Available online: http://old.iss.it/binary/publ/cont/14_6_web.pdf (accessed on 15 August 2018).
- Musso, N.; Carloni, B.; Chiusano, M.C.; Giusti, M. Simple dietary advice reduces 24-hour urinary sodium excretion, blood pressure, and drug consumption in hypertensive patients. J. Am. Soc. Hypertens. 2018, 12, 652–659. [Google Scholar] [CrossRef] [PubMed]
- WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC Classification and DDD Assignment; Norwegian Institute of Public Health: Oslo, Norway, 2017.
- Greenblatt, D.J.; Ransil, B.J.; Harmatz, J.S.; Smith, T.W.; Duhme, D.W.; Koch-Weser, J. Variability of 24-hour urinary creatinine excretion by normal subjects. J. Clin. Pharmacol. 1976, 16, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Sawant, P.D.; Kumar, S.A.; Wankhede, S.; Rao, D.D. Creatinine as a normalization factor to estimate the representativeness of urine sample. Intra-subject and inter-subject variability studies. Appl. Radiat. Isot. 2018, 136, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Murakami, K.; Sasaki, S.; Takahashi, Y.; Uenishi, K.; Watanabe, T.; Kohri, T.; Yamasaki, M.; Watanabe, R.; Baba, K.; Shibata, K.; et al. Sensitivity and specificity of published strategies using urinary creatinine to identify incomplete 24-h urine collection. Nutrition 2008, 24, 16–22. [Google Scholar] [CrossRef] [PubMed]
- John, K.A.; Cogswell, M.E.; Campbell, N.R.; Nowson, C.A.; Legetic, B.; Hennis, A.J.M.; Patel, S.M. Accuracy and usefulness of select methods for assessing complete collection of 24-hour urine: A systematic review. J. Clin. Hypertens. 2016, 18, 456–467. [Google Scholar] [CrossRef] [PubMed]
- Nath, S.K.; Moinier, B.; Thuillier, F.; Rongier, M.; Desjeux, J.F. Urinary excretion of iodide and fluoride from supplemented food grade salt. Int. J. Vitam. Nutr. Res. 1992, 62, 66–72. [Google Scholar] [PubMed]
- WHO-Salt Reduction. Available online: https://www.who.int/news-room/fact-sheets/detail/salt-reduction (accessed on 15 August 2018).
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Musso, N.; Conte, L.; Carloni, B.; Campana, C.; Chiusano, M.C.; Giusti, M. Low-Salt Intake Suggestions in Hypertensive Patients Do not Jeopardize Urinary Iodine Excretion. Nutrients 2018, 10, 1548. https://doi.org/10.3390/nu10101548
Musso N, Conte L, Carloni B, Campana C, Chiusano MC, Giusti M. Low-Salt Intake Suggestions in Hypertensive Patients Do not Jeopardize Urinary Iodine Excretion. Nutrients. 2018; 10(10):1548. https://doi.org/10.3390/nu10101548
Chicago/Turabian StyleMusso, Natale, Lucia Conte, Beatrice Carloni, Claudia Campana, Maria C. Chiusano, and Massimo Giusti. 2018. "Low-Salt Intake Suggestions in Hypertensive Patients Do not Jeopardize Urinary Iodine Excretion" Nutrients 10, no. 10: 1548. https://doi.org/10.3390/nu10101548
APA StyleMusso, N., Conte, L., Carloni, B., Campana, C., Chiusano, M. C., & Giusti, M. (2018). Low-Salt Intake Suggestions in Hypertensive Patients Do not Jeopardize Urinary Iodine Excretion. Nutrients, 10(10), 1548. https://doi.org/10.3390/nu10101548





